Herbal Infusions as a Valuable Functional Food
Abstract
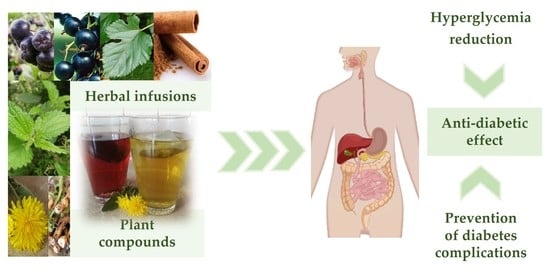
1. Introduction
2. Materials and Methods
2.1. Herbal Tea Blends
2.2. Chemical Reagents
2.3. Extracts Preparations
2.4. Total Phenolic Content (TPC) and Total Flavonoid Content (TFC) Analysis
2.5. High-Performance Liquid Chromatography (HPLC) Analysis
2.6. Determination of Hypoglycemic Potential
2.6.1. α-Glucosidase Inhibitory Assay
2.6.2. α-Amylase Inhibitory Assay
2.7. Determination of the Preventive Potential for Type II Diabetes Complications
2.7.1. DPPH and CUPRAC Assays
2.7.2. Determination of Fe2+ Chelating Activity
2.7.3. Determination of Anti-Collagenase Potential
2.8. Statistical Analysis
3. Results
3.1. Phytochemical Characterization of Herbal Blends
3.2. Determination of Hypoglycemic Potential
3.3. Determination of the Preventive Potential for Type II Diabetes Complications
3.3.1. In Vitro Antioxidant Activity
3.3.2. In Vitro Anti-Inflammatory Activity
3.4. Summary of Antidiabetic Potential of Tested Herbal Blends
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Diabetes. Available online: https://www.who.int/news-room/fact-sheets/detail/diabetes (accessed on 4 November 2021).
- Wierusz-Wysocka, B.; Araszkiewicz, A.; Schlaffke, J. Końcowe produkty glikacji—Nowy biomarker cukrzycy i jej powikłań? Clin. Diabetol. 2013, 2, 96–103. [Google Scholar]
- Abdulmalik, H.; Tadiwos, Y.; Legese, N. Assessment of drug-related problems among type 2 diabetic patients on follow up at Hiwot Fana Specialized University Hospital, Harar, Eastern Ethiopia. BMC Res. Notes 2019, 12, 771. [Google Scholar] [CrossRef] [PubMed]
- Latek, D.; Rutkowska, E.; Niewieczerzal, S.; Cielecka-Piontek, J. Drug-induced diabetes type 2: In silico study involving class B GPCRs. PLoS ONE 2019, 14, e0208892. [Google Scholar] [CrossRef]
- Pasznik, P.; Rutkowska, E.; Niewieczerzal, S.; Cielecka-Piontek, J.; Latek, D. Potential off-target effects of beta-blockers on gut hormone receptors: In silico study including GUT-DOCK—A web service for small-molecule docking. PLoS ONE 2019, 14, e0210705. [Google Scholar] [CrossRef] [PubMed]
- Deacon, C.F.; Lebovitz, H.E. Comparative review of dipeptidyl peptidase-4 inhibitors and sulphonylureas. Diabetes Obes. Metab. 2016, 18, 333–347. [Google Scholar] [CrossRef]
- Sonia, T.A.; Sharma, C.P. Oral Delivery of Insulin; Elsevier: Cambridge, UK, 2014; ISBN 1908818689. [Google Scholar]
- Stamataki, N.S.; Yanni, A.E.; Karathanos, V.T. Bread making technology influences postprandial glucose response: A review of the clinical evidence. Br. J. Nutr. 2017, 117, 1001–1012. [Google Scholar] [CrossRef] [PubMed]
- Babu, P.V.A.; Liu, D.; Gilbert, E.R. Recent advances in understanding the anti-diabetic actions of dietary flavonoids. J. Nutr. Biochem. 2013, 24, 1777–1789. [Google Scholar] [CrossRef]
- Purohit, P.; Mishra, B. Systematic review on interaction studies of synthetic antidiabetic drugs and herbal therapies. J. Pharm. Res. 2017, 16, 86–94. [Google Scholar] [CrossRef]
- EMA. European Medicines Agency. Committee on Herbal Medicinal Products (HMPC). Available online: https://www.ema.europa.eu/en/committees/committee-herbal-medicinal-products-hmpc (accessed on 30 April 2021).
