Plant-Derived Lactobacillus paracasei IJH-SONE68 Improves Chronic Allergy Status: A Randomized, Double-Blind, Placebo-Controlled Clinical Trial
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Study Capsules and Placebo
2.3. Study Design
2.4. Statistical Analysis
3. Results
3.1. Recruitment of Subjects
3.2. Effects of IJH-SONE68 on Primary Outcomes
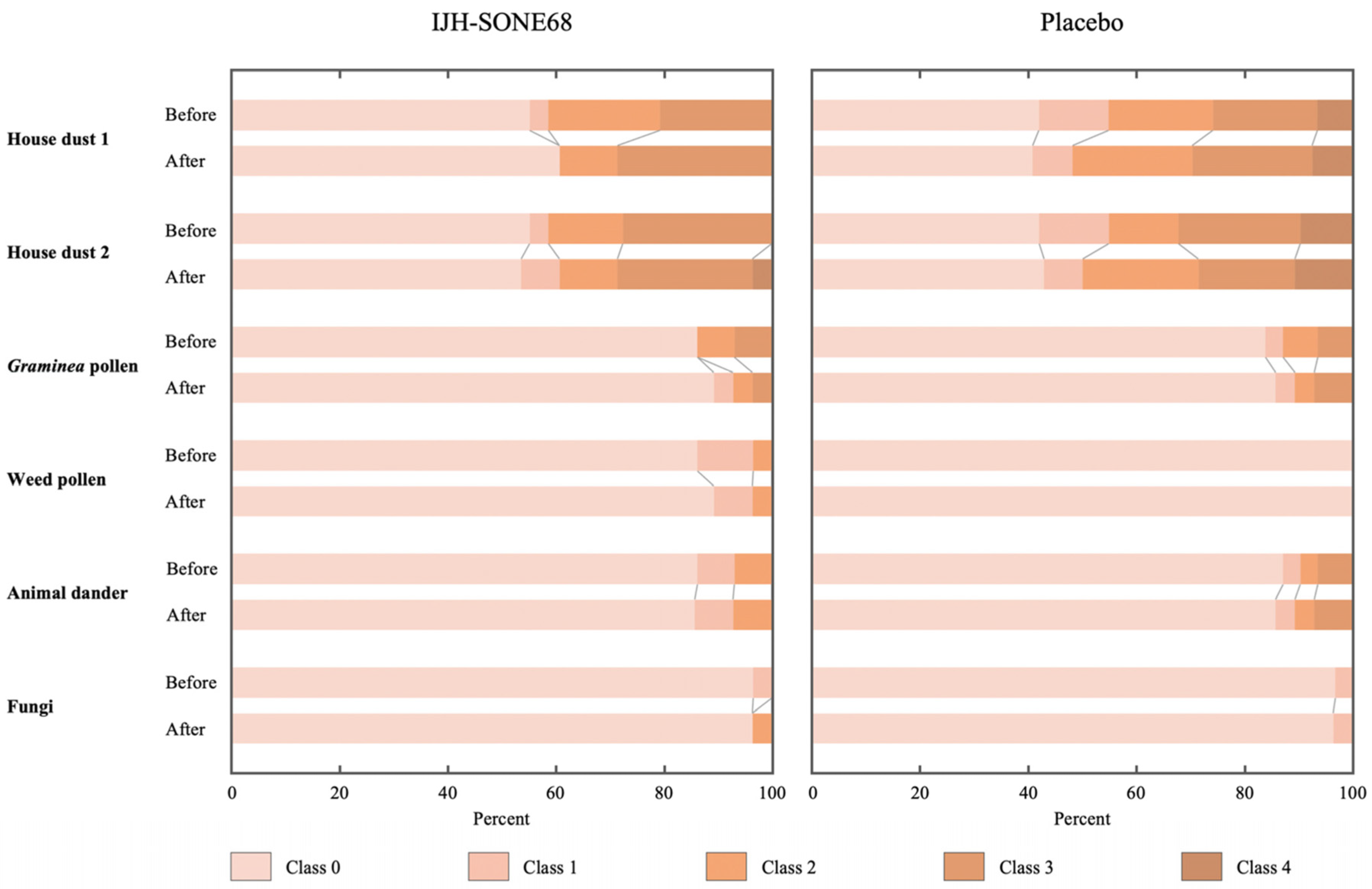
3.3. Effects of IJH-SONE68 on Secondary Outcomes
3.4. Monitoring the Adverse Effects
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Liva, G.A.; Karatzanis, A.D.; Prokopakis, E.P. Review of rhinitis: Classification, types, pathophysiology. J. Clin. Med. 2021, 10, 3183. [Google Scholar] [CrossRef]
- Barnes, P.J. Pathophysiology of allergic inflammation. Immunol. Rev. 2011, 242, 31–50. [Google Scholar] [CrossRef]
- Fan, P.S.; Sun, M.J.; Qin, D.; Yuan, C.S.; Chen, X.G.; Liu, Y. Nanosystems as curative platforms for allergic disorder management. J. Mater. Chem. B. 2021, 9, 1729–1744. [Google Scholar] [CrossRef]
- Mandhane, S.N.; Shah, J.H.; Thennati, R. Allergic rhinitis: An update on disease, present treatments and future prospects. Int. Immunopharmacol. 2011, 11, 1646–1662. [Google Scholar] [CrossRef]
- Settipane, R.A.; Charnock, D.R. Epidemiology of rhinitis: Allergic and nonallergic. Clin. Allergy Immunol. 2007, 19, 23–34. [Google Scholar]
- Okubo, K.; Kurono, Y.; Ichimura, K.; Enomoto, T.; Okamoto, Y.; Kawauchi, H.; Suzaki, H.; Fujieda, S.; Masuyama, K.; The Japanese Society of Allergology. Japanese guidelines for allergic rhinitis 2020. Allergol. Int. 2020, 69, 331–345. [Google Scholar] [CrossRef]
- Liu, W.; Pang, H.; Zhang, H.; Cai, Y. Biodiversity of lactic acid bacteria. In Bacteria Fundamentals and Practice; Zhang, H., Cai, Y., Eds.; Springer: Heidelberg, Germany, 2014; pp. 103–203. [Google Scholar]
- Cotter, P.D.; Ross, P.R.; Hill, C. Bacteriocins—a viable alternative to antibiotics? Nat. Rev. Microbiol. 2013, 11, 95–105. [Google Scholar] [CrossRef]
- Adolfsson, O.; Meydani, S.N.; Russell, R.M. Yogurt and gut function. Am. J. Clin. Nutr. 2004, 80, 245–256. [Google Scholar] [CrossRef]
- Sanders, M.E. Probiotics: Definition, source, selection, and uses. Clin. Infect. Dis. 2008, 46, S58–S61. [Google Scholar] [CrossRef]
- Higashikawa, F.; Noda, M.; Awaya, T.; Nomura, K.; Oku, H.; Sugiyama, M. Improvement of constipation and liver function by plant-derived lactic acid bacteria: A double-blind, randomized trial. Nutrition 2010, 26, 367–374. [Google Scholar] [CrossRef]
