Resting Energy Expenditure Is Not Altered in Children and Adolescents with Obesity. Effect of Age and Gender and Association with Serum Leptin Levels
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Selection and Study Design
2.2. Anthropometric Measurements and Resting Energy Expenditure
2.3. Blood Analyses
2.4. Statistical Analysis
3. Results
3.1. Clinical Characteristics of the Cohort
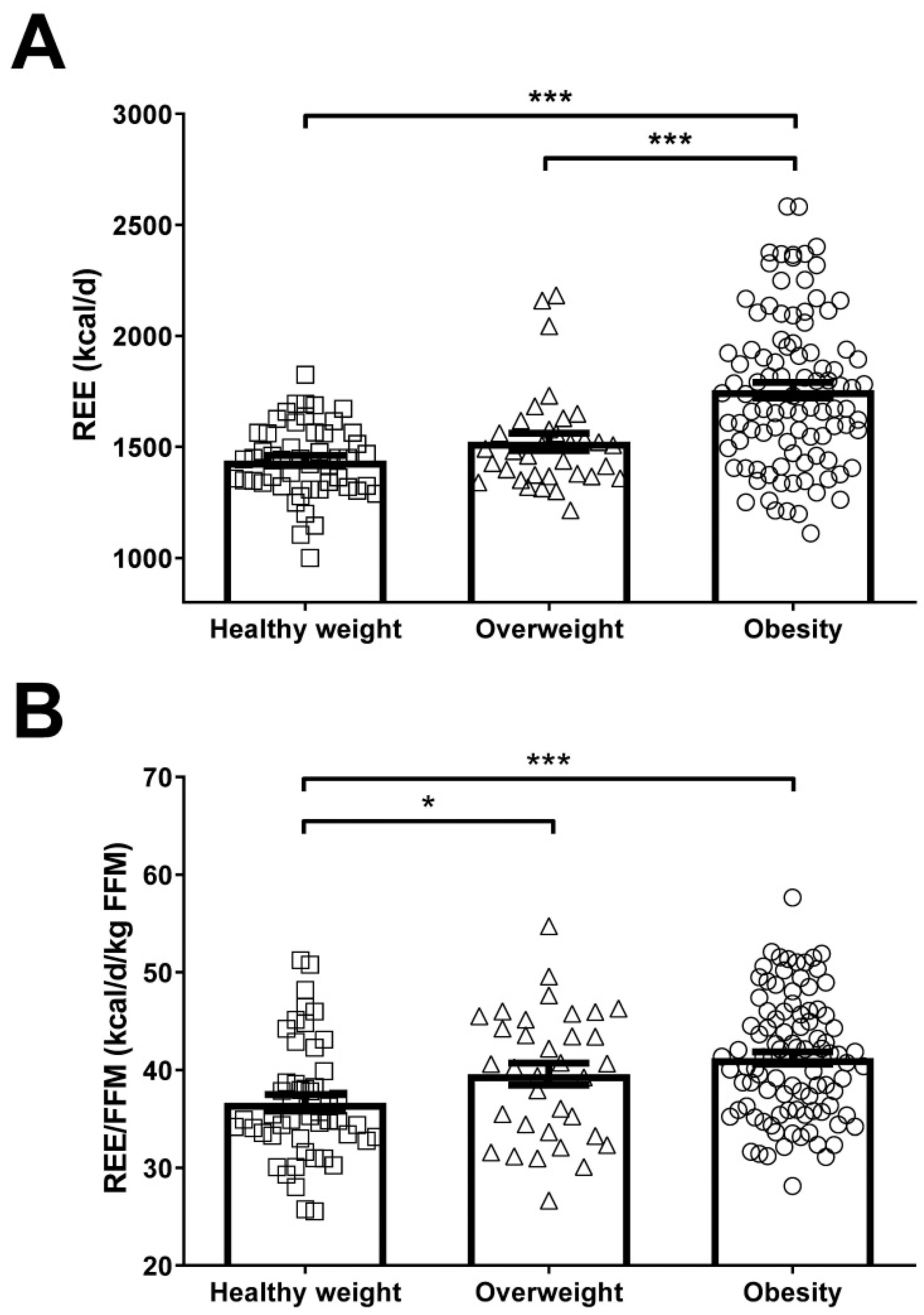
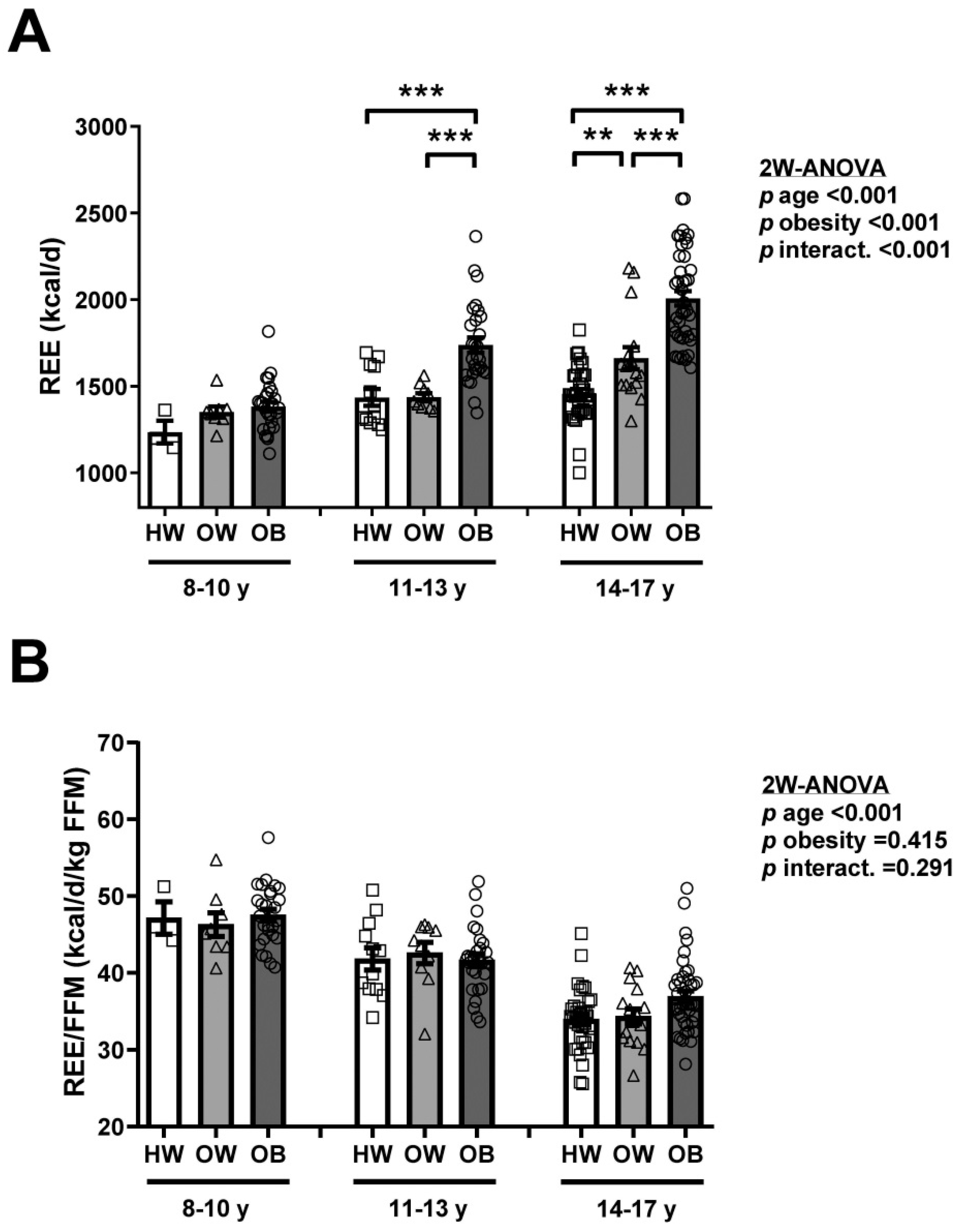
3.2. Obesity Is Associated with Increased REE, but Not REE/FFM
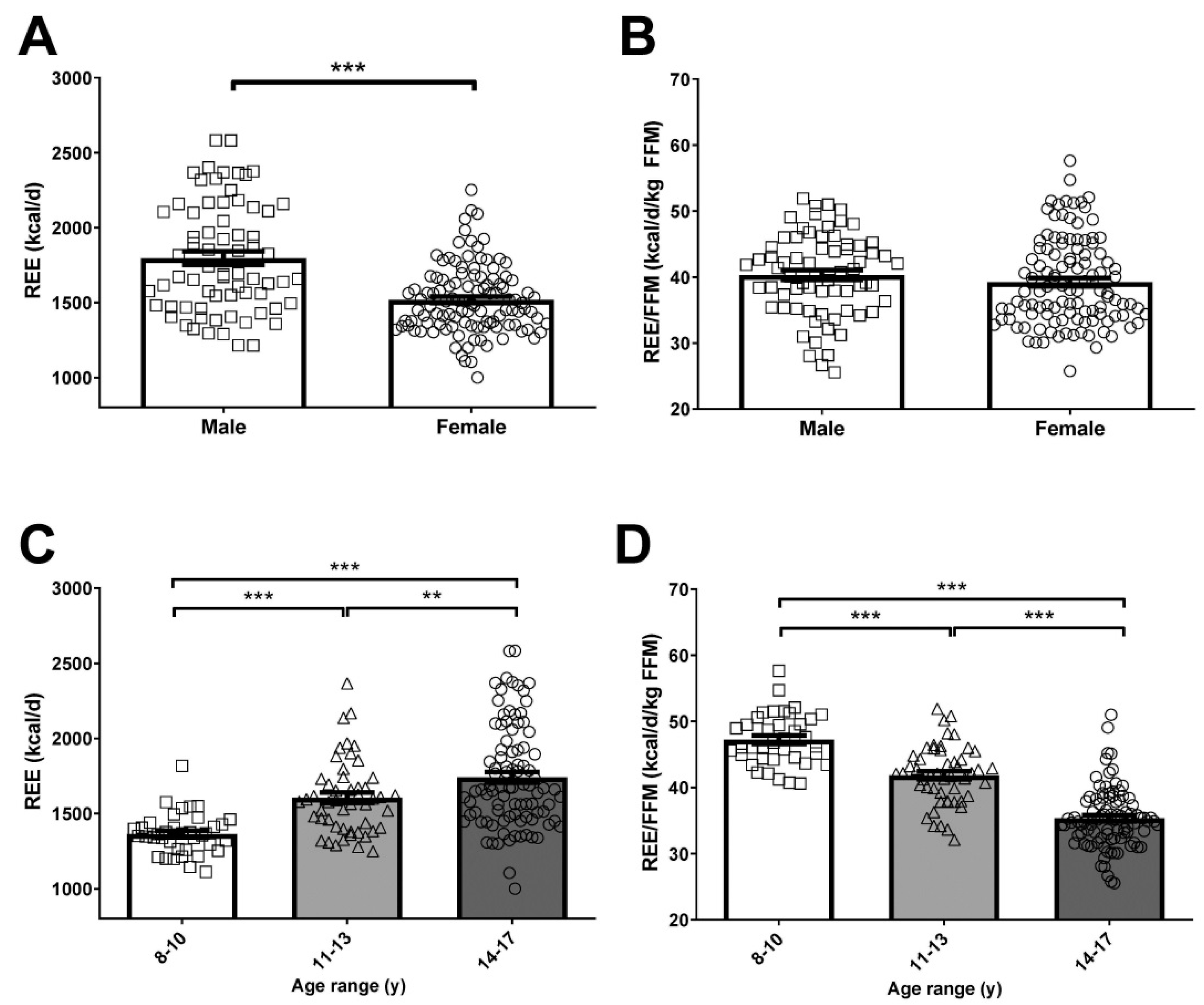
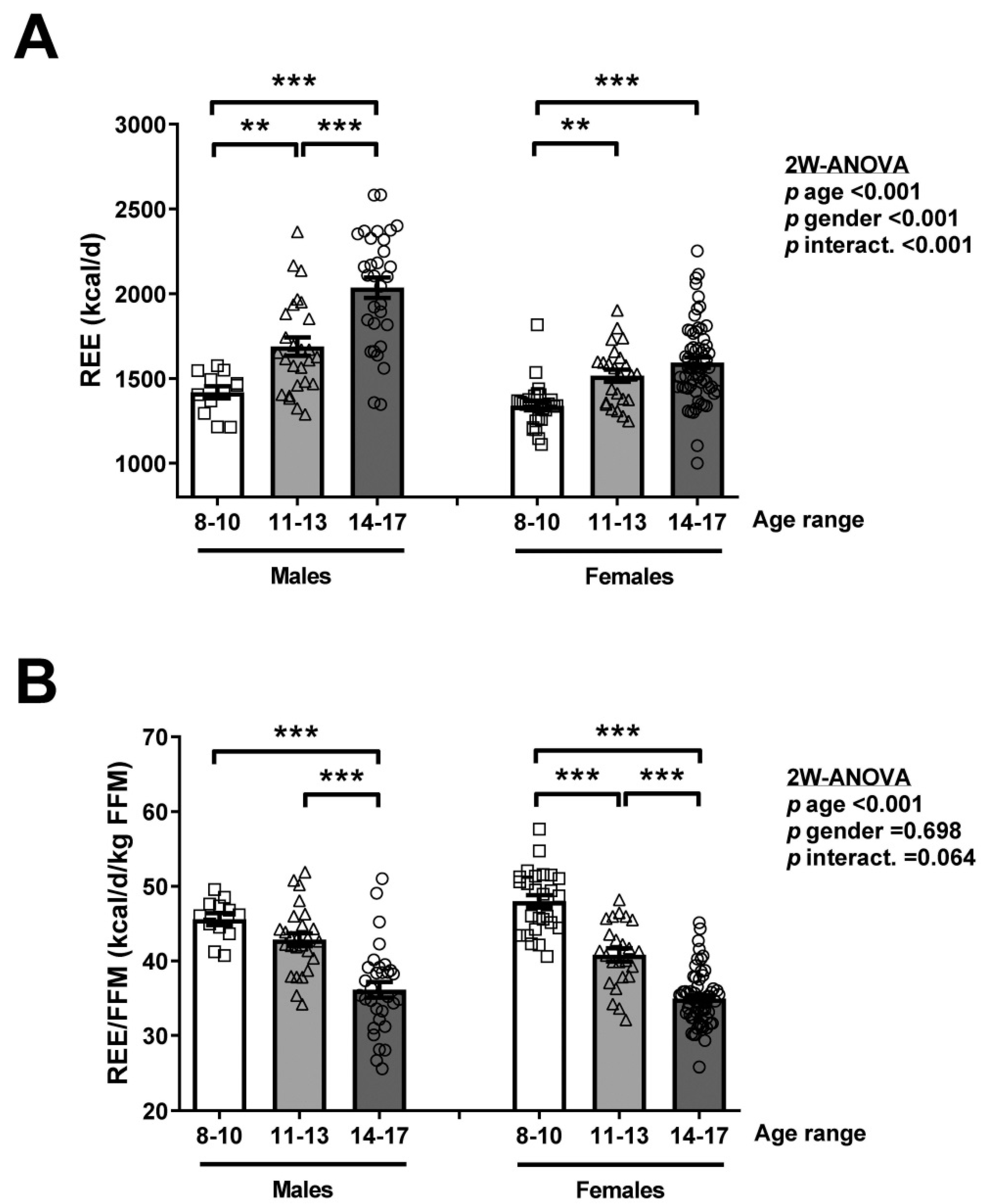
3.3. Age, but Not Gender, Influences REE/FFM in Children and Adolescents
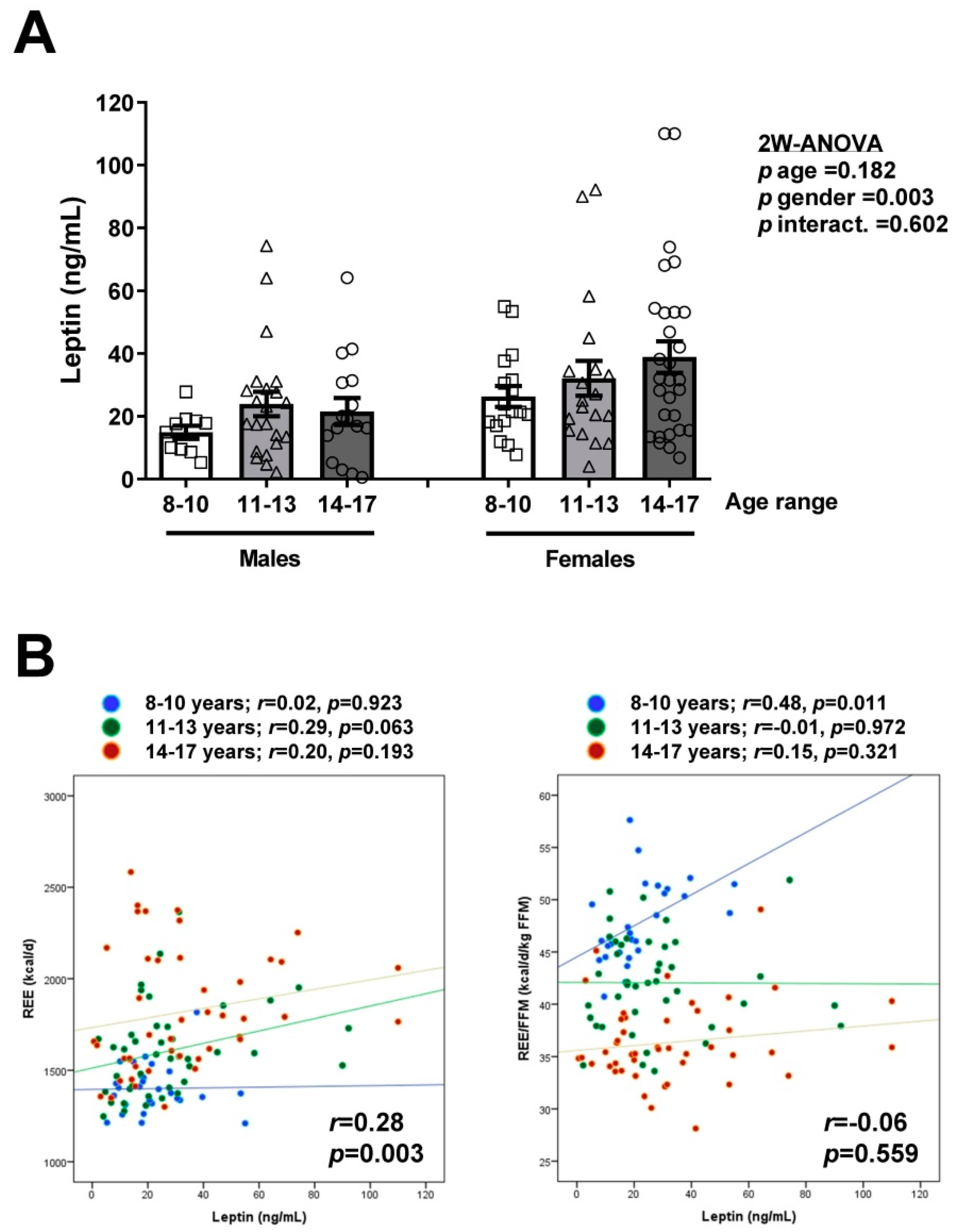
3.4. Association between Serum Leptin Concentrations and REE/FFM in Children and Adolescents
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- The GBD 2015 Obesity Collaborators. Health effects of overweight and obesity in 195 countries over 25 years. N. Engl. J. Med. 2017, 377, 13–27. [Google Scholar] [CrossRef] [PubMed]
- Skinner, A.C.; Ravanbakht, S.N.; Skelton, J.A.; Perrin, E.M.; Armstrong, S.C. Prevalence of Obesity and Severe Obesity in US Children, 1999–2016. Pediatrics 2018, 141, e20173459. [Google Scholar] [CrossRef] [PubMed]
- Ogden, C.L.; Fryar, C.D.; Hales, C.M.; Carroll, M.D.; Aoki, Y.; Freedman, D.S. Differences in Obesity Prevalence by Demographics and Urbanization in US Children and Adolescents, 2013–2016. JAMA 2018, 319, 2410–2418. [Google Scholar] [CrossRef] [PubMed]
- Garrido-Miguel, M.; Cavero-Redondo, I.; Alvarez-Bueno, C.; Rodriguez-Artalejo, F.; Moreno, L.A.; Ruiz, J.R.; Ahrens, W.; Martinez-Vizcaino, V. Prevalence and trends of overweight and obesity in european children from 1999 to 2016: A systematic review and meta-analysis. JAMA Pediatr. 2019, 173, e192430. [Google Scholar] [CrossRef]
- Weiss, R.; Dziura, J.; Burgert, T.S.; Tamborlane, W.V.; Taksali, S.E.; Yeckel, C.W.; Allen, K.; Lopes, M.; Savoye, M.; Morrison, J.; et al. Obesity and the Metabolic Syndrome in Children and Adolescents. N. Engl. J. Med. 2004, 350, 2362–2374. [Google Scholar] [CrossRef]
- Koren, D.; Chirinos, J.A.; Katz, L.E.L.; Mohler, E.R.; Gallagher, P.R.; Mitchell, G.F.; Marcus, C.L. Interrelationships between obesity, obstructive sleep apnea syndrome and cardiovascular risk in obese adolescents. Int. J. Obes. 2015, 39, 1086–1093. [Google Scholar] [CrossRef]
- Furer, A.; Afek, A.; Sommer, A.; Keinan-Boker, L.; Derazne, E.; Levi, Z.; Tzur, D.; Tiosano, S.; Shina, A.; Glick, Y.; et al. Adolescent obesity and midlife cancer risk: A population-based cohort study of 2.3 million adolescents in Israel. Lancet Diabetes Endocrinol. 2020, 8, 216–225. [Google Scholar] [CrossRef]
- Caprio, M.; Santoro, N.; Weiss, R. Childhood obesity and the associated rise in cardiometabolic complications. Nat. Metab. 2020, 2, 223–232. [Google Scholar] [CrossRef]
- Bjerregaard, L.G.; Jensen, B.W.; Angquist, L.; Osler, M.; Sørensen, T.I.; Baker, J.L. Change in Overweight from Childhood to Early Adulthood and Risk of Type 2 Diabetes. N. Engl. J. Med. 2018, 378, 1302–1312. [Google Scholar] [CrossRef]
