Curcumin in Metabolic Health and Disease
Abstract
:1. Introduction
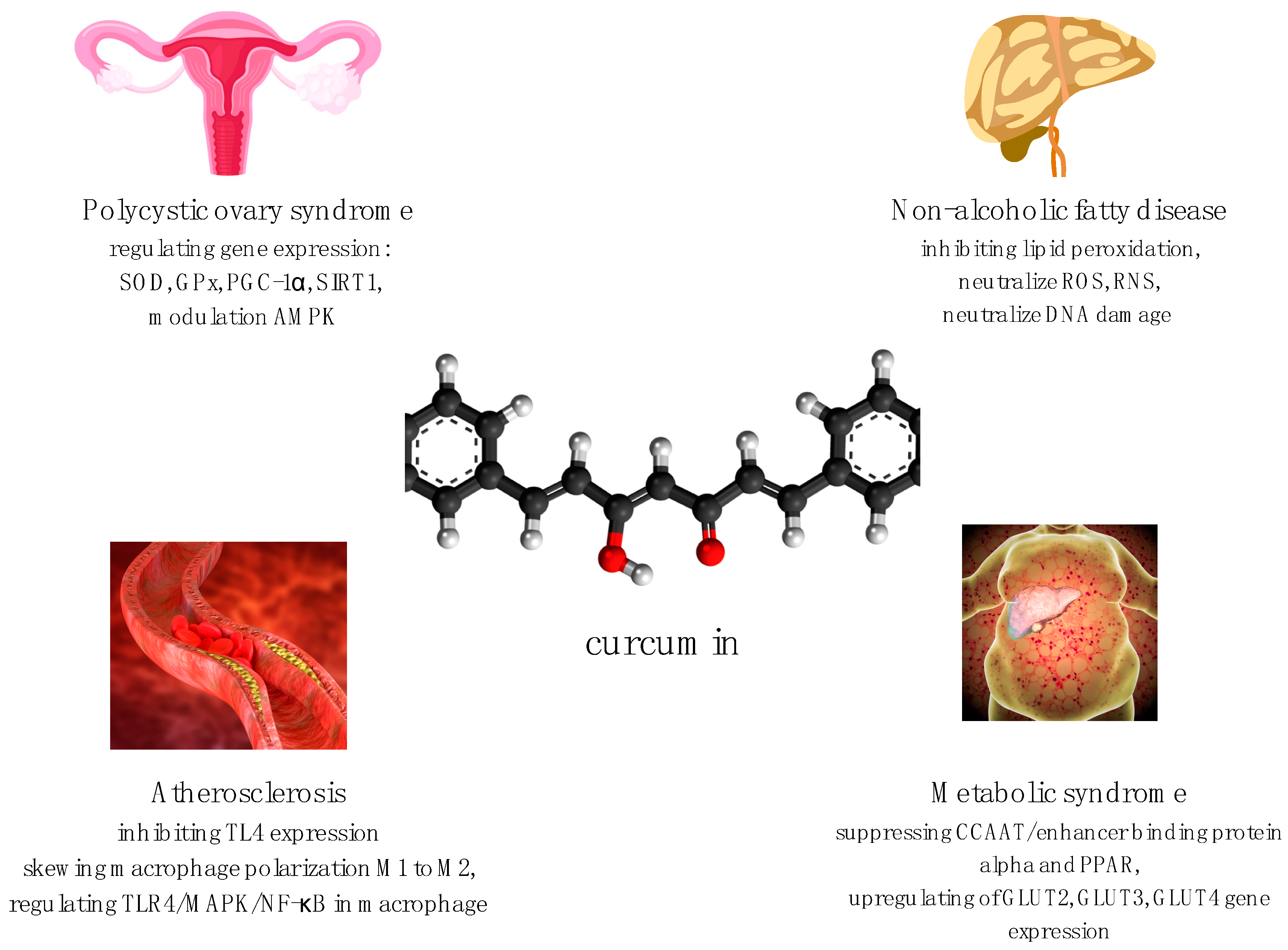
1.1. Curcumin for Treatment of Polycystic Ovary Syndrome (PCOS)
1.2. Curcumin for Treatment of Metabolic Syndrome
1.3. Curcumin for Non-Alcoholic Fatty Liver Disease (NAFLD)
1.4. Curcumin for Treatment of Atherosclerosis
2. Summary
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Różański, G.; Kujawski, S.; Newton, J.L.; Zalewski, P.; Słomko, J. Curcumin and Biochemical Parameters in Metabolic-Associated Fatty Liver Disease (MAFLD)-A Review. Nutrients 2021, 13, 2654. [Google Scholar] [CrossRef]
- Chang, G.-R.; Hsieh, W.-T.; Chou, L.-S.; Lin, C.-S.; WU, C.-F.; Lin, J.-W.; Lin, W.-L.; Lin, T.-C.; Liao, H.-J.; Kao, C.-Y.; et al. Curcumin Improved Glucose Intolerance, Renal Injury, and Nonalcoholic Fatty Liver Disease and Decreased Chromium Loss through Urine in Obese Mice. Processes 2021, 9, 1132. [Google Scholar] [CrossRef]
- Hewlings, S.J.; Kalman, D.S. Curcumin: A Review of Its Effects on Human Health. Foods 2017, 6, 92. [Google Scholar] [CrossRef] [PubMed]
- Jabczyk, M.; Nowak, J.; Hudzik, B.; Zubelewicz-Szkodzińska, B. Curcumin and Its Potential Impact on Microbiota. Nutrients 2021, 13, 2004. [Google Scholar] [CrossRef]
- Karthikeyan, A.; Senthil, N.; Min, T. Nanocurcumin: A promising Candidate for Therapeutic Applications. Front. Pharmacol. 2020, 11, 487. [Google Scholar] [CrossRef] [PubMed]
- Nasery, M.M.; Abadi, B.; Poormoghadam, D.; Zarrabi, A.; Keyhanvar, P.; Khanbabaei, H.; Ashrafizadeh, M.; Mohammadinejad, R.; Tavakol, S.; Sethi, G. Curcumin Delivery Mediated by Bio-Based Nanoparticles: A Review. Molecules 2020, 25, 689. [Google Scholar] [CrossRef] [Green Version]
- Ferrari, R.; Sponchioni, M.; Morbidelli, M.; Moscatelli, D. Polymer nanoparticles for the intravenous delivery of anticancer drugs: The checkpoints on the road from the synthesis to clinical translation. Nanoscale 2018, 10, 22701–22719. [Google Scholar] [CrossRef]
- Nambiar, S.; Osei, E.; Fleck, A.; Darko, J.; Mutsaers, A.J.; Wettig, S. Synthesis of curcumin-functionalized gold nanoparticles and cytotoxicity studies in human prostate cancer cell line. Appl. Nanosci. 2018, 8, 347–357. [Google Scholar] [CrossRef]
- Roacho-Pérez, J.A.; Ruiz-Hernandez, F.G.; Chapa-Gonzalec, C.; Martinez-Rodriguez, H.G.; Flores-Urquizo, I.A.; Pedroza-Montoya, F.E.; Garza-Treviño, E.N.; Bautista-Villareal, M.; García-Casillas, P.E.; Sánchez-Domínguez, C.N. Magnetite Nanoparticles Coated with PEG 3350-Tween 80: In Vitro Characterization Using Primary Cell Cultures. Polymers 2020, 12, 300. [Google Scholar] [CrossRef] [Green Version]