- Higashikawa, F.; Noda, M.; Awaya, T.; Danshiitsoodol, N.; Matoba, Y.; Kumagai, T.; Sugiyama, M. Antiobesity effect of Pediococcus pentosaceus LP28 on overweight subjects: A randomized, double-blind, placebo-controlled clinical trial. Eur. J. Clin. Nutr. 2016, 70, 582–587. [Google Scholar] [CrossRef]
- Higashikawa, F.; Danshiitsoodol, N.; Kanno, K.; Ishida, R.; Tazuma, S.; Sugiyama, M. Lactobacillus plantarum SN13T cells improve hepatic dysfunction and fecal microbiota: A randomized pilot study. Arch. Clin. Biomed. Res. 2020, 4, 605–625. [Google Scholar] [CrossRef]
- Yasutake, T.; Kumagai, T.; Inoue, A.; Kobayashi, K.; Noda, M.; Orikawa, A.; Matoba, Y.; Sugiyama, M. Characterization of the LP28 strain-specific exopolysaccharide biosynthetic gene cluster found in the whole circular genome of Pediococcus pentosaceus. Biochem. Biophys. Rep. 2016, 5, 271–299. [Google Scholar] [CrossRef]
- Panthavee, W.; Noda, M.; Danshiitsoodol, N.; Kumagai, T.; Sugiyama, M. Characterization of exopolysaccharides produced by thermophilic lactic acid bacteria isolated from tropical fruits of Thailand. Biol. Pharm. Bull. 2017, 40, 621–629. [Google Scholar] [CrossRef]
- Noda, M.; Shiraga, M.; Kumagai, T.; Danshiitsoodol, N.; Sugiyama, M. Characterization of the SN35N strain-specific exopolysaccharide encoded in the whole circular genome of a plant-derived Lactobacillus plantarum. Biol. Pharm. Bull. 2018, 41, 536–545. [Google Scholar] [CrossRef]
- Noda, M.; Sugimoto, S.; Hayashi, I.; Danshiitsoodol, N.; Fukamachi, M.; Sugiyama, M. A novel structure of exopolysaccharide produced by a plant-derived lactic acid bacterium Lactobacillus paracasei IJH-SONE68. J. Biochem. 2018, 164, 87–92. [Google Scholar] [CrossRef]
- Bourguignon, L.Y.; Wong, G.; Earle, C.A.; Xia, W. Interaction of low molecular weight hyaluronan with CD44 and toll-like receptors promotes the actin filament-associated protein 110-actin binding and MyD88-NFκB signaling leading to proinflammatory cytokine/chemokine production and breast tumor invasion. Cytoskeleton 2011, 68, 671–693. [Google Scholar] [CrossRef]
- Jiang, D.; Liang, J.; Noble, P.W. Hyaluronan in tissue injury and repair. Annu. Rev. Cell. Dev. Biol. 2007, 23, 435–461. [Google Scholar] [CrossRef]
