1. Introduction
With the rapid development of society, people’s lifestyles and eating habits have gradually changed. Gastrointestinal diseases in the population have been widespread. Peptic ulcer is now one of the most serious gastrointestinal diseases, which not only seriously affects the health and quality of life of contemporary people, but also leads to a large health care cost and social burden and is considered a global public health problem [
1]. Peptic ulcer disease is a multifactorial and complex disease involving gastric and duodenal ulcers, mainly occurring in the stomach and duodenal bulb. It is generally accepted that peptic ulcer is the result of an imbalance between the protective factors of the gastric and duodenal mucosa and the factors that cause gastrointestinal mucosal damage [
2,
3,
4].
Invasive factors including hydrochloric acid, pepsin, smoking and drinking, helicobacter pylori infection, non-steroidal anti-inflammatory drugs, certain dietary habits, and psychological stress can cause gastrointestinal mucosal lesions, which in severe cases can lead to ulcers [
5,
6]. Alcohol consumption worldwide increases as people’s material well-being increases, and the number of alcohol-related gastrointestinal diseases increases year by year [
7]. The damage of ethanol to the gastric and duodenal mucosa is involved in many aspects and complex mechanisms. High concentrations of ethanol into the digestive tract can increase vascular permeability, edema formation, and epithelial cell loss, leading to significant gastrointestinal mucosal damage [
8,
9]. It has been demonstrated that ethanol can damage the gastrointestinal mucosa by promoting gastric acid secretion, inducing oxidative stress, activating inflammatory pathways, and affecting normal mucosal microcirculation and cell apoptosis [
10,
11]. Clinical use of synthetic drugs such as proton-pump inhibitor and receptor antagonist in the treatment of gastroduodenal diseases, but long-term use can cause side effects such as poor healing of the stomach and recurrence of ulcers and adverse effects [
12,
13,
14].
There is growing evidence that bioactive peptides have a wide range of physiological activities and play an essential role in improving human health [
15]. Natural bioactive peptides with multiple biological mechanisms play a vital role in preventing and treating gastric and peptic ulcer diseases. For example, a collagen peptide derived from the skin of Cod (Gadus macrocephalus) has a significant protective effect against acetic acid-induced gastric ulcers [
16]. Fish provides a rich source of collagen with high nutritional quality and is an ideal source for the preparation of collagen peptides [
17,
18]. Many studies have shown that bioactive peptides derived from Tilapia have various unique physiological functions, such as antioxidation, anti-aging, lowering blood pressure, immune regulation, antibacterial activity, and the ability to repair tissue defects [
19,
20,
21,
22]. Furthermore, tilapia collagen oligopeptides (TCOPs) extracted from tilapia have lower molecular weight, better digestibility and absorption [
19,
23], and great value in the prevention and treatment of gastroduodenal injury. Whey protein is a recognized high-quality protein, which contains all 20 amino acids that make up proteins. It is mainly composed of β-lactoglobulin, α-whey protein, and immunoglobulin, as well as other protein components. It has multifarious health benefits, such as boosting immunity, inhibiting cancer cell formation, and reducing intestinal strain [
24]. The whey protein group was used as a positive control to eliminate the false-positive results caused by extra protein intake.
This study investigated the possible protective effects of TCOPs on ethanol-induced gastroduodenal mucosa injury in rats and explored its potential mechanism by biomolecular assay.
2. Materials and Methods
2.1. Preparation of TCOPs
Tilapia collagen oligopeptides: solid white powder, provided by Shengmeinuo Biotechnology Co., Ltd. (Hainan, China), mainly composed of oligopeptides with molecular weight less than 1000; the specific molecular weight distribution was <180 Da (9.97%), 180~500 Da (56.06%), 500~1000 Da (26.67%), which was a mixture of small molecular active peptides obtained from tilapia scales by enzymolysis technology. The detailed amino acid composition of the sample is shown in
Table 1.
