Association between Reduced Serum Zinc and Diastolic Dysfunction in Maintenance Hemodialysis Patients
Abstract
:1. Introduction
2. Materials and Methods
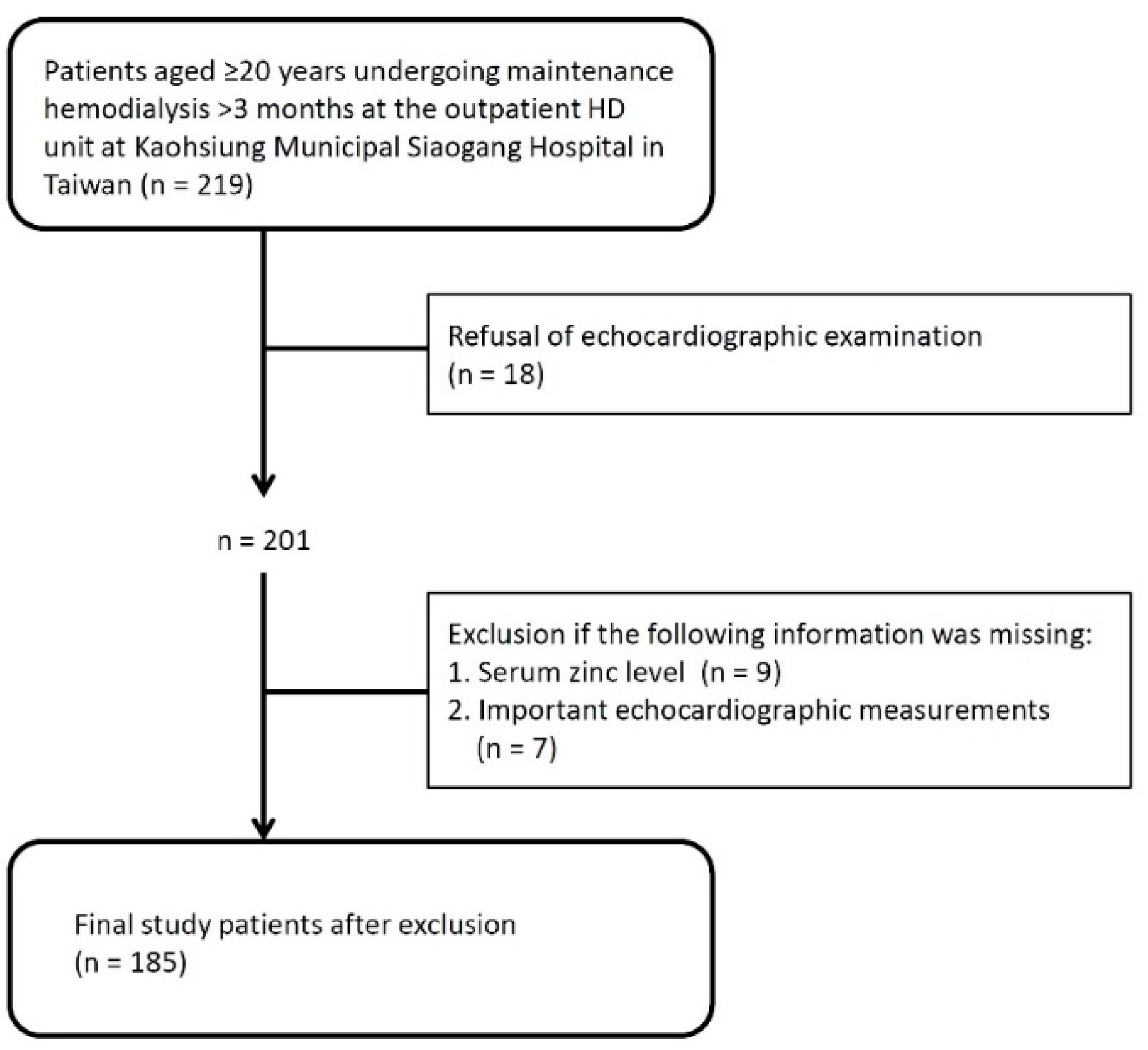
2.1. Study Participants
2.2. Demographic, Medical and Biochemical Information
2.3. Measurement of Serum Zinc Levels
2.4. Echocardiographic Measurements
2.5. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bikbov, B.; A Purcell, C.; Levey, A.S.; Smith, M.; Abdoli, A.; Abebe, M.; Adebayo, O.M.; Afarideh, M.; Agarwal, S.K.; Agudelo-Botero, M.; et al. Global, regional, and national burden of chronic kidney disease, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2020, 395, 709–733. [Google Scholar] [CrossRef] [Green Version]
- Romagnani, P.; Remuzzi, G.; Glassock, R.; Levin, A.; Jager, K.J.; Tonelli, M.; Massy, Z.; Wanner, C.; Anders, H.-J. Chronic kidney disease. Nat. Rev. Dis. Primers. 2017, 3, 17088. [Google Scholar] [CrossRef] [PubMed]
- Webster, A.C.; Nagler, E.V.; Morton, R.L.; Masson, P. Chronic Kidney Disease. Lancet 2017, 389, 1238–1252. [Google Scholar] [CrossRef]
- Liyanage, T.; Ninomiya, T.; Jha, V.; Neal, B.; Patrice, H.M.; Okpechi, I.; Zhao, M.-H.; Lv, J.; Garg, A.X.; Knight, J.; et al. Worldwide access to treatment for end-stage kidney disease: A systematic review. Lancet 2015, 385, 1975–1982. [Google Scholar] [CrossRef]
- House, A.A.; Wanner, C.; Sarnak, M.J.; Piña, I.L.; McIntyre, C.W.; Komenda, P.; Kasiske, B.L.; Deswal, A.; Defilippi, C.R.; Cleland, J.G.F.; et al. Heart failure in chronic kidney disease: Conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference. Kidney Int. 2019, 95, 1304–1317. [Google Scholar] [CrossRef] [Green Version]
- McCullough, P.A.; Roberts, W.C. Influence of Chronic Renal Failure on Cardiac Structure. J. Am. Coll. Cardiol. 2016, 67, 1183–1185. [Google Scholar] [CrossRef]
- Huang, J.-C.; Su, H.-M.; Wu, P.-Y.; Lee, J.-J.; Lee, W.-H.; Chen, S.-C.; Chiu, Y.-W.; Hsu, Y.-L.; Chang, J.-M.; Chen, H.-C. Ratio of Early Mitral Inflow Velocity to the Global Diastolic Strain Rate and Global Left Ventricular Longitudinal Systolic Strain Predict Overall Mortality and Major Adverse Cardiovascular Events in Hemodialysis Patients. Dis. Markers 2019, 2019, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Thomas, L.; Marwick, T.H.; Popescu, B.A.; Donal, E.; Badano, L.P. Left Atrial Structure and Function, and Left Ventricular Diastolic Dysfunction: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2019, 73, 1961–1977. [Google Scholar] [CrossRef]
