Abstract
Objective: To review the scientific literature on the influence of verified nutrition, food and diet interventions on occupational health. Method: This study involved a critical analysis of articles retrieved from MEDLINE (via PubMed), Embase, Cochrane Library, PsycINFO, Scopus, Web of Science, Latin American and Caribbean Health Sciences Literature (LILACS) and Medicina en Español (MEDES) using the descriptors “Diet, Food, and Nutrition” and “Occupational Health” and applying the filters “Clinical Trial”, “Humans” and “Adult: 19+ years”; the search was conducted on 29 May 2021. Results: A total of 401 references were retrieved from the bibliographic databases, with an additional 16 identified through a secondary search; among the studies retrieved, 34 clinical trials were selected after applying the inclusion and exclusion criteria. The interventions were grouped into seven categories: (1) dietary interventions associated with exercise or educational programs; (2) individual environmental interventions or other educational actions; (3) educational interventions oriented toward lifestyle, dietetics, physical activity and stress management; (4) economic incentives; (5) multicomponent interventions (combination of mindfulness, e-coaching and the addition of fruits and vegetables); or dietary interventions (facilitating greater food supply in cafeterias); or interventions focused on physical exercise. Conclusions: Given that most people spend a large part of their time in the workplace and, therefore, eat at least one of their daily meals there, well-planned interventions—preferably including several strategies—have been demonstrated, in general, as useful for combating overweight and obesity. From the meta-regression study, it was observed that the interventions give better results in people who presented high Body Mass Index (BMI) values (obesity). In contrast, intervention 2 (interventions related to workplace environment) would not give the expected results (it would increase the BMI).
1. Introduction
The importance of good health, physical activity and adequate nutrition is frequently discussed. However, there are many occasions in which we do not realize that health and work go hand-in-hand, influencing each other. In this relationship, it must be taken into account that a large number of people eat at least one of their daily meals in the workplace, which makes food very important in working life.
A proper diet together with adequate hydration has the potential to influence many aspects of work. However, well-designed nutritional interventions as measures to improve the health and performance of workers are scarce []. Importantly, nutrition is an essential part of economic development because it influences the health and productivity of workers [,].
Community health focuses on the influence of adequate food/nutrition (diet) on occupational health and how to address dietary limitations (malnutrition) and dietary excesses (obesity). In this sense, the National Institute for Occupational Safety and Health (NIOSH), which is part of the US Centers for Disease Control and Prevention, aims to raise awareness among employers and empower workers to create safe and healthy workplaces. NIOSH encourages “Total Worker Health”, a strategy that integrates occupational safety and health protection to prevent worker injuries and illnesses and improve their health and well-being, with access to healthy and affordable food being an important topic [].
The worldwide prevalence of overweight and obesity has tripled since the mid-1970s. Data for 2016 show that more than 1.9 billion adults were overweight, of whom more than 650 million were obese []. This trend is based on overeating, sedentary behaviors, unhealthy lifestyles, insufficient levels of physical activity, poor diet (highly caloric and processed foods), as well as a higher proportion of sedentary occupations [,].
Obesity significantly increases the risk of developing metabolic disorders, hypertension, coronary heart disease, stroke, dyslipidemia, type 2 diabetes, sleep apnea, acute respiratory distress syndrome and several types of cancer. In addition, it is associated with an increase in mortality and a low quality of life [].
Additionally, this morbidity is also related to indirect costs, defined as losses due to reduced labor productivity. In fact, obesity and related diseases have been associated with an increased risk of workplace absenteeism (refers to the time taken off work due to sick leave, disability, injuries, or other reasons), presenteeism (refers to situations where people continue to work while unwell and not functioning to their full capacity) and permanent loss of work, which includes pensions for disability and premature death, generating massive costs for governments, society and employers [,]. In fact, productivity losses due to sick leave and presenteeism are even greater than the direct costs of medical treatment (an average of 2.30 USD in lost productivity for every dollar in medical expenses) [].
This evidence urges governments, scientific organizations and companies to implement occupational safety and health measures, policies and global strategies that focus on organizational, behavioral and environmental factors related to work and that directly influence the overall health of workers and companies, paying special attention to nutrition. Consequently, companies and institutions have the responsibility of ensuring that the foods available in the workplace are nutritionally adequate or making unhealthy options unavailable.