- Vinayagam, R.; Xu, B. Antidiabetic properties of dietary flavonoids: A cellular mechanism review. Nutr. Metab. 2015, 12, 1–20. [Google Scholar] [CrossRef]
- Studzińska-Sroka, E.; Dudek-Makuch, M.; Chanaj-Kaczmarek, J.; Czepulis, N.; Korybalska, K.; Rutkowski, R.; Łuczak, J.; Grabowska, K.; Bylka, W.; Witowski, J. Anti-inflammatory Activity and Phytochemical Profile of Galinsoga Parviflora Cav. Molecules 2018, 23, 2133. [Google Scholar] [CrossRef]
- Makowska-Wąs, J.; Galanty, A.; Gdula-Argasińska, J.; Tyszka-Czochara, M.; Szewczyk, A.; Nunes, R.; Carvalho, I.S.; Michalik, M.; Paśko, P. Identification of predominant phytochemical compounds and cytotoxic activity of wild olive leaves (Olea europaea L. ssp. sylvestris) harvested in south Portugal. Chem. Biodivers. 2017, 14, e1600331. [Google Scholar] [CrossRef] [PubMed]
- Studzińska-Sroka, E.; Czapska, I.; Bylka, W. Biological Activity and Polyphenol Content in Selected Herbal Tea Blends Used in Diabetes. Acta Pol. Pharm. Res. 2019, 76, 1037–1042. [Google Scholar]
- Dinis, T.C.P.; Madeira, V.M.C.; Almeida, L.M. Action of phenolic derivatives (acetaminophen, salicylate, and 5-aminosalicylate) as inhibitors of membrane lipid peroxidation and as peroxyl radical scavengers. Arch. Biochem. Biophys. 1994, 315, 161–169. [Google Scholar] [CrossRef]
- Widodo, W.S.; Widowati, W.; Ginting, C.N.; Lister, I.; Armansyah, A.; Girsang, E. Comparison of antioxidant and anti-collagenase activity of genistein and epicatechin. Pharm. Sci. Res. 2019, 6, 6. [Google Scholar]
- Hunyadi, A.; Martins, A.; Hsieh, T.J.; Seres, A.; Zupkó, I. Chlorogenic Acid and Rutin Play a Major Role in the In Vivo Anti-Diabetic Activity of Morus alba Leaf Extract on Type II Diabetic Rats. PLoS ONE 2012, 7, e50619. [Google Scholar] [CrossRef]
- Frizzell, N.; Baynes, J.W. Chelation therapy for the management of diabetic complications: A hypothesis and a proposal for clinical laboratory assessment of metal ion homeostasis in plasma. Clin. Chem. Lab. Med. 2014, 52, 69–75. [Google Scholar] [CrossRef]
- European Pharmacopoeia, 10th ed.; Council of Europe: Strasbourg, France, 2019; p. 1390, 1407–1409, 1551.