2.2. Animals
Seventy-two healthy SPF male SD rats aged from 6 to 8 weeks. Provided by the Peking University Health Science Center. Reared in the SPF animal house, with a temperature range of 22 ± 2 °C, relative humidity of 50%~60%, and time between day and night of 12 h: 12 h. The animals ate freely during the experiment. Laboratory animal production license number: SCXK (Beijing) 2016-0010, Laboratory animal use license number: SYXK (Beijing) 2016-0041. The animal feeding management and the experimental operation followed the experimental animal ethics and the regulations of the Beijing Municipality on the administration of experimental animals.
2.3. Ethanol-Induced Gastric and Duodenal Mucosa Injury Model
Rats were randomly divided into six groups according to body weight: normal control group, ethanol group, whey protein control group (250 mg/kg BW), and collagen oligopeptide low, medium, and high dose group (250, 500, 1000 mg/kg BW, respectively referred to as TCOPs-L, TCOPs-M, TCOPs-H). The subjects were given daily by gavage, the normal control group and ethanol group were given distilled water, the whey protein group and collagen peptide group were given corresponding concentrations of the subjects. After the 30th day of administration, all experimental animals were strictly forbidden to eat (without water) for 24 h, during which the subjects were also forbidden to be given. The next day, after 1 h of intragastric administration of each dose group, except the normal control group, the other groups were given anhydrous ethanol (5 mL/kg) by intragastric gavage and anesthetized with pentobarbital 1 h later, and the rats were euthanized. Subsequently, gastroduodenal injury assessment and related biochemical indexes were determined.
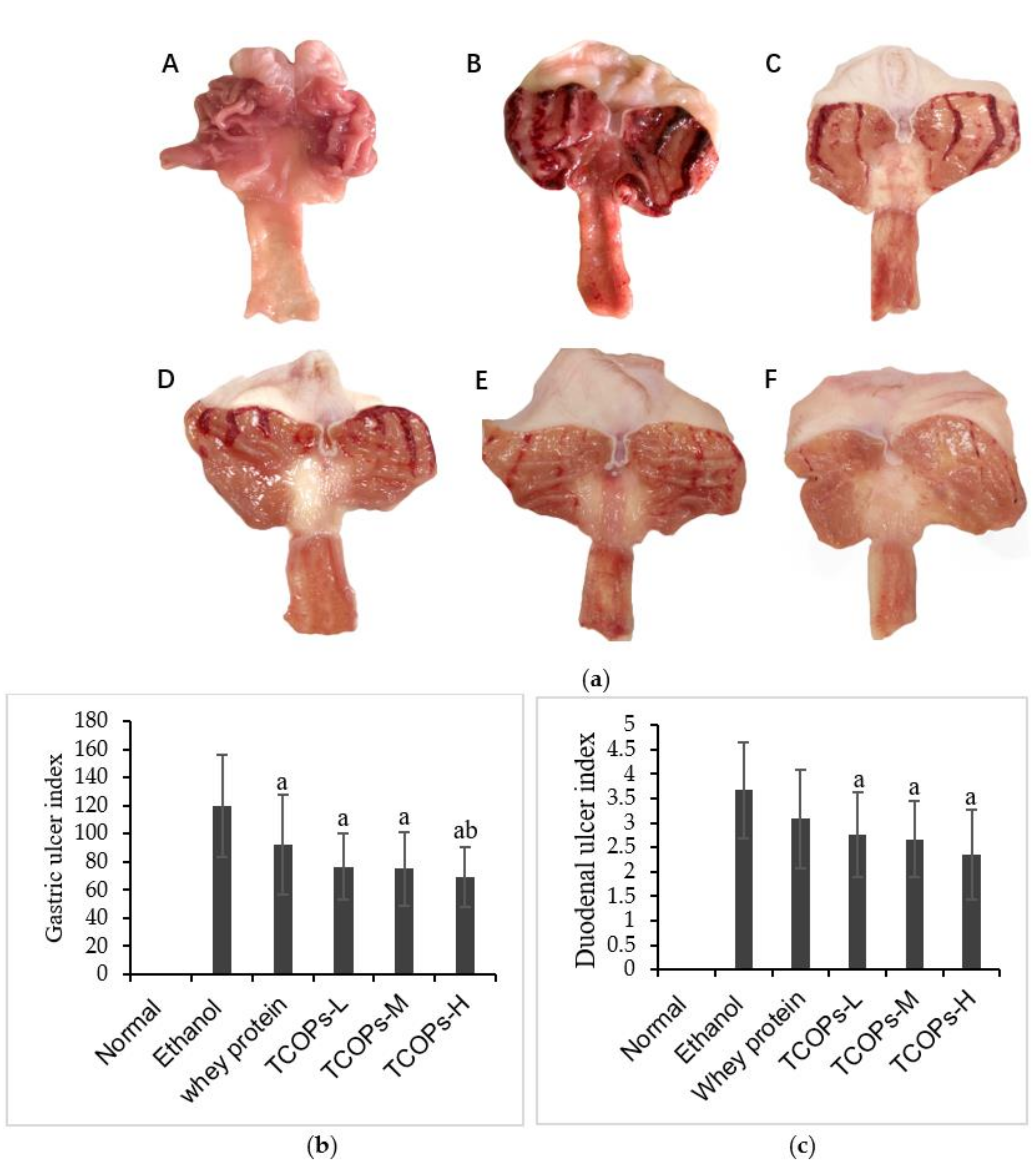
2.4. Macroscopic Observation and Evaluation of Gastric and Duodenal Mucosa Injury
The whole stomach was cut along the greater curvature of the stomach, the duodenum was cut along the mesentery, and the contents were rinsed with cold physiological saline. The gastric and duodenal tissues were flattened with the surface facing upwards to evaluate the injury of the gastroduodenal mucosa. The gastric ulcer index was calculated by Guth’s improved method [
25,
26]. As shown in
Table 2.
On the mucosal side of the duodenum, the degree of peptic ulcer was evaluated as follows [
27]: 0: no lesion; 1: ulcer area with the longest diameter <2 mm; 2: the longest diameter is 2~5 mm; 3: the longest diameter is 6~8 mm; 4: the longest diameter >9 mm, 5: ulcer perforation.
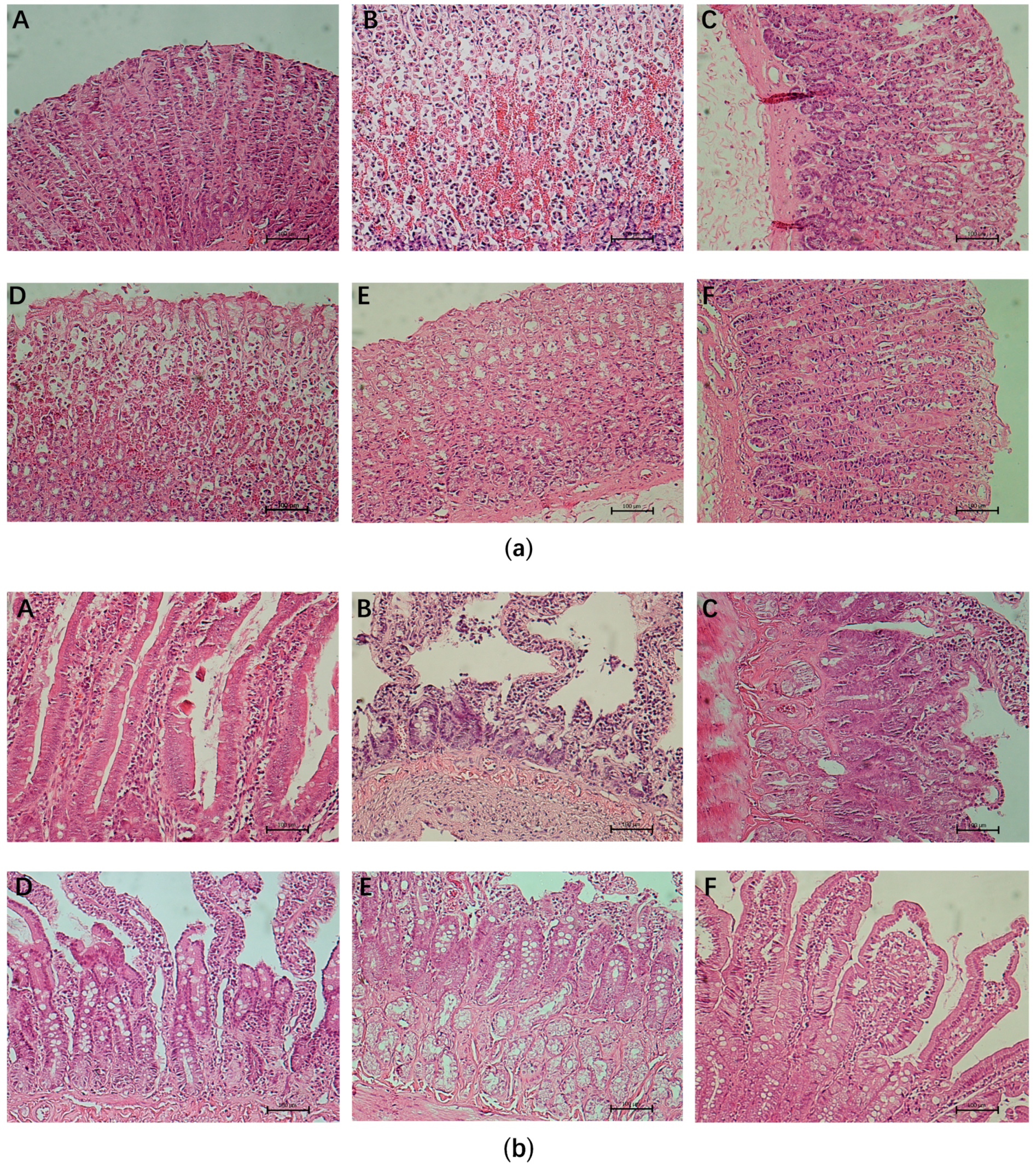
2.5. Histopathological Analysis