Among the current trends focused on nutrition and occupational health, the creation of a new concept, nutra-ergonomics, stands out. Nutra-ergonomics is defined as the interface between workers, their work environment and their performance in relation to their nutritional status. Nutrition is an integral part of a safe and productive workplace that encompasses physical and mental health as well as the long-term well-being of workers [].
From this global perspective, health and well-being programs in the workplace are presented as the best tools to address this growing problem; these programs comprise a set of coordinated strategies (including programs, policies, benefits, environmental support and links to the surrounding community) that are implemented in the workplace, designed to improve the health and safety of all employees [], and there are studies that support the effectiveness of these programs in improving employee health and productivity [,,].
In addition, there is a general consensus that the combination of multicomponent interventions (focused on lifestyle management that includes stress management, physical activity, nutrition, and controlling smoking and alcohol consumption) is more effective than programs that focus on a single intervention (only exercise, for example) [,].
The objective of this review was to review the scientific literature on the influence of verified nutrition, food and diet interventions on occupational health.
2. Materials and Methods
2.1. Design
This was a cross-sectional descriptive study and critical analysis of studies retrieved through a systematic review. The structure of this review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, and the methodological framework proposed by Arksey & O’Malley [] for scoping studies.
2.2. Source of Data Collection
The data were obtained from direct consultation and access, via the internet, to the following bibliographic databases in the field of health sciences: MEDLINE (via PubMed), Embase, Cochrane Library, PsycINFO, Scopus, Web of Science, and Latin American & Caribbean Health Sciences Literature (LILACS) and Medicina en Español (MEDES).
2.3. Unit of Analysis
We analyzed articles published and retrieved from the indicated bibliographic databases.
2.4. Information Processing
Search terms were selected using the Thesaurus of Health Sciences Descriptors (DeCS) developed by the Latin American and Caribbean Center on Health Sciences Information (BIREME) and equivalent terms established by the US National Library of Medicine, Medical Subject Headings (MeSH).
Based on the hierarchy of both thesaurus and their indexing files, the following search equations were considered adequate:
- Equation (1): Occupational Health
“Occupational Health” [Mesh] OR “Occupational Health” [Title/Abstract] OR “Industrial Hygiene” [Title/Abstract] OR “Industrial Health” [Title/Abstract] OR “Occupational Safety” [Title/Abstract] OR “Employee Health” [Title/Abstract] OR “Occupational exposure” [Mesh] OR “Occupational exposure” [Title/Abstract] OR “Occupational stress” [Mesh] OR “Occupational stress” [Title/Abstract] OR “Occupational diseases” [Mesh] OR “Occupational diseases” [Title/Abstract] OR “Occupational hazards” [Title/Abstract] OR “Occupational medicine” [Mesh] OR “Occupational medicine” [Title/Abstract] OR “Occupational health safety” [Title/Abstract] OR “Occupational Health Services” [Title/Abstract] OR “Occupational Health Services” [Mesh] OR “National Institute for Occupational Safety and Health (U.S.)” [Mesh] OR “Occupational stressors” [Title/Abstract] OR “Occupational stressor” [Title/Abstract] OR “Occupational Factors “[Title/Abstract] OR “Workplace” [Mesh] OR “Workplace” [Title/Abstract] OR “Workplace Health” [Title/Abstract] OR “Workplace safety” [Title/Abstract] OR “Safety climate” [Title/Abstract] OR “Total worker health” [Title/Abstract] OR “Working Environment” [Title/Abstract] OR “Job Satisfaction” [Mesh] OR “Job Satisfaction” [Title/Abstract] OR “Job Stress” [Title/Abstract] OR “Job security” [Title/Abstract] OR “Psychosocial working conditions” [Title/Abstract] OR “Employee Health” [Title/Abstract].