- Han, J.H.; Han, J.S.; Kim, E.J.; Doh, F.M.; Koo, H.M.; Kim, C.H.; Lee, M.J.; Oh, H.J.; Park, J.T.; Han, S.H.; et al. Diastolic Dysfunction Is an Independent Predictor of Cardiovascular Events in Incident Dialysis Patients with Preserved Systolic Function. PLoS ONE 2015, 10, e0118694. [Google Scholar] [CrossRef] [Green Version]
- Kim, S.J.; Han, S.H.; Park, J.T.; Kim, J.-K.; Oh, H.J.; Yoo, D.E.; Yoo, T.-H.; Kang, S.-W.; Choi, K.H. Left atrial volume is an independent predictor of mortality in CAPD patients. Nephrol. Dial. Transplant. 2011, 26, 3732–3739. [Google Scholar] [CrossRef] [Green Version]
- Prasad, A.S. Lessons Learned from Experimental Human Model of Zinc Deficiency. J. Immunol. Res. 2020, 2020, 9207279. [Google Scholar] [CrossRef]
- Roohani, N.; Hurrell, R.; Kelishadi, R.; Schulin, R. Zinc and its importance for human health: An integrative review. J. Res. Med. Sci. 2013, 18, 144–157. [Google Scholar]
- Olechnowicz, J.; Tinkov, A.; Skalny, A.; Suliburska, J. Zinc status is associated with inflammation, oxidative stress, lipid, and glucose metabolism. J. Physiol. Sci. 2018, 68, 19–31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dvornik, S.; Cuk, M.; Racki, S.; Zaputović, L. Serum zinc concentrations in the maintenance hemodialysis patients. Coll. Antropol. 2006, 30, 125–129. [Google Scholar] [PubMed]
- Lee, S.H.; Huang, J.-W.; Hung, K.Y.; Leu, L.J.; Kan, Y.T.; Yang, C.S.; Chung Wu, D.; Huang, C.L.; Chen, P.Y.; Chen, J.S.; et al. Trace Metals’ Abnormalities in Hemodialysis Patients: Relationship with Medications. Artif. Organs 2000, 24, 841–844. [Google Scholar] [CrossRef] [PubMed]
- Escoli, R.; Carvalho, M.J.; Cabrita, A.; Rodrigues, A. Diastolic Dysfunction, an Underestimated New Challenge in Dialysis. Ther. Apher. Dial. 2019, 23, 108–117. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gonçalves, A.F.; Polegato, B.F.; Fernandes, A.A.; Ishikawa, L.L.; Okoshi, K.; Bazan, S.G.Z.; Minicucci, M.F.; Azevedo, P.S.; Ikoma, M.R.; Penitenti, M.; et al. Zinc Supplementation Attenuates Cardiac Remodeling After Experimental Myocardial Infarction. Cell. Physiol. Biochem. 2018, 50, 353–362. [Google Scholar] [CrossRef]
- Brugger, D.; Windisch, W.M. Short-Term Subclinical Zinc Deficiency in Weaned Piglets Affects Cardiac Redox Metabolism and Zinc Concentration. J. Nutr. 2017, 147, 521–527. [Google Scholar] [CrossRef] [Green Version]
- Yu, X.; Huang, L.; Zhao, J.; Wang, Z.; Yao, W.; Wu, X.; Huang, J.; Bian, B. The Relationship between Serum Zinc Level and Heart Failure: A Meta-Analysis. Biomed. Res. Int. 2018, 2018, 2739014. [Google Scholar] [CrossRef]