- Brown, A.; Anderson, D.; Racicot, K.; Pilkenton, S.J.; Apostolidis, E. Evaluation of Phenolic Phytochemical Enriched Commercial Plant Extracts on the In Vitro Inhibition of α-Glucosidase. Front. Nutr. 2017, 4, 56. [Google Scholar] [CrossRef] [PubMed]
- Domínguez Avila, J.A.; Rodrigo García, J.; González Aguilar, G.A.; de la Rosa, L.A. The Antidiabetic Mechanisms of Polyphenols Related to Increased Glucagon-Like Peptide-1 (GLP1) and Insulin Signaling. Molecules 2017, 22, 903. [Google Scholar] [CrossRef]
- Guo, H.; Xia, M.; Zou, T.; Ling, W.; Zhong, R.; Zhang, W. Cyanidin 3-glucoside attenuates obesity-associated insulin resistance and hepatic steatosis in high-fat diet-fed and db/db mice via the transcription factor FoxO1. J. Nutr. Biochem. 2012, 23, 349–360. [Google Scholar] [CrossRef] [PubMed]
- Kawser Hossain, M.; Abdal Dayem, A.; Han, J.; Yin, Y.; Kim, K.; Kumar Saha, S.; Yang, G.-M.; Choi, H.Y.; Cho, S.-G. Molecular Mechanisms of the Anti-Obesity and Anti-Diabetic Properties of Flavonoids. Int. J. Mol. Sci. 2016, 17, 569. [Google Scholar] [CrossRef] [PubMed]
- Kopustinskiene, D.M.; Jakstas, V.; Savickas, A.; Bernatoniene, J. Flavonoids as Anticancer Agents. Nutrients 2020, 12, 457. [Google Scholar] [CrossRef]
- Peng, C.-H.; Lin, H.-T.; Chung, D.-J.; Huang, C.-N.; Wang, C.-J. Mulberry leaf extracts prevent obesity-induced NAFLD with regulating adipocytokines, inflammation and oxidative stress. J. Food Drug Anal. 2018, 26, 778–787. [Google Scholar] [CrossRef]
- Yan, Y.; Zhou, X.; Guo, K.; Zhou, F.; Yang, H. Use of Chlorogenic Acid against Diabetes Mellitus and Its Complications. J. Immunol. Res. 2020, 2020, 9680508. [Google Scholar] [CrossRef]
- Naveed, M.; Hejazi, V.; Abbas, M.; Kamboh, A.A.; Khan, G.J.; Shumzaid, M.; Ahmad, F.; Babazadeh, D.; FangFang, X.; Modarresi-Ghazani, F.; et al. Chlorogenic acid (CGA): A pharmacological review and call for further research. Biomed. Pharmacother. 2018, 97, 67–74. [Google Scholar] [CrossRef]
- Zuñiga, L.Y.; Aceves-de la Mora, M.C.A.; González-Ortiz, M.; Ramos-Núñez, J.L.; Martínez-Abundis, E. Effect of Chlorogenic Acid Administration on Glycemic Control, Insulin Secretion, and Insulin Sensitivity in Patients with Impaired Glucose Tolerance. J. Med. Food 2018, 21, 469–473. [Google Scholar] [CrossRef]
- Adefegha, S.A.; Oboh, G.; Ejakpovi, I.I.; Oyeleye, S.I. Antioxidant and antidiabetic effects of gallic and protocatechuic acids: A structure–function perspective. Comp. Clin. Pathol. 2015, 24, 1579–1585. [Google Scholar] [CrossRef]
- Patel, S.S.; Goyal, R.K. Cardioprotective effects of gallic acid in diabetes-induced myocardial dysfunction in rats. Pharmacogn. Res. 2011, 3, 239–245. [Google Scholar] [CrossRef]
- Polumackanycz, M.; Wesolowski, M.; Viapiana, A. Morus alba L. and Morus nigra L. Leaves as a Promising Food Source of Phenolic Compounds with Antioxidant Activity. Plant Foods Hum. Nutr. 2021, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Miyake, K.; Arima, H.; Hirayama, F.; Yamamoto, M.; Horikawa, T.; Sumiyoshi, H.; Noda, S.; Uekama, K. Improvement of solubility and oral bioavailability of rutin by complexation with 2-hydroxypropyl-beta-cyclodextrin. Pharm. Dev. Technol. 2000, 5, 399–407. [Google Scholar] [CrossRef]
