Vascular Effects of the Polyphenolic Nutraceutical Supplement Taurisolo®: Focus on the Protection of the Endothelial Function
Abstract
:1. Introduction
2. Materials and Methods
2.1. Taurisolo® Supplement
2.2. Cell Cultures
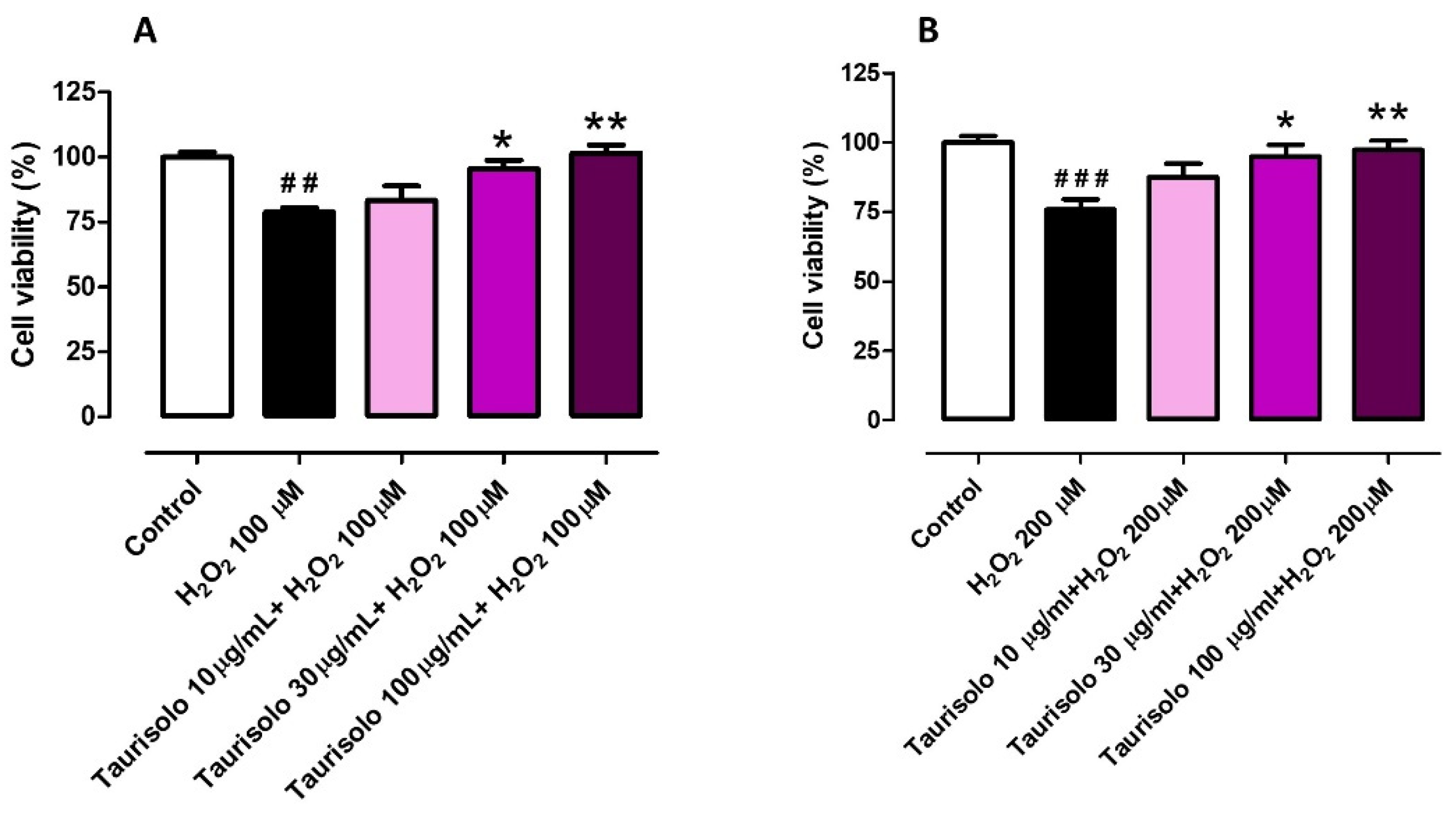
2.2.1. Evaluation of the Cell Viability Preservation against H2O2-Induced Cell Damage in HASMCs and HUVECs
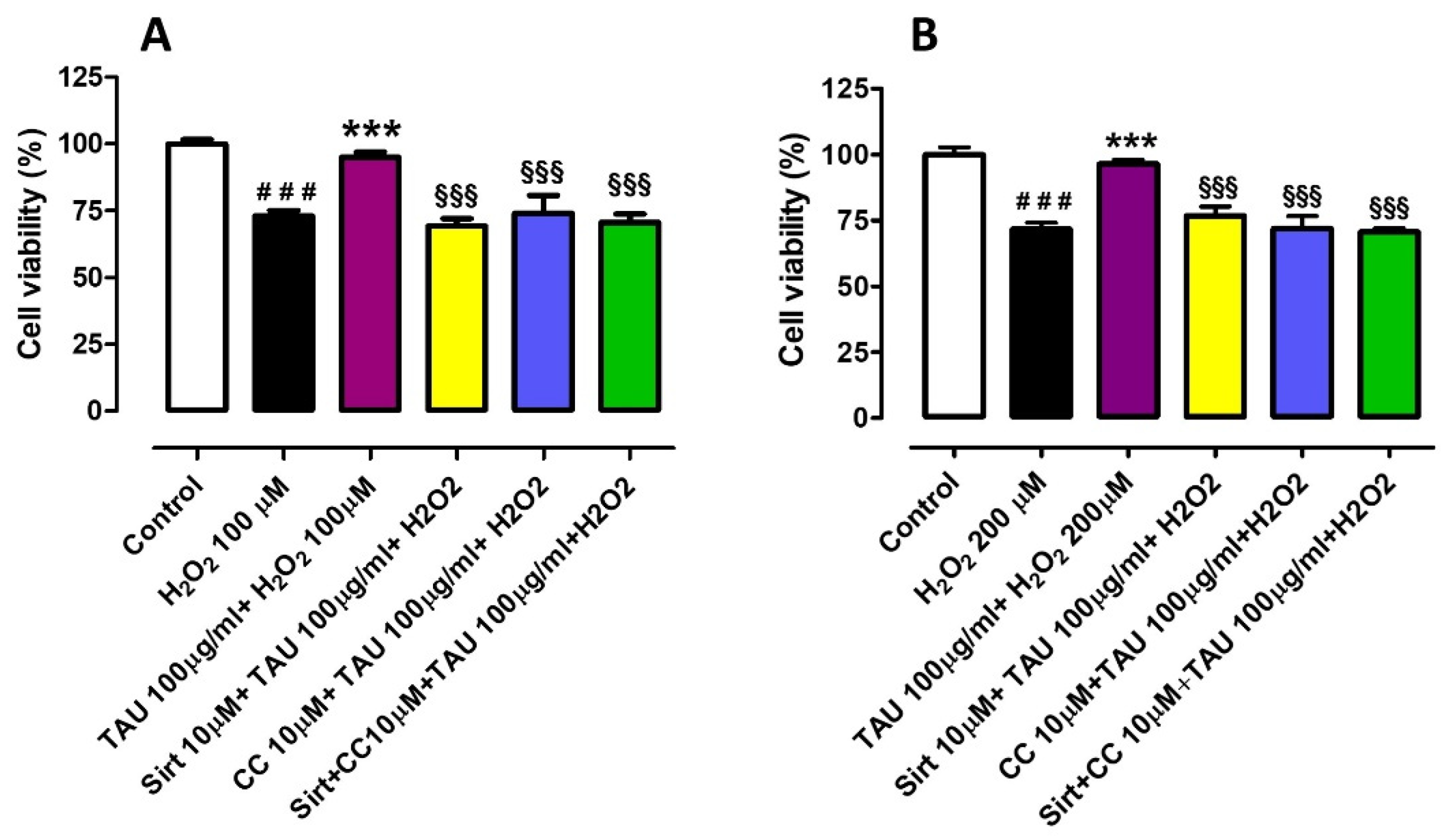
2.2.2. Evaluation of Cell Viability Preservation against H2O2-Induced Cell Damage in HASMCs and HUVECs in the Presence of Sirtuins and AMPK Inhibitors
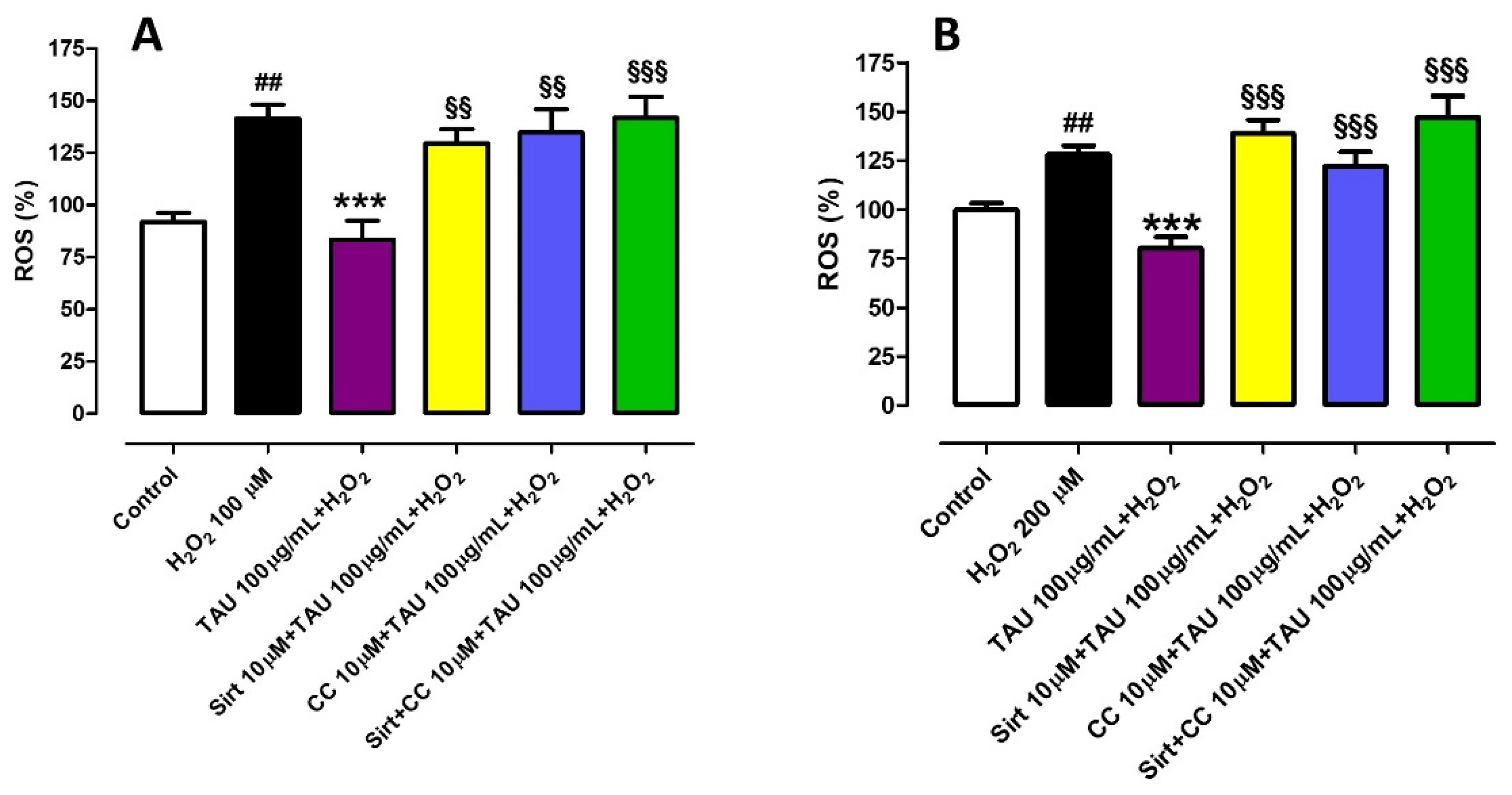
2.2.3. Measurement of Intracellular H2O2-Induced ROS Production in HUVECs and HASMCs in the Presence of Sirtuins and AMPK Inhibitors
2.2.4. Cell Experiments Data Analysis
2.3. Animals Protocols and Ethical Statements
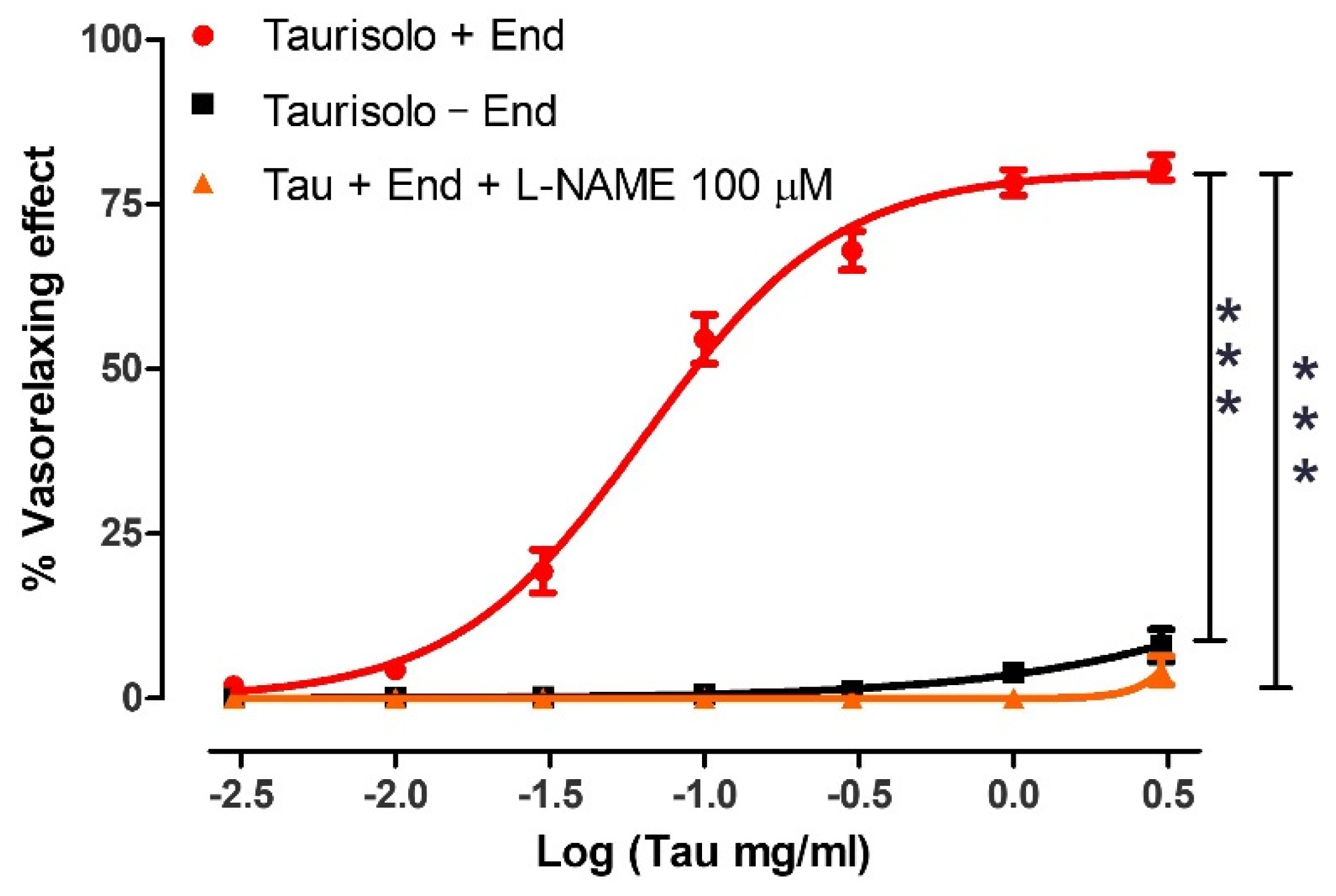
2.3.1. Evaluation of the Vasorelaxing Effect of Taurisolo® on Rat Aorta Rings in the Presence and Absence of Endothelium
2.3.2. Evaluation of the Involvement of Sirtuins and AMPK Pathways in the Vasorelaxing Activity of Taurisolo®
2.3.3. Evaluation of the Efficacy of Taurisolo® to Restrain Noradrenaline (NA)-Induced Vasoconstriction
2.3.4. In Vitro Experiments Statistical Analysis
2.4. Anti-Hypertensive Effects of Taurisolo® in Spontaneously Hypertensive Rats (SHRs) In Vivo Model
2.4.1. Evaluation of Taurisolo® Protection against Endothelial Dysfunction in SHRs
2.4.2. Effect of Taurisolo® on Glycemic and Lipid Parameters in SHRs
2.4.3. Preventive Effects of Taurisolo® against Cardiac Hypertrophy in SHRs
2.5. Measurement of Coagulation Factors and Fibrinogen
Clot Retraction Assay
2.6. Human Clinical Studies on the Effects of Taurisolo® on Endothelial Function
2.6.1. Study Population and Protocol
2.6.2. Blood Parameter Analyses
2.6.3. Brachial Artery Flow-Mediated Dilation (FMD) and Reactive Hyperemia Index (RHI)
3. Results
3.1. Evaluation of the Protective Effect Induced by Taurisolo® on HUVEC and HASMC Cell Viability, against the H2O2-Induced Oxidative Damage
3.2. Investigation of the Potential Mechanisms of Action Involved in the Protective Effect Induced by Taurisolo® on HUVEC and HASMC Cell Viability, against the H2O2-Induced Oxidative Damage. Evaluation of Sirtuins and AMPK Pathways
3.3. Investigation of the Potential Mechanisms of Action Involved in the Protective Effect Induced by Taurisolo® on HUVECs and HASMCs, against the H2O2-Induced ROS Production. Evaluation of Sirtuins and AMPK Pathways
3.4. Evaluation of the Direct Vasorelaxant Effect Induced by Taurisolo® in Endothelial Intact or Endothelial Denuded Rat Aortic Rings: Involvement of Endogenous NO
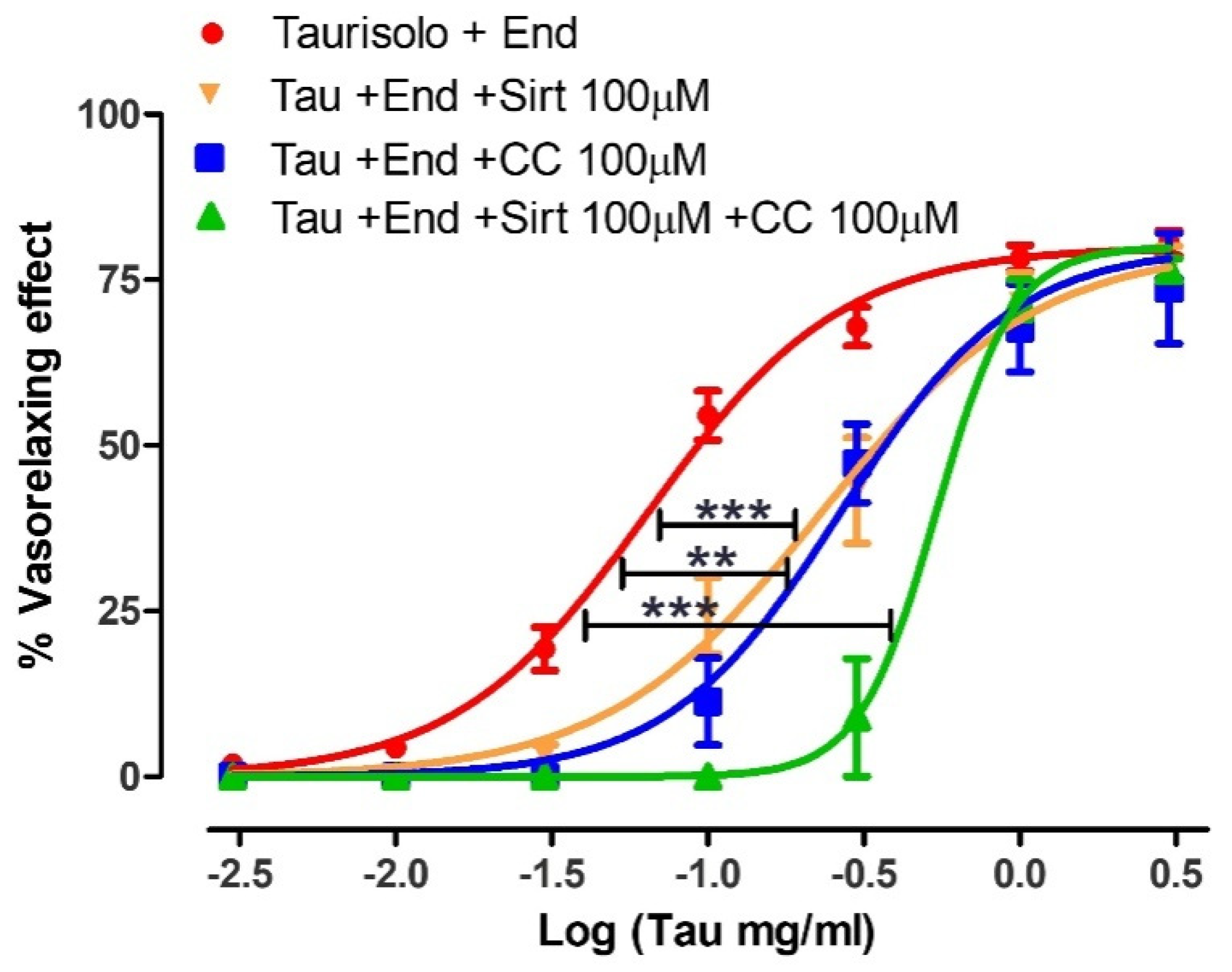
3.5. Evaluation of the Direct Vasorelaxant Effect Induced by Taurisolo® in Endothelial Intact or Endothelial Denuded Rat Aortic Rings in the Presence or in the Absence of Specific Inhibitors of Sirtuins (Sirtinol 100 µM) or AMPK (Compound C 100 µM) Pathways
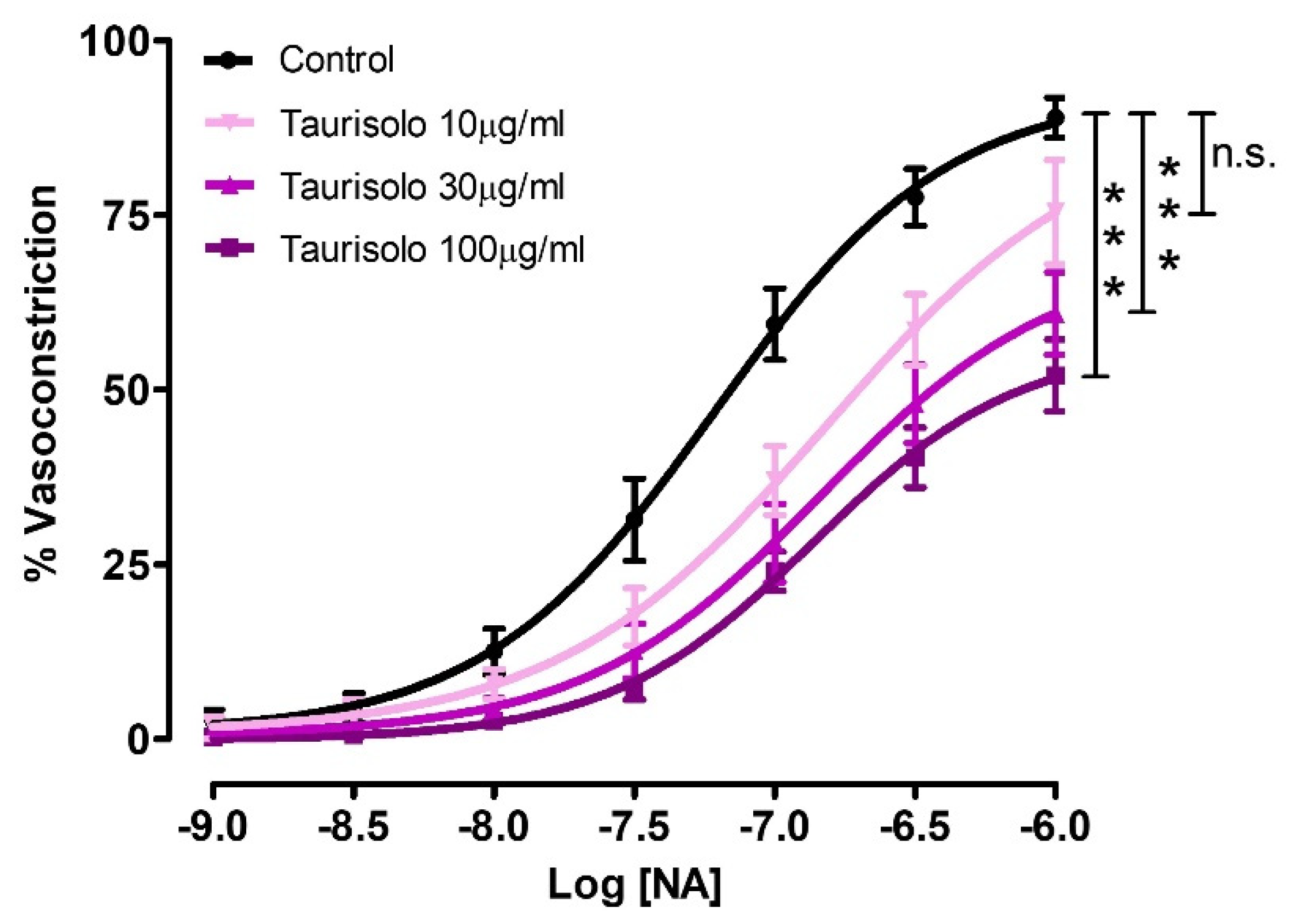
