Gluten-Free Diet: Nutritional Strategies to Improve Eating Habits in Children with Celiac Disease: A Prospective, Single-arm Intervention Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Nutritional Assessment
2.3. Nutrition Education
2.4. Statistical Analysis
3. Results
3.1. Subjects’ Characteristics
3.2. Dietary Intake
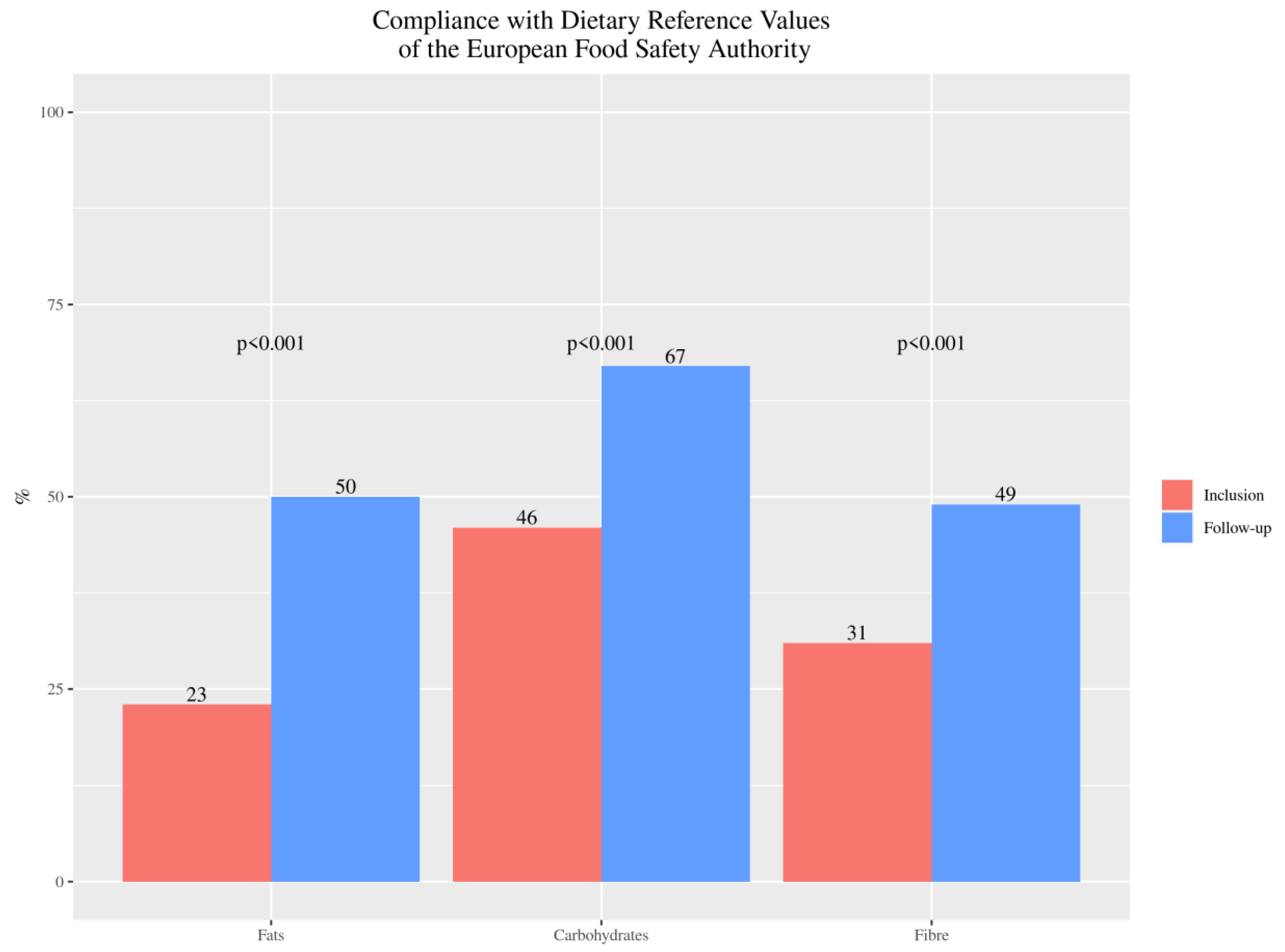
3.2.1. Macronutrients
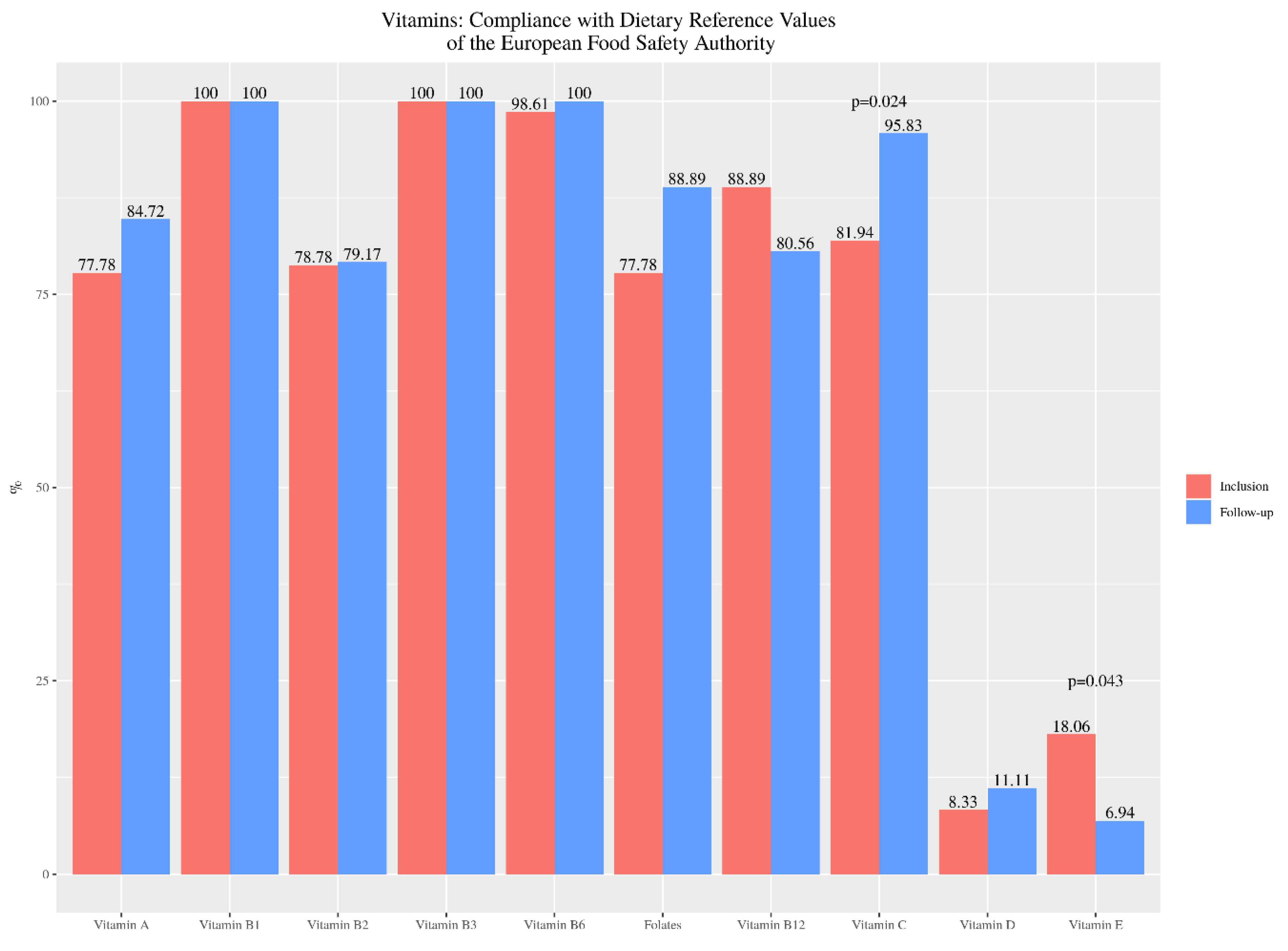
3.2.2. Micronutrients
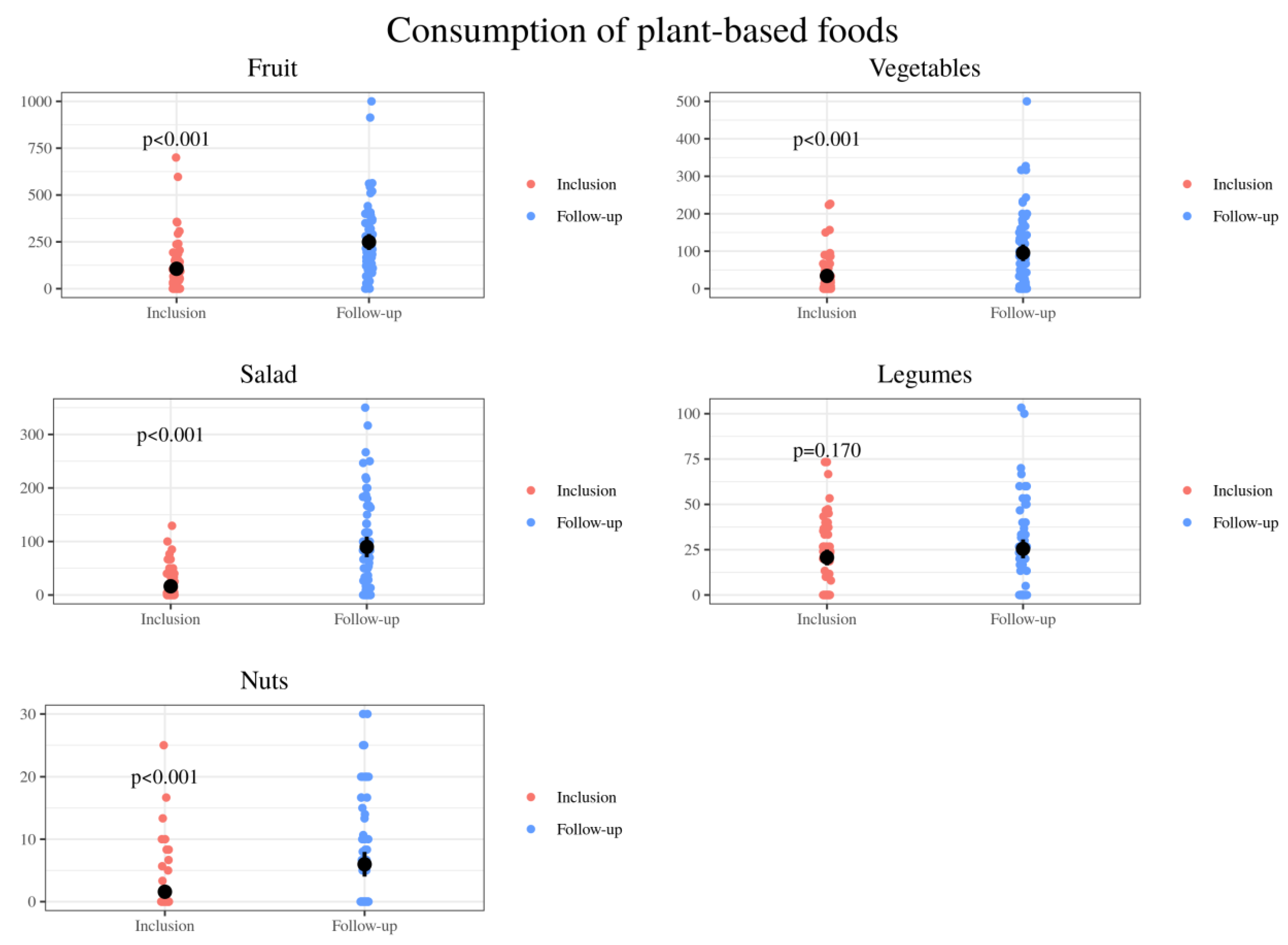
3.2.3. Foods
3.3. Stools’ Characteristics
3.4. Relationship of the Lipid Profile With Dietary Variables
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Singh, P.; Arora, A.; Strand, T.A.; Leffler, D.A.; Catassi, C.; Green, P.H.; Kelly, C.P.; Ahuja, V.; Makharia, G.K. Global Prevalence of Celiac Disease: Systematic Review and Meta-Analysis. Clin. Gastroenterol. Hepatol. 2018, 16, 823–836.e2. [Google Scholar] [CrossRef]
- Fasano, A.; Catassi, C. Clinical Practice. Celiac Disease. N. Engl. J. Med. 2012, 367, 2419–2426. [Google Scholar] [CrossRef]
- Silvester, J.A.; Weiten, D.; Graff, L.A.; Walker, J.R.; Duerksen, D.R. Living Gluten-Free: Adherence, Knowledge, Lifestyle Adaptations and Feelings towards a Gluten-Free Diet. J. Hum. Nutr. Diet. 2016, 29, 374–382. [Google Scholar] [CrossRef]
- Sue, A.; Dehlsen, K.; Ooi, C.Y. Paediatric Patients with Coeliac Disease on a Gluten-Free Diet: Nutritional Adequacy and Macro- and Micronutrient Imbalances. Curr. Gastroenterol. Rep. 2018, 20, 2. [Google Scholar] [CrossRef] [PubMed]
- Larretxi, I.; Simon, E.; Benjumea, L.; Miranda, J.; Bustamante, M.A.; Lasa, A.; Eizaguirre, F.J.; Churruca, I. Gluten-Free-Rendered Products Contribute to Imbalanced Diets in Children and Adolescents with Celiac Disease. Eur. J. Nutr. 2019, 58, 775–783. [Google Scholar] [CrossRef]