After macroscopic observation, the gastric and duodenal tissues were immersed in 10% formalin solution for 24 h, then dehydrated in 95% ethanol. The tissues were embedded in paraffin wax, cut into 5 μm thickness, and stained with hematoxylin and eosin (H&E). The pathological observation and evaluation of the whole layer of gastrointestinal mucosa were performed by fluorescence microscope (E400; Nikon, Tokyo, Japan).
2.6. Measurement of Gastric Juice
Gastric juice and contents were collected in a test tube. The supernatant was then centrifuged at a speed of 3000 rpm for 10 min. The volume of the supernatant was measured accurately with a 10 mL cylinder, and the pH value of gastric juice was measured with a micro-pH meter.
2.7. Enzyme-Linked Immunoabsorbent Assay
Fresh gastroduodenal tissue was taken, and the inflammatory factors (IL-1β, TNF-α, IL-10, MPO) levels and oxidative stress biomarkers (SOD, GSH-Px, CAT, MDA), and the PGE2 and NO contents in gastric and duodenal tissues in different dose groups were determined by ELISA according to the instructions of the kit (Nanjing Jian Cheng Bioengineering Institute, Nanjing, China). Blood was taken from the femoral artery of rats, the blood sample was kept at 4 °C, and then the supernatant was extracted by centrifugation at the speed of 3500 r/min for 10 min. The PG1, PG2 levels, and serum gastrin in rats were detected according to the instructions of the test kit.