3.6. Inhibition of NA-Induced Vasoconstriction by Three Different Concentrations of Taurisolo® Pre-Incubated in Endothelial-Intact Rat Aortic Rings
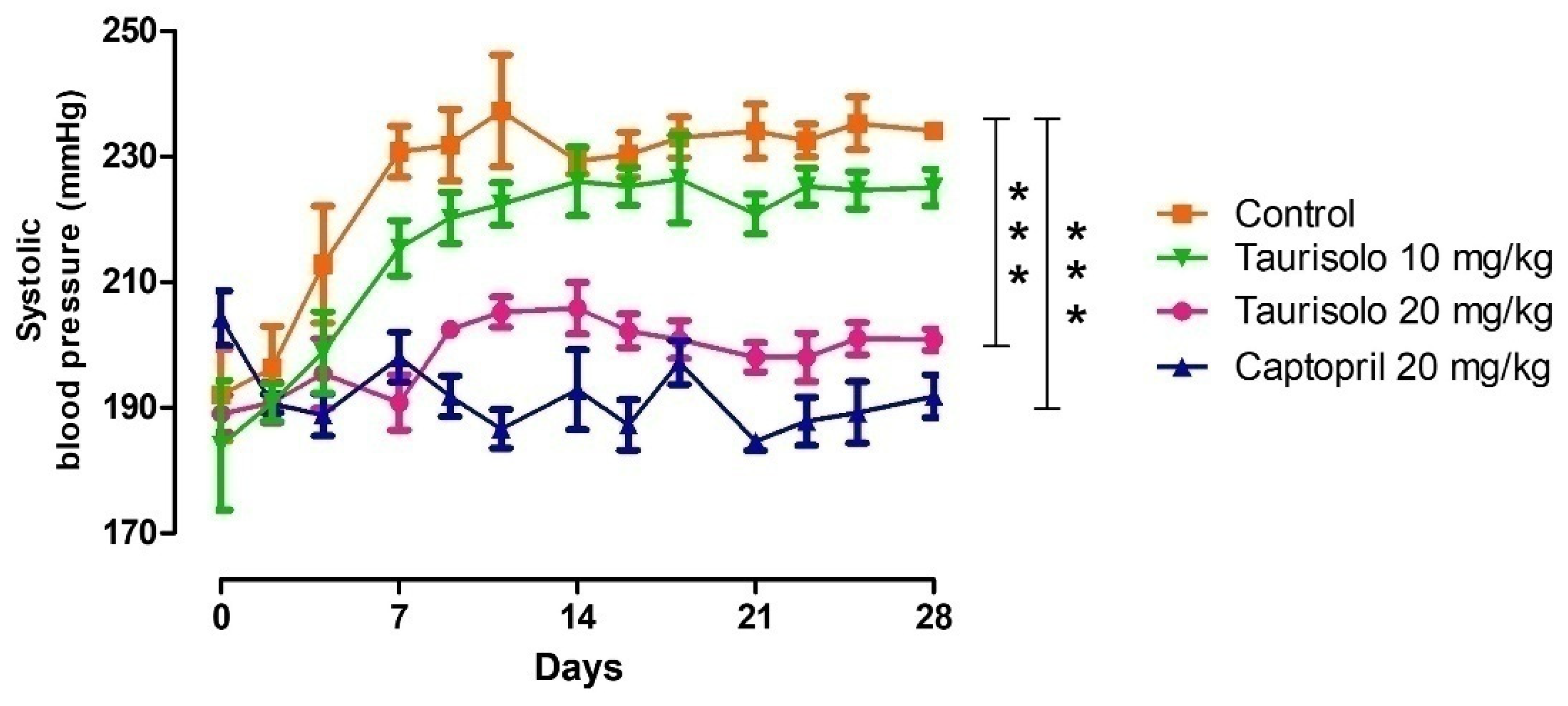
3.7. Effect of Taurisolo® In Vivo Chronic Administration on Systolic Blood Pressure Values in SHRs
3.8. Effect of Taurisolo® on Glycaemic Levels and the Lipid Panel of the SHRs at the End of the In Vivo Chronic Treatment
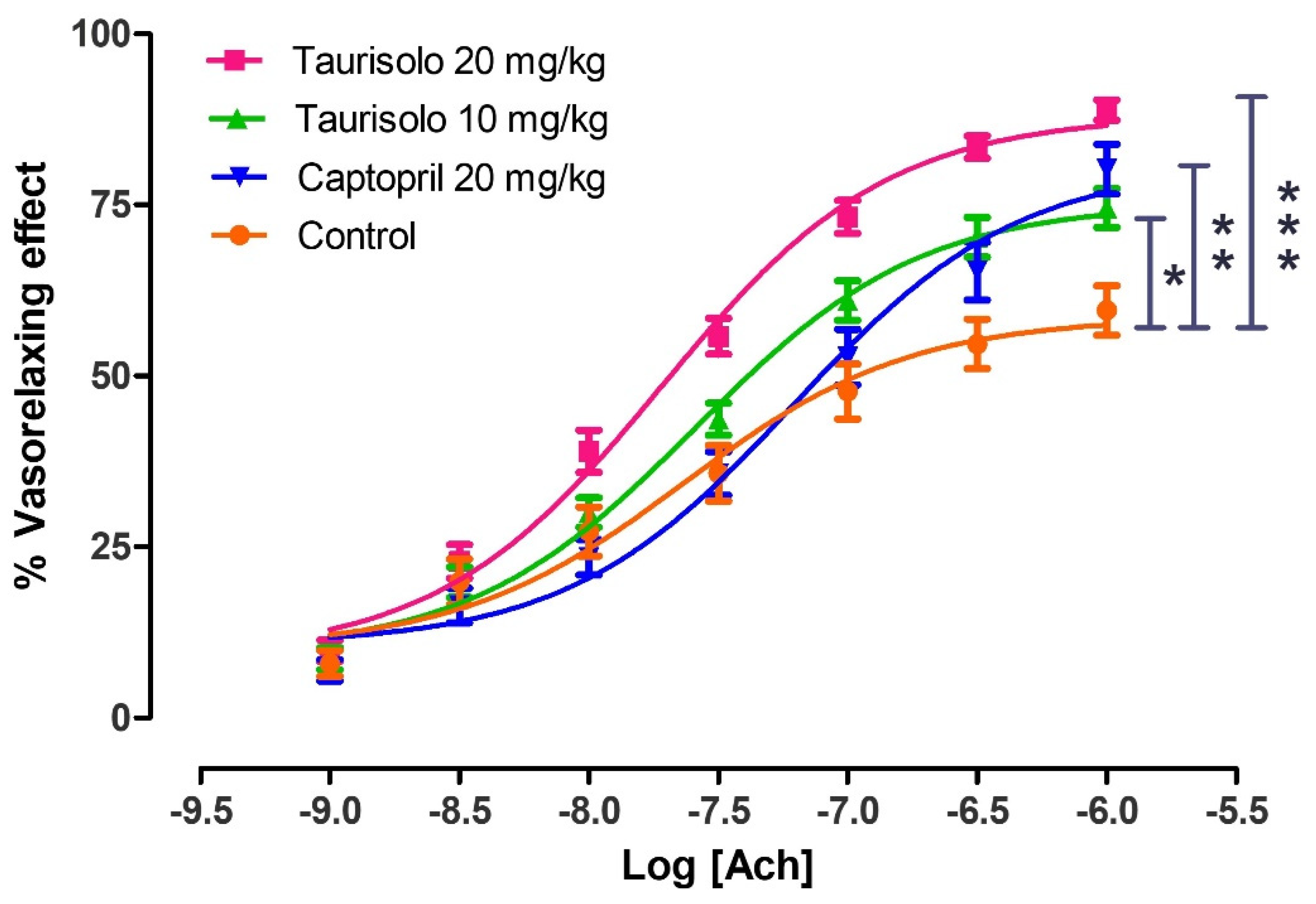
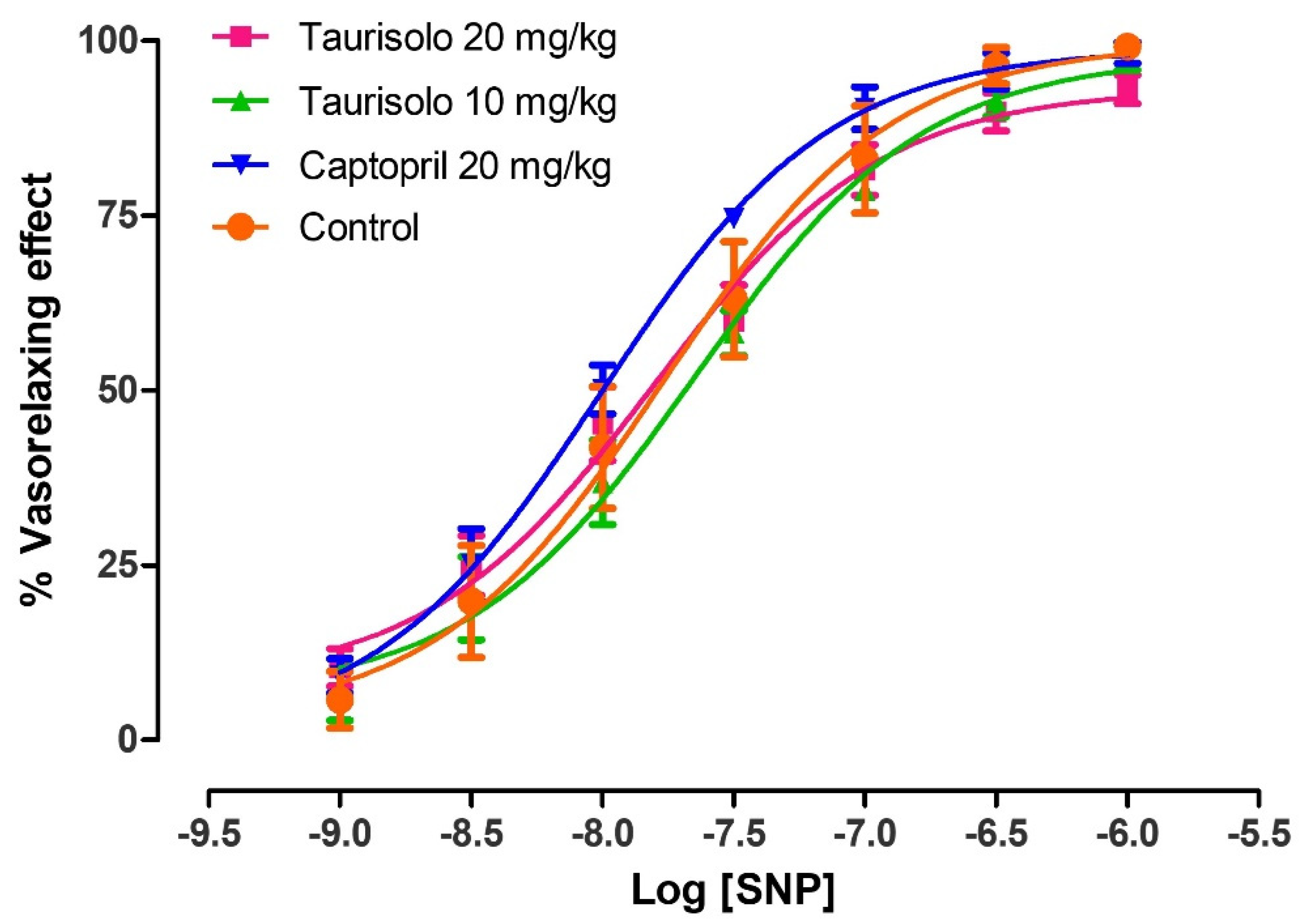
3.9. Evaluation of the Protection Induced by Taurisolo® against the Endothelial Dysfunction Exhibited by SHRs
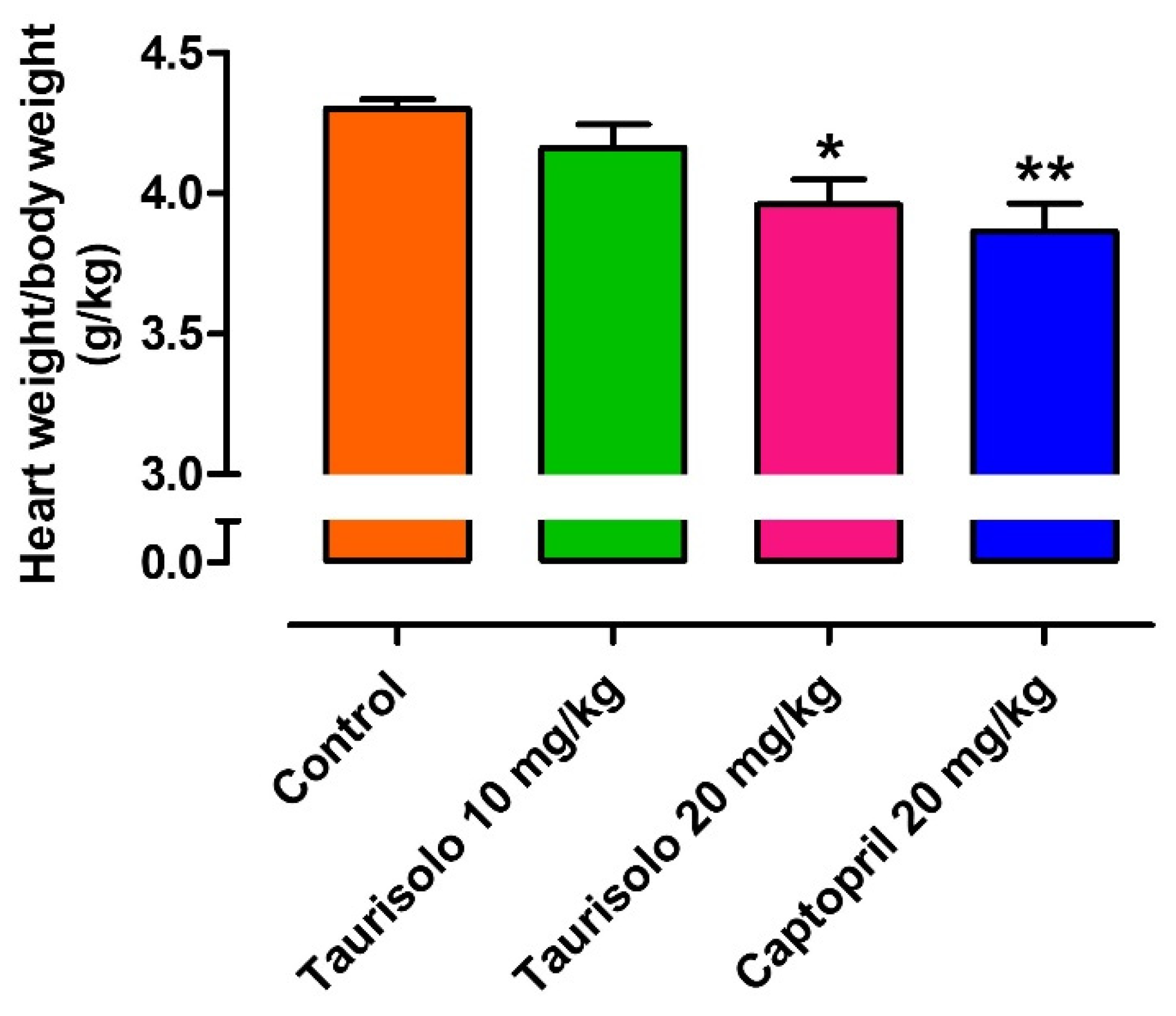
3.10. Evaluation of the Protective Effect Induced by Taurisolo® against the Cardiac Hypertrophy Exhibited by SHRs
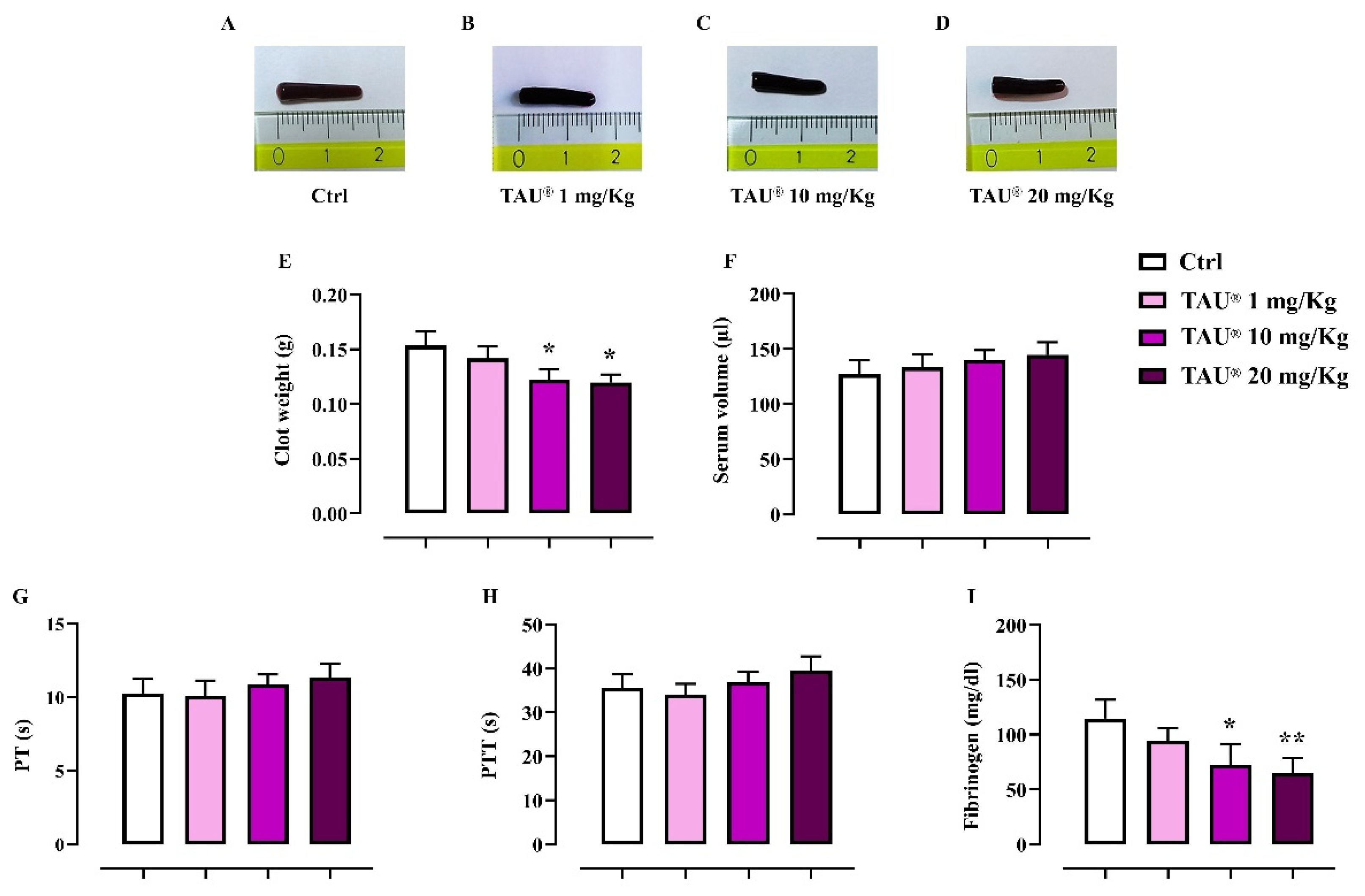
3.11. Effect of Taurisolo® on Indexes of Coagulation and Clot Retraction
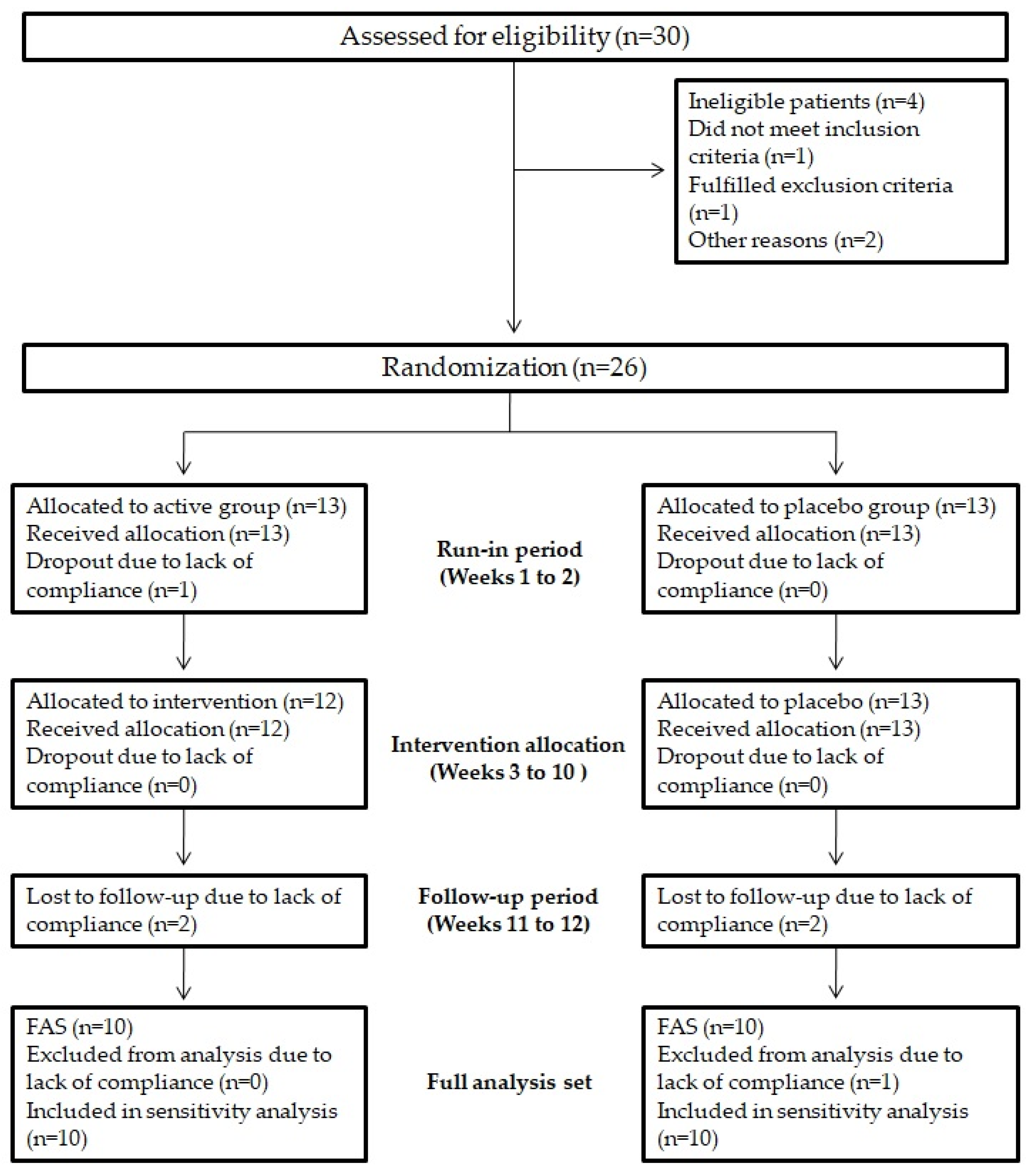
3.12. Enrolment and Subject Attrition
3.13. Baseline Characteristics of Study Participants
3.14. In Vivo Effects of Taurisolo® on Endothelial Function and Oxidative Stress-Related Biomarkers
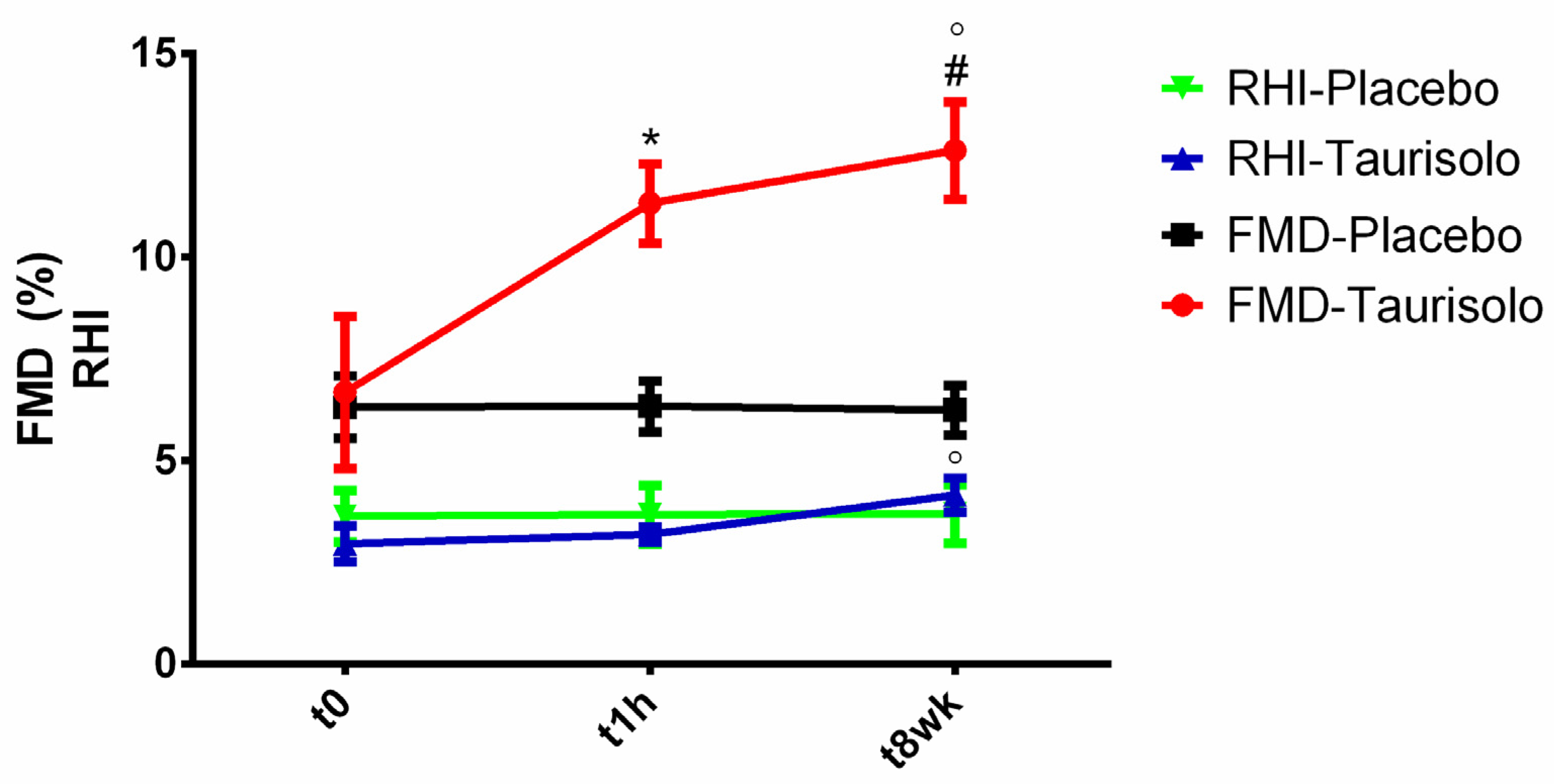
3.14.1. In Vivo Effects of Taurisolo® on Endothelial Function
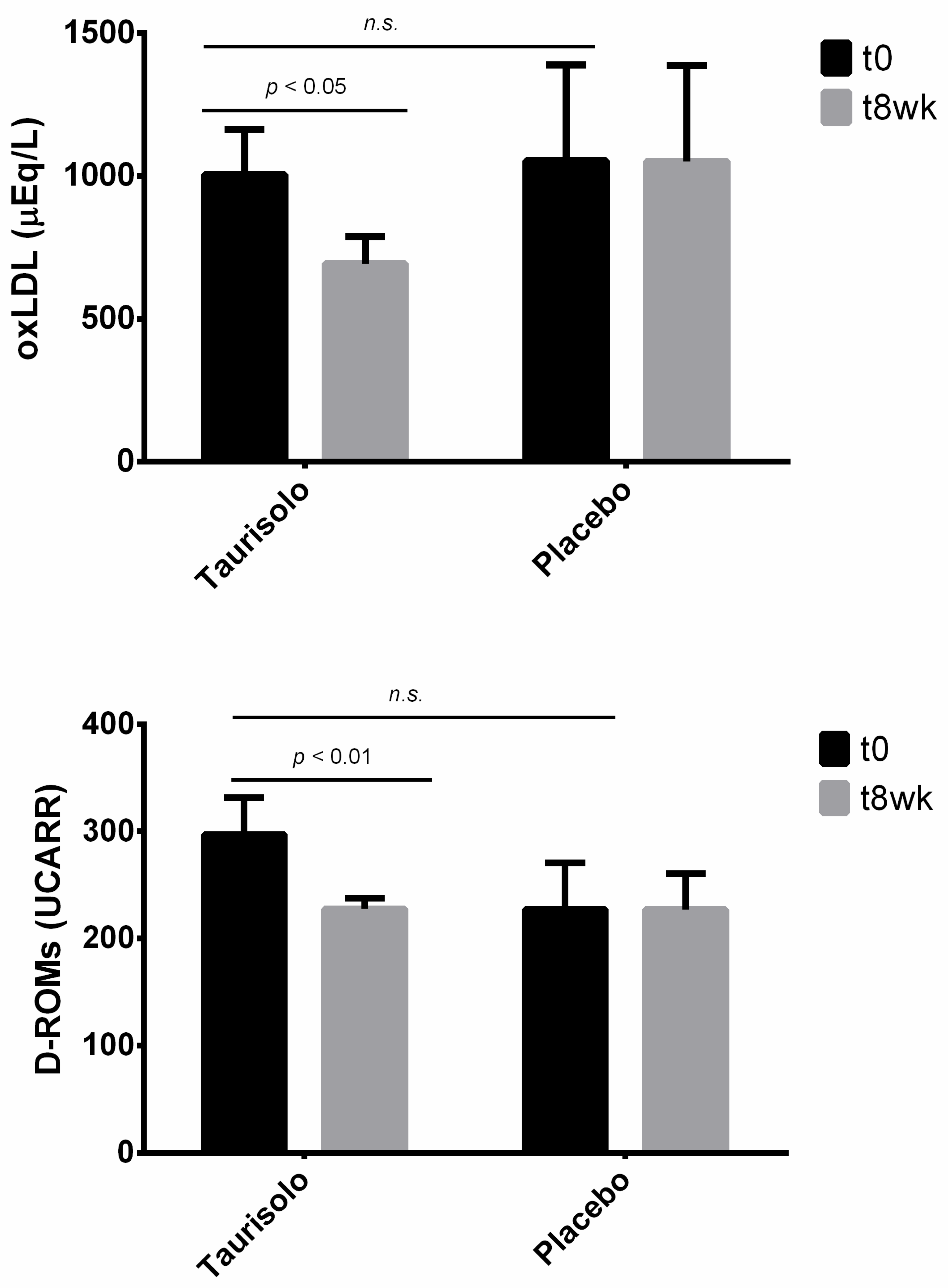
3.14.2. In Vivo Effects of Taurisolo® on Oxidative Stress-Related Biomarkers
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Corretti, M.C.; Anderson, T.J.; Benjamin, E.J.; Celermajer, D.; Charbonneau, F.; Creager, M.A.; Deanfield, J.; Drexler, H.; Gerhard-Herman, M.; Herrington, D. Guidelines for the ultrasound assessment of endothelial-dependent flow-mediated vasodilation of the brachial artery: A report of the International Brachial Artery Reactivity Task Force. J. Am. Coll. Cardiol. 2002, 39, 257–265. [Google Scholar] [CrossRef] [Green Version]
- Martelli, A.; Citi, V.; Calderone, V. Recent efforts in drug discovery on vascular inflammation and consequent atherosclerosis. Expert Opin. Drug Discov. 2020, 1–17. [Google Scholar] [CrossRef]
- Annunziata, G.; Jiménez-García, M.; Capó, X.; Moranta, D.; Arnone, A.; Tenore, G.; Sureda, A.; Tejada, S. Microencapsulation as a tool to counteract the typical low bioavailability of polyphenols in the management of diabetes. Food Chem. Toxicol. 2020, 139, 111248. [Google Scholar] [CrossRef] [PubMed]
- Annunziata, G.; Maisto, M.; Schisano, C.; Ciampaglia, R.; Narciso, V.; Tenore, G.C.; Novellino, E. Effects of grape pomace polyphenolic extract (Taurisolo®) in reducing TMAO serum levels in humans: Preliminary results from a randomized, placebo-controlled, cross-over study. Nutrients 2019, 11, 139. [Google Scholar] [CrossRef] [Green Version]
- Annunziata, G.; Maisto, M.; Schisano, C.; Ciampaglia, R.; Narciso, V.; Hassan, S.T.; Tenore, G.C.; Novellino, E. Effect of grape pomace polyphenols with or without pectin on TMAO serum levels assessed by LC/MS-based assay: A preliminary clinical study on overweight/obese subjects. Front. Pharmacol. 2019, 10, 575. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, Y.; Dai, M. Trimethylamine N-Oxide Generated by the Gut Microbiota Is Associated with Vascular Inflammation: New Insights into Atherosclerosis. Mediat. Inflamm. 2020, 2020. [Google Scholar] [CrossRef] [Green Version]