- Babio, N.; Alcázar, M.; Castillejo, G.; Recasens, M.; Martínez-Cerezo, F.; Gutiérrez-Pensado, V.; Masip, G.; Vaqué, C.; Vila-Martí, A.; Torres-Moreno, M.; et al. Patients With Celiac Disease Reported Higher Consumption of Added Sugar and Total Fat Than Healthy Individuals. J. Pediatr. Gastroenterol. Nutr. 2017, 64, 63–69. [Google Scholar] [CrossRef]
- Martin, J.; Geisel, T.; Maresch, C.; Krieger, K.; Stein, J. Inadequate Nutrient Intake in Patients with Celiac Disease: Results from a German Dietary Survey. Digestion 2013, 87, 240–246. [Google Scholar] [CrossRef] [PubMed]
- Ohlund, K.; Olsson, C.; Hernell, O.; Ohlund, I. Dietary Shortcomings in Children on a Gluten-Free Diet. J. Hum. Nutr. Diet. Off. J. Br. Diet. Assoc. 2010, 23, 294–300. [Google Scholar] [CrossRef]
- Hopman, E.G.D.; le Cessie, S.; von Blomberg, B.M.E.; Mearin, M.L. Nutritional Management of the Gluten-Free Diet in Young People with Celiac Disease in The Netherlands. J. Pediatr. Gastroenterol. Nutr. 2006, 43, 102–108. [Google Scholar] [CrossRef]
- Aguayo-Patrón, S.V.; Calderón de la Barca, A.M. Old Fashioned vs. Ultra-Processed-Based Current Diets: Possible Implication in the Increased Susceptibility to Type 1 Diabetes and Celiac Disease in Childhood. Foods 2017, 6, 100. [Google Scholar] [CrossRef] [PubMed]
- Wild, D.; Robins, G.G.; Burley, V.J.; Howdle, P.D. Evidence of High Sugar Intake, and Low Fibre and Mineral Intake, in the Gluten-Free Diet. Aliment. Pharmacol. Ther. 2010, 32, 573–581. [Google Scholar] [CrossRef]
- Thompson, T.; Dennis, M.; Higgins, L.A.; Lee, A.R.; Sharrett, M.K. Gluten-Free Diet Survey: Are Americans with Coeliac Disease Consuming Recommended Amounts of Fibre, Iron, Calcium and Grain Foods? J. Hum. Nutr. Diet. 2005, 18, 163–169. [Google Scholar] [CrossRef]