- La’Ulu, S.L.; Roberts, W.L. Performance Characteristics of Six Intact Parathyroid Hormone Assays. Am. J. Clin. Pathol. 2010, 134, 930–938. [Google Scholar] [CrossRef]
- Daugirdas, J.T. Second generation logarithmic estimates of single-pool variable volume Kt/V: An analysis of error. J. Am. Soc. Nephrol. 1993, 4, 1205–1213. [Google Scholar] [CrossRef] [PubMed]
- Lang, R.M.; Badano, L.P.; Mor-Avi, V.; Afilalo, J.; Armstrong, A.; Ernande, L.; Flachskampf, F.A.; Foster, E.; Goldstein, S.A.; Kuznetsova, T.; et al. Recommendations for Cardiac Chamber Quantification by Echocardiography in Adults: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J. Am. Soc. Echocardiogr. 2015, 28, 1–39.e14. [Google Scholar] [CrossRef] [Green Version]
- Mitter, S.S.; Shah, S.J.; Thomas, J.D. A Test in Context: E/A and E/e′ to Assess Diastolic Dysfunction and LV Filling Pressure. J. Am. Coll. Cardiol. 2017, 69, 1451–1464. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.-C.; Tsai, Y.-C.; Wu, P.-Y.; Lee, J.-J.; Chen, S.-C.; Chiu, Y.-W.; Hsu, Y.-L.; Chang, J.-M.; Chen, H.-C. Independent Association of Overhydration with All-Cause and Cardiovascular Mortality Adjusted for Global Left Ventricular Longitudinal Systolic Strain and E/E’ Ratio in Maintenance Hemodialysis Patients. Kidney Blood Press. Res. 2018, 43, 1322–1332. [Google Scholar] [CrossRef] [PubMed]
- Shizuku, J.; Yamashita, T.; Ohba, T.; Kabaya, T.; Nitta, K. Left Atrial Volume Is an Independent Predictor of All-Cause Mortality in Chronic Hemodialysis Patients. Intern. Med. 2012, 51, 1479–1485. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ogawa, T.; Nitta, K. Clinical Impact of Left Ventricular Diastolic Dysfunction in Chronic Kidney Disease. Contrib. Nephrol. 2018, 195, 81–91. [Google Scholar] [CrossRef]
- Shokrzadeh, M.; Ghaemian, A.; Salehifar, E.; Aliakbari, S.; Saravi, S.S.; Ebrahimi, P. Serum Zinc and Copper Levels in Ischemic Cardiomyopathy. Biol. Trace Elem. Res. 2009, 127, 116–123. [Google Scholar] [CrossRef]
- Salehifar, E.; Shokrzadeh, M.; Ghaemian, A.; Aliakbari, S.; Saravi, S.S.S. The Study of Cu and Zn Serum Levels in Idiopathic Dilated Cardiomyopathy (IDCMP) Patients and its Comparison with Healthy Volunteers. Biol. Trace Elem. Res. 2008, 125, 97–108. [Google Scholar] [CrossRef] [PubMed]