- Giusti, F.; Caprioli, G.; Ricciutelli, M.; Vittori, S.; Sagratini, G. Determination of fourteen polyphenols in pulses by high performance liquid chromatography-diode array detection (HPLC-DAD) and correlation study with antioxidant activity and colour. Food Chem. 2017, 221, 689–697. [Google Scholar] [CrossRef]
- Kilkenny, C.; Browne, W.; Cuthill, I.C.; Emerson, M.; Altman, D.G. Animal research: Reporting in vivo experiments: The ARRIVE guidelines. Br. J. Pharmacol. 2010, 160, 1577–1579. [Google Scholar] [CrossRef]
- McGrath, J.C.; Lilley, E. Implementing guidelines on reporting research using animals (ARRIVE etc.): New requirements for publication in BJP. Br. J. Pharmacol. 2015, 172, 3189–3493. [Google Scholar] [CrossRef] [Green Version]
- Calderone, V.; Fiamingo, F.L.; Giorgi, I.; Leonardi, M.; Livi, O.; Martelli, A.; Martinotti, E. Heterocyclic analogs of benzanilide derivatives as potassium channel activators. IX. Eur. J. Med. Chem. 2006, 41, 761–767. [Google Scholar] [CrossRef]
- Bertini, S.; Calderone, V.; Carboni, I.; Maffei, R.; Martelli, A.; Martinelli, A.; Minutolo, F.; Rajabi, M.; Testai, L.; Tuccinardi, T. Synthesis of heterocycle-based analogs of resveratrol and their antitumor and vasorelaxing properties. Bioorg. Med. Chem. 2010, 18, 6715–6724. [Google Scholar] [CrossRef] [PubMed]
- Calderone, V.; Martelli, A.; Testai, L.; Martinotti, E.; Breschi, M.C. Functional contribution of the endothelial component to the vasorelaxing effect of resveratrol and NS 1619, activators of the large-conductance calcium-activated potassium channels. Naunyn-Schmiedeberg’s Arch. Pharmacol. 2007, 375, 73–80. [Google Scholar] [CrossRef] [PubMed]
- Martelli, A.; Piragine, E.; Citi, V.; Testai, L.; Pagnotta, E.; Ugolini, L.; Lazzeri, L.; Di Cesare Mannelli, L.; Manzo, O.L.; Bucci, M. Erucin exhibits vasorelaxing effects and antihypertensive activity by H2S-releasing properties. Br. J. Pharmacol. 2020, 177, 824–835. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Breschi, M.C.; Calderone, V.; Digiacomo, M.; Martelli, A.; Martinotti, E.; Minutolo, F.; Rapposelli, S.; Balsamo, A. NO-sartans: A new class of pharmacodynamic hybrids as cardiovascular drugs. J. Med. Chem. 2004, 47, 5597–5600. [Google Scholar] [CrossRef]
- Breschi, M.C.; Calderone, V.; Digiacomo, M.; Macchia, M.; Martelli, A.; Martinotti, E.; Minutolo, F.; Rapposelli, S.; Rossello, A.; Testai, L. New NO-releasing pharmacodynamic hybrids of losartan and its active metabolite: Design, synthesis, and biopharmacological properties. J. Med. Chem. 2006, 49, 2628–2639. [Google Scholar] [CrossRef] [PubMed]