- Ayubi, M.; Karimi, M.; Abdpour, S.; Rostamizadeh, K.; Parsa, M.; Zamanic, M.; Saedia, A. Magnetic nanoparticles decorated with PEGylated curcumin as dual targeted drug delivery: Synthesis, toxicity and biocompatibility study. Mater. Sci. Eng. C 2019, 104, 109810. [Google Scholar] [CrossRef]
- Nahar, P.P.; Slitt, A.L.; Seeram, N.P. Anti-Inflammatory Effects of Novel Standarized Solid Lipid Curcumin Formulations. J. Med. Food 2015, 18, 786–792. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brahmkhatri, V.P.; Sharna, N.; Sunanda, P.; D’Suoza, A.; Raghothama, S.; Atreya, H.S. Curcumin nanoconjugate inhibits aggregation of N-terminal region (Aβ-16) of an amyloid beta peptide. New J. Chem. 2018, 42, 19881–19892. [Google Scholar] [CrossRef]
- Rana, S.; Bhattacharjee, J.; Barick, K.C.; Verma, G.; Hassan, P.A.; Yakhmi, J.V. Interfacial engineering of nanoparticles for cancer therapeutics. In Nanostructures for Cancer Therapy; Ficai, A., Grumezescu, A.M., Eds.; Elsevier: Amsterdam, The Netherlands, 2017; pp. 177–209. [Google Scholar]
- Akaberi, M.; Sahebkar, A.; Emami, A.A. Turmeric and Curcumin: From Traditional to Modern Medicine. Adv. Exp. Med. Biol. 2021, 1291, 15–39. [Google Scholar] [CrossRef] [PubMed]
- Heshmati, J.; Golab, F.; Morvaridzadeh, M.; Potter, E.; Akbar-Fakhrabadi, M.; Farsi, F.; Tanbakooei, S.; Shidfar, F. The effects of curcumin supplementation on oxidative stress, Sirtuin-1 and peroxisome proliferator activated receptor γ coactivator 1α gene expression in polycystic ovarian syndrome (PCOS) patients: A randomized placebo-controlled clinical trial. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 77–82. [Google Scholar] [CrossRef]
- Shehzad, A.; Qureshi, M.; Anwar, M.N.; Lee, Y.S. Multifunctional Curcumin Mediate Multitherapeutic Effects. J. Food Sci. 2017, 82, 2006–2015. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mantovani, A.; Byrne, C.D.; Bonora, E.; Targher, G. Nonalcoholic Fatty Liver Disease and Risk of Incident Type 2 Diabetes: A Meta-analysis. Diabetes Care 2018, 41, 372–382. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Farzaei, M.H.; Zobeiri, M.; Parvizi, F.; El-Senduny, F.F.; Marmouzi, I.; Coy-Barrera, E.; Naseri, R.; Nabavi, S.M.; Rahimi, R.; Abdollahi, M. Curcumin in Liver Diseases: A systematic Review of the Cellular Mechanisms of Oxidative Stress and Clinical Perspective. Nutrients 2018, 10, 855. [Google Scholar] [CrossRef] [Green Version]