- Kim, G.-N.; Jang, H.-D. Flavonol content in the water extract of the mulberry (Morus alba L.) leaf and their antioxidant capacities. J. Food Sci. 2011, 76, C869–C873. [Google Scholar] [CrossRef] [PubMed]
- Hwang, S.H.; Li, H.M.; Lim, S.S.; Wang, Z.; Hong, J.-S.; Huang, B. Evaluation of a standardized extract from morus alba against α-glucosidase inhibitory effect and postprandial antihyperglycemic in patients with impaired glucose tolerance: A randomized double-blind clinical trial. Evid. Based Complementary Altern. Med. 2016, 2016, 8983232. [Google Scholar] [CrossRef]
- Dabur, R.; Sharma, B.; Mittal, A. Mechanistic approach of anti-diabetic compounds identified from natural sources. Chem. Biol. Lett. 2018, 5, 63–99. [Google Scholar]
- Zheng, Y.; Yang, W.; Sun, W.; Chen, S.; Liu, D.; Kong, X.; Tian, J.; Ye, X. Inhibition of porcine pancreatic α-amylase activity by chlorogenic acid. J. Funct. Foods 2020, 64, 103587. [Google Scholar] [CrossRef]
- Dubey, S.; Ganeshpurkar, A.; Ganeshpurkar, A.; Bansal, D.; Dubey, N. Glycolytic enzyme inhibitory and antiglycation potential of rutin. Future J. Pharm. Sci. 2017, 3, 158–162. [Google Scholar] [CrossRef]
- Ranilla, L.G.; Kwon, Y.-I.; Apostolidis, E.; Shetty, K. Phenolic compounds, antioxidant activity and in vitro inhibitory potential against key enzymes relevant for hyperglycemia and hypertension of commonly used medicinal plants, herbs and spices in Latin America. Bioresour. Technol. 2010, 101, 4676–4689. [Google Scholar] [CrossRef] [PubMed]
- Adisakwattana, S.; Lerdsuwankij, O.; Poputtachai, U.; Minipun, A.; Suparpprom, C. Inhibitory activity of cinnamon bark species and their combination effect with acarbose against intestinal α-glucosidase and pancreatic α-amylase. Plant Foods Hum. Nutr. 2011, 66, 143–148. [Google Scholar] [CrossRef]
- Adisakwattana, S. Cinnamic Acid and Its Derivatives: Mechanisms for Prevention and Management of Diabetes and Its Complications. Nutrients 2017, 9, 163. [Google Scholar] [CrossRef]
- Lin, G.-M.; Chen, Y.-H.; Yen, P.-L.; Chang, S.-T. Antihyperglycemic and antioxidant activities of twig extract from Cinnamomum osmophloeum. J. Tradit. Complementary Med. 2016, 6, 281–288. [Google Scholar] [CrossRef]
- Tao, Y.; Zhang, Y.; Cheng, Y.; Wang, Y. Rapid screening and identification of α-glucosidase inhibitors from mulberry leaves using enzyme-immobilized magnetic beads coupled with HPLC/MS and NMR. Biomed. Chromatogr. 2013, 27, 148–155. [Google Scholar] [CrossRef] [PubMed]
- Sui, X.; Zhang, Y.; Zhou, W. In vitro and in silico studies of the inhibition activity of anthocyanins against porcine pancreatic α-amylase. J. Funct. Foods 2016, 21, 50–57. [Google Scholar] [CrossRef]
- Barik, S.K.; Russell, W.R.; Moar, K.M.; Cruickshank, M.; Scobbie, L.; Duncan, G.; Hoggard, N. The anthocyanins in black currants regulate postprandial hyperglycaemia primarily by inhibiting α-glucosidase while other phenolics modulate salivary α-amylase, glucose uptake and sugar transporters. J. Nutr. Biochem. 2020, 78, 108325. [Google Scholar] [CrossRef]