- Bjerregaard, L.G.; Adelborg, K.; Baker, J.L. Change in body mass index from childhood onwards and risk of adult cardiovascular disease. Trends Cardiovasc. Med. 2020, 30, 39–45. [Google Scholar] [CrossRef]
- Bray, G.A.; Frühbeck, G.; Ryan, D.H.; Wilding, J.P.H. Management of obesity. Lancet 2016, 387, 1947–1956. [Google Scholar] [CrossRef]
- Soares, M.J.; Müller, M.J. Resting energy expenditure and body composition: Critical aspects for clinical nutrition. Eur. J. Clin. Nutr. 2018, 72, 1208–1214. [Google Scholar] [CrossRef] [PubMed]
- Hall, K.D.; Heymsfield, S.B.; Kemnitz, J.W.; Klein, S.; Schoeller, D.A.; Speakman, J.R. Energy balance and its components: Implications for body weight regulation. Am. J. Clin. Nutr. 2012, 95, 989–994. [Google Scholar] [CrossRef] [PubMed]
- Frühbeck, G. Does a NEAT difference in energy expenditure lead to obesity? Lancet 2005, 366, 615–616. [Google Scholar] [CrossRef]
- Kenny, G.P.; Notley, S.R.; Gagnon, D. Direct calorimetry: A brief historical review of its use in the study of human metabolism and thermoregulation. Eur. J. Appl. Physiol. 2017, 117, 1765–1785. [Google Scholar] [CrossRef]
- Westerterp, K.R. Doubly labelled water assessment of energy expenditure: Principle, practice, and promise. Eur. J. Appl. Physiol. 2017, 117, 1277–1285. [Google Scholar] [CrossRef]
- Delsoglio, M.; Achamrah, N.; Berger, M.M.; Pichard, C. Indirect Calorimetry in Clinical Practice. J. Clin. Med. 2019, 8, 1387. [Google Scholar] [CrossRef] [PubMed]
- Hopkins, M.; Blundell, J.E. Energy balance, body composition, sedentariness and appetite regulation: Pathways to obesity. Clin. Sci. 2016, 130, 1615–1628. [Google Scholar] [CrossRef]
- Carneiro, I.P.; Elliott, S.A.; Siervo, M.; Padwal, R.; Bertoli, S.; Battezzati, A.; Prado, C.M. Is Obesity Associated with Altered Energy Expenditure? Adv. Nutr. 2016, 7, 476–487. [Google Scholar] [CrossRef]
- Bandini, L.G.; Schoeller, D.A.; Dietz, W.H. Energy Expenditure in Obese and Nonobese Adolescents. Pediatr. Res. 1990, 27, 198–202. [Google Scholar] [CrossRef]
- Goran, M.I.; Treuth, M.S. Energy expenditure, physical activity, and obesity in children. Pediatr. Clin. N. Am. 2001, 48, 931–953. [Google Scholar] [CrossRef]
- Salbe, A.D.; Nicolson, M.; Ravussin, E. Total energy expenditure and the level of physical activity correlate with plasma leptin concentrations in five-year-old children. J. Clin. Investig. 1997, 99, 592–595. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Butte, N.F.; Puyau, M.R.; Vohra, F.A.; Adolph, A.L.; Mehta, N.R.; Zakeri, I. Body Size, Body Composition, and Metabolic Profile Explain Higher Energy Expenditure in Overweight Children. J. Nutr. 2007, 137, 2660–2667. [Google Scholar] [CrossRef] [PubMed]
- Ravussin, E.; Burnand, B.; Schutz, Y.; Jéquier, E. Twenty-four-hour energy expenditure and resting metabolic rate in obese, moderately obese, and control subjects. Am. J. Clin. Nutr. 1982, 35, 566–573. [Google Scholar] [CrossRef] [PubMed]