- Barone, M.; Della Valle, N.; Rosania, R.; Facciorusso, A.; Trotta, A.; Cantatore, F.P.; Falco, S.; Pignatiello, S.; Viggiani, M.T.; Amoruso, A.; et al. A Comparison of the Nutritional Status between Adult Celiac Patients on a Long-Term, Strictly Gluten-Free Diet and Healthy Subjects. Eur. J. Clin. Nutr. 2016, 70, 23–27. [Google Scholar] [CrossRef] [PubMed]
- Bardella, M.T.; Fredella, C.; Prampolini, L.; Molteni, N.; Giunta, A.M.; Bianchi, P.A. Body Composition and Dietary Intakes in Adult Celiac Disease Patients Consuming a Strict Gluten-Free Diet. Am. J. Clin. Nutr. 2000, 72, 937–939. [Google Scholar] [CrossRef]
- Mariani, P.; Viti, M.G.; Montuori, M.; La Vecchia, A.; Cipolletta, E.; Calvani, L.; Bonamico, M. The Gluten-Free Diet: A Nutritional Risk Factor for Adolescents with Celiac Disease? J. Pediatr. Gastroenterol. Nutr. 1998, 27, 519–523. [Google Scholar] [CrossRef] [PubMed]
- Rubio-Tapia, A.; Hill, I.D.; Kelly, C.P.; Calderwood, A.H.; Murray, J.A. American College of Gastroenterology ACG Clinical Guidelines: Diagnosis and Management of Celiac Disease. Am. J. Gastroenterol. 2013, 108, 656–676. [Google Scholar] [CrossRef] [PubMed]
- Theethira, T.G.; Dennis, M. Celiac Disease and the Gluten-Free Diet: Consequences and Recommendations for Improvement. Dig. Dis. 2015, 33, 175–182. [Google Scholar] [CrossRef] [PubMed]
- Kinsey, L.; Burden, S.T.; Bannerman, E. A Dietary Survey to Determine If Patients with Coeliac Disease Are Meeting Current Healthy Eating Guidelines and How Their Diet Compares to That of the British General Population. Eur. J. Clin. Nutr. 2008, 62, 1333–1342. [Google Scholar] [CrossRef]
- Thompson, T. Folate, Iron, and Dietary Fiber Contents of the Gluten-Free Diet. J. Am. Diet. Assoc. 2000, 100, 1389–1396. [Google Scholar] [CrossRef]