- Equation (2): Diet, Food, and Nutrition
“Diet, Food, and Nutrition” [Mesh] OR “Nutritional Status” [Mesh] OR “Nutritional Status” [Title/Abstract] OR “Nutrition Therapy” [Mesh] OR “Nutrition Therapy” [Title/Abstract] OR “Nutrition Assessment” [Mesh] OR “Nutrition Assessment” [Title/Abstract] OR “Nutrition Surveys” [Mesh] OR “Nutrition Surveys” [Title/Abstract] OR “Diet” [Mesh] OR “Diet” [Title/Abstract] OR “Healthy Diet” [Mesh] OR “Healthy Diet” [Title/Abstract] OR “Healthy Eating” [Title/Abstract] OR “Energy Intake” [Mesh] OR “Energy Intake” [Title/Abstract] OR “Meals” [Mesh] OR “Meals” [Title/Abstract] OR “Meal Time” [Title/Abstract] OR “Dinner Time” [Title/Abstract] OR “Breakfast” [Mesh] OR “Breakfast” [Title/Abstract] OR “Breakfast Time “[Title/Abstract] OR “Morning Meal” [Title/Abstract] OR “Food Services” [Mesh] OR “Food Services” [Title/Abstract] OR “Eating Practices” [Title/Abstract] OR “Dietary practices” [Title/Abstract] OR “Unhealthy food options” [Title/Abstract] OR “Eat and drink” [Title/Abstract] OR “Meal breaks” [Title/Abstract] OR “Dietary habits” [Title/Abstract] OR “Eating behavior” [Title/Abstract] OR “Meal timing” [Title/Abstract] OR “Eating at night” [Title/Abstract] OR “Body weight” [Title/Abstract] OR “BMI” [Title/Abstract] OR “Shiftwork” [Title/Abstract] OR “Work Hygiene” [Title/Abstract] OR “Healthy Lifestyle” [Mesh] OR “Feeding Behavior” [Mesh] OR “Feeding Behavior” [Title/Abstract] OR “Feeding Behaviors” [Title/Abstract] OR “Eating Behaviors” [Title/Abstract] OR “Feeding Patterns” [Title/Abstract] OR “Feeding Pattern” [Title/Abstract] OR “Food Habits” [Title/Abstract] OR “Food Habit” [Title/Abstract] OR “Eating Habits” [Title/Abstract] OR “Eating Habit” [Title/Abstract] OR “Diet Habits” [Title/Abstract] OR “Diet Habit” [Title/Abstract].
The final search equation was developed for use in MEDLINE via PubMed through the Boolean union of the 2 proposed equations (Equation (1) AND Equation (2)) using the filters Clinical Trial, Humans and Adult: 19+ years.
This strategy was subsequently adapted to the characteristics of each of the other databases consulted, performing the search from the first available date in each of the selected databases until 29 May 2021. Additionally, a complementary search strategy was performed to reduce the possibility of publication bias by manually searching the reference lists of the clinical trials that were selected for the review. Likewise, experts in the subject under study were contacted to determine the possible existence of gray literature (materials and research produced by organizations outside traditional commercial or academic publications that are disseminated through other distribution channels).
2.5. Final Selection of Articles
For the review and critical analysis, articles that met the following criteria were chosen:
- Inclusion: met the objectives of the search; clinical trial; published in a peer-reviewed journal and written in English, Spanish or Portuguese.
- Exclusion: full text could not be found; no relationship between the intervention and the outcome under study (causality criterion), and included a nonadult population (under 18 years of age).
The selection of relevant articles was performed by two authors of the present review (L.M-F. and A.F-P.). To validate the inclusion of the articles, the assessment of the agreement between the authors (kappa index = KI) had to be greater than 0.60 []. Provided that this condition was met, possible disagreements were resolved by consensus among all authors of the review.
2.6. Completeness of Reporting, Level of Evidence and Grade of Recommendation
The adequacy of the selected articles was assessed using the CONSORT (Consolidated Standards of Reporting Trials) guidelines for reporting clinical trials []. This checklist contains 25 essential elements (items) that should be described in this type of study. One point was assigned for each item present (if not applicable, the item was not scored). When an item comprised several points, each was evaluated independently, giving the same weight to each point, and then the points for the item were averaged to obtain a final result, therefore, in no case was it possible to score more than 1 point per item.
To determine the level of evidence and its degree of recommendation, the recommendations of the Scottish Intercollegiate Guidelines Network Grading Review Group (SIGN) [] were used.
2.7. Data Extraction
Data correction was performed by inputting the data into duplicate tables, thus allowing the detection of deviations and their correction through consultation of the original document.
The elimination of duplicate records (present in more than one database) was executed using the multiplatform program ZOTERO (bibliographic reference manager developed by the Center for History and New Media of George Mason University).
To determine the actuality of the studies, the Burton–Kebler half-period (BK) and the Price index (PI) were calculated.
The articles were grouped based on the variables under study to systematize and facilitate the understanding of the results, considering the following data: first author, year of publication, population studied, pathology of the population, country where the study was developed, period of the study, type of intervention performed, and main results influenced by the effect of the intervention.
2.8. Data Analysis
Data related to information retrieval are presented as frequencies and percentages.
To determine the BK, the median age was calculated based on the time range analyzed, and the PI was calculated as the percentage of articles 5 years old or newer.