- Prentice, A.M.; Black, A.E.; Coward, W.A.; Davies, H.L.; Goldberg, G.R.; Murgatroyd, P.R.; Ashford, J.; Sawyer, M.; Whitehead, R.G. High levels of energy expenditure in obese women. BMJ 1986, 292, 983–987. [Google Scholar] [CrossRef] [PubMed]
- Verga, S.; Buscemi, S.; Caimi, G. Resting energy expenditure and body composition in morbidly obese, obese and control subjects. Acta Diabetol. 1994, 31, 47–51. [Google Scholar] [CrossRef] [PubMed]
- Dal, U.; Erdoğan, A.T.; Cureoglu, A.; Beydağı, H.; Beydagi, H. Resting Energy Expenditure in Normal-Weight and Overweight/Obese Subjects Was Similar Despite Elevated Sympathovagal Balance. Obes. Facts 2012, 5, 776–783. [Google Scholar] [CrossRef]
- Weijs, P.J.; VanSant, G.A. Validity of predictive equations for resting energy expenditure in Belgian normal weight to morbid obese women. Clin. Nutr. 2010, 29, 347–351. [Google Scholar] [CrossRef]
- Frühbeck, G. Intracellular signalling pathways activated by leptin. Biochem. J. 2005, 393, 7–20. [Google Scholar] [CrossRef]
- Blüher, M.; Mantzoros, C.S. From leptin to other adipokines in health and disease: Facts and expectations at the beginning of the 21st century. Metabolism 2015, 64, 131–145. [Google Scholar] [CrossRef]
- Gómez-Ambrosi, J.; Salvador, J.; Silva, C.; Pastor, C.; Rotellar, F.; Gil, M.J.; Cienfuegos, J.A.; Frühbeck, G. Increased cardiovascular risk markers in obesity are associated with body adiposity: Role of leptin. Thromb. Haemost. 2006, 95, 991–996. [Google Scholar] [CrossRef] [PubMed]
- Könner, A.C.; Brüning, J.C. Selective Insulin and Leptin Resistance in Metabolic Disorders. Cell Metab. 2012, 16, 144–152. [Google Scholar] [CrossRef]
- Jørgensen, J.O.; Vahl, N.; Dall, R.; Christiansen, J.S. Resting metabolic rate in healthy adults: Relation to growth hormone status and leptin levels. Metabolism 1998, 47, 1134–1139. [Google Scholar] [CrossRef]
- Bi, X.; Loo, Y.T.; Henry, C.J. Does circulating leptin play a role in energy expenditure? Nutrition 2019, 60, 6–10. [Google Scholar] [CrossRef]
- Kennedy, A.; Gettys, T.W.; Watson, P.; Wallace, P.; Ganaway, E.; Pan, Q.; Garvey, W.T. The Metabolic Significance of Leptin in Humans: Gender-Based Differences in Relationship to Adiposity, Insulin Sensitivity, and Energy Expenditure. J. Clin. Endocrinol. Metab. 1997, 82, 1293–1300. [Google Scholar] [CrossRef]
- Johnstone, A.M.; Murison, S.D.; Duncan, J.S.; Rance, K.A.; Speakman, J.R. Factors influencing variation in basal metabolic rate include fat-free mass, fat mass, age, and circulating thyroxine but not sex, circulating leptin, or triiodothyronine. Am. J. Clin. Nutr. 2005, 82, 941–948. [Google Scholar] [CrossRef]
- Dulloo, A.G.; Stock, M.J.; Solinas, G.; Boss, O.; Montani, J.P.; Seydoux, J. Leptin directly stimulates thermogenesis in skeletal muscle. FEBS Lett. 2002, 515, 109–113. [Google Scholar] [CrossRef]
- Pandit, R.; Beerens, S.; Adan, R.A.H. Role of leptin in energy expenditure: The hypothalamic perspective. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2017, 312, R938–R947. [Google Scholar] [CrossRef]
- Caron, A.; Lee, S.; Elmquist, J.K.; Gautron, L. Leptin and brain-adipose crosstalks. Nat. Rev. Neurosci. 2018, 19, 153–165. [Google Scholar] [CrossRef]