- Boath, A.S.; Stewart, D.; McDougall, G.J. Berry components inhibit α-glucosidase in vitro: Synergies between acarbose and polyphenols from black currant and rowanberry. Food Chem. 2012, 135, 929–936. [Google Scholar] [CrossRef] [PubMed]
- Chokki, M.; Cudălbeanu, M.; Zongo, C.; Dah-Nouvlessounon, D.; Ghinea, I.O.; Furdui, B.; Raclea, R.; Savadogo, A.; Baba-Moussa, L.; Avamescu, S.M. Exploring antioxidant and enzymes (A-amylase and B-Glucosidase) inhibitory activity of Morinda lucida and Momordica charantia leaves from Benin. Foods 2020, 9, 434. [Google Scholar] [CrossRef]
- Castro-Acosta, M.L.; Smith, L.; Miller, R.J.; McCarthy, D.I.; Farrimond, J.A.; Hall, W.L. Drinks containing anthocyanin-rich blackcurrant extract decrease postprandial blood glucose, insulin and incretin concentrations. J. Nutr. Biochem. 2016, 38, 154–161. [Google Scholar] [CrossRef]
- Tsui, P.-F.; Lin, C.-S.; Ho, L.-J.; Lai, J.-H. Spices and atherosclerosis. Nutrients 2018, 10, 1724. [Google Scholar] [CrossRef]
- Jin, Q.; Yang, J.; Ma, L.; Wen, D.; Chen, F.; Li, J. Identification of polyphenols in mulberry (genus Morus) cultivars by liquid chromatography with time-of-flight mass spectrometer. J. Food Compos. Anal. 2017, 63, 55–64. [Google Scholar] [CrossRef]
- Ouyang, P.; Gottlieb, S.H.; Culotta, V.L.; Navas-Acien, A. EDTA chelation therapy to reduce cardiovascular events in persons with diabetes. Curr. Cardiol. Rep. 2015, 17, 1–9. [Google Scholar] [CrossRef]
- Lakey-Beitia, J.; Burillo, A.M.; La Penna, G.; Hegde, M.L.; Rao, K.S. Polyphenols as Potential Metal Chelation Compounds Against Alzheimer’s Disease. J. Alzheimer’s Dis. 2021, 82, S335–S357. [Google Scholar] [CrossRef] [PubMed]
- Santana-Gálvez, J.; Cisneros-Zevallos, L.; Jacobo-Velázquez, D.A. Chlorogenic Acid: Recent Advances on Its Dual Role as a Food Additive and a Nutraceutical against Metabolic Syndrome. Molecules 2017, 22, 358. [Google Scholar] [CrossRef] [PubMed]
- Sharma, U.K.; Sharma, A.K.; Pandey, A.K. Medicinal attributes of major phenylpropanoids present in cinnamon. BMC Complementary Altern. Med. 2016, 16, 156. [Google Scholar] [CrossRef] [PubMed]
- Łabuda, H.; Buczkowska, H.; Papliński, R.; Najda, A. Secondary metabolites of Phaseoli pericarpium. Acta Sci. Pol. Hortorum Cultus 2017, 16, 187–200. [Google Scholar] [CrossRef]
- Druzynska, B.; Klepacka, M. Wlasciwosci przeciwutleniajace preparatow polifenoli otrzymanych z okrywy nasiennej fasoli czarnej, rozowej i bialej [Phaseolus]. Żywność Nauka Technol. Jakość 2004, 11, 69–78. [Google Scholar]
- Adhikari, B.M.; Bajracharya, A.; Shrestha, A.K. Comparison of nutritional properties of Stinging nettle (Urtica dioica) flour with wheat and barley flours. Food Sci. Nutr. 2016, 4, 119–124. [Google Scholar] [CrossRef]
- Otles, S.; Yalcin, B. Phenolic compounds analysis of root, stalk, and leaves of nettle. Sci. World J. 2012, 2012, 564367. [Google Scholar] [CrossRef]