- Martelli, A.; Testai, L.; Anzini, M.; Cappelli, A.; Di Capua, A.; Biava, M.; Poce, G.; Consalvi, S.; Giordani, A.; Caselli, G. The novel anti-inflammatory agent VA694, endowed with both NO-releasing and COX2-selective inhibiting properties, exhibits NO-mediated positive effects on blood pressure, coronary flow and endothelium in an experimental model of hypertension and endothelial dysfunction. Pharmacol. Res. 2013, 78, 1–9. [Google Scholar] [CrossRef]
- Feng, L.; Yang, X.; Shi, Y.; Liang, S.; Zhao, T.; Duan, J.; Sun, Z. Co-exposure subacute toxicity of silica nanoparticles and lead acetate on cardiovascular system. Int. J. Nanomed. 2018, 13, 7819–7834. [Google Scholar] [CrossRef] [Green Version]
- Kim, S.; Foong, D.; Cooper, M.S.; Seibel, M.J.; Zhou, H. Comparison of blood sampling methods for plasma corticosterone measurements in mice associated with minimal stress-related artefacts. Steroids 2018, 135, 69–72. [Google Scholar] [CrossRef]
- Law, D.A.; DeGuzman, F.R.; Heiser, P.; Ministri-Madrid, K.; Killeen, N.; Phillips, D.R. Integrin cytoplasmic tyrosine motif is required for outside-in αIIbβ3 signalling and platelet function. Nature 1999, 401, 808–811. [Google Scholar] [CrossRef]
- Tucker, K.L.; Sage, T.; Gibbins, J.M. Clot retraction. In Platelets and Megakaryocytes; Springer: Berlin/Heidelberg, Germany, 2012; pp. 101–107. [Google Scholar]
- Curtis, M.J.; Alexander, S.; Cirino, G.; Docherty, J.R.; George, C.H.; Giembycz, M.A.; Hoyer, D.; Insel, P.A.; Izzo, A.A.; Ji, Y. Experimental design and analysis and their reporting II: Updated and simplified guidance for authors and peer reviewers. Br. J. Pharmacol. 2018, 175, 987–993. [Google Scholar] [CrossRef] [Green Version]
- George, C.H.; Stanford, S.C.; Alexander, S.; Cirino, G.; Docherty, J.R.; Giembycz, M.A.; Hoyer, D.; Insel, P.A.; Izzo, A.A.; Ji, Y. Updating the guidelines for data transparency in the British Journal of Pharmacology–data sharing and the use of scatter plots instead of bar charts. Br. J. Pharmacol. 2017, 174, 2801–2804. [Google Scholar] [CrossRef] [Green Version]
- Alexander, S.P.; Roberts, R.E.; Broughton, B.R.; Sobey, C.G.; George, C.H.; Stanford, S.C.; Cirino, G.; Docherty, J.R.; Giembycz, M.A.; Hoyer, D. Goals and practicalities of immunoblotting and immunohistochemistry: A guide for submission to the British Journal of Pharmacology. Br. J. Pharmacol. 2018, 175, 407–411. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barrea, L.; Fabbrocini, G.; Annunziata, G.; Muscogiuri, G.; Donnarumma, M.; Marasca, C.; Colao, A.; Savastano, S. Role of nutrition and adherence to the mediterranean diet in the multidisciplinary approach of hidradenitis suppurativa: Evaluation of nutritional status and its association with severity of disease. Nutrients 2019, 11, 57. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Di Minno, M.N.D.; Ambrosino, P.; Buonomo, A.R.; Pinchera, B.; Calcaterra, I.; Crispo, M.; Scotto, R.; Borgia, F.; Mattia, C.; Gentile, I. Direct-acting antivirals improve endothelial function in patients with chronic hepatitis: A prospective cohort study. Intern. Emerg. Med. 2020, 15, 263–271. [Google Scholar] [CrossRef] [PubMed]