- Fischer, A.W.; Cannon, B.; Nedergaard, J. Leptin: Is it thermogenic? Endocr. Rev. 2020, 41, 232–260. [Google Scholar] [CrossRef] [PubMed]
- Laessle, R.G.; Wurmser, H.; Pirke, K.M. A Comparison of Resting Metabolic Rate, Self-Rated Food Intake, Growth Hormone, and Insulin Levels in Obese and Nonobese Preadolescents. Physiol. Behav. 1997, 61, 725–729. [Google Scholar] [CrossRef]
- Treuth, M.; Figueroa-Colon, R.; Hunter, G.; Weinsier, R.; Butte, N.; Goran, M. Energy expenditure and physical fitness in overweight vs non-overweight prepubertal girls. Int. J. Obes. 1998, 22, 440–447. [Google Scholar] [CrossRef] [PubMed]
- Ekelund, U.; Aman, J.; Yngve, A.; Renman, C.; Westerterp, K.; Sjöström, M. Physical activity but not energy expenditure is reduced in obese adolescents: A case-control study. Am. J. Clin. Nutr. 2002, 76, 935–941. [Google Scholar] [CrossRef] [PubMed]
- Ekelund, U.; Franks, P.W.; Wareham, N.J.; Åman, J. Oxygen Uptakes Adjusted for Body Composition in Normal-Weight and Obese Adolescents. Obes. Res. 2004, 12, 513–520. [Google Scholar] [CrossRef] [PubMed]
- Bitar, A.; Fellmann, N.; Vernet, J.; Coudert, J.; Vermorel, M. Variations and determinants of energy expenditure as measured by whole-body indirect calorimetry during puberty and adolescence. Am. J. Clin. Nutr. 1999, 69, 1209–1216. [Google Scholar] [CrossRef]
- Barlow, S.E.; Expert, C. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: Summary report. Pediatrics 2007, 120 (Suppl. S4), S164–S192. [Google Scholar] [CrossRef]
- Fields, D.A.; Higgins, P.B.; Radley, D. Air-displacement plethysmography: Here to stay. Curr. Opin. Clin. Nutr. Metab. Care 2005, 8, 624–629. [Google Scholar] [CrossRef]
- Añón-Hidalgo, J.; Catalán, V.; Rodríguez, A.; Ramírez, B.; Idoate-Bayón, A.; Silva, C.; Mugueta, C.; Galofré, J.C.; Salvador, J.; Frühbeck, G.; et al. Circulating Concentrations of GDF11 are Positively Associated with TSH Levels in Humans. J. Clin. Med. 2019, 8, 878. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Ambrosi, J.; Rodríguez, A.; Catalán, V.; Ramírez, B.; Silva, C.; Rotellar, F.; Gil, M.J.; Salvador, J.; Frühbeck, G. Serum retinol-binding protein 4 is not increased in obesity or obesity-associated type 2 diabetes mellitus, but is reduced after relevant reductions in body fat following gastric bypass. Clin. Endocrinol. 2008, 69, 208–215. [Google Scholar] [CrossRef]
- Bogardus, C.; Lillioja, S.; Ravussin, E.; Abbott, W.; Zawadzki, J.K.; Young, A.; Knowler, W.C.; Jacobowitz, R.; Moll, P.P. Familial Dependence of the Resting Metabolic Rate. N. Engl. J. Med. 1986, 315, 96–100. [Google Scholar] [CrossRef]
- Weinsier, R.L.; Schutz, Y.; Bracco, D. Reexamination of the relationship of resting metabolic rate to fat-free mass and to the metabolically active components of fat-free mass in humans. Am. J. Clin. Nutr. 1992, 55, 790–794. [Google Scholar] [CrossRef]
- Goran, M.I.; Kaskoun, M.; Johnson, R. Determinants of resting energy expenditure in young children. J. Pediatr. 1994, 125, 362–367. [Google Scholar] [CrossRef]