- Carrasco-Castilla, J.; Hernández-Álvarez, A.J.; Jiménez-Martínez, C.; Jacinto-Hernández, C.; Alaiz, M.; Girón-Calle, J.; Vioque, J.; Dávila-Ortiz, G. Antioxidant and metal chelating activities of peptide fractions from phaseolin and bean protein hydrolysates. Food Chem. 2012, 135, 1789–1795. [Google Scholar] [CrossRef]
- Gülçin, I.; Küfrevioglu, O.I.; Oktay, M.; Büyükokuroglu, M.E. Antioxidant, antimicrobial, antiulcer and analgesic activities of nettle (Urtica dioica L.). J. Ethnopharmacol. 2004, 90, 205–215. [Google Scholar] [CrossRef] [PubMed]
- Balci Yuce, H.; Karatas, Ö.; Tulu, F.; Altan, A.; Gevrek, F. Effect of diabetes on collagen metabolism and hypoxia in human gingival tissue: A stereological, histopathological, and immunohistochemical study. Biotech. Histochem. 2019, 94, 65–73. [Google Scholar] [CrossRef]
- Pradeepkumar Singh, L.; Vivek Sharma, A.; Swarnakar, S. Upregulation of collagenase-1 and-3 in indomethacin-induced gastric ulcer in diabetic rats: Role of melatonin. J. Pineal Res. 2011, 51, 61–74. [Google Scholar] [CrossRef] [PubMed]
- Thrailkill, K.M.; Bunn, R.C.; Moreau, C.S.; Cockrell, G.E.; Simpson, P.M.; Coleman, H.N.; Frindik, J.P.; Kemp, S.F.; Fowlkes, J.L. Matrix metalloproteinase-2 dysregulation in type 1 diabetes. Diabetes Care 2007, 30, 2321–2326. [Google Scholar] [CrossRef]
- Drankowska, J.; Kos, M.; Kościuk, A.; Marzęda, P.; Boguszewska-Czubara, A.; Tylus, M.; Święch-Zubilewicz, A. MMP targeting in the battle for vision: Recent developments and future prospects in the treatment of diabetic retinopathy. Life Sci. 2019, 229, 149–156. [Google Scholar] [CrossRef]
- Kozakova, M.; Morizzo, C.; Goncalves, I.; Natali, A.; Nilsson, J.; Palombo, C. Cardiovascular organ damage in type 2 diabetes mellitus: The role of lipids and inflammation. Cardiovasc. Diabetol. 2019, 18, 1–11. [Google Scholar] [CrossRef]
- Anuar, N.N.M.; Zulkafali, N.I.N.; Ugusman, A. Modulation of Matrix Metalloproteinases by Plant-derived Products. Curr. Cancer Drug Targets 2021, 21, 91–106. [Google Scholar] [CrossRef] [PubMed]
- Shukri, S.M.; Pardi, F.; Sidik, N.J. In Vitro anti-collagenase activity and total phenolic content of five selected herbs: A review. Sci. Lett. 2021, 15, 117–127. [Google Scholar] [CrossRef]
- Thring, T.S.A.; Hili, P.; Naughton, D.P. Anti-collagenase, anti-elastase and anti-oxidant activities of extracts from 21 plants. BMC Complementary Altern. Med. 2009, 9, 27. [Google Scholar] [CrossRef]
- Wittenauer, J.; Mäckle, S.; Sußmann, D.; Schweiggert-Weisz, U.; Carle, R. Inhibitory effects of polyphenols from grape pomace extract on collagenase and elastase activity. Fitoterapia 2015, 101, 179–187. [Google Scholar] [CrossRef] [PubMed]
- Salam, M.A.; Al-Zhrani, G.; Kosa, S.A. Simultaneous removal of copper(II), lead(II), zinc(II) and cadmium(II) from aqueous solutions by multi-walled carbon nanotubes. C. R. Chim. 2012, 15, 398–408. [Google Scholar] [CrossRef]
- Choi, E.-Y.; Kim, E.-H.; Lee, J.-B.; Do, E.-J.; Kim, S.-J.; Kim, S.-H.; Park, J.-Y.; Lee, J.-T. Mechanisms for anti-wrinkle activities from fractions of Black Chokeberries. J. Life Sci. 2016, 26, 34–41. [Google Scholar] [CrossRef]