- Di Minno, A.; Gentile, M.; Iannuzzo, G.; Calcaterra, I.; Tripaldella, M.; Porro, B.; Cavalca, V.; Di Taranto, M.D.; Tremoli, E.; Fortunato, G. Endothelial function improvement in patients with familial hypercholesterolemia receiving PCSK-9 inhibitors on top of maximally tolerated lipid lowering therapy. Thromb. Res. 2020, 194, 229–236. [Google Scholar] [CrossRef]
- Calvert, M.; Blazeby, J.; Altman, D.G.; Revicki, D.A.; Moher, D.; Brundage, M.D. CONSORT PRO Group. Reporting of patient-reported outcomes in randomized trials: The CONSORT PRO extension. JAMA 2013, 309, 814–822. [Google Scholar] [CrossRef] [Green Version]
- Cohen, H.Y.; Miller, C.; Bitterman, K.J.; Wall, N.R.; Hekking, B.; Kessler, B.; Howitz, K.T.; Gorospe, M.; de Cabo, R.; Sinclair, D.A. Calorie restriction promotes mammalian cell survival by inducing the SIRT1 deacetylase. Science 2004, 305, 390–392. [Google Scholar] [CrossRef] [Green Version]
- San Cheang, W.; Wong, W.T.; Wang, L.; Cheng, C.K.; Lau, C.W.; Ma, R.C.W.; Xu, A.; Wang, N.; Huang, Y.; Tian, X.Y. Resveratrol ameliorates endothelial dysfunction in diabetic and obese mice through sirtuin 1 and peroxisome proliferator-activated receptor δ. Pharmacol. Res. 2019, 139, 384–394. [Google Scholar] [CrossRef]
- Bonnefont-Rousselot, D. Resveratrol and cardiovascular diseases. Nutrients 2016, 8, 250. [Google Scholar] [CrossRef]
- Xia, N.; Förstermann, U.; Li, H. Resveratrol and endothelial nitric oxide. Molecules 2014, 19, 16102–16121. [Google Scholar] [CrossRef]
- Lapi, D.; Stornaiuolo, M.; Sabatino, L.; Sommella, E.; Tenore, G.; Daglia, M.; Scuri, R.; Di Maro, M.; Colantuoni, A.; Novellino, E. The pomace extract taurisolo protects rat brain from ischemia-reperfusion injury. Front. Cell. Neurosci. 2020, 14, 3. [Google Scholar] [CrossRef] [PubMed]
- Reagan-Shaw, S.; Nihal, M.; Ahmad, N. Dose translation from animal to human studies revisited. FASEB J. 2008, 22, 659–661. [Google Scholar] [CrossRef] [Green Version]
- Wong, R.H.; Berry, N.M.; Coates, A.M.; Buckley, J.D.; Bryan, J.; Kunz, I.; Howe, P.R. Chronic resveratrol consumption improves brachial flow-mediated dilatation in healthy obese adults. J. Hypertens. 2013, 31, 1819–1827. [Google Scholar] [CrossRef] [PubMed]
- Papamichael, C.; Karatzis, E.; Karatzi, K.; Aznaouridis, K.; Papaioannou, T.; Protogerou, A.; Stamatelopoulos, K.; Zampelas, A.; Lekakis, J.; Mavrikakis, M. Red wine’s antioxidants counteract acute endothelial dysfunction caused by cigarette smoking in healthy nonsmokers. Am. Heart J. 2004, 147, 274. [Google Scholar] [CrossRef]
- Lekakis, J.; Rallidis, L.S.; Andreadou, I.; Vamvakou, G.; Kazantzoglou, G.; Magiatis, P.; Skaltsounis, A.-L.; Kremastinos, D.T. Polyphenols compounds from red grapes acutely improve endothelial function in patients with coronary heart disease. Eur. J. Prev. Cardiol. 2005, 12, 596–600. [Google Scholar] [CrossRef]
- Boban, M.; Modun, D.; Music, I.; Vukovic, J.; Brizic, I.; Salamunic, I.; Obad, A.; Palada, I.; Dujic, Z. Red wine induced modulation of vascular function: Separating the role of polyphenols, ethanol, and urates. J. Cardiovasc. Pharmacol. 2006, 47, 695–701. [Google Scholar] [CrossRef] [Green Version]
