Associations of Lifestyle Factors with Osteopenia and Osteoporosis in Polish Patients with Inflammatory Bowel Disease
Abstract
1. Introduction
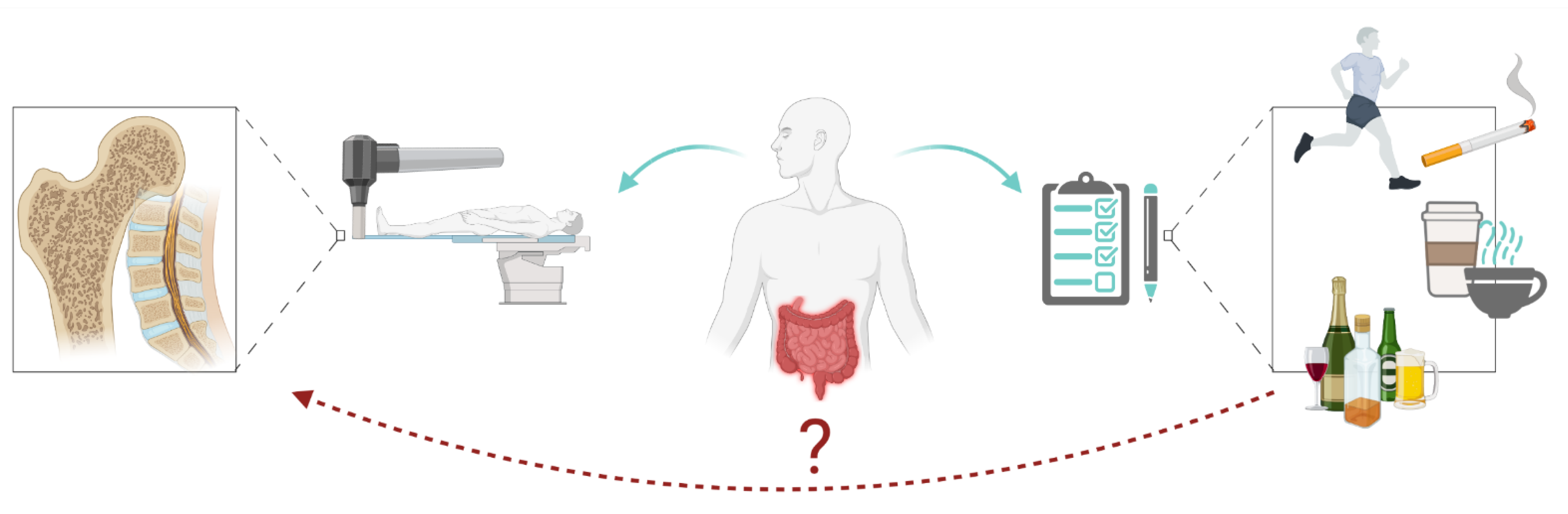
2. The Aim of the Study
3. Patients and Methods
3.1. Densitometry
- Normal: T-score ≥ −1 SD (standard deviation);
- Osteopenia (low bone mass): T-score <−1 SD and >−2.5 SD;
- Osteoporosis: T-score ≤ −2.5 SD;
- Severe osteoporosis: T-score ≤ −2.5 SD with fragility fractures [19].