| Herbal Blend | Herbals Content of the Preparations |
|---|---|
| HB1 | Mori albi folium 100% |
| HB2 | Mori albi folium 25%, Phaseoli pericarpium 25%, Fagopyrum esculentum squama 25%, Taraxaci radix 12.5%, Urticae folium 12.5% |
| HB3 | Phaseoli pericarpium 40%, Urticae herba 17%, Mori albi folium 15%, Taraxaci herba 15%, Graminis rhizoma 13% |
| HB4 | Phaseoli pericarpium 40%, Urticae herba vel Urticae folium 30%, Graminis rhizoma 20%, Taraxaci herba et radix 10% |
| HB5 | Mori albi folium 70%, Cinnamomi cortex 30% |
| HB6 | Mori albi folium 95%, Cinnamomi cortex 5% |
| HB7 | Ribes nigrum fructus 29%, Aronia fructus 29%, Mali fructus 26%, Mori albi folium 15,4%, Fagopyrum esculentum squama 0.3%, Phaseoli pericarpium 0.3% |
| Herbal Blend | Content of Active Substances | Content of Active Substances in the Daily Dose Recommended by the Manufacturer | ||
|---|---|---|---|---|
| TPC (mg GAE/g HB) | TFC (mg QE/g HB) | Polyphenols (mg/day) | Flavonoids (mg/day) | |
| HB1 | 14.94 ± 0.24 | 3.06 ± 0.05 | 89.64 | 18.36 |
| HB2 | 15.30 ± 0.30 | 1.30 ± 0.06 | 61.20 | 5.20 |
| HB3 | 11.89 ± 0.36 | 1.43 ± 0.05 | 35.67 | 4.29 |
| HB4 | 3.83 ± 0.17 | 0.56 ± 0.06 | 30.64 | 4.48 |
| HB5 | 16.06 ± 0.63 | 2.23 ± 0.03 | 96.36 | 13.38 |
| HB6 | 13.97 ± 0.53 | 2.03 ± 0.03 | 83.82 | 12.18 |
| HB7 | 10.92 ± 0.42 | 1.08 ± 0.07 | 98.28 | 9.72 |
| Herbal Blend | Content of Selected Polyphenolic Compounds (mg/g Herbal Blend) | |||
|---|---|---|---|---|
| Chlorogenic Acid | Gallic Acid | Protocatechuic Acid | Rutin | |
| HB1 | 1.490 ± 0.057 | 0.275 ± 0.009 | 0.060 ± 0.010 | 0.236 ± 0.015 |
| HB2 | 0.474 ± 0.026 | 0.079 ± 0.007 | 0.040 ± 0.010 | 0.071 ± 0.007 |
| HB3 | 0.722 ± 0.040 | 0.046 ± 0.003 | n.a. | 0.058 ± 0.010 |
| HB4 | 0.079 ± 0.009 | n.a. | 0.070 ± 0.010 | 0.043 ± 0.006 |
| HB5 | 0.407 ± 0.028 | 0.462 ± 0.014 | n.a. | 0.029 ± 0.008 |
| HB6 | 0.107 ± 0.015 | 0.363 ± 0.021 | 0.147 ± 0.015 | n.a. |
| HB7 | 1.896 ± 0.143 | 0.066 ± 0.009 | n.a. | 0.100 ± 0.023 |
| Herbal Blend | Inhibition of α-Glucosidase Activity [%] | |||
| Concentration | ||||
| 1.7 mg/mL | 3.3 mg/mL | 6.7 mg/mL | 13.3 mg/mL | |
| HB1 | 35.26 ± 1.11 | 83.02 ± 1.72 | 92.82 ± 0.52 | 98.84 ± 1.48 |
| HB2 | 6.73 ± 1.23 | 12.43 ± 2.28 | 44.60 ± 1.03 | 68.49 ± 4.69 |
| HB3 | 6.91 ± 0.80 | 17.86 ± 5.81 | 29.70 ± 1.12 | 57.30 ± 5.55 |
| HB4 | 2.87 ± 0.95 | 8.83 ± 0.50 | 17.13 ± 2.00 | 37.38 ± 3.59 |
| HB5 | 93.65 ± 1.11 | 98.06 ± 0.90 | 99.78 ± 0.24 | 100.00 |
| HB6 | 48.66 ± 3.51 | 73.71 ± 0.55 | 81.81 ± 1.78 | 88.14 ± 1.14 |
| HB7 | 86.97 ± 5.63 | 97.27 ± 0.37 | 99.82 ± 0.26 | 99.22 ± 0.94 |
| Acarbose | 80.83 ± 1.02 | 88.07 ± 0.77 | 91.98 ± 0.17 | 93.73 ± 0.03 |
| Active Compound | Concentration | |||
| 0.17 mg/mL | 0.33 mg/mL | 3.3 mg/mL | 6.7 mg/mL | |
| Chlorogenic acid | 46.44 ± 1.02 | 81.35 ± 3.34 | n.d. | n.d. |
| Gallic acid | n.d. | n.d. | 18.00 ± 5.09 | 99.65 ± 2.34 |
| Protocatechuic acid | n.d. | n.d. | 0.46 ± 1.42 | 99.99 ± 0.13 |