- Müller, M.J.; Geisler, C.; Hübers, M.; Pourhassan, M.; Braun, W.; Bosy-Westphal, A. Normalizing resting energy expenditure across the life course in humans: Challenges and hopes. Eur. J. Clin. Nutr. 2018, 72, 628–637. [Google Scholar] [CrossRef] [PubMed]
- Elberg, J.; McDuffie, J.R.; Sebring, N.G.; Salaita, C.; Keil, M.; Robotham, D.; Reynolds, J.C.; Yanovski, J.A. Comparison of methods to assess change in children’s body composition123. Am. J. Clin. Nutr. 2004, 80, 64–69. [Google Scholar] [CrossRef] [PubMed]
- Wells, J.; Fuller, N. Precision of measurement and body size in whole-body air-displacement plethysmography. Int. J. Obes. 2001, 25, 1161–1167. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Vermorel, M.; Lazzer, S.; Bitar, A.; Ribeyre, J.; Montaurier, C.; Fellmann, N.; Coudert, J.; Meyer, M.; Boirie, Y. Contributing factors and variability of energy expenditure in non-obese, obese, and post-obese adolescents. Reprod. Nutr. Dev. 2005, 45, 129–142. [Google Scholar] [CrossRef][Green Version]
- Oria, H.E.; Carrasquilla, C.; Cunningham, P.; Hess, D.S.; Johnell, P.; Kligman, M.D.; Moorehead, M.K.; Papadia, F.S.; Renquist, K.E.; American Society for Bariatric Surgery Standards Committee; et al. Guidelines for weight calculations and follow-up in bariatric surgery. Surg. Obes. Relat. Dis. 2005, 1, 67–68. [Google Scholar] [CrossRef]
- Molnár, D.; Schutz, Y. Fat oxidation in nonobese and obese adolescents: Effect of body composition and pubertal development. J. Pediatr. 1998, 132, 98–104. [Google Scholar] [CrossRef]
- Rodríguez, G.; Moreno, L.A.; Sarría, A.; Pineda, I.; Fleta, J.; Pérez-González, J.M.; Bueno, M. Determinants of resting energy expenditure in obese and non-obese children and adolescents. J. Physiol. Biochem. 2002, 58, 9–15. [Google Scholar] [CrossRef]
- Henry, C.; Dyer, S.; Ghusain-Choueiri, A. New equations to estimate basal metabolic rate in children aged 10–15 years. Eur. J. Clin. Nutr. 1999, 53, 134–142. [Google Scholar] [CrossRef]
- Lazzer, S.; Patrizi, A.; De Col, A.; Saezza, A.; Sartorio, A. Prediction of basal metabolic rate in obese children and adolescents considering pubertal stages and anthropometric characteristics or body composition. Eur. J. Clin. Nutr. 2014, 68, 695–699. [Google Scholar] [CrossRef] [PubMed]
- Ribeyre, J.; Fellmann, N.; Montaurier, C.; Delaître, M.; Vernet, J.; Coudert, J.; Vermorel, M. Daily energy expenditure and its main components as measured by whole-body indirect calorimetry in athletic and non-athletic adolescents. Br. J. Nutr. 2000, 83, 355–362. [Google Scholar]
- Gazzaniga, J.M.; Burns, T.L. Relationship between diet composition and body fatness, with adjustment for resting energy expenditure and physical activity, in preadolescent children. Am. J. Clin. Nutr. 1993, 58, 21–28. [Google Scholar] [CrossRef]
- Grund, A.; Vollbrecht, H.; Frandsen, W.; Krause, H.; Siewers, M.; Rieckert, H.; Müller, M. No effect of gender on different components of daily energy expenditure in free living prepubertal children. Int. J. Obes. 2000, 24, 299–305. [Google Scholar] [CrossRef][Green Version]