3.2. Lifestyle Factors
3.3. Data Analysis
4. Results
5. Discussion
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hidalgo, D.F.; Boonpheng, B.; Phemister, J.; Hidalgo, J.; Young, M. Inflammatory Bowel Disease and Risk of Osteoporotic Fractures: A Meta-Analysis. Cureus 2019, 11, e5810. [Google Scholar] [CrossRef] [PubMed]
- Krela-Kaźmierczak, I.; Michalak, M.; Szymczak-Tomczak, A.; Łykowska-Szuber, L.; Stawczyk-Eder, K.; Waszak, K.; Kucharski, M.A.; Dobrowolska, A.; Eder, P. Prevalence of Osteoporosis and Osteopenia in a Population of Patients with Inflammatory Bowel Diseases from the Wielkopolska Region. Pol. Arch. Intern. Med. 2018, 128, 447–454. [Google Scholar] [CrossRef] [PubMed]
- Ribaldone, D.G.; Procopio, M.; Pellicano, R.; Barale, M.; Giudici, G.; Morino, M.; Saracco, G.M.; Astegiano, M. Predictors of Risk of Fracture in Inflammatory Bowel Diseases: A Prospective Study Using FRAX Score. Minerva Gastroenterol. Dietol. 2020, 66, 106–112. [Google Scholar] [CrossRef] [PubMed]
- Ratajczak, A.E.; Rychter, A.M.; Zawada, A.; Dobrowolska, A.; Krela-Kaźmierczak, I. Nutrients in the Prevention of Osteoporosis in Patients with Inflammatory Bowel Diseases. Nutrients 2020, 12, 1702. [Google Scholar] [CrossRef] [PubMed]
- Nawrat-Szołtysik, A.; Miodońska, Z.; Zarzeczny, R.; Zając-Gawlak, I.; Opara, J.; Grzesińska, A.; Matyja, B.; Polak, A. Osteoporosis in Polish Older Women: Risk Factors and Osteoporotic Fractures: A Cross-Sectional Study. Int. J. Environ. Res. Public. Health 2020, 17, 3725. [Google Scholar] [CrossRef] [PubMed]
- Ratajczak, A.E.; Szymczak-Tomczak, A.; Zawada, A.; Rychter, A.M.; Dobrowolska, A.; Krela-Kaźmierczak, I. Does Drinking Coffee and Tea Affect Bone Metabolism in Patients with Inflammatory Bowel Diseases? Nutrients 2021, 13, 216. [Google Scholar] [CrossRef]
- Barthel, C.; Wiegand, S.; Scharl, S.; Scharl, M.; Frei, P.; Vavricka, S.R.; Fried, M.; Sulz, M.C.; Wiegand, N.; Rogler, G.; et al. Patients’ Perceptions on the Impact of Coffee Consumption in Inflammatory Bowel Disease: Friend or Foe?--A Patient Survey. Nutr. J. 2015, 14, 78. [Google Scholar] [CrossRef]
- Ward, K.D.; Klesges, R.C. A Meta-Analysis of the Effects of Cigarette Smoking on Bone Mineral Density. Calcif. Tissue Int. 2001, 68, 259–270. [Google Scholar] [CrossRef]
- Piovani, D.; Danese, S.; Peyrin-Biroulet, L.; Nikolopoulos, G.K.; Lytras, T.; Bonovas, S. Environmental Risk Factors for Inflammatory Bowel Diseases: An Umbrella Review of Meta-Analyses. Gastroenterology 2019, 157, 647–659.e4. [Google Scholar] [CrossRef]
- Regueiro, M.; Kip, K.E.; Cheung, O.; Hegazi, R.A.; Plevy, S. Cigarette Smoking and Age at Diagnosis of Inflammatory Bowel Disease. Inflamm. Bowel Dis. 2005, 11, 42–47. [Google Scholar] [CrossRef]
- Rubin, D.T.; Hanauer, S.B. Smoking and Inflammatory Bowel Disease. Eur. J. Gastroenterol. Hepatol. 2000, 12, 855–862. [Google Scholar] [CrossRef] [PubMed]
- Thomas, T.; Chandan, J.S.; Li, V.S.W.; Lai, C.Y.; Tang, W.; Bhala, N.; Kaplan, G.G.; Ng, S.C.; Ghosh, S. Global Smoking Trends in Inflammatory Bowel Disease: A Systematic Review of Inception Cohorts. PLoS ONE 2019, 14, e0221961. [Google Scholar] [CrossRef]