| Rutin | 65.33 ± 3.42 | 97.07 ± 0.55 | n.d. | n.d. |
| Herbal Blend | Inhibition of α-Amylase Activity [%] | |
|---|---|---|
| Concentration | ||
| 26.7 mg/mL | 0.00267 mg/mL | |
| HB1 | 3.62 ± 4.95 | n.d. |
| HB2 | 4.02 ± 3.96 | n.d. |
| HB3 | 0.31 ± 0.77 | n.d. |
| HB4 | 0.13 ± 0.31 | n.d. |
| HB5 | 20.14 ± 5.94 | n.d. |
| HB6 | 5.62 ± 7.32 | n.d. |
| HB7 | 96.16 ± 6.00 | n.d. |
| Acarbose | n.d. | 28.11 ± 2.80 |
| Herbal Blend | Antioxidant Activity | |
|---|---|---|
| DPPH• (IC50 µg/mL) 1 | CUPRAC (IC0.5 µg/mL) 1 | |
| HB1 | 310.03 | 368.15 |
| HB2 | 715.58 | 686.43 |
| HB3 | 744.74 | 680.14 |
| HB4 | 1336.03 | 931.00 |
| HB5 | 350.52 | 344.43 |
| HB6 | 394.76 | 409.92 |
| HB7 | 361.17 | 591.50 |
| vitamin C | 7.62 | 14.64 |
| Herbal Blend | Chelating Activity Fe2+ [%] | ||||
|---|---|---|---|---|---|
| Concentration | |||||
| 0.45 mg/mL | 0.9 mg/mL | 2.3 mg/mL | 4.6 mg/mL | 9.1 mg/mL | |
| HB1 | 43.92 ± 1.34 | 70.36 ± 7.02 | 92.01 ± 0.68 | 95.55 ± 0.63 | 99.34 ± 1.38 |
| HB2 | 27.53 ± 3.05 | 51.16 ± 1.80 | 89.49 ± 2.45 | 89.85 ± 1.75 | 87.98 ± 0.10 |
| HB3 | 56.38 ± 5.93 | 89.47 ± 1.74 | 96.58 ± 0.79 | 96.15 ± 1.23 | 97.11 ± 0.57 |
| HB4 | 62.81 ± 1.72 | 88.31 ± 0.35 | 94.05 ± 0.48 | 94.35 ± 0.28 | 93.21 ± 0.53 |
| HB5 | 34.15 ± 1.14 | 67.49 ± 1.90 | 94.11 ± 0.58 | 94.65 ± 0.42 | 97.15 ± 1.64 |
| HB6 | 62.10 ± 3.16 | 91.10 ± 1.17 | 98.38 ± 0.54 | 98.41 ± 1.06 | 99.44 ± 2.99 |
| HB7 | n.a. | n.a. | 5.91 ± 4.33 | 9.43 ± 4.72 | 9.33 ± 3.19 |
| Reference | Concentration | ||||
| 0.01 mg/mL | 0.023 mg/mL | 0.045 mg/mL | - | - | |
| EDTA | 66.50 ± 2.20 | 99.59 ± 0.57 | 100.24 ± 0.20 | - | - |
| Herbal Blend | Inhibition of Collagenase Activity [%] | ||
|---|---|---|---|
| Concentration | |||
| 2.4 mg/mL | 0.24 mg/mL | 0.024 mg/mL | |
| HB1 | 16.22 ± 3.22 | n.d. | n.d. |
| HB2 | 21.46 ± 3.04 | n.d. | n.d. |
| HB3 | n.a. | n.d. | n.d. |
| HB4 | 8.47 ± 4.66 | n.d. | n.d. |
| HB5 | 28.79 ± 2.65 | n.d. | n.d. |
| HB6 | 13.68 ± 6.21 | n.d. | n.d. |
| HB7 | 18.42 ± 7.68 | n.d. | n.d. |
| EGCG | n.d. | 84.30 ± 8.83 | 35.78 ± 5.52 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Studzińska-Sroka, E.; Galanty, A.; Gościniak, A.; Wieczorek, M.; Kłaput, M.; Dudek-Makuch, M.; Cielecka-Piontek, J. Herbal Infusions as a Valuable Functional Food. Nutrients 2021, 13, 4051. https://doi.org/10.3390/nu13114051
Studzińska-Sroka E, Galanty A, Gościniak A, Wieczorek M, Kłaput M, Dudek-Makuch M, Cielecka-Piontek J. Herbal Infusions as a Valuable Functional Food. Nutrients. 2021; 13(11):4051. https://doi.org/10.3390/nu13114051
Chicago/Turabian StyleStudzińska-Sroka, Elżbieta, Agnieszka Galanty, Anna Gościniak, Mateusz Wieczorek, Magdalena Kłaput, Marlena Dudek-Makuch, and Judyta Cielecka-Piontek. 2021. "Herbal Infusions as a Valuable Functional Food" Nutrients 13, no. 11: 4051. https://doi.org/10.3390/nu13114051
APA StyleStudzińska-Sroka, E., Galanty, A., Gościniak, A., Wieczorek, M., Kłaput, M., Dudek-Makuch, M., & Cielecka-Piontek, J. (2021). Herbal Infusions as a Valuable Functional Food. Nutrients, 13(11), 4051. https://doi.org/10.3390/nu13114051