- Shepherd, S.J.; Gibson, P.R. Nutritional Inadequacies of the Gluten-Free Diet in Both Recently-Diagnosed and Long-Term Patients with Coeliac Disease. J. Hum. Nutr. Diet. 2013, 26, 349–358. [Google Scholar] [CrossRef]
- Grace-Farfaglia, P. Bones of Contention: Bone Mineral Density Recovery in Celiac Disease—A Systematic Review. Nutrients 2015, 7, 3347–3369. [Google Scholar] [CrossRef] [PubMed]
- Kupper, C. Dietary Guidelines and Implementation for Celiac Disease. Gastroenterology 2005, 128, S121–S127. [Google Scholar] [CrossRef] [PubMed]
- Penagini, F.; Dilillo, D.; Meneghin, F.; Mameli, C.; Fabiano, V.; Zuccotti, G.V. Gluten-Free Diet in Children: An Approach to a Nutritionally Adequate and Balanced Diet. Nutrients 2013, 5, 4553–4565. [Google Scholar] [CrossRef]
- Caruso, R.; Pallone, F.; Stasi, E.; Romeo, S.; Monteleone, G. Appropriate Nutrient Supplementation in Celiac Disease. Ann. Med. 2013, 45, 522–531. [Google Scholar] [CrossRef] [PubMed]
- Mager, D.R.; Qiao, J.; Turner, J. Vitamin D and K Status Influences Bone Mineral Density and Bone Accrual in Children and Adolescents with Celiac Disease. Eur. J. Clin. Nutr. 2012, 66, 488–495. [Google Scholar] [CrossRef]
- Saturni, L.; Ferretti, G.; Bacchetti, T. The Gluten-Free Diet: Safety and Nutritional Quality. Nutrients 2010, 2, 16–34. [Google Scholar] [CrossRef] [PubMed]
- Hallert, C.; Grant, C.; Grehn, S.; Grännö, C.; Hultén, S.; Midhagen, G.; Ström, M.; Svensson, H.; Valdimarsson, T. Evidence of Poor Vitamin Status in Coeliac Patients on a Gluten-Free Diet for 10 Years. Aliment. Pharmacol. Ther. 2002, 16, 1333–1339. [Google Scholar] [CrossRef] [PubMed]
- Laurikka, P.; Lindfors, K.; Oittinen, M.; Huhtala, H.; Salmi, T.; Lähdeaho, M.-L.; Ilus, T.; Mäki, M.; Kaukinen, K.; Kurppa, K. Dietary Factors and Mucosal Immune Response in Celiac Disease Patients Having Persistent Symptoms Despite a Gluten-Free Diet. J. Clin. Gastroenterol. 2019, 53, 507–513. [Google Scholar] [CrossRef] [PubMed]