- Panahi, Y.; Ahmadi, Y.; Teymouri, M.; Johnston, T.P.; Sahebkar, A. Curcumin as a potential candidate for treating hyperlipidemia: A review of cellular and metabolic mechanisms. J. Cell. Physiol. 2018, 233, 142–152. [Google Scholar] [CrossRef] [PubMed]
- Singh, L.; Sharma, S.; Xu, S.; Tewari, D.; Fang, J. Curcumin as a Natural Remedy for Atherosclerosis: A pharmacological Review. Molecules 2021, 26, 4036. [Google Scholar] [CrossRef]
- Zhou, Y.; Zhang, T.; Wang, X.; Chen, Y.; Guo, L.; Zhang, J.; Wang, C. Curcumin Modulates Macrophage Polarization Through the Inhibition of the Toll-like Receptor 4 Expression and its Signaling Pathways. Cell. Physiol. Biochem. 2015, 36, 631–641. [Google Scholar] [CrossRef]
- Bannigida, D.M.; Nayak, S.; Vijayaraghavan, R. Insulin resistance and oxidative marker in women with PCOS. Arch. Physiol. Biochem. 2020, 126, 183–185. [Google Scholar] [CrossRef] [PubMed]
- Rajska, A.; Buszewska-Forajta, M.; Rachoń, D.; Markuszoewaki, M.J. Metabolomic Insgiht into Polycystic Ovary Syndrome–An Overview. Int. J. Mol. Sci. 2020, 21, 1853. [Google Scholar] [CrossRef]
- Dantas, W.S.; Gualano, B.; Rocha, M.P.; Barcellos, C.R.G.; Yance, V.D.R.V.; Marcondes, J.A.M. Metabolic Disturbance in PCOS: Clinical and Molecular Effects on Skeletal Muscle Tissue. Sci. World J. 2013, 2014, 178364. [Google Scholar] [CrossRef] [Green Version]
- Chien, Y.-J.; Chang, C.-Y.; Wu, M.-Y.; Chen, C.-H.; Horng, Y.-S.; Wu, H.-C. Effects of Curcumin on Glycemic Control and Lipid Profile in Polycystic Ovary Syndrome: Systematic Review with Meta-Analysis and Trial Sequential Analysis. Nutrients 2021, 13, 684. [Google Scholar] [CrossRef]
- Jamilian, M.; Foroozanfard, F.; Kavossian, E.; Aghadavod, E.; Shafabakhsh, R.; Hoseini, A.; Asemi, Z. Effects of curcumin on body weight, glycemic control and serum lipids in women with polycystic ovary syndrome: A randomized, double-blind, placebo-controlled trial. Clin. Nutr. ESPEN 2020, 36, 128–133. [Google Scholar] [CrossRef]
- Sohaei, S.; Amani, R.; Tarrahi, M.J.; Ghasemi-Tehrani, H. The effects of curcumin supplementation on glycemic status, lipid profile and hs-CRP levels in overweight/obese women with polycystic ovary syndrome: A randomized, double-blind, placebo-controlled clinical trial. Complement. Ther. Med. 2019, 47, 102201. [Google Scholar] [CrossRef]