- Litwiniuk, M.; Krejner, A.; Speyrer, M.S.; Gauto, A.R.; Grzela, T. Hyaluronic acid in inflammation and tissue regeneration. Wounds 2010, 28, 78–88. [Google Scholar]
- Turley, E.A.; Noble, P.W.; Bourguignon, L.Y. Signaling properties of hyaluronan receptors. J. Biol. Chem. 2002, 277, 4589–4592. [Google Scholar] [CrossRef]
- Yang, C.H.; Srivastava, P.N. Purification and properties of hyaluronidase from bull sperm. J. Biol. Chem. 1975, 250, 79–83. [Google Scholar] [CrossRef]
- Kakegawa, H.; Matsumoto, H.; Satoh, T. Activation of hyaluronidase by metallic salts and compound 48/80, and inhibitory effect of anti-allergic agents on hyaluronidase. Chem. Pharm. Bull. 1985, 33, 642–646. [Google Scholar] [CrossRef]
- Fujitani, N.; Sakai, S.; Yamaguchi, Y.; Takenaka, H. Inhibitory effects of microalgae on the activation of hyaluronidase. J. Appl. Phycol. 2001, 13, 489–492. [Google Scholar] [CrossRef]
- Maeda, Y.; Yamamoto, M.; Masui, T.; Sugiyama, K.; Yokota, M.; Nakagomi, K.; Tanaka, H.; Takahashi, T.; Kobayashi, E. Inhibitory effect of tea extracts on hyaluronidase. Shokuhin Eiseigaku Zashi 1990, 31, 233–237. [Google Scholar] [CrossRef]
- Noda, M.; Sultana, N.; Hayashi, I.; Fukamachi, M.; Sugiyama, M. Exopolysaccharide produced by Lactobacillus paracasei IJH-SONE68 prevents and improves the picryl chloride-induced contact dermatitis. Molecules 2019, 24, 2970. [Google Scholar] [CrossRef]
- Noda, M.; Danshiitsoodol, N.; Kanno, K.; Uchida, T.; Sugiyama, M. The exopolysaccharide produced by Lactobacillus paracasei IJH-SONE68 prevents and ameliorates inflammatory responses in DSS–induced ulcerative colitis. Microorganisms 2021, 9, 2243. [Google Scholar] [CrossRef]
- Okuda, M.; Okubo, K.; Gotoh, M.; Okamoto, Y.; Konno, A.; Baba, K.; Ogino, S.; Ishikawa, T.; Takenaka, H.; Soh, N.; et al. Standard questionnaire for QOL of Japanese patients with allergic rhinitis. Allergy 2003, 52, 21–56. [Google Scholar]
- Umehara, S.; Arima, H.; Arima, S.; Asayama, K.; Dohi, Y.; Hirooka, Y.; Horio, T.; Hoshide, S.; Ikeda, S.; Ishimitsu, T.; et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019). Hypertens. Res. 2019, 42, 1235–1481. [Google Scholar]
- Li, P.; Stuart, E.A.; Allison, D.B. Multiple imputation: A flexible tool for handling missing data. JAMA 2015, 314, 1966–1967. [Google Scholar] [CrossRef]
- Saleh, H.A.; Durham, S.R. Perennial rhinitis. BMJ 2007, 335, 502–507. [Google Scholar] [CrossRef]