- Alexanian, I.; Parissis, J.; Farmakis, D.; Athanaselis, S.; Pappas, L.; Gavrielatos, G.; Mihas, C.; Paraskevaidis, I.; Sideris, A.; Kremastinos, D.; et al. Clinical and echocardiographic correlates of serum copper and zinc in acute and chronic heart failure. Clin. Res. Cardiol. 2014, 103, 938–949. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.; Teng, T.; Bian, B.; Yao, W.; Yu, X.; Wang, Z.; Xu, Z.; Sun, Y. Zinc Levels in Left Ventricular Hypertrophy. Biol. Trace Elem. Res. 2017, 176, 48–55. [Google Scholar] [CrossRef] [PubMed]
- Jankowski, J.; Floege, J.; Fliser, D.; Böhm, M.; Marx, N. Cardiovascular Disease in Chronic Kidney Disease: Pathophysiological Insights and Therapeutic Options. Circulation 2021, 143, 1157–1172. [Google Scholar] [CrossRef] [PubMed]
- Tuegel, C.; Bansal, N. Heart failure in patients with kidney disease. Heart 2017, 103, 1848–1853. [Google Scholar] [CrossRef] [PubMed]
- Toida, T.; Toida, R.; Ebihara, S.; Takahashi, R.; Komatsu, H.; Uezono, S.; Sato, Y.; Fujimoto, S. Association between Serum Zinc Levels and Clinical Index or the Body Composition in Incident Hemodialysis Patients. Nutrients 2020, 12, 3187. [Google Scholar] [CrossRef] [PubMed]
- Dawson, J.; Brennan, F.P.; Hoffman, A.; Josland, E.; Li, K.C.; Smyth, A.; Brown, M.A. Prevalence of Taste Changes and Association with Other Nutrition-Related Symptoms in End-Stage Kidney Disease Patients. J. Ren. Nutr. 2021, 31, 80–84. [Google Scholar] [CrossRef]
- Liu, Y.; Zheng, Y.; Wang, L.; Zhong, X.; Qin, D.; Chen, W.; Tan, R.; Liu, Y. Lower Levels of Blood Zinc Associated with Intradialytic Hypertension in Maintenance Hemodialysis Patients. Biol. Trace Elem. Res. 2020, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Kunutsor, S.K.; Laukkanen, J.A. Serum zinc concentrations and incident hypertension: New findings from a population-based cohort study. J. Hypertens. 2016, 34, 1055–1061. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zalewski, P.D.; Beltrame, J.F.; Wawer, A.A.; Abdo, A.I.; Murgia, C. Roles for endothelial zinc homeostasis in vascular physiology and coronary artery disease. Crit. Rev. Food Sci. Nutr. 2019, 59, 3511–3525. [Google Scholar] [CrossRef]
- Efeovbokhan, N.; Bhattacharya, S.K.; Ahokas, R.A.; Sun, Y.; Guntaka, R.V.; Gerling, I.C.; Weber, K.T. Zinc and the Prooxidant Heart Failure Phenotype. J. Cardiovasc. Pharmacol. 2014, 64, 393–400. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jeejeebhoy, F.; Keith, M.; Freeman, M.; Barr, A.; McCall, M.; Kurian, R.; Mazer, D.; Errett, L. Nutritional supplementation with MyoVive repletes essential cardiac myocyte nutrients and reduces left ventricular size in patients with left ventricular dysfunction. Am. Heart J. 2002, 143, 1092–1100. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | 1st Tertile of Serum Zinc (<98.4 μg/dL) (n = 62) | 2nd Tertile of Serum Zinc (98.4–111.2 μg/dL) (n = 62) | 3rd Tertile of Serum Zinc (>111.2 μg/dL) (n = 61) | p-Value |