The measure of agreement to determine the relevance of the selected articles was performed using the KI. The agreement between authors was considered valid when the KI value was greater than 60% (good or very good agreement).
The scores of the CONSORT questionnaire were analyzed using the median, maximum and minimum. The evolution of this score, in relation to the years of publication, was obtained by Pearson’s correlation analysis.
2.9. Meta-Analysis and Meta-Regression
To find out the effects of the interventions on workers’ BMI, we analyzed the effect size using a meta-analysis of the studies included in the systematic review. The estimated model was the random-effects model. The results of the effect size and its 95% confidence interval were presented in the Forest plot, together with the percentage of heterogeneity, the Tau value for the contrast and the corresponding heterogeneity test.
Publication bias occurs when only favorable results are published, and it is suspected that studies with non-significant results failed to be published. The absence of such studies may overestimate the results. In this study, the Funnel plot has been used. In the Funnel plot, the effect measure of each study is plotted on the x-axis and a measure of precision, such as the standard error on the y-axis. A meta-analysis without publication bias would show a point cloud in the shape of an inverted funnel. Based on this assumption, we performed the non-parametric trim-and-fill analysis proposed by Duval and Tweedie [], adjusting for the number of missing studies and re-estimating the results by including these missing studies. Another approach to estimating the number of missing studies was proposed by Copas et al. [], which we have also used.
Meta-regression was used to determine whether intervention type or baseline BMI status would influence heterogeneity and effect sizes. Bivariate and multivariate models were applied. Baseline BMI status was divided into three groups, normal weight, overweight and obese, and five interventions were studied.
The results of the articles selected from the systematic review are shown by their authors in three different ways: the results before and after the interventions in terms of mean and standard deviation, the difference between before and after the interventions in terms of mean and 95% CI and finally, the difference between before and after the interventions in terms of mean and standard deviation. In order to unify the criteria, the last option was used in the meta-analysis. Therefore, for the first situation, the difference of means and the weighted standard deviation were calculated for the first case. For the second case, the estimated standard error was obtained from the width of the 95% CI and the sample size.
All calculations were performed in the R programming environment using the packages meta version 4.10-0 and metas version 0.4-0 [].
2.10. Ethical Aspects
All data were obtained from published articles. Therefore, and in accordance with Spanish Law 14/2007, approval by an ethics committee was not necessary for the use of secondary data.
3. Results
A total of 401 articles were retrieved: 121 (30.17%) in MEDLINE (via PubMed), 47 (11.72%) in Embase, 62 (15.46%) in Cochrane Library, 82 (20.45%) in Scopus, 33 (8.23%) in Web of Science, 50 (12.47%) in PsycINFO and six (1.502%) in MEDES. No documents were found in the LILACS bibliographic database. Consultation of the bibliographic lists of selected articles allowed the identification of another 16 studies.
After filtering the 75 repeated records and applying the inclusion and exclusion criteria (Figure 1), 34 clinical trials [,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,] were selected for review and critical analysis (see Table 1).
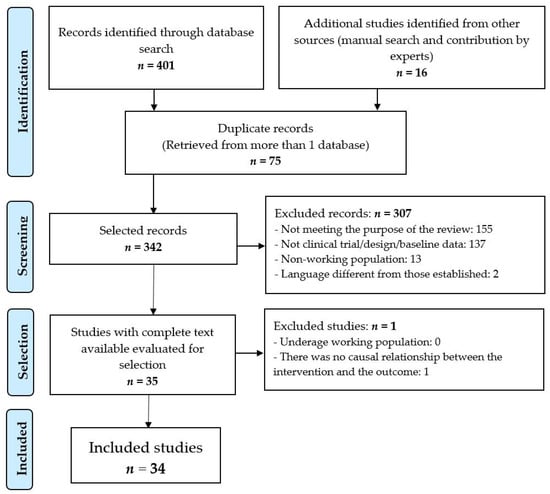
Figure 1.
Selection procedure of the studies.

Table 1.
Summary of the studies reviewed.
The agreement among the evaluators regarding the relevance of selected studies, calculated using the KI, was 74.88% (p = 0.01).
The selected articles had an actuality, as determined by the BK, equal to 7.50 years, with a PI of 29.41%. The years with the highest number of published works were 2012, 2015 and 2017, with four trials published each of those years; see Table 1.