- Lechner, K.; von Schacky, C.; McKenzie, A.L.; Worm, N.; Nixdorff, U.; Lechner, B.; Kränkel, N.; Halle, M.; Krauss, R.M.; Scherr, J. Lifestyle Factors and High-Risk Atherosclerosis: Pathways and Mechanisms beyond Traditional Risk Factors. Eur. J. Prev. Cardiol. 2020, 27, 394–406. [Google Scholar] [CrossRef]
- Mozaffarian, D. Dietary and Policy Priorities for Cardiovascular Disease, Diabetes, and Obesity: A Comprehensive Review. Circulation 2016, 133, 187–225. [Google Scholar] [CrossRef]
- Husby, S.; Koletzko, S.; Korponay-Szabó, I.R.; Mearin, M.L.; Phillips, A.; Shamir, R.; Troncone, R.; Giersiepen, K.; Branski, D.; Catassi, C.; et al. European Society for Pediatric Gastroenterology, Hepatology, and Nutrition Guidelines for the Diagnosis of Celiac Disease. J. Pediatr. Gastroenterol. Nutr. 2012, 54, 136–160. [Google Scholar] [CrossRef] [PubMed]
- Lewis, S.J.; Heaton, K.W. Stool Form Scale as a Useful Guide to Intestinal Transit Time. Scand. J. Gastroenterol. 1997, 32, 920–924. [Google Scholar] [CrossRef] [PubMed]
- Organizador Dietético Metabólico. Available online: http://www.odimet.es/ (accessed on 20 February 2020).
- Dietary Reference Values|DRV Finder. Available online: https://www.efsa.europa.eu/en/interactive-pages/drvs (accessed on 5 March 2020).
- Boston, 677 Huntington Avenue; Ma 02115 +1495-1000 El Plato Para Comer Saludable (Spanish). Available online: https://www.hsph.harvard.edu/nutritionsource/healthy-eating-plate/translations/spanish/ (accessed on 27 December 2019).
- R: The R Project for Statistical Computing. Available online: https://www.r-project.org/ (accessed on 13 March 2020).