- Cheng, Y.; Yang, X.; Na, L.-X.; Li, Y.; Sun, C.-H. Gender- and Age-Specific REE and REE/FFM Distributions in Healthy Chinese Adults. Nutrients 2016, 8, 536. [Google Scholar] [CrossRef] [PubMed]
- Roberts, S.B.; Rosenberg, I. Nutrition and Aging: Changes in the Regulation of Energy Metabolism with Aging. Physiol. Rev. 2006, 86, 651–667. [Google Scholar] [CrossRef] [PubMed]
- Maffeis, C.; Schutz, Y.; Micciolo, R.; Zoccante, L.; Pinelli, L. Resting metabolic rate in six- to ten-year-old obese and nonobese children. J. Pediatr. 1993, 122, 556–562. [Google Scholar] [CrossRef]
- Molnár, D.; Schutz, Y. The effect of obesity, age, puberty and gender on resting metabolic rate in children and adolescents. Eur. J. Nucl. Med. Mol. Imaging 1997, 156, 376–381. [Google Scholar] [CrossRef] [PubMed]
- Nagy, T.R.; Gower, B.A.; Trowbridge, C.A.; Dezenberg, C.; Shewchuk, R.M.; Goran, M.I. Effects of Gender, Ethnicity, Body Composition, and Fat Distribution on Serum Leptin Concentrations in Children. J. Clin. Endocrinol. Metab. 1997, 82, 2148–2152. [Google Scholar] [CrossRef]
- Ten, S.; Bhangoo, A.; Ramchandani, N.; Mueller, C.; Vogiatzi, M.; New, M.; Lesser, M.; MacLaren, N. Resting Energy Expenditure in Insulin Resistance Falls with Decompensation of Insulin Secretion in Obese Children. J. Pediatr. Endocrinol. Metab. 2008, 21, 359–368. [Google Scholar] [CrossRef] [PubMed]
- Arslanian, S.; Suprasongsin, C.; Kalhan, S.C.; Drash, A.L.; Brna, R.; Janosky, J.E. Plasma leptin in children: Relationship to puberty, gender, body composition, insulin sensitivity, and energy expenditure. Metabolism 1998, 47, 309–312. [Google Scholar] [CrossRef]
- Haas, V.K.; Gaskin, K.J.; Kohn, M.R.; Clarke, S.D.; Müller, M.J. Different thermic effects of leptin in adolescent females with varying body fat content. Clin. Nutr. 2010, 29, 639–645. [Google Scholar] [CrossRef]
- Souza, M.S.; Cardoso, A.L.; Yasbek, P., Jr.; Faintuch, J. Aerobic endurance, energy expenditure, and serum leptin response in obese, sedentary, prepubertal children and adolescents participating in a short-term treadmill protocol. Nutrition 2004, 20, 900–904. [Google Scholar] [CrossRef]
- Chrysafi, P.; Perakakis, N.; Farr, O.M.; Stefanakis, K.; Peradze, N.; Sala-Vila, A.; Mantzoros, C.S. Leptin alters energy intake and fat mass but not energy expenditure in lean subjects. Nat. Commun. 2020, 11, 1–15. [Google Scholar] [CrossRef]
- Frühbeck, G.; Catalán, V.; Rodríguez, A.; Gómez-Ambrosi, J. Adiponectin-leptin ratio: A promising index to estimate adipose tissue dysfunction. Relation with obesity-associated cardiometabolic risk. Adipocyte 2018, 7, 57–62. [Google Scholar] [CrossRef] [PubMed]
- Hall, K.D. Modeling Metabolic Adaptations and Energy Regulation in Humans. Annu. Rev. Nutr. 2012, 32, 35–54. [Google Scholar] [CrossRef]
- Browning, M.G.; Evans, R.K. The contribution of fat-free mass to resting energy expenditure: Implications for weight loss strategies in the treatment of adolescent obesity. Int. J. Adolesc. Med. Health 2015, 27, 241–246. [Google Scholar] [CrossRef] [PubMed]