2.8. Western Blot
Two hundred microliters of protein lysates was added to every 10 mg tissue and ground to homogenate for complete cleavage. The protein was extracted at 4 °C and centrifuged for 10 min at 12,000 rpm. The concentration of protein was determined according to the operating instructions of the BCA protein quantitative reagent kit (Sigma, St. Louis, MO, USA). The 20 ug sample was subjected to electrophoresis on a sodium lauryl sulfate-polyacrylamide gel. After electrophoresis, the separated proteins were transferred to a polyvinylidene fluoride membrane (Millipore, Billerica, MA, USA). The membrane was immersed in 5% skimmed milk powder prepared with TBST and sealed for 4 h, followed by incubation with primary antibodies against Bcl-2 (ab194583; Abcam, Cambridge, UK) at 1:1000 (loading control), Bax (ab32503; Abcam, Cambridge, UK) at 1:5000, Caspase-3 (#9662; CST, Danvers, MA, USA) at 1:1000, and β-actin at 1:2000 (ab8227; Abcam, Cambridge, UK) overnight at 4 °C, Then, a blocking solution was used to dilute HRP-labeled secondary antibodies, the membranes were incubated with secondary antibody goat anti-rabbit IgG (1:10,000) at room temperature for 4 h, and the HRP was incubated with the membrane for 4 h after the membrane was diluted with the sealing solution. Visual detection using ECL chemiluminescence developer (Millipore, Billerica, MA, USA). Finally, Image-Pro Plus (IPP) software (Media Cybernetics, Rockville, MD, USA) was used for quantification and processing.
2.9. Statistical Analysis
The data were expressed as ± standard deviation (). Using IBM SPSS 24.0 software (IBM, Armonk, NY, USA) for one-way analysis of variance, the variance homogeneity test was conducted for those with significant differences. The variance homogeneity test was conducted for those with the LSD method to analyze the differences between the average values of each experimental group and the control group. If the variance was not up to the standard, we used the rank-sum test to do the statistical analysis. The difference was significant with p < 0.05.
4. Discussion
As an example of gastroduodenal mucosal injury, peptic ulcer is a disease causing increased morbidity and mortality among humans worldwide. It is a heterogeneous disease with multiple etiologies, and it has been shown that heavy drinking is associated with gastrointestinal disorders. The primary pharmacological treatment of the disease is anti-gastric acid secretion drugs, but long-term use of these drugs treatment can have a variety of side effects [
12,
28]. Finding new therapies that produce minimal side effects or no side effects is the focus of medical research to prevent gastrointestinal injury effectively. Peptides are structural and functional fragments of proteins. Small molecule oligopeptides are generally composed of less than 10 amino acids. Compared with proteins, small molecular peptides are characterized by low molecular weight, high absorbability, high bioavailability, and low sensitization and exist in proteins as important bioactive components. In addition, amino acids, like a small pearl, are very limited in function and are easily saturated with absorption. If they are linked into a peptide chain, they will have their own special biological activity. Presently, a variety of natural active ingredients are widely used in research to prevent gastrointestinal diseases [
29,
30,
31,
32]. Collagen peptides derived from marine fish have great potential in preventing and treating gastroduodenal diseases due to their excellent antioxidant [
33,
34], cytogenetic, and tissue repair abilities [
35].
In this study, we investigated the protective effects of TCOPs on ethanol-induced gastroduodenal injury in rats. Among the destructive factors, ethanol is a significant external factor. Ethanol has both hydrophobic alkyl groups and hydrophilic hydroxyl groups in its molecular structure, which can destroy the barrier defense system of gastric mucosa and weaken the ability of gastric mucosa to defend against the invasion of gastric acid, bile, and many digestive enzymes. It plays a role in the destruction of gastric and duodenal mucosal cells [
36]. The animal model of ethanol-induced gastrointestinal injury has been widely used as an experimental model to study the pathophysiological mechanism of gastrointestinal mucosal injury [
37,
38]. We refer to previous studies combined with pre-experiments. It was found that 5 mL/kg of anhydrous ethanol could cause significant damage to the gastroduodenal mucosa without causing death in rats. Therefore, an acute gastroduodenal injury model was established with this dose [
26,
39].
In this study, compared with the normal control group, the ethanol group of rats’ gastroduodenal mucosa damage significantly severe, the injury rate was 100%, and injury index significantly increased. It resulted in visible bleeding, edema, and erosion of the gastroduodenal tissue. When rats were pretreated with TCOPs, the gastroduodenal hemorrhage induced by ethanol was significantly reduced, and the pathological changes of gastroduodenal mucosa were improved considerably, especially in the high-dose group. These results demonstrate that TCOPs have beneficial effects on ethanol-induced gastric and duodenal lesions.