- Bush, R.K. Etiopathogenesis and management of perennial allergic rhinitis: A state-of-the-art review. Treat. Respir. Med. 2004, 3, 45–57. [Google Scholar] [CrossRef] [PubMed]
- Inagaki, N.; Miura, T.; Nagai, H.; Koda, A. Active cutaneous anaphylaxis (ACA) in the mouse ear. Jpn. J. Pharmacol. 1992, 59, 201–208. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Noda, M.; Sugiyama, M. Studies aiming for the development of medicines to treat inflammatory disorders. Seibutsu-kogaku Kaishi 2021, 99. in press. [Google Scholar]
- Waugh, D.J.J.; Wilson, C. The interleukin-8 pathway in cancer. Clin. Cancer Res. 2008, 14, 6735–6741. [Google Scholar] [CrossRef] [PubMed]
- Acosta, J.C.; O’Loghlen, A.; Banito, A.; Guijarro, M.V.; Augert, A.; Raguz, S.; Fumagalli, M.; Da Costa, M.; Brown, C.; Popov, N.; et al. Chemokine signaling via the CXCR2 receptor reinforces senescence. Cell 2008, 133, 1006–1018. [Google Scholar] [CrossRef]
- Bernhard, S.; Hug, S.; Stratmann, A.E.P.; Erber, M.; Vidoni, L.; Knapp, C.L.; Thomaß, B.D.; Fauler, M.; Nilsson, B.; Nilsson Ekdahl, K.; et al. Interleukin 8 elicits rapid physiological changes in neutrophils that are altered by inflammatory conditions. J. Innate Immun. 2021, 13, 225–241. [Google Scholar] [CrossRef]
- Giannini, E.G.; Testa, R.; Savarino, V. Liver enzyme alteration: A guide for clinicians. CMAJ 2005, 172, 367–379. [Google Scholar] [CrossRef]
- Sharma, U.; Pai, D.; Prasad, R. Alkaline phosphatase: An overview. Indian J. Clin. Biochem. 2014, 29, 269–278. [Google Scholar] [CrossRef]
- Meng, F.; Yin, X.; Ma, X.; Guo, X.D.; Jin, B.; Li, H. Assessment of the value of serum cholinesterase as a liver function test for cirrhotic patients. Biomed. Rep. 2013, 1, 265–268. [Google Scholar] [CrossRef] [PubMed]
- Oda, E. Metabolic syndrome: Its history, mechanisms, and limitations. Acta Diabetol. 2012, 49, 89–95. [Google Scholar] [CrossRef]
- Oda, E. Associations between serum cholinesterase and incident hyper-LDL cholesterolemia, hypertriglyceridemia and hypo-HDL cholesterolemia as well as changes in lipid levels in a health screening population. Atherosclerosis 2015, 241, 1–5. [Google Scholar] [CrossRef] [PubMed]



| Score | Items | |||||
|---|---|---|---|---|---|---|
| Frequency of Sneezing (Average Times/Day) | Frequency of Blowing (Average Times/Day) | Nasal Congestion | Itchy Eyes | Watery Eyes | Head Dullness | |