- Karatzi, K.; Papamichael, C.; Karatzis, E.; Papaioannou, T.G.; Voidonikola, P.T.; Vamvakou, G.D.; Lekakis, J.; Zampelas, A. Postprandial improvement of endothelial function by red wine and olive oil antioxidants: A synergistic effect of components of the Mediterranean diet. J. Am. Coll. Nutr. 2008, 27, 448–453. [Google Scholar] [CrossRef]
- Karatzi, K.; Papamichael, C.; Karatzis, E.; Papaioannou, T.G.; Voidonikola, P.T.; Lekakis, J.; Zampelas, A. Acute smoking induces endothelial dysfunction in healthy smokers. Is this reversible by red wine’s antioxidant constituents? J. Am. Coll. Nutr. 2007, 26, 10–15. [Google Scholar] [CrossRef]
- Hampton, S.; Isherwood, C.; Kirkpatrick, V.; Lynne-Smith, A.; Griffin, B. The influence of alcohol consumed with a meal on endothelial function in healthy individuals. J. Hum. Nutr. Diet. 2010, 23, 120–125. [Google Scholar] [CrossRef]
- Li, S.-H.; Tian, H.-B.; Zhao, H.-J.; Chen, L.-H.; Cui, L.-Q. The acute effects of grape polyphenols supplementation on endothelial function in adults: Meta-analyses of controlled trials. PLoS ONE 2013, 8, e69818. [Google Scholar] [CrossRef]
- Clifton, P.M. Effect of grape seed extract and quercetin on cardiovascular and endothelial parameters in high-risk subjects. J. Biomed. Biotechnol. 2004, 2004, 272–278. [Google Scholar] [CrossRef] [Green Version]
- Barona, J.; Aristizabal, J.C.; Blesso, C.N.; Volek, J.S.; Fernandez, M.L. Grape polyphenols reduce blood pressure and increase flow-mediated vasodilation in men with metabolic syndrome. J. Nutr. 2012, 142, 1626–1632. [Google Scholar] [CrossRef] [Green Version]
- Akbari, M.; Tamtaji, O.R.; Lankarani, K.B.; Tabrizi, R.; Dadgostar, E.; Kolahdooz, F.; Jamilian, M.; Mirzaei, H.; Asemi, Z. The effects of resveratrol supplementation on endothelial function and blood pressures among patients with metabolic syndrome and related disorders: A systematic review and meta-analysis of randomized controlled trials. High Blood Press. Cardiovasc. Prev. 2019, 26, 305–319. [Google Scholar] [CrossRef]
- Annunziata, G.; Jimenez-García, M.; Tejada, S.; Moranta, D.; Arnone, A.; Ciampaglia, R.; Tenore, G.C.; Sureda, A.; Novellino, E.; Capó, X. Grape polyphenols ameliorate muscle decline reducing oxidative stress and oxidative damage in aged rats. Nutrients 2020, 12, 1280. [Google Scholar] [CrossRef]
- Cesarone, M.; Belcaro, G.; Carratelli, M.; Cornelli, U. A simple test to monitor oxidative stress. Int. Angiol. 1999, 18, 127. [Google Scholar]
- Alberti, A.; Bolognini, L.; Macciantelli, D.; Caratelli, M. The radical cation of N, N-diethyl-para-phenylendiamine: A possible indicator of oxidative stress in biological samples. Res. Chem. Intermed. 2000, 26, 253–267. [Google Scholar] [CrossRef]
- Trotti, R.; Carratelli, M.; Barbieri, M.; Micieli, G.; Bosone, D.; Rondanelli, M.; Bo, P. Oxidative stress and a thrombophilic condition in alcoholics without severe liver disease. Haematologica 2001, 86, 85–91. [Google Scholar]