The involvement of acute alcohol-induced oxidative stress in the pathogenesis of gastrointestinal mucosal injury has been demonstrated by many studies [
40]. Ethanol can induce oxidative stress through various pathways, including the production of reactive oxygen species; oxidative stress plays a vital role in the development of gastric diseases such as gastric adenocarcinoma, peptic ulcer, or gastritis [
41]. In this regard, the gastrointestinal mucosa, through a series of endogenous antioxidant defense systems, resists the invasion of harmful substances. Nonenzymatic and enzymatic antioxidants have antioxidant defenses, and ethanol inhibits the activities of these enzymes in the gastrointestinal mucosa, leading to the accumulation of hydrogen peroxide and lipid oxidation, which ultimately leads to the loss of membrane integrity [
42]. SOD and CAT are major antioxidant enzymes, and the levels of SOD and CAT are essential indicators of the ability to scavenge free radicals. Furthermore, GSH-Px is one of the crucial antioxidant enzymes. Its primary physiological function is to clear the body of free radicals. Ethanol-induced gastrointestinal injury is often accompanied by a significant decrease in GSH-Px level, mainly due to the oxidation of GSH-Px after the formation of ethanol-induced superoxides or the combination of acetaldehyde and GSH-Px from the oxidation of alcohol [
43]. Lipid peroxidation is thought to be a significant factor in the development of alcohol-induced oxidative damage to the gastrointestinal mucosa, and MDA is a considerable indicator of lipid peroxidation. The activities of SOD, CAT, and GSH-Px in the ethanol group were significantly decreased, and the MDA contents were significantly increased, which indicated that oxidative stress and lipid peroxidation reaction occurred in the gastric and duodenal tissues of rats. The activities of SOD, CAT, and GSH-Px in gastroduodenal tissues were significantly increased, and MDA levels were significantly decreased in TCOPs groups. The results showed that pretreatment with TCOPs significantly enhanced the activity of antioxidant enzymes and inhibited the activity of lipid peroxidation. It can effectively relieve acute ethanol-induced oxidative stress in gastroduodenal mucosa.
Inflammation is a momentous pathogenesis of gastrointestinal injury. When the gastrointestinal tract is stimulated by alcohol, the inflammatory cells overreact and produce many inflammatory factors [
44,
45]. TNF-α and IL-1β are crucial inflammatory cytokines. External stimuli may stimulate the innate immune system, leading to the release of inflammatory cytokines such as TNF-α and IL-1β, enhancing cell apoptosis and neutrophil migration by promoting oxygen free radicals and the caspase cascade pathway and eventually lead to severe gastrointestinal mucosal damage [
46]. MPO is a marker of neutrophil infiltration, which indicates the degree of inflammation. This is because the inflammatory tissues are heavily infiltrated by neutrophils, which contain MPO, which is involved in the development of inflammation [
47]. IL-10 plays an important role in down-regulating the inflammatory cascade by enhancing anti-inflammatory cytokines and slowing down the production of pro-inflammatory cytokines and preventing autoimmune diseases. The expression of TNF-α, IL-1β, and MPO may be increased after gastrointestinal mucosa injury [
48]. In this study, the levels of TNF-α, IL-1β, and MPO were significantly increased, and the levels of Il-10 were decreased considerably in the gastric and duodenal tissues of the ethanol group after ethanol stimulation of the gastroduodenal mucosa leading to injury and inflammation. However, the intervention of TCOPs significantly reduced the levels of inflammatory factors in rat gastroduodenal tissues, ameliorated the infiltration of inflammatory cells, reduced the inflammatory response, and showed a good anti-inflammatory effect to inhibit the injury in gastroduodenal. Furthermore, alcohol may increase the expression of H
+-K
+-ATP on the cell membrane. Ethanol can stimulate parietal cells to overproduce gastric acid, thus reducing the pH value of gastric juice and increasing gastric juice volume [
49]. The results showed that the gastric juice secretion of rats pretreated by TCOPs decreased significantly. The pH value of gastric juice increased to different degrees, significantly different from that of the ethanol group. This result is consistent with the previous study [
50]. These results suggest that TCOPs can reduce gastric acid invasion on gastric and duodenal mucosa by affecting gastric juice secretion and have a good protective effect on the gastric and duodenal tissue.