- Lakatos, P.L.; Szamosi, T.; Lakatos, L. Smoking in Inflammatory Bowel Diseases: Good, Bad or Ugly? World J. Gastroenterol. WJG 2007, 13, 6134–6139. [Google Scholar] [CrossRef] [PubMed]
- Silvennoinen, J.A.; Lehtola, J.K.; Niemelä, S.E. Smoking Is a Risk Factor for Osteoporosis in Women with Inflammatory Bowel Disease. Scand. J. Gastroenterol. 1996, 31, 367–371. [Google Scholar] [CrossRef] [PubMed]
- Bergmann, M.M.; Hernandez, V.; Bernigau, W.; Boeing, H.; Chan, S.S.M.; Luben, R.; Khaw, K.-T.; van Schaik, F.; Oldenburg, B.; Bueno-de-Mesquita, B.; et al. No Association of Alcohol Use and the Risk of Ulcerative Colitis or Crohn’s Disease: Data from a European Prospective Cohort Study (EPIC). Eur. J. Clin. Nutr. 2017, 71, 512–518. [Google Scholar] [CrossRef] [PubMed]
- Swanson, G.R.; Sedghi, S.; Farhadi, A.; Keshavarzian, A. Pattern of Alcohol Consumption and Its Effect on Gastrointestinal Symptoms in Inflammatory Bowel Disease. Alcohol Fayettev. N 2010, 44, 223–228. [Google Scholar] [CrossRef]
- Troy, K.L.; Mancuso, M.E.; Butler, T.A.; Johnson, J.E. Exercise Early and Often: Effects of Physical Activity and Exercise on Women’s Bone Health. Int. J. Environ. Res. Public Health 2018, 15, 878. [Google Scholar] [CrossRef]
- van Langenberg, D.R.; Papandony, M.C.; Gibson, P.R. Sleep and Physical Activity Measured by Accelerometry in Crohn’s Disease. Aliment. Pharmacol. Ther. 2015, 41, 991–1004. [Google Scholar] [CrossRef]
- WHO Scientific Group on the Prevention and Management of Osteoporosis (2000: Geneva, Switzerland). Prevention and Management of Osteoporosis: Report of a WHO Scientific Group; World Health Organization: Geneva, Switzerland, 2003; Volume 921, pp. 1–164. [Google Scholar]
- Sheu, A.; Diamond, T. Bone Mineral Density: Testing for Osteoporosis. Aust. Prescr. 2016, 39, 35–39. [Google Scholar] [CrossRef] [PubMed]
- Argollo, M.; Gilardi, D.; Peyrin-Biroulet, C.; Chabot, J.-F.; Peyrin-Biroulet, L.; Danese, S. Comorbidities in Inflammatory Bowel Disease: A Call for Action. Lancet Gastroenterol. Hepatol. 2019, 4, 643–654. [Google Scholar] [CrossRef]
- Schüle, S.; Rossel, J.-B.; Frey, D.; Biedermann, L.; Scharl, M.; Zeitz, J.; Freitas-Queiroz, N.; Kuntzen, T.; Greuter, T.; Vavricka, S.R.; et al. Widely Differing Screening and Treatment Practice for Osteoporosis in Patients with Inflammatory Bowel Diseases in the Swiss IBD Cohort Study. Medicine 2017, 96, e6788. [Google Scholar] [CrossRef]
- Komaki, Y.; Komaki, F.; Micic, D.; Ido, A.; Sakuraba, A. Risk of Fractures in Inflammatory Bowel Diseases: A Systematic Review and Meta-Analysis. J. Clin. Gastroenterol. 2019, 53, 441–448. [Google Scholar] [CrossRef]
- Adriani, A.; Pantaleoni, S.; Luchino, M.; Ribaldone, D.G.; Reggiani, S.; Sapone, N.; Sguazzini, C.; Isaia, G.; Pellicano, R.; Astegiano, M. Osteopenia and Osteoporosis in Patients with New Diagnosis of Inflammatory Bowel Disease. Panminerva Med. 2014, 56, 145–149. [Google Scholar] [PubMed]