| 0 | No sneezing | No sneezing | None of the time | None of the time | None of the time | None of the time |
| 1 | 1–5 | 1–5 | A little of the time (without mouth-breathing) | Mild | Mild | Mild |
| 2 | 6–10 | 6–10 | Some of the time (with mouth-breathing) | Moderate to severe | Moderate to severe | Moderate to severe |
| 3 | 11–20 | 11–20 | Most of the time (with mouth-breathing) | Severe | Severe | Severe |
| 4 | 21 or more | 21 or more | All of the time (with mouth-breathing) | Very severe | Very severe | Very severe |
| IJH-SONE68 (n = 29) | Placebo (n = 31) | p Value | |
|---|---|---|---|
| Age (years) | 51.6 ± 14.4 | 54.8 ± 10.5 | 0.331 |
| Male | 53.0 ± 17.4 (n = 7) | 56.3 ± 12.0 (n = 9) | 0.674 |
| Female | 51.1 ± 13.8 (n = 22) | 54.2 ± 10.1 (n = 22) | 0.408 |
| Height (cm) | 160.1 ± 9.6 | 160.0 ± 7.7 | 0.834 |
| Body weight (kg) | 55.4 ± 15.6 | 56.4 ± 12.4 | 0.796 |
| Systolic blood pressure (mmHg) | 110.1 ± 15.5 | 118.6 ± 16.9 | 0.067 |
| Diastolic blood pressure (mmHg) | 67.8 ± 11.2 | 73.5 ± 12.3 | 0.067 |
| IJH-SONE68 (n = 29) | Placebo (n = 31) | p Value | |
|---|---|---|---|
| Summary of self-questionnaire score | 0.008 | ||
| Baseline | 10.1 ± 0.6 | 9.5 ± 0.3 | |
| Change at 12 week | −3.6 ± 0.5 | −1.9 ± 0.5 | |
| VAS value | 0.380 | ||
| Baseline | 52.3 ± 2.7 | 57.4 ± 3.4 | |
| Change at 12 week | −17.6 ± 3.6 | −13.1 ± 3.5 |
| IJH-SONE68 (n = 29) | Placebo (n = 31) | p Value | ||
|---|---|---|---|---|
| Frequency of sneezing | <0.05 | |||
| Baseline | 1.9 ± 0.2 | 1.7 ± 0.2 | ||
| 12 week | 1.2 ± 0.2 | 1.5 ± 0.1 | ||
| Frequency of blowing | <0.05 | |||
| Baseline | 2.0 ± 0.2 | 2.0 ± 0.2 | ||
| 12 week | 1.3 ± 0.2 | 1.7 ± 0.2 | ||
| Nasal congestion | - | |||
| Baseline | 1.8 ± 0.1 | 1.9 ± 0.2 | ||
| 12 week | 1.3 ± 0.2 | 1.4 ± 0.2 | ||
| Itchy eyes | - | |||
| Baseline | 1.8 ± 0.2 | 1.5 ± 0.1 | ||
| 12 week | 1.0 ± 0.2 | 1.1 ± 0.1 | ||
| Watery eyes | <0.05 | |||
| Baseline | 1.1 ± 0.1 | 0.9 ± 0.1 | ||
| 12 week | 0.6 ± 0.1 | 0.9 ± 0.1 | ||
| Head dullness | <0.05 | |||
| Baseline | 1.6 ± 0.2 | 1.4 ± 0.2 | ||
| 12 week | 1.1 ± 0.2 | 1.1 ± 0.2 | ||
| IJH-SONE68 (n = 29) | Placebo (n = 31) | p Value | |
|---|---|---|---|
| Total IgE (log10 IU/mL) | 0.361 | ||
| Baseline | 1.87 ± 0.10 | 1.90 ± 0.10 | |
| Change at 12 week | −0.004 ± 0.019 | 0.021 ± 0.019 |
| Class | Specific IgE Titer (UA/mL) | Quantitative Analysis |
|---|---|---|
| 0 | <0.35 | Negative |