- Heshmati, J.; Moini, A.; Sepidarkish, M.; Morvaridzadeh, M.; Salehi, M.; Palmowski, A.; Mojathedi, M.F.; Shidfar, F. Effects of curcumin supplementation on blood glucose, insulin resistance and androgens in patients with polycystic ovary syndrome: A randomized double-blind placebo-controlles clinical trial. Phytomedicine 2021, 80, 153395. [Google Scholar]
- Wickenberg, J.; Ingemansson, S.L.; Hlebowicz, J. Effects of Curcuma longa (turmeric) on postprandial plasma glucose and insulin in healthy subjects. Nutr. J. 2010, 9, 43. [Google Scholar]
- Sohrevardi, S.M.; Heydari, B.; Azarpazhooh, M.R.; Teymourzadeh, M.; Simental-Mendia, L.E.; Atkin, S.L.; Sahebkar, A.; Karimi-Zarchi, M. Therapeutic Effect of Curcumin in Women with Polycystic Ovary Syndrome Receiving Metformin: A Randomized Controlled Trial. Adv. Exp. Med. Biol. 2021, 1308, 109–117. [Google Scholar] [PubMed]
- Mohammadi, S.; Kayedpoor, P.; Karimzadeh-Bardei, L.; Nabiuni, M. The Effect of Curcumin on TNF-α, IL-6 and CRP Expression in a Model of Polycsystic Ovary Syndrome as an Inflammation State. J. Reprod. Infertil. 2017, 18, 352–360. [Google Scholar]
- Abuelezz, N.Z.; Shabana, M.E.; Abdel-Mageed, H.M.; Rashed, L.; Morcos, G.N. Nanocurcumin alleviates insulin resistance and pancreatic deficits in polycystic ovary syndrome rats: Insights on PI3K/AkT/mTOR and TNF-α modulations. Life Sci. 2020, 256, 11800. [Google Scholar] [CrossRef] [PubMed]
- Ashtary-Larky, D.; Jelishadi, M.R.; Bagheri, R.; Moosavian, S.; Wong, A.; Davoodi, S.; Khalili, P.; Dutheil, F.; Suzuki, K.; Asbaghi, O. The Effects of Nano-Curcumin Supplementation on Risk Factors for Cardiovascular Disease: A GRADE-Assessed Systematic Review and Meta-Analysis of Clinical Trials. Antioxidants 2021, 10, 1015. [Google Scholar] [CrossRef]
- Abhari, S.M.F.A.; Khanbabaei, R.; Roodbari, N.H.; Parivar, K.; Yaghmaei, P. Curcumin-loaded super-paramagnetic iron oxide nanoparticle affects on apoptotic factors expression and histological changes in a prepubertal mouse model of polycystic ovary syndrome-induced by—A molecular and stereological study. Life Sci. 2020, 249, 117515. [Google Scholar] [CrossRef]
- Kheiripour, N.; Khodamoradi, Z.; Ranjbar, A.; Borzouei, S. The positive effect of short-term nano-curcumin therapy on insulin resistance and serum levels of afamin in patients with metabolic syndrome. Avicenna J. Phytomedicine 2021, 11, 146–153. [Google Scholar]