- Bamberger, S.; Martinez Vinson, C.; Mohamed, D.; Viala, J.; Carel, J.-C.; Hugot, J.-P.; Simon, D. Growth and Adult Height in Patients with Crohn’s Disease Treated with Anti-Tumor Necrosis Factor α Antibodies. PLoS ONE 2016, 11, e0163126. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Lombardi, G.; Jiao, W.; Banfi, G. Effects of Exercise on Bone Status in Female Subjects, from Young Girls to Postmenopausal Women: An Overview of Systematic Reviews and Meta-Analyses. Sports Med. Auckl. NZ 2016, 46, 1165–1182. [Google Scholar] [CrossRef] [PubMed]
- Paudel, S.; Owen, A.J.; Owusu-Addo, E.; Smith, B.J. Physical Activity Participation and the Risk of Chronic Diseases among South Asian Adults: A Systematic Review and Meta-Analysis. Sci. Rep. 2019, 9, 9771. [Google Scholar] [CrossRef]
- Wang, Q.; Xu, K.-Q.; Qin, X.-R.; Lu, W.; Liu, Y.; Wang, X.-Y. Association between Physical Activity and Inflammatory Bowel Disease Risk: A Meta-Analysis. Dig. Liver Dis. Off. J. Ital. Soc. Gastroenterol. Ital. Assoc. Study Liver 2016, 48, 1425–1431. [Google Scholar] [CrossRef] [PubMed]
- Chang, H.-C.; Hsieh, C.-F.; Lin, Y.-C.; Tantoh, D.M.; Ko, P.-C.; Kung, Y.-Y.; Wang, M.-C.; Hsu, S.-Y.; Liaw, Y.-C.; Liaw, Y.-P. Does Coffee Drinking Have Beneficial Effects on Bone Health of Taiwanese Adults? A Longitudinal Study. BMC Public Health 2018, 18, 1273. [Google Scholar] [CrossRef] [PubMed]
- Yang, P.; Zhang, X.-Z.; Zhang, K.; Tang, Z. Associations between Frequency of Coffee Consumption and Osteoporosis in Chinese Postmenopausal Women. Int. J. Clin. Exp. Med. 2015, 8, 15958–15966. [Google Scholar]
- Hallström, H.; Byberg, L.; Glynn, A.; Lemming, E.W.; Wolk, A.; Michaëlsson, K. Long-Term Coffee Consumption in Relation to Fracture Risk and Bone Mineral Density in Women. Am. J. Epidemiol. 2013, 178, 898–909. [Google Scholar] [CrossRef]
- Głąbska, D.; Guzek, D.; Lech, G. Analysis of the Nutrients and Food Products Intake of Polish Males with Ulcerative Colitis in Remission. Nutrients 2019, 11, 2333. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Xiang, L.; He, J. Beverage Intake and Risk of Crohn Disease. Medicine 2019, 98, e15795. [Google Scholar] [CrossRef] [PubMed]
- Swanson, G.R.; Tieu, V.; Shaikh, M.; Forsyth, C.; Keshavarzian, A. Is Moderate Red Wine Consumption Safe in Inactive Inflammatory Bowel Disease? Digestion 2011, 84, 238–244. [Google Scholar] [CrossRef]
- Ayling, R.M.; Kok, K. Fecal Calprotectin. Adv. Clin. Chem. 2018, 87, 161–190. [Google Scholar] [CrossRef] [PubMed]
- Malik, P.; Gasser, R.W.; Kemmler, G.; Moncayo, R.; Finkenstedt, G.; Kurz, M.; Fleischhacker, W.W. Low Bone Mineral Density and Impaired Bone Metabolism in Young Alcoholic Patients without Liver Cirrhosis: A Cross-Sectional Study. Alcohol. Clin. Exp. Res. 2009, 33, 375–381. [Google Scholar] [CrossRef] [PubMed]
- Cheraghi, Z.; Doosti-Irani, A.; Almasi-Hashiani, A.; Baigi, V.; Mansournia, N.; Etminan, M.; Mansournia, M.A. The Effect of Alcohol on Osteoporosis: A Systematic Review and Meta-Analysis. Drug Alcohol Depend. 2019, 197, 197–202. [Google Scholar] [CrossRef] [PubMed]
- Cho, Y.; Choi, S.; Kim, K.; Lee, G.; Park, S.M. Association between Alcohol Consumption and Bone Mineral Density in Elderly Korean Men and Women. Arch. Osteoporos. 2018, 13, 46. [Google Scholar] [CrossRef] [PubMed]