Pepsinogen is an inactive precursor of pepsin secreted by the principal cells of the gastric mucosa. They are classified as PGI and PGII in biochemistry and immunochemistry and are converted to active pepsin by the action of gastric acid or activated pepsin, PGI, and PGII, and the ratio of PGI to PGII (PGR) levels reflect the functional and morphological status of the gastric mucosa [
51]. Pepsinogen is more sensitive to damage to the gastric mucosa, and in general, when PGI and PGII are higher than normal, the risk of gastric mucosa injury is higher [
52]. The decrease in PGR is currently used to detect atrophic gastritis [
53]. In this study, the ethanol group had significantly higher pepsinogen levels than the normal control group, and the pepsinogen levels were significantly decreased after intervention with TCOPs, suggesting that TCOPs can protect gastroduodenal mucosa by reducing the pepsinogen levels. GAS can stimulate gastric acid secretion. Excessive gastric acid secretion can lead to gastric mucosal permeability changes and accelerate the formation of ulcers. In this study, GAS levels increased significantly in the ethanol group. Still, GAS levels decreased significantly in all dose groups of TCOPs, indicating that TCOPs can protect gastrointestinal mucosa by decreasing GAS levels.
A variety of PGs help maintain mucosal integrity, a phenomenon known as “gastric cell protection”. PGE2 promotes the flow of gastric mucosal microcirculation, stimulates the secretion of hydrogen carbonate, mediates adaptive immune protection, increases protein synthesis and cell regeneration, and enhances the resistance of gastric mucosal cells to strong stimuli [
54,
55], and ultimately enhances the ability to repair damaged gastrointestinal mucosa [
56]. NO and PGE2 are known as vasodilators, which can inhibit platelet aggregation and thrombosis and accelerate the flow of gastrointestinal mucosal microcirculation. NO is thought to act with PGE2 on the regulation of gastric mucosal integrity and acidity and participate in the inhibition of neutrophil aggregation and the increase of blood flow. The results showed that the levels of PGE2 and NO in the ethanol group were significantly lower than those in the normal control group, suggesting that ethanol inhibits the synthesis and secretion of endogenous NO and PGE2 and participates in the damage of the gastroduodenal tissue. However, TCOPs can increase the levels of PGE2 and NO in acute alcohol-induced gastroduodenal injury and play an important role in maintaining gastroduodenal microcirculation and reducing gastroduodenal injury.
Previous studies have shown that ethanol-induced gastrointestinal injury is closely associated with apoptosis, which breaks down the gastrointestinal mucosal barrier and eventually leads to peptic ulcers [
57]. Oxidative stress in the ulcer region can initiate the intrinsic pathway of apoptosis and activate pro-apoptotic protein Bax. The translocation of activated Bax to mitochondria stimulated the formation of apoptotic bodies and finally activated the executor of apoptosis, Caspase-3 [
58]. Anti-apoptotic members of the Bcl-2 family block the release of Cytochrome C, and Bcl-2 binds to pro-apoptotic proteins or interacts directly with Bax to prevent mitochondrial pore formation [
59]. In this study, compared with the normal control group, the expression of Bax and Caspase-3 was significantly increased. The expression of Bcl-2 was decreased in the gastric, duodenal tissues of the ethanol group, suggesting that ethanol-induced gastroduodenal injury was related to the mechanism of apoptosis. Compared with the ethanol group, pretreatment with TCOPs significantly decreased the expression of Bax protein and increased the expression of Bcl-2 protein, indicating that TCOPs reduced ethanol-induced mitochondrial apoptosis. In addition, pretreatment with TCOPs reduced the expression of caspase-3 in rat gastric, duodenal tissues. Among them, the high dose of TCOPs had the best regulatory effect on anti-apoptotic protein Bcl-2 and pro-apoptotic protein Bax and caspase-3. Therefore, this study suggests that the protective effect of tilapia collagen oligopeptide on ethanol-induced gastroduodenal injury may be related to the reduction of apoptosis.