- Heymsfield, S.B.; Thomas, D.; Bosy-Westphal, A.; Shen, W.; Peterson, C.M.; Müller, M.J. Evolving concepts on adjusting human resting energy expenditure measurements for body size. Obes. Rev. 2012, 13, 1001–1014. [Google Scholar] [CrossRef] [PubMed]
| Healthy Weight | Overweight | Obesity | p | |
|---|---|---|---|---|
| n | 50 | 34 | 97 | |
| Sex, M/F | 15/35 | 8/26 | 46/51 | 0.018 |
| Age, years | 14.5 ± 0.3 | 13.2 ± 0.5 * | 13.3 ± 0.3 * | 0.002 |
| Height, cm | 161 ± 2 | 156 ± 2 | 156 ± 2 | 0.120 |
| Weight, kg | 53.5 ± 1.5 | 60.1 ± 2.5 | 75.2 ± 2.4 *,† | <0.001 |
| BMI, kg/m2 | 20.5 ± 0.3 | 24.2 ± 0.4 * | 29.9 ± 0.5 *,† | <0.001 |
| Body fat, % | 24.0 ± 1.3 | 33.3 ± 1.3 * | 40.4 ± 0.7 *,† | <0.001 |
| FFM, kg | 40.4 ± 1.2 | 40.1 ± 2.1 | 44.2 ± 1.3 | 0.083 |
| Waist circumference, cm | 74 ± 1 | 80 ± 1 * | 92 ± 1 *,† | <0.001 |
| SBP, mm Hg | 99 ± 2 | 105 ± 2 * | 110 ± 1 *,† | <0.001 |
| DBP, mm Hg | 60 ± 1 | 62 ± 1 | 67 ± 1 *,† | <0.001 |
| REE, kcal/d | 1439 ± 24 | 1523 ± 39 | 1756 ± 35 *,† | <0.001 |
| REE/FFM, kcal/d/kg | 36.6 ± 0.8 | 39.6 ± 1.1 * | 41.2 ± 0.6 * | <0.001 |
| Glucose, mg/dL | 86 ± 1 | 87 ± 1 | 89 ± 1 | 0.104 |
| Insulin, μU/mL | 11.7 ± 2.1 | 10.2 ± 1.1 | 19.8 ± 1.9 *,† | 0.006 |
| HOMA | 2.6 ± 0.5 | 2.2 ± 0.3 | 4.4 ± 0.4 *,† | 0.004 |
| Triglycerides, mg/dL | 65 ± 3 | 75 ± 6 | 89 ± 4 * | <0.001 |
| Total cholesterol, mg/dL | 159 ± 4 | 160 ± 5 | 165 ± 3 | 0.502 |
| LDL-cholesterol, mg/dL | 89 ± 4 | 91 ± 4 | 96 ± 3 | 0.347 |
| HDL-cholesterol, mg/dL | 57 ± 2 | 54 ± 2 | 51 ± 1 * | 0.019 |
| CRP, mg/L | 0.8 ± 0.2 | 1.3 ± 0.3 | 3.9 ± 1.1 *,† | <0.001 |
| TSH, µU/mL | 2.16 ± 0.20 | 2.55 ± 0.31 | 2.62 ± 0.15 | 0.273 |
| Leptin, ng/mL | 10.0 ± 1.2 | 26.0 ± 2.9 * | 35.2 ± 2.8 * | <0.001 |
| All (n = 181) | 8–10 y (n = 38) | 11–13 y (n = 50) | 14–17 y (n = 93) | |||||
|---|---|---|---|---|---|---|---|---|
| REE | REE/FFM | REE | REE/FFM | REE | REE/FFM | REE | REE/FFM | |
| Age | 0.46 | −0.74 | 0.33 | −0.44 | 0.19 | −0.45 | 0.11 | −0.07 |
| <0.001 | <0.001 | 0.042 | 0.005 | 0.194 | <0.001 | 0.285 | 0.507 | |
| Height | 0.67 | −0.76 | 0.70 | −0.57 | 0.67 | −0.50 | 0.56 | −0.36 |
| <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | |
| Weight | 0.88 | −0.44 | 0.86 | −0.37 | 0.82 | −0.26 | 0.88 | 0.15 |
| <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | 0.064 | <0.001 | 0.145 | |
| BMI | 0.73 | −0.10 | 0.63 | −0.08 | 0.64 | −0.06 | 0.74 | 0.31 |
| <0.001 | 0.187 | <0.001 | 0.652 | <0.001 | 0.676 | <0.001 | 0.002 | |
| Body fat% | 0.33 | 0.38 | 0.29 | 0.40 | 0.37 | 0.34 | 0.42 | 0.60 |
| <0.001 | <0.001 | 0.075 | 0.014 | 0.009 | 0.015 | <0.001 | <0.001 | |
| FFM | 0.83 | −0.72 | 0.82 | −0.73 | 0.83 | −0.60 | 0.80 | −0.34 |
| <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | 0.001 | |
| WC | 0.78 | −0.18 | 0.62 | −0.41 | 0.69 | 0.01 | 0.77 | 0.28 |
| <0.001 | 0.017 | <0.001 | 0.010 | <0.001 | 0.942 | <0.001 | 0.007 | |
| SBP | 0.49 | 0.05 | 0.32 | −0.13 | 0.45 | 0.03 | 0.58 | 0.26 |
| <0.001 | 0.515 | 0.059 | 0.462 | 0.001 | 0.859 | <0.001 | 0.015 | |
| DBP | 0.50 | 0.01 | 0.11 | 0.05 | 0.44 | 0.14 | 0.54 | 0.27 |