- Cremers, J.; Mulder, K.T.; Klugkist, I. Circular Interpretation of Regression Coefficients. Br. J. Math. Stat. Psychol. 2018, 71, 75–95. [Google Scholar] [CrossRef]
- Suárez-González, M.; Bousoño García, C.; Jiménez Treviño, S.; Iglesias Cabo, T.; Díaz Martín, J.J. Influence of Nutrition Education in Paediatric Coeliac Disease: Impact of the Role of the Registered Dietitian: A Prospective, Single-Arm Intervention Study. J. Hum. Nutr. Diet. Off. J. Br. Diet. Assoc. 2020, 33, 775–785. [Google Scholar] [CrossRef] [PubMed]
- Moubarac, J.-C.; Parra, D.C.; Cannon, G.; Monteiro, C.A. Food Classification Systems Based on Food Processing: Significance and Implications for Policies and Actions: A Systematic Literature Review and Assessment. Curr. Obes. Rep. 2014, 3, 256–272. [Google Scholar] [CrossRef]
- Juul, F.; Martinez-Steele, E.; Parekh, N.; Monteiro, C.A.; Chang, V.W. Ultra-Processed Food Consumption and Excess Weight among US Adults. Br. J. Nutr. 2018, 120, 90–100. [Google Scholar] [CrossRef]
- Monteiro, C.A.; Moubarac, J.-C.; Levy, R.B.; Canella, D.S.; da Louzada, M.L.C.; Cannon, G. Household Availability of Ultra-Processed Foods and Obesity in Nineteen European Countries. Public Health Nutr. 2018, 21, 18–26. [Google Scholar] [CrossRef] [PubMed]
- Srour, B.; Fezeu, L.K.; Kesse-Guyot, E.; Allès, B.; Debras, C.; Druesne-Pecollo, N.; Chazelas, E.; Deschasaux, M.; Hercberg, S.; Galan, P.; et al. Ultra-processed Food Consumption and Risk of Type 2 Diabetes Among Participants of the NutriNet-Santé Prospective Cohort. JAMA Intern. Med. 2020, 180, 283–291. [Google Scholar] [CrossRef] [PubMed]
- Srour, B.; Fezeu, L.K.; Kesse-Guyot, E.; Allès, B.; Méjean, C.; Andrianasolo, R.M.; Chazelas, E.; Deschasaux, M.; Hercberg, S.; Galan, P.; et al. Ultra-processed Food Intake and Risk of Cardiovascular Disease: Prospective Cohort Study (NutriNet-Santé). BMJ 2019, 365, l1451. [Google Scholar] [CrossRef]
- Fiolet, T.; Srour, B.; Sellem, L.; Kesse-Guyot, E.; Allès, B.; Méjean, C.; Deschasaux, M.; Fassier, P.; Latino-Martel, P.; Beslay, M.; et al. Consumption of Ultra-Processed Foods and Cancer Risk: Results from NutriNet-Santé Prospective Cohort. BMJ 2018, 360, k322. [Google Scholar] [CrossRef]
- Lustig, R.H. Ultraprocessed Food: Addictive, Toxic, and Ready for Regulation. Nutrients 2020, 12, 3401. [Google Scholar] [CrossRef]
- Djupegot, I.L.; Nenseth, C.B.; Bere, E.; Bjørnarå, H.B.T.; Helland, S.H.; Øverby, N.C.; Torstveit, M.K.; Stea, T.H. The Association between Time Scarcity, Sociodemographic Correlates and Consumption of Ultra-Processed Foods among Parents in Norway: A Cross-Sectional Study. BMC Public Health 2017, 17, 447. [Google Scholar] [CrossRef]
- Miranda, J.; Lasa, A.; Bustamante, M.A.; Churruca, I.; Simon, E. Nutritional Differences between a Gluten-Free Diet and a Diet Containing Equivalent Products with Gluten. Plant Foods Hum. Nutr. 2014, 69, 182–187. [Google Scholar] [CrossRef] [PubMed]
- Kulai, T.; Rashid, M. Assessment of Nutritional Adequacy of Packaged Gluten-Free Food Products. Can. J. Diet. Pract. Res. 2014, 75, 186–190. [Google Scholar] [CrossRef] [PubMed]
- Cornicelli, M.; Saba, M.; Machello, N.; Silano, M.; Neuhold, S. Nutritional Composition of Gluten-Free Food versus Regular Food Sold in the Italian Market. Dig. Liver Dis. 2018, 50, 1305–1308. [Google Scholar] [CrossRef]
- Fry, L.; Madden, A.M.; Fallaize, R. An Investigation into the Nutritional Composition and Cost of Gluten-Free versus Regular Food Products in the UK. J. Hum. Nutr. Diet. 2018, 31, 108–120. [Google Scholar] [CrossRef]