- Rojas, E.; Castro, A.; Manzano, A.; Suarez, M.K.; Lameda, V.; Carrasquero, R.; Nava, M.; Bermudez, V. Diagnostic criteria and management of metabolic syndrome: Evolution overtime. Gac Méd Caracas 2020, 128, 480–504. [Google Scholar] [CrossRef]
- Bateni, Z.; Rahimi, H.R.; Hadeyati, M.; Afsharian, S.; Goudarzi, R.; Sohrab, G. The effects of nano-curcumin supplementation on glycemic control, blood pressure, lipid profile, and insulin resistance in patients with the metabolic syndrome: A randomized, double-blind clinical trial. Phytother Res. 2021, 35, 3945–3953. [Google Scholar] [CrossRef]
- Shamsi-Goushki, A.; Mortazavi, Z.; Mirshekar, M.A.; Mohammadi, M.; Moradi-Kor, N.; Jafari-Maskouni, S.; Shahraki, M. Comparative effects of curcumin versus nano-curcumin on insulin resistance, serum levels of apelin and lipid profile in type 2 diabetic rats. Diabetes Metab. Syndr. Obes. Targets Ther. 2020, 13, 2337–2346. [Google Scholar] [CrossRef]
- Rahimi, H.R.; Mohammadpour, A.H.; Dastani, M.; Jaafari, M.R.; Abnous, K.; Mobarham, M.G.; Oskuee, R.K. The effect of nano-curcumin on HbA1c, fasting glucose, and lipid profile in diabetic subjects: A randomized clinical trial. Avicenna J. Phytomedicine 2016, 6, 567–577. [Google Scholar]
- Eslam, M.; Sanyal, A.J.; George, J. MAFLD: A Consensus-Driven Proposed Nomenclature for Metabolic Associated Fatty Liver Disease. Gastroenterology 2020, 158, 1999–2014. [Google Scholar] [CrossRef] [PubMed]
- Jalali, M.; Mahmoodi, M.; Mosallanezhad, Z.; Jalali, R.; Imanieh, M.H.; Moosavian, S.P. The effects of curcumin supplementation on liver function, metabolic profile and body composition in patients with non-alcoholic fatty liver disease: A systematic review and meta-analysis of randomized controlled trials. Complement. Ther. Med. 2020, 48, 102283. [Google Scholar] [CrossRef]
- Li, H.; Sureda, A.; Devkota, H.P.; Pittalà, V.; Barreca, D.; Silva, A.S.; Tewari, D.; Xu, S.; Nabavi, S.M. Curcumin, the golden spice in treating cardiovascular diseases. Biotechnol. Adv. 2020, 38, 107343. [Google Scholar] [CrossRef]
- Lin, K.; Chen, H.; Chen, X.; Qian, J.; Huang, S.; Huang, W. Efficacy of Curcumin on Aortic Atherosclerosis: A Systematic Review and Meta-Analysis in Mouse Studies and Insights into Possible Mechanisms. Oxidative Med. Cell. Longev. 2020, 2020, 1520747. [Google Scholar] [CrossRef] [PubMed]