| <0.001 | 0.944 | 0.542 | 0.771 | 0.002 | 0.350 | <0.001 | 0.011 | |
| Glucose | 0.22 | 0.06 | 0.23 | 0.15 | 0.11 | −0.08 | 0.30 | 0.20 |
| 0.007 | 0.470 | 0.221 | 0.426 | 0.467 | 0.584 | 0.008 | 0.085 | |
| Insulin | 0.36 | −0.20 | 0.53 | −0.01 | 0.49 | −0.16 | 0.21 | −0.04 |
| <0.001 | 0.019 | 0.003 | 0.972 | <0.001 | 0.282 | 0.102 | 0.742 | |
| HOMA | 0.37 | −0.20 | 0.54 | 0.01 | 0.49 | −0.17 | 0.23 | −0.04 |
| <0.001 | 0.019 | 0.002 | 0.986 | <0.001 | 0.277 | 0.079 | 0.759 | |
| Triglycerides | 0.25 | 0.07 | 0.19 | −0.30 | 0.23 | 0.17 | 0.37 | 0.18 |
| 0.002 | 0.396 | 0.312 | 0.103 | 0.135 | 0.291 | <0.001 | 0.125 | |
| T. cholest. | −0.04 | 0.17 | 0.15 | −0.18 | −0.26 | 0.36 | 0.08 | 0.13 |
| 0.613 | 0.037 | 0.436 | 0.330 | 0.093 | 0.018 | 0.485 | 0.249 | |
| LDL-cholest. | 0.01 | 0.18 | 0.13 | −0.11 | −0.23 | 0.34 | 0.17 | 0.13 |
| 0.882 | 0.028 | 0.481 | 0.552 | 0.144 | 0.027 | 0.153 | 0.277 | |
| HDL-cholest. | −0.31 | 0.02 | 0.01 | −0.03 | −0.34 | 0.12 | −0.39 | −0.08 |
| <0.001 | 0.859 | 0.972 | 0.895 | 0.027 | 0.441 | <0.001 | 0.502 | |
| CRP | 0.27 | 0.35 | 0.29 | 0.18 | 0.29 | 0.43 | 0.64 | 0.49 |
| 0.038 | 0.006 | 0.266 | 0.485 | 0.145 | 0.027 | 0.005 | 0.046 | |
| TSH | 0.04 | 0.10 | 0.32 | −0.27 | 0.17 | 0.03 | 0.03 | 0.15 |
| 0.628 | 0.265 | 0.124 | 0.197 | 0.316 | 0.855 | 0.792 | 0.210 | |
| Leptin | 0.28 | −0.06 | 0.02 | 0.48 | 0.29 | −0.01 | 0.20 | 0.15 |
| 0.003 | 0.559 | 0.923 | 0.011 | 0.063 | 0.972 | 0.193 | 0.321 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zapata, J.K.; Catalán, V.; Rodríguez, A.; Ramírez, B.; Silva, C.; Escalada, J.; Salvador, J.; Calamita, G.; Azcona-Sanjulian, M.C.; Frühbeck, G.; et al. Resting Energy Expenditure Is Not Altered in Children and Adolescents with Obesity. Effect of Age and Gender and Association with Serum Leptin Levels. Nutrients 2021, 13, 1216. https://doi.org/10.3390/nu13041216
Zapata JK, Catalán V, Rodríguez A, Ramírez B, Silva C, Escalada J, Salvador J, Calamita G, Azcona-Sanjulian MC, Frühbeck G, et al. Resting Energy Expenditure Is Not Altered in Children and Adolescents with Obesity. Effect of Age and Gender and Association with Serum Leptin Levels. Nutrients. 2021; 13(4):1216. https://doi.org/10.3390/nu13041216
Chicago/Turabian StyleZapata, J. Karina, Victoria Catalán, Amaia Rodríguez, Beatriz Ramírez, Camilo Silva, Javier Escalada, Javier Salvador, Giuseppe Calamita, M. Cristina Azcona-Sanjulian, Gema Frühbeck, and et al. 2021. "Resting Energy Expenditure Is Not Altered in Children and Adolescents with Obesity. Effect of Age and Gender and Association with Serum Leptin Levels" Nutrients 13, no. 4: 1216. https://doi.org/10.3390/nu13041216
APA StyleZapata, J. K., Catalán, V., Rodríguez, A., Ramírez, B., Silva, C., Escalada, J., Salvador, J., Calamita, G., Azcona-Sanjulian, M. C., Frühbeck, G., & Gómez-Ambrosi, J. (2021). Resting Energy Expenditure Is Not Altered in Children and Adolescents with Obesity. Effect of Age and Gender and Association with Serum Leptin Levels. Nutrients, 13(4), 1216. https://doi.org/10.3390/nu13041216