- Bainbridge, K.E.; Sowers, M.; Lin, X.; Harlow, S.D. Risk Factors for Low Bone Mineral Density and the 6-Year Rate of Bone Loss among Premenopausal and Perimenopausal Women. Osteoporos. Int. J. Establ. Result Coop. Eur. Found. Osteoporos. Natl. Osteoporos. Found. USA 2004, 15, 439–446. [Google Scholar] [CrossRef][Green Version]
- Cawthon, P.M.; Harrison, S.L.; Barrett-Connor, E.; Fink, H.A.; Cauley, J.A.; Lewis, C.E.; Orwoll, E.S.; Cummings, S.R. Alcohol Intake and Its Relationship with Bone Mineral Density, Falls, and Fracture Risk in Older Men. J. Am. Geriatr. Soc. 2006, 54, 1649–1657. [Google Scholar] [CrossRef]
- Berg, K.M.; Kunins, H.V.; Jackson, J.L.; Nahvi, S.; Chaudhry, A.; Harris, K.A.; Malik, R.; Arnsten, J.H. Association between Alcohol Consumption and Both Osteoporotic Fracture and Bone Density. Am. J. Med. 2008, 121, 406–418. [Google Scholar] [CrossRef]

| Category | Osteoporosis n (%) | Osteopenia n (%) | Normal Bone Mass n (%) | p-Value | |
|---|---|---|---|---|---|
| Group | |||||
| L2–L4 | |||||
| CD | 12 (11.7%) | 38 (36.9%) | 53 (51.5%) | p = 0.0269 | |
| UC | 4 (3.8%) | 31 (29.5%) | 70 (66.7%) | ||
| FN | |||||
| CD | 6 (5.8%) | 37 (35.9%) | 60 (58.3%) | p = 0.1218 | |
| UC | 3 (2.9%) | 27 (25.7%) | 75 (71.4%) | ||
| Demographic Characteristics | CD | Osteopenia and Osteoporosis | Normal BMD | p-Value |
|---|---|---|---|---|
| N (%) | 103 | 61 (59.2%) | 42 (40%) | |
| Age (Years) (mean ± SD) | 35.78 ± 12.78 | 37.03 ± 13.27 | 33.95 ± 11.95 | p = 0.2693 |
| Weight (kg) (mean ± SD) | 63.39 ± 13.71 | 59.2 ± 12 | 69.48 ± 13.89 | p = 0.0004 |
| Height (m) (mean ± SD) | 171.17 ± 10.19 | 168.49 ± 9.82 | 175.07 ± 9.54 | p = 0.0017 |
| Demographic Characteristics | UC | Osteopenia and Osteoporosis | Normal BMD | p-Value |
|---|---|---|---|---|
| N (%) | 105 | 48 (45.7%) | 57 (54.3%) | |
| Age (Years) (mean ± SD) | 39.56 ± 14.97 | 44.38 ± 15.62 | 34.94 ± 12.72 | p = 0.0036 |
| Weight (kg) (mean ± SD) | 68.38 ± 14.83 | 65.78 ± 15.43 | 70.06 ± 13.95 | p = 0.1355 |
| Height (m) (mean ± SD) | 171.01 ± 9.8 | 168.94 ± 10.04 | 173.69 ± 9.45 | p = 0.0554 |
| BMI (kg/m2) (mean ± SD) | 23.29 ± 4.28 | 22.99 ± 4.78 | 23.15 ± 3.93 | p = 0.4451 |
| Demographic Characteristics | All Subjects (IBD) Female | Osteopenia and Osteoporosis | Normal BMD | p-Value |
|---|---|---|---|---|
| N (%) | 107 | 56 (52.3%) | 51 (47.7%) | |
| Age (Years) (mean ± SD) | 39.58 ± 14.71 | 43.91 ± 15.49 | 34.82 ± 12.29 | p = 0.0024 |
| Weight (kg) (mean ± SD) | 58.73 ± 12.43 | 55.07 ± 11.17 | 62.74 ± 12.61 | p = 0.0019 |
| Height (m) (mean ± SD) | 164.08 ± 7.34 | 161.16 ± 5.42 | 167.29 ± 7.85 | p < 0.0001 |
| BMI (kg/m2) (mean ± SD) | 21.77 ± 4.18 | 21.2 ± 4.21 | 22.39 ± 4.09 | p = 0.1103 |
| Demographic Characteristics | All Subjects (IBD) Male | Osteopenia and Osteoporosis | Normal BMD | p-Value |
|---|---|---|---|---|
| N (%) | 101 | 52 | 49 | |
| Age (Years) (mean ± SD) | 35.68 ± 13.03 | 36.27 ± 12.88 | 35.06 ± 13.29 | p = 0.5338 |
| Weight (kg) (mean ± SD) | 73.52 ± 12.49 | 69.6 ± 12.68 | 77.68 ± 10.94 | p = 0.0007 |
| Height (m) (mean ± SD) | 178.51 ± 6.37 | 176.79 ± 6.61 | 180.35 ± 5.6 | p = 0.0121 |
| BMI (kg/m2) (mean ± SD) | 23.08 ± 3.93 | 22.28 ± 4.07 | 23.94 ± 3.63 | p = 0.0174 |