- Gerardi, G.; Usberti, M.; Martini, G.; Albertini, A.; Sugherini, L.; Pompella, A.; Di Lorenzo, D. Plasma total antioxidant capacity in hemodialyzed patients and its relationships to other biomarkers of oxidative stress and lipid peroxidation. Clin. Chem. Lab. Med. 2002, 40, 104–110. [Google Scholar] [CrossRef]
- Zhu, Q.Y.; Huang, Y.; Tsang, D.; Chen, Z.-Y. Regeneration of α-tocopherol in human low-density lipoprotein by green tea catechin. J. Agric. Food Chem. 1999, 47, 2020–2025. [Google Scholar] [CrossRef] [PubMed]
- Lupoli, R.; Ciciola, P.; Costabile, G.; Giacco, R.; Minno, M.N.D.D.; Capaldo, B. Impact of Grape Products on Lipid Profile: A Meta-Analysis of Randomized Controlled Studies. J. Clin. Med. 2020, 9, 313. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Frankel, E.; German, J.; Kinsella, J.; Parks, E.; Kanner, J. Inhibition of oxidation of human low-density lipoprotein by phenolic substances in red wine. Lancet 1993, 341, 454–457. [Google Scholar] [CrossRef]
- Macri, A.; Scanarotti, C.; Bassi, A.M.; Giuffrida, S.; Sangalli, G.; Traverso, C.E.; Iester, M. Evaluation of oxidative stress levels in the conjunctival epithelium of patients with or without dry eye, and dry eye patients treated with preservative-free hyaluronic acid 0.15% and vitamin B12 eye drops. Graefe’s Arch. Clin. Exp. Ophthalmol. 2015, 253, 425–430. [Google Scholar] [CrossRef] [PubMed]
- Mancini, S.; Mariani, F.; Sena, P.; Benincasa, M.; Roncucci, L. Myeloperoxidase expression in human colonic mucosa is related to systemic oxidative balance in healthy subjects. Redox Rep. 2017, 22, 399–407. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Week | Control | Taurisolo® 10 mg/Kg/die | Taurisolo® 20 mg/Kg/die | Captopril 20 mg/Kg/die |
| 0 | 184 ± 6 | 178 ± 7 | 185 ± 4 | 194 ± 2 |
| 1 | 212 ± 4 | 202 ± 3 | 192 ± 3 ** | 193 ± 2 ** |
| 2 | 233 ± 5 | 223 ± 4 | 205 ± 2 *** | 191 ± 3 *** |
| 3 | 232 ± 3 | 224 ± 4 | 200 ± 2 *** | 190 ± 2 *** |
| 4 | 234 ± 2 | 225 ± 1 | 200 ± 2 *** | 189 ± 3 *** |
| Variable | Value ± SD |
|---|---|
| Demographic characteristics | |
| Subjects (No) | 20 |
| Age (years) | 24.46 ± 2.99 |
| Male sex (No (%)) | 11 (55%) |
| White ethnicity (No (%)) | 20 (100%) |
| Smokers (No (%)) | 7 (35%) |
| Regular physical activity (No (%)) | 11 (55%) |
| Anthropometric characteristics | |
| Weight (Kg) | 66.03 ± 11.79 |
| Height (cm) | 1.69 ± 0.10 |
| BMI (Kg/m2) | 22.30 ± 4.87 |
| WC (cm) | 76.82 ± 11.52 |
| HC (cm) | 98.09 ± 5.37 |
| WHR | 0.72 ± 0.25 |
| Serum parameters | |
| Glycaemia (mg/dL) | 66.78 ± 12.71 |
| TC (mg/dL) | 145.85 ± 32.82 |
| TG (mg/dL) | 51.92 ± 16.86 |
| HDL-c (mg/dL) | 49.22 ± 12.14 |
| LDL-c (mg/dL) | 84.05 ± 34.00 |
| OxLDL (µEq/L) | 1031.15 ± 676.50 |
| D-ROMs (UCARR) | 259.33 ± 104.94 |
| Endothelial function | |
| FMD (%) | 6.48 ± 3.28 |
| RHI | 3.26 ± 1.24 |
| Parameters | Taurisolo® (n = 10) | Placebo (n = 10) | p-Value | ||||
|---|---|---|---|---|---|---|---|
| Initial | Final | Initial | Final | Initial (Taurisolo® vs. Placebo) | Taurisolo® (Initial vs. Final) | Placebo (Initial vs. Final) | |