- Mazzeo, T.; Cauzzi, S.; Brighenti, F.; Pellegrini, N. The Development of a Composition Database of Gluten-Free Products. Public Health Nutr. 2015, 18, 1353–1357. [Google Scholar] [CrossRef]
- Lionetti, E.; Antonucci, N.; Marinelli, M.; Bartolomei, B.; Franceschini, E.; Gatti, S.; Catassi, G.N.; Verma, A.K.; Monachesi, C.; Catassi, C. Nutritional Status, Dietary Intake, and Adherence to the Mediterranean Diet of Children with Celiac Disease on a Gluten-Free Diet: A Case-Control Prospective Study. Nutrients 2020, 12, 143. [Google Scholar] [CrossRef] [PubMed]
- Forchielli, M.L.; Diani, L.; Labriola, F.; Bolasco, G.; Rocca, A.; Salfi, N.C.; Leone, A.; Miserocchi, C.; Andreozzi, L.; Levi Della Vida, F.; et al. Gluten Deprivation: What Nutritional Changes Are Found During the First Year in Newly Diagnosed Coeliac Children? Nutrients 2019, 12, 60. [Google Scholar] [CrossRef]
- Pan, A.; Sun, Q.; Bernstein, A.M.; Schulze, M.B.; Manson, J.E.; Stampfer, M.J.; Willett, W.C.; Hu, F.B. Red Meat Consumption and Mortality: Results from 2 Prospective Cohort Studies. Arch. Intern. Med. 2012, 172, 555–563. [Google Scholar] [CrossRef]
- Locke, A.; Schneiderhan, J.; Zick, S.M. Diets for Health: Goals and Guidelines. Am. Fam. Physician 2018, 97, 721–728. [Google Scholar] [PubMed]
- Macêdo, M.I.P.; Albuquerque, M.d.F.M.; Tahan, S.; de Morais, M.B. Is There Any Association between Overweight, Physical Activity, Fat and Fiber Intake with Functional Constipation in Adolescents? Scand. J. Gastroenterol. 2020, 1–7. [Google Scholar] [CrossRef]
- Southwell, B.R. Treatment of Childhood Constipation: A Synthesis of Systematic Reviews and Meta-Analyses. Expert Rev. Gastroenterol. Hepatol. 2020, 14, 163–174. [Google Scholar] [CrossRef] [PubMed]
- Barton, S.H.; Kelly, D.G.; Murray, J.A. Nutritional Deficiencies in Celiac Disease. Gastroenterol. Clin. N. Am. 2007, 36, 93–108. [Google Scholar] [CrossRef]
- Zuccotti, G.; Fabiano, V.; Dilillo, D.; Picca, M.; Cravidi, C.; Brambilla, P. Intakes of Nutrients in Italian Children with Celiac Disease and the Role of Commercially Available Gluten-Free Products. J. Hum. Nutr. Diet. 2013, 26, 436–444. [Google Scholar] [CrossRef]
- Turnbull, B.; Lanigan, J.; Singhal, A. Toddler Diets in the U.K.: Deficiencies and Imbalances. 1. Risk of Micronutrient Deficiencies. J. Fam. Health Care 2007, 17, 167–170. [Google Scholar] [PubMed]
- Dunn, J.T. Iodine Should Be Routinely Added to Complementary Foods. J. Nutr. 2003, 133, 3008S–3010S. [Google Scholar] [CrossRef]
- Kapourchali, F.R.; Surendiran, G.; Goulet, A.; Moghadasian, M.H. The Role of Dietary Cholesterol in Lipoprotein Metabolism and Related Metabolic Abnormalities: A Mini-Review. Crit. Rev. Food Sci. Nutr. 2016, 56, 2408–2415. [Google Scholar] [CrossRef]
- Lebwohl, B.; Sanders, D.S.; Green, P.H.R. Coeliac Disease. Lancet 2018, 391, 70–81. [Google Scholar] [CrossRef]
- Bascuñán, K.A.; Vespa, M.C.; Araya, M. Celiac Disease: Understanding the Gluten-Free Diet. Eur. J. Nutr. 2017, 56, 449–459. [Google Scholar] [CrossRef]
- Alzaben, A.S.; Turner, J.; Shirton, L.; Samuel, T.M.; Persad, R.; Mager, D. Assessing Nutritional Quality and Adherence to the Gluten-Free Diet in Children and Adolescents with Celiac Disease. Can. J. Diet. Pract. Res. 2015, 76, 56–63. [Google Scholar] [CrossRef]
- Wu, J.H.Y.; Neal, B.; Trevena, H.; Crino, M.; Stuart-Smith, W.; Faulkner-Hogg, K.; Yu Louie, J.C.; Dunford, E. Are Gluten-Free Foods Healthier than Non-Gluten-Free Foods? An Evaluation of Supermarket Products in Australia. Br. J. Nutr. 2015, 114, 448–454. [Google Scholar] [CrossRef] [PubMed]