|---|---|---|---|---|
| Age (year) | 62.9 ± 12.2 | 60.9 ± 10.2 | 58.9 ± 12.7 | 0.184 |
| Men (%) | 43.5 | 51.6 | 57.4 | 0.305 |
| Dialysis vintage (year) | 6.5 (1.4–12.4) | 6.1 (2.6–10.7) | 8.8 (3.7–11.9) | 0.232 |
| Diabetes mellitus (%) | 48.4 | 50.0 | 39.3 | 0.443 |
| Coronary artery disease (%) | 19.4 | 9.7 | 14.8 | 0.312 |
| Congestive heart failure (%) | 33.9 | 22.6 | 19.7 | 0.160 |
| Stroke (%) | 12.9 | 9.7 | 6.6 | 0.494 |
| Current smoking (%) | 9.7 | 14.5 | 16.4 | 0.531 |
| Body mass index (kg/m2) | 23.4 ± 3.6 | 23.5 ± 3.2 | 23.8 ± 4.2 | 0.808 |
| Systolic BP (mmHg) | 148.8 ± 24.5 | 162.8 ± 28.6 * | 156.1 ± 28.8 | 0.030 |
| Diastolic BP (mmHg) | 77.9 ± 15.3 | 86.5 ± 14.0 * | 81.2 ± 17.2 | 0.016 |
| Laboratory parameters | ||||
| Albumin (g/dL) | 3.75 ± 0.29 | 3.85 ± 0.36 | 3.94 ± 0.29 * | 0.005 |
| Hemoglobin (g/dL) | 10.4 ± 1.1 | 10.4 ± 1.3 | 10.7 ± 1.3 | 0.270 |
| Total cholesterol (mg/dL) | 177.3 ± 40.6 | 180.0 ± 44.8 | 178.9 ± 35.5 | 0.897 |
| HDL-C (mg/dL) | 41.8 ± 12.1 | 40.5 ± 12.7 | 42.1 ± 12.1 | 0.748 |
| LDL-C (mg/dL) | 83.8 ± 29.3 | 89.4 ± 30.8 | 83.1 ± 24.8 | 0.406 |
| Triglycerides (mg/dL) | 123.5 (90.5–206) | 147.5(79.8–206.8) | 117.0 (83.5–233.5) | 0.674 |
| Total calcium (mg/dL) | 9.2 ± 1.1 | 9.3 ± 1.1 | 9.2 ± 0.9 | 0.607 |
| Phosphorous (mg/dL) | 4.6 ± 1.4 | 4.4 ± 0.9 | 4.5 ± 1.1 | 0.508 |
| Potassium (mmol/L) | 4.6 ± 0.8 | 4.7 ± 0.7 | 4.6 ± 0.7 | 0.836 |
| iPTH (pg/mL) | 442 (226–733) | 342 (151–559) | 335 (164–552) | 0.123 |
| hs-CRP (mg/L) | 3.2 (1.4–7.0) | 1.7 (0.8–4.6) | 2.2 (1.0–8.6) | 0.773 |
| spKt/V | 1.6 ± 0.3 | 1.6 ± 0.3 | 1.6 ± 0.3 | 0.778 |
| Zinc (μg/dL) | 89.4 ± 6.7 | 104.8 ± 3.5 * | 122.5 ± 9.2 *,† | <0.001 |
| Echocardiographic parameters | ||||
| LVEF (%) | 65.7 ± 9.8 | 66.0 ± 10.1 | 68.4 ± 9.9 | 0.256 |
| LV mass (g) | 218.7 ± 74.4 | 229.7 ± 82.3 | 221.8 ± 73.0 | 0.712 |
| LVMI (g/m2) | 133.6 ± 38.7 | 140.5 ± 49.1 | 133.3 ± 39.5 | 0.566 |
| Relative wall thickness | 0.42 ± 0.11 | 0.41 ± 0.10 | 0.43 ± 0.10 | 0.576 |
| E (cm/s) | 89.6 ± 37.5 | 81.4 ± 28.4 | 77.4 ± 22.9 | 0.075 |
| e’ (cm/s) | 6.5 ± 2.4 | 6.6 ± 2.4 | 7.0 ± 2.1 | 0.441 |
| EDT (ms) | 179.2 ± 55.8 | 193.4 ± 71.7 | 193.9 ± 57.3 | 0.328 |
| E/e’ ratio | 16.7 ± 1.3 | 14.1 ± 0.8 | 12.3 ± 0.6 * | 0.034 |
| LA diameter (cm) | 3.8 ± 0.6 | 3.5 ± 0.6 | 3.5 ± 0.8 | 0.051 |
| LAVI (mL/m2) | 37.2 ± 12.3 | 32.3 ± 11.5 | 30.8 ± 10.3 * | 0.005 |