- Pello, O.M.; Silvestre, C.; De Pizzol, M.; Andres, V. A glimpse on the phenomenon of macrophage polarization during atherosclerosis. Immunobiology 2011, 216, 1172–1176. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Zou, J.; Li, P.; Zheng, X.; Feng, D. Curcumin Protects against Atherosclerosis in Apolipoprotein E-Knockout Mice by Inhibiting Toll-like Receptor 4 Expression. J. Agric. Food. Chem. 2018, 66, 449–456. [Google Scholar] [CrossRef] [PubMed]
- Meng, Z.; Yan, C.; Deng, Q.; Gao, D.F.; Niu, X.L. Curcumin inhibits LPS-induced inflammation in rat vascular smooth muscle cells in vitro via ROS-relative TLR4-MAPK/NF- κB pathways. Acta Pharmacol. Sin. 2013, 34, 901–911. [Google Scholar] [CrossRef] [Green Version]
| Characteristics of Study and Dose of Curcumin | Impact on Parameters in PCOS | Results (Curcumin-Placebo) | p | References |
|---|---|---|---|---|
| Meta-analysis of three random-ized-control trials (168 patients) 500–1500 mg per day 6–12 weeks | Fasting glucose | −2.77 | 0.001 | [25,26,27,28] |
| Fasting insulin | −1.33 | 0.002 | ||
| HOMA-IR | −0.32 | 0.002 | ||
| QUICKI | 0.010 | 0.005 | ||
| TC | −12.45 | 0.011 | ||
| HDL | −1.92 | 0.018 | ||
| LDL | −6.02 | 0.567 | ||
| TG | 8.22 | 0.639 |
| Characteristics of the Study and Dose of Nano-Curcumin | Impact on Parameters in Metabolic Syndrome | Results | p | References |
|---|---|---|---|---|
| (Nano-Curcumin-Placebo) | ||||
| Randomized double-blind clinical trial (43 patients); 80 mg per day of nanocur-cumin; 3 months | Fasting glucose | −6.9 ± 55.2 | 0.642 | [37] |
| Fasting insulin | −1.1 ± 5.6 | 0.253 | ||
| HbA1c | −0.05 ± 1.59 | 0.124 | ||
| HOMA-IR | 0.3 ± 1.9 | 0.309 | ||
| HOMA-ß | −5.7 ± 48.2 | 0.882 | ||
| TC | −5.1 ± 37.4 | 0.356 | ||
| HDL | 3.2 ± 13.07 | 0.142 | ||
| LDL | 1.6 ± 42.9 | 0.218 | ||
| TG | −60.5 ± 121.7 | 0.024 | ||
| Randomized clinical trial (70 type 2 diabetic patients); 80 mg per day of nano-curcumin (SinaCur-cumin®); 3 months | Fasting glucose | −17.12 ± 40.38 | 0.657 | [39] |
| HbA1c | −0.91 ± 1.11 | 0.013 | ||
| TC | −15.45 ± 44.75 | 0.889 | ||
| HDL-C | 1.83 ± 13.11 | 0.952 | ||
| LDL-C | −16.41 ± 30.93 | 0.046 | ||
| TG | −6.7 ± 67.52 | 0.772 | ||
| BMI | −1.34 ± 1.88 | 0.001 | ||
| (30 patients); 80 mg per day nano-curcumin; 2 months | Fasting glucose | 0.016 | [35] | |
| Fasting insulin | - | 0.017 | ||
| HOMA-IR | - | 0.006 | ||
| TC | 190.06 ± 32.89 | 0.786 | ||
| HDL-C | 40.52 ± 9.08 | 0.15 | ||
| LDL-C | 108.23 ± 20.46 | 0.459 | ||
| TG | 176.30 ± 11.34 | 0.32 | ||
| BMI | 32.07 ± 4.15 | 0.816 | ||