- de Deus Mendonça, R.; Lopes, A.C.S.; Pimenta, A.M.; Gea, A.; Martinez-Gonzalez, M.A.; Bes-Rastrollo, M. Ultra-Processed Food Consumption and the Incidence of Hypertension in a Mediterranean Cohort: The Seguimiento Universidad de Navarra Project. Am. J. Hypertens. 2017, 30, 358–366. [Google Scholar] [CrossRef]
- Giménez, A.; de Saldamando, L.; Curutchet, M.R.; Ares, G. Package Design and Nutritional Profile of Foods Targeted at Children in Supermarkets in Montevideo, Uruguay. Cad. Saude Publica 2017, 33, e00032116. [Google Scholar] [CrossRef] [PubMed]
- Wilkin, T.J. The Convergence of Type 1 and Type 2 Diabetes in Childhood: The Accelerator Hypothesis. Pediatr. Diabetes 2012, 13, 334–339. [Google Scholar] [CrossRef] [PubMed]
- Madrigal, C.; Soto-Méndez, M.J.; Hernández-Ruiz, Á.; Valero, T.; Ávila, J.M.; Ruiz, E.; Lara Villoslada, F.; Leis, R.; de Martínez Victoria, E.; Moreno, J.M.; et al. Energy Intake, Macronutrient Profile and Food Sources of Spanish Children Aged One to <10 Years—Results from the EsNuPI Study. Nutrients 2020, 12, 893. [Google Scholar] [CrossRef] [PubMed]
- Estudio PASOS resultados finales. In Gasol Found; España, 2019.
- Kautto, E.; Ivarsson, A.; Norström, F.; Högberg, L.; Carlsson, A.; Hörnell, A. Nutrient Intake in Adolescent Girls and Boys Diagnosed with Coeliac Disease at an Early Age Is Mostly Comparable to Their Non-Coeliac Contemporaries. J. Hum. Nutr. Diet. 2014, 27, 41–53. [Google Scholar] [CrossRef] [PubMed]





| Lipid Profile | Dietary Variables | Correlation Coefficient R | p-Value | Test |
|---|---|---|---|---|
| Total cholesterol | Biscuits | 0.318 | 0.019 | Spearman´s |
| Low-fat yogurt | –0.274 | 0.047 | Spearman´s | |
| Total sugars | 0.289 | 0.034 | Spearman´s | |
| Saturated fat | 0.271 | 0.047 | Pearson´s | |
| HDL cholesterol | Sugary breakfast cereals | –0.364 | 0.010 | Spearman´s |
| Low-fat yogurt | –0.338 | 0.019 | Spearman´s | |
| LDL cholesterol | Processed meats | 0.365 | 0.011 | Spearman´s |
| Saturated fat | 0.285 | 0.050 | Pearson´s | |
| Sugary cocoa powder | 0.276 | 0.058 | Spearman´s | |
| Triglyceride | Sugary breakfast cereals | 0.288 | 0.039 | Spearman´s |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Suárez-González, M.; Bousoño-García, C.; Jiménez-Treviño, S.; Díaz-Martín, J.J. Gluten-Free Diet: Nutritional Strategies to Improve Eating Habits in Children with Celiac Disease: A Prospective, Single-arm Intervention Study. Nutrients 2021, 13, 1108. https://doi.org/10.3390/nu13041108
Suárez-González M, Bousoño-García C, Jiménez-Treviño S, Díaz-Martín JJ. Gluten-Free Diet: Nutritional Strategies to Improve Eating Habits in Children with Celiac Disease: A Prospective, Single-arm Intervention Study. Nutrients. 2021; 13(4):1108. https://doi.org/10.3390/nu13041108
Chicago/Turabian StyleSuárez-González, Marta, Carlos Bousoño-García, Santiago Jiménez-Treviño, and Juan José Díaz-Martín. 2021. "Gluten-Free Diet: Nutritional Strategies to Improve Eating Habits in Children with Celiac Disease: A Prospective, Single-arm Intervention Study" Nutrients 13, no. 4: 1108. https://doi.org/10.3390/nu13041108
APA StyleSuárez-González, M., Bousoño-García, C., Jiménez-Treviño, S., & Díaz-Martín, J. J. (2021). Gluten-Free Diet: Nutritional Strategies to Improve Eating Habits in Children with Celiac Disease: A Prospective, Single-arm Intervention Study. Nutrients, 13(4), 1108. https://doi.org/10.3390/nu13041108