| Echocardiographic Parameters | Pearson’s r | p-Value |
|---|---|---|
| LVEF (%) | 0.072 | 0.332 |
| LV mass (g) | −0.005 | 0.945 |
| LVMI (g/m2) | −0.057 | 0.438 |
| Relative wall thickness | 0.082 | 0.269 |
| E (cm/s) | −0.204 | 0.005 |
| e’ (cm/s) | 0.112 | 0.131 |
| EDT (ms) | 0.131 | 0.076 |
| E/e’ ratio | −0.217 | 0.003 |
| LA diameter (cm) | −0.134 | 0.069 |
| LAVI (mL/m2) | −0.197 | 0.007 |
| Covariates | Univariate | Multivariate | ||
|---|---|---|---|---|
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | |
| Age (per 1 year) | 1.056 (1.024–1.089) | 0.001 | 1.038 (1.004–1.074) | 0.029 |
| Sex (male vs. female) | 1.237 (0.658–2.329) | 0.509 | – | – |
| Current smoking | 1.131 (0.457–2.801) | 0.790 | – | – |
| Diabetes mellitus | 3.512 (1.803–6.838) | <0.001 | 2.559 (1.249–5.244) | 0.010 |
| Coronary artery disease | 4.438 (1.900–10.369) | 0.001 | 2.569 (1.012–6.517) | 0.047 |
| Stroke | 2.043 (0.760–5.491) | 0.157 | – | – |
| Dialysis vintage (per 1 year) | 0.979 (0.923–1.039) | 0.482 | – | – |
| Body mass index (per 1 kg/m2) | 0.971 (0.889–1.061) | 0.513 | – | – |
| Systolic BP (per 1 mmHg) | 1.011 (0.998–1.024) | 0.098 | – | – |
| Diastolic BP (per 1 mmHg) | 0.990 (0.968–1.012) | 0.383 | – | – |
| Albumin (per 1 g/dL) | 0.475 (0.179–1.258) | 0.134 | – | – |
| Hemoglobin (per 1 g/dL) | 0.961 (0.744–1.241) | 0.760 | – | – |
| Total cholesterol (per 1 mg/dL) | 0.995 (0.987–1.003) | 0.217 | – | – |
| Triglycerides (per log mg/dL) | 1.296 (0.402–4.172) | 0.664 | – | – |
| HDL-C (per 1 mg/dL) | 0.988 (0.962–1.015) | 0.381 | – | – |
| LDL-C (per 1 mg/dL) | 0.998 (0.987–1.010) | 0.777 | – | – |
| Phosphate (per 1 mg/dL) | 0.947 (0.718–1.250) | 0.701 | – | – |
| Total calcium (per 1 mg/dL) | 1.221 (0.900–1.657) | 0.199 | – | – |
| Potassium (per 1 mmol/L) | 0.888 (0.576–1.369) | 0.591 | – | – |
| iPTH (per log pg/mL) | 1.388 (0.641–3.007) | 0.406 | – | – |
| hs-CRP (per log mg/L) | 1.679 (0.969–2.908) | 0.065 | – | – |
| spKt/V (per 1 unit) | 1.037 (0.356–3.021) | 0.947 | – | – |
| Serum zinc (per 1 μg/dL) | 0.970 (0.948–0.992) | 0.008 | 0.974 (0.950–0.999) | 0.039 |
| Covariates | Univariate | Multivariate | ||
|---|---|---|---|---|
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | |
| Age (per 1 year) | 1.009 (0.984–1.035) | 0.468 | – | – |
| Sex (male vs. female) | 1.366 (0.754–2.473) | 0.303 | – | – |
| Current smoking | 1.538 (0.659–3.590) | 0.319 | – | – |
| Diabetes mellitus | 2.507 (1.367–4.595) | 0.003 | 2.453 (1.312–4.585) | 0.005 |