| Afamin | - | 0.047 |
| Characteristics of the Study and Dose of Curcumin | Impact on Metabolic Parameters in NAFLD | Results | p | References |
|---|---|---|---|---|
| (Curcumin-Placebo) | ||||
| Meta-analysis of nine ran-domized controlled trials; 500–1500 mg per day 2–3 months | Fasting glucose | 0.221 | 0.027 | [41] |
| Fasting insulin | −0.487 | 0.003 | ||
| HbA1c | −0.159 | 0.213 | ||
| HOMA-IR | 0.365 | 0.031 | ||
| TC | 0.645 | 0.002 | ||
| HDL | 0.88 | 0.139 | ||
| LDL | −1.028 | 0.028 | ||
| TG | 0.608 | 0.065 | ||
| ALT | −0.458 | 0.049 | ||
| AST | −0.784 | 0.032 | ||
| BMI | −0.179 | 0.058 |
| Characteristics of the Study and Dose of Nano-Curcumin | Impact on Metabolic Parameters | Results | p | References |
|---|---|---|---|---|
| (Curcumin-Placebo) | ||||
| Meta-analysis of nine random-ized control trials GRADE (510 patients); 6–12 weeks 40–120 mg per day | Fasting glucose | 221,218.1 | 0.001 | [33] |
| Fasting insulin | 22,121.21 | <0.001 | ||
| HbA1c | 22,120.66 | 0.081 | ||
| HOMA-IR | 22,120.28 | <0.001 | ||
| QUCIKI | 22,123.34 | 0.554 | ||
| TC overall | 22,120.53 | 0.945 | ||
| TC < 200 | 221,210.9 | <0.001 | ||
| TC ≥ 200 | 5.77 | <0.001 | ||
| HDL overall | 2.01 | 0.028 | ||
| HDL < 40 | 7.61 | <0.001 | ||
| HDL ≥ 40 | 22,123.59 | 0.562 | ||
| LDL overall | 22,120.14 | 0.986 | ||
| LDL < 100 | 221,213.7 | <0.001 | ||
| LDL ≥ 100 | 22,129.76 | 0.404 | ||
| TG overall | 25.53 | 0.29 | ||
| TG < 150 mg/dL | 221,224.9 | <0.001 | ||
| TG ≥ 150 mg/dL | 22,122.74 | 0.858 | ||
| BMI: 25–29.9 | 221,227.2 | 0.002 | ||
| BMI > 30 | 221,218.1 | 0.001 | ||
| CRP | 22,121.29 | 0.003 | ||
| IL-6 | 22,122.78 | <0.0001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jabczyk, M.; Nowak, J.; Hudzik, B.; Zubelewicz-Szkodzińska, B. Curcumin in Metabolic Health and Disease. Nutrients 2021, 13, 4440. https://doi.org/10.3390/nu13124440
Jabczyk M, Nowak J, Hudzik B, Zubelewicz-Szkodzińska B. Curcumin in Metabolic Health and Disease. Nutrients. 2021; 13(12):4440. https://doi.org/10.3390/nu13124440
Chicago/Turabian StyleJabczyk, Marzena, Justyna Nowak, Bartosz Hudzik, and Barbara Zubelewicz-Szkodzińska. 2021. "Curcumin in Metabolic Health and Disease" Nutrients 13, no. 12: 4440. https://doi.org/10.3390/nu13124440
APA StyleJabczyk, M., Nowak, J., Hudzik, B., & Zubelewicz-Szkodzińska, B. (2021). Curcumin in Metabolic Health and Disease. Nutrients, 13(12), 4440. https://doi.org/10.3390/nu13124440