| Age (years) | 24.17 ± 0.98 | - | 24.71 ± 4.11 | - | 0.757 | - | - |
| Male sex (No (%)) | 6 (60%) | - | 5 (50%) | - | χ2 = 0.202; p = 0.653 | - | - |
| Smokers (No (%)) | 4 (40%) | - | 3 (30%) | - | χ2 = 0.219; p = 0.639 | - | - |
| Regular physical activity (No (%)) | 5 (50%) | - | 6 (60%) | χ2 = 0.202; p = 0.653 | - | - | |
| Weight (Kg) | 67.53 ± 11.82 | 67.33 ± 11.23 | 64.52 ± 12.67 | 64.35 ± 13.13 | 0.679 | 0.672 | 0.602 |
| Height (cm) | 1.67 ± 0.10 | - | 1.71 ± 0.11 | - | 0.499 | - | - |
| BMI (Kg/m2) | 24.24 ± 2.59 | 24.19 ± 2.42 | 21.97 ± 2.26 | 21.89 ± 2.39 | 0.136 | 0.738 | 0.524 |
| WC (cm) | 78.75 ± 15.15 | 78.38 ± 15.19 | 74.50 ± 5.72 | 74.64 ± 5.06 | 0.570 | 0.188 | 0.744 |
| HC (cm) | 101.92 ± 2.15 | 101.60 ± 2.54 | 93.50 ± 4.24 | 93.28 ± 4.25 | 0.002 | 0.242 | 0.189 |
| WHR | 0.77 ± 0.14 | 0.77 ± 0.13 | 0.80 ± 0.05 | 0.80 ± 0.05 | 0.716 | 0.475 | 0.403 |
| Glycaemia (mg/dL) | 63.32 ± 11.55 | 74.68 ± 5.82 | 69.76 ± 13.77 | 72.66 ± 6.50 | 0.386 | 0.234 | 0.420 |
| TC (mg/dL) | 143.67 ± 39.88 | 154.25 ± 14.48 | 147.71 ± 28.63 | 142.57 ± 18.87 | 0.835 | 0.055 | 0.318 |
| TG (mg/dL) | 56.83 ± 17.88 | 52.25 ± 27.28 | 47.71 ± 16.04 | 51.57 ± 18.83 | 0.353 | 0.474 | 0.125 |
| HDL-c (mg/dL) | 43.63 ± 5.77 | 53.75 ± 6.55 | 54.01 ± 14.46 | 51.56 ± 12.95 | 0.129 | 0.062 | 0.122 |
| LDL-c (mg/dL) | 88.67 ± 37.61 | 90.05 ± 20.73 | 80.10 ± 33.06 | 80.70 ± 23.09 | 0.670 | 0.744 | 0.910 |
| oxLDL (µEq/L) | 1005.00 ± 389.81 | 639.50 ± 188.74 | 1053.57 ± 887.36 | 1051.43 ± 889.95 | 0.904 | 0.043 | 0.945 |
| D-ROMs (UCARR) | 297.08 ± 84.06 | 227.75 ± 20.01 | 226.97 ± 116.16 | 227.11 ± 88.26 | 0.246 | 0.008 | 0.995 |
| FMD (%) | 6.67 ± 4.56 | 12.61 ± 2.92 | 6.31 ± 2.03 | 6.24 ± 1.62 | 0.852 | 0.019 | 0.763 |
| RHI | 2.95 ± 1.10 | 4.15 ± 1.03 | 3.63 ± 1.43 | 3.69 ± 1.60 | 0.394 | 0.079 | 0.920 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martelli, A.; Flori, L.; Gorica, E.; Piragine, E.; Saviano, A.; Annunziata, G.; Di Minno, M.N.D.; Ciampaglia, R.; Calcaterra, I.; Maione, F.; et al. Vascular Effects of the Polyphenolic Nutraceutical Supplement Taurisolo®: Focus on the Protection of the Endothelial Function. Nutrients 2021, 13, 1540. https://doi.org/10.3390/nu13051540
Martelli A, Flori L, Gorica E, Piragine E, Saviano A, Annunziata G, Di Minno MND, Ciampaglia R, Calcaterra I, Maione F, et al. Vascular Effects of the Polyphenolic Nutraceutical Supplement Taurisolo®: Focus on the Protection of the Endothelial Function. Nutrients. 2021; 13(5):1540. https://doi.org/10.3390/nu13051540
Chicago/Turabian StyleMartelli, Alma, Lorenzo Flori, Era Gorica, Eugenia Piragine, Anella Saviano, Giuseppe Annunziata, Matteo Nicola Dario Di Minno, Roberto Ciampaglia, Ilenia Calcaterra, Francesco Maione, and et al. 2021. "Vascular Effects of the Polyphenolic Nutraceutical Supplement Taurisolo®: Focus on the Protection of the Endothelial Function" Nutrients 13, no. 5: 1540. https://doi.org/10.3390/nu13051540