| CD | Osteopenia and Osteoporosis | Normal BMD | p-Value | |
|---|---|---|---|---|
| N (%) | 103 | 61 (59.2%) | 42 (40%) | |
| Smoker N (%) | 28 (27.2%) | 14 (23%) | 14 (33.3%) | p = 0.2445 |
| Alcohol consumption N (%) | 36 (35%) | 21 (34.4%) | 15 (35.7%) | p = 0.8928 |
| Coffee drinker N (%) | 57 (55.3%) | 33 (54.1%) | 24 (57.1%) | p = 0.76 |
| Exercise N (%) | 66 (64.1%) | 34 (55.7%) | 32 (76.2%) | p = 0.0335 |
| Demographic Characteristics | UC | Osteopenia and Osteoporosis | Normal BMD | p-Value |
|---|---|---|---|---|
| N (%) | 105 | 48 (45.7%) | 57 (54.3%) | |
| Smoker N (%) | 8 (7.6%) | 3 (6.3%) | 5 (8.8%) | p = 0.6674 |
| Alcohol consumption N (%) | 42 (40%) | 19 (39.6%) | 23 (40.4%) | p = 0.9361 |
| Coffee drinker N (%) | 67 (63.8%) | 31 (64.6%) | 36 (63.2%) | p = 0.6801 |
| Exercise N (%) | 62 (59%) | 27 (56.3%) | 35 (61.4%) | p = 0.7639 |
| Demographic Characteristics | All Female Subjects (IBD) | Osteopenia and Osteoporosis | Normal BMD | p-Value |
|---|---|---|---|---|
| N (%) | 107 | 56 (52.3%) | 51 (47.7%) | |
| Smoker N (%) | 10 (9.3%) | 6 (10.7%) | 4 (7.8%) | p = 0.6063 |
| Alcohol consumption N (%) | 33 (30.8%) | 17 (30.4%) | 16 (31.4%) | p = 0.911 |
| Coffee drinker N (%) | 65 (60.7%) | 32 (57.1%) | 33 (64.7%) | p = 0.4214 |
| Exercise N (%) | 56 (52.3%) | 23 (41.1%) | 33 (64.7%) | p = 0.0146 |
| Demographic Characteristics | All Male Subjects (IBD) | Osteopenia and Osteoporosis | Normal BMD | p-Value |
|---|---|---|---|---|
| N (%) | 101 | 52 (51.5%) | 49 (48.5%) | |
| Smoker N (%) | 26 (25.7%) | 11 (21.2%) | 15 (30.6%) | p = 0.2803 |
| Alcohol consumption N (%) | 45 (44.6%) | 23 (44.2%) | 22 (44.9%) | p = 0.9436 |
| Coffee drinker N (%) | 59 (58.4%) | 32 (61.5%) | 27 (55.1%) | p = 0.5143 |
| Exercise N (%) | 72 (71.3%) | 38 (73.1%) | 34 (69.4%) | p = 0.6812 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rychter, A.M.; Ratajczak, A.E.; Szymczak-Tomczak, A.; Michalak, M.; Eder, P.; Dobrowolska, A.; Krela-Kaźmierczak, I. Associations of Lifestyle Factors with Osteopenia and Osteoporosis in Polish Patients with Inflammatory Bowel Disease. Nutrients 2021, 13, 1863. https://doi.org/10.3390/nu13061863
Rychter AM, Ratajczak AE, Szymczak-Tomczak A, Michalak M, Eder P, Dobrowolska A, Krela-Kaźmierczak I. Associations of Lifestyle Factors with Osteopenia and Osteoporosis in Polish Patients with Inflammatory Bowel Disease. Nutrients. 2021; 13(6):1863. https://doi.org/10.3390/nu13061863
Chicago/Turabian StyleRychter, Anna Maria, Alicja Ewa Ratajczak, Aleksandra Szymczak-Tomczak, Michał Michalak, Piotr Eder, Agnieszka Dobrowolska, and Iwona Krela-Kaźmierczak. 2021. "Associations of Lifestyle Factors with Osteopenia and Osteoporosis in Polish Patients with Inflammatory Bowel Disease" Nutrients 13, no. 6: 1863. https://doi.org/10.3390/nu13061863
APA StyleRychter, A. M., Ratajczak, A. E., Szymczak-Tomczak, A., Michalak, M., Eder, P., Dobrowolska, A., & Krela-Kaźmierczak, I. (2021). Associations of Lifestyle Factors with Osteopenia and Osteoporosis in Polish Patients with Inflammatory Bowel Disease. Nutrients, 13(6), 1863. https://doi.org/10.3390/nu13061863