| 1 | 0.35 to <0.70 | Boundary |
| 2 | 0.70 to <3.50 | Positive |
| 3 | 3.50 to <17.5 | Positive |
| 4 | 17.5 to <50.0 | Positive |
| 5 | 50.0 to <100 | Positive |
| 6 | 100< | Positive |
| IJH-SONE68 (n = 29) | Placebo (n = 31) | p Value | ||
|---|---|---|---|---|
| Anemia | 0.229 | |||
| Grade 1 | 2 (7%) | 0 | ||
| Blood bilirubin increased | 0.942 | |||
| Grade 1 | 0 | 2 (6%) | ||
| Blood lactate dehydrogenase increased | 0.355 | |||
| Grade 1 | 1 (3%) | 4 (13%) | ||
| Cholesterol high | 0.518 | |||
| Grade 1 | 12 (41%) | 16 (52%) | ||
| Grade 2 | 1 (3%) | 0 | ||
| Creatinine increased | 1.000 | |||
| Grade 1 | 2 (7%) | 2 (6%) | ||
| Weight gain | 0.737 | |||
| Grade 1 | 0 | 1 (3%) | ||
| Grade 2 | 1 (3%) | 0 | ||
| White blood cell decreased | 0.666 | |||
| Grade 1 | 3 (10%) | 2 (6%) | ||
| Hyperglycemia | 0.148 | |||
| Grade 1 | 2 (7%) | 7 (23%) | ||
| Hypertriglyceridemia | 0.355 | |||
| Grade 1 | 1 (3%) | 4 (13%) | ||
| Hyperuricemia | 1.000 | |||
| Grade 1 | 1 (3%) | 2 (6%) | ||
| Hypoalbuminemia | 1.000 | |||
| Grade 1 | 0 | 1 (3%) | ||
| Hypertension | 0.581 | |||
| Grade 1 | 7 (24%) | 9 (29%) | ||
| Grade 2 | 2 (7%) | 4 (13%) | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Noda, M.; Kanno, K.; Danshiitsoodol, N.; Higashikawa, F.; Sugiyama, M. Plant-Derived Lactobacillus paracasei IJH-SONE68 Improves Chronic Allergy Status: A Randomized, Double-Blind, Placebo-Controlled Clinical Trial. Nutrients 2021, 13, 4022. https://doi.org/10.3390/nu13114022
Noda M, Kanno K, Danshiitsoodol N, Higashikawa F, Sugiyama M. Plant-Derived Lactobacillus paracasei IJH-SONE68 Improves Chronic Allergy Status: A Randomized, Double-Blind, Placebo-Controlled Clinical Trial. Nutrients. 2021; 13(11):4022. https://doi.org/10.3390/nu13114022
Chicago/Turabian StyleNoda, Masafumi, Keishi Kanno, Narandalai Danshiitsoodol, Fumiko Higashikawa, and Masanori Sugiyama. 2021. "Plant-Derived Lactobacillus paracasei IJH-SONE68 Improves Chronic Allergy Status: A Randomized, Double-Blind, Placebo-Controlled Clinical Trial" Nutrients 13, no. 11: 4022. https://doi.org/10.3390/nu13114022
APA StyleNoda, M., Kanno, K., Danshiitsoodol, N., Higashikawa, F., & Sugiyama, M. (2021). Plant-Derived Lactobacillus paracasei IJH-SONE68 Improves Chronic Allergy Status: A Randomized, Double-Blind, Placebo-Controlled Clinical Trial. Nutrients, 13(11), 4022. https://doi.org/10.3390/nu13114022