| Coronary artery disease | 2.215 (0.970–5.057) | 0.059 | – | – |
| Stroke | 1.287 (0.483–3.433) | 0.614 | – | – |
| Dialysis vintage (per 1 year) | 0.960 (0.908–1.016) | 0.158 | – | – |
| Body mass index (per 1 kg/m2) | 1.015 (0.936–1.110) | 0.719 | – | – |
| Systolic BP (per 1 mmHg) | 1.009 (0.998–1.021) | 0.117 | – | – |
| Diastolic BP (per 1 mmHg) | 1.006 (0.986–1.026) | 0.550 | – | – |
| Albumin (per 1 g/dL) | 0.891 (0.355–2.237) | 0.805 | – | – |
| Hemoglobin (per 1 g/dL) | 0.941 (0.740–1.197) | 0.622 | – | – |
| Total cholesterol (per 1 mg/dL) | 0.992 (0.984–1.000) | 0.042 | 0.998 (0.985–1.010) | 0.691 |
| Triglycerides (per log mg/dL) | 0.982 (0.328–2.939) | 0.975 | – | – |
| HDL-C (per 1 mg/dL) | 0.995 (0.971–1.020) | 0.686 | – | – |
| LDL-C (per 1 mg/dL) | 0.986 (0.975–0.997) | 0.015 | 0.988 (0.971–1.006) | 0.196 |
| Phosphate (per 1 mg/dL) | 1.094 (0.845–1.145) | 0.495 | – | – |
| Total calcium (per 1 mg/dL) | 1.083 (0.815–1.439) | 0.585 | – | – |
| Potassium (per 1 mmol/L) | 1.227 (0.822–1.832) | 0.317 | – | – |
| iPTH (per log pg/mL) | 1.185 (0.587–2.392) | 0.636 | – | – |
| hs-CRP (per log mg/L) | 0.875 (0.526–1.456) | 0.608 | – | – |
| spKt/V (per 1 unit) | 0.576 (0.207–1.600) | 0.290 | – | – |
| Serum zinc (per 1 μg/dL) | 0.978 (0.958–0.998) | 0.034 | 0.978 (0.958–0.999) | 0.041 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, J.-C.; Huang, Y.-C.; Wu, P.-Y.; Lee, W.-H.; Tsai, Y.-C.; Chen, Y.-P.; Chen, S.-C.; Su, H.-M.; Chiu, Y.-W.; Chang, J.-M. Association between Reduced Serum Zinc and Diastolic Dysfunction in Maintenance Hemodialysis Patients. Nutrients 2021, 13, 2077. https://doi.org/10.3390/nu13062077
Huang J-C, Huang Y-C, Wu P-Y, Lee W-H, Tsai Y-C, Chen Y-P, Chen S-C, Su H-M, Chiu Y-W, Chang J-M. Association between Reduced Serum Zinc and Diastolic Dysfunction in Maintenance Hemodialysis Patients. Nutrients. 2021; 13(6):2077. https://doi.org/10.3390/nu13062077
Chicago/Turabian StyleHuang, Jiun-Chi, Ya-Chin Huang, Pei-Yu Wu, Wen-Hsien Lee, Yi-Chun Tsai, Yi-Ping Chen, Szu-Chia Chen, Ho-Ming Su, Yi-Wen Chiu, and Jer-Ming Chang. 2021. "Association between Reduced Serum Zinc and Diastolic Dysfunction in Maintenance Hemodialysis Patients" Nutrients 13, no. 6: 2077. https://doi.org/10.3390/nu13062077
APA StyleHuang, J.-C., Huang, Y.-C., Wu, P.-Y., Lee, W.-H., Tsai, Y.-C., Chen, Y.-P., Chen, S.-C., Su, H.-M., Chiu, Y.-W., & Chang, J.-M. (2021). Association between Reduced Serum Zinc and Diastolic Dysfunction in Maintenance Hemodialysis Patients. Nutrients, 13(6), 2077. https://doi.org/10.3390/nu13062077