When evaluating the transparency of reporting of the trials selected for the review, the CONSORT checklist scores ranged from a minimum of 3.50 (14% compliance) to a maximum of 20.50 (82.50% compliance) with a median of 12.75 (Table 2), observing, across time, a good increasing exponential trend (R2 = 0.62; p < 0.001).

Table 2.
Assessment of study quality according to the 25-item CONSORT guidelines.
Based on the SIGN criteria, this review presented evidence with a grade of 1- (systematic review of randomized clinical trials or randomized clinical trials with a high risk of bias) with a recommendation grade of B (a body of evidence that includes studies directly applicable to the target population and that demonstrates global consistency of the results or the extrapolation of studies rated as 1).
The majority of the studies included in the review were from the USA, with 17 trials [,,,,,,,,,,,,,,,,] and the Netherlands, with three trials [,,].
The study with the largest population was that by Fernández et al. [], with n = 2614 workers, and the study with the smallest population was that by Almeida et al. [], with 28 workers. All participants were of working age (between 18 and 65 years).
The mean body mass index (BMI) in the intervention group fluctuated between a minimum of 23.8 ± 3.5 in the study by Iturriaga et al. [] and a maximum of 39.4 ± 6.9 in the study by Barham et al. []. There were four clinical trials that did not report BMI: Shrivastava et al. [] only indicated the percent of obese individuals; Follick et al. [] only included the percent of overweight individuals; Baer [] only reported weight in kilograms and Ferdowsian et al. [] did not report any measure related to BMI.
The main pathologies observed in the study population were overweight and obesity [,,,,,,,,,,,,,]; overweight [,,,]; obesity [,,]; overweight, obesity and diabetes [,,,,,]; abdominal obesity and dyslipidemia [,]; overweight and musculoskeletal disorders []; obesity, diabetes and cardiovascular disease []; metabolic syndrome []; metabolic disease [], and metabolic disease [].
The intervention period ranged from a minimum of 10 weeks [,] to a maximum of 3 years [], with 12 months being the most frequent intervention period [,,,,,,,,,].
3.1. Types of Interventions Performed
Due to the heterogeneity of the actions carried out, in the clinical trials analyzed, the different interventions carried out were grouped into the following seven categories:
- Dietary interventions associated with other actions (exercise or educational program): seven studies [,,,,,,].
- Interventions related to the workplace environment, including educational actions, financial incentives, availability and price of food and portion control: five studies [,,,,].
- Exclusive educational interventions aimed toward lifestyle, dietetics, physical activity, and stress management, including televigilance devices and counseling: 16 studies [,,,,,,,,,,,,,,,].
- Economic incentives added to training actions aimed at weight loss, physical activity and dieting: three studies [,,].
Multicomponent intervention, through the combination of mindfulness, e-coaching and the addition of fruits and vegetables: one study []; or dietary intervention (facilitating a greater supply of food in cafeterias): one study []; or intervention focused on physical exercise: one study [].
3.2. Main Results Derived from the Interventions
From the interventions developed, the following results could be verified:
Dietary interventions associated with other actions (mainly physical exercise) decreased body weight in the intervention group [,,]. Gepner et al. [] also observed improvements in cardiometabolic markers, and Ferdowsian et al. [], along with weight loss, reported a decrease in waist circumference. The intervention program implemented by Röhling et al. [] (the SAMMAS intervention) achieved long-term weight loss maintenance. In contrast, in a previous trial, Leslie et al. [] concluded that the body weight maintenance intervention was not effective.
Behavioral environmental strategies improved food selection, which, according to Thorndike et al. [], resulted in improvements in body weight. Even educational actions were effective in promoting healthy diets [] and were postulated as promising long-term interventions (2 years) []. However, Linde et al. [] and Brehm et al. [] indicated that environmental changes in the workplace were not enough to improve the weight and health of workers.
Educational interventions showed their suitability for implementation in the workplace; such interventions resulted in a decrease in weight and BMI in the treatment group [,,,,]. Kempf et al. [] also observed a decrease in BMI in the intervention group, but their results were not supported by intention-to-treat analysis. Mitchell et al. [] confirmed that weight loss was associated with greater attendance at educational intervention sessions. Likewise, educational actions improve metabolic parameters [], cardiometabolic risk factors [] and the prevalence of metabolic syndrome []. Furthermore, this type of intervention was shown to be valid in improving the risks associated with coronary disease [].
For the follow-up of these training activities, van Wier et al. [] demonstrated that telephone follow-up was effective. However, Solenhill et al. [] found that telephone counseling did not have positive effects on employees, and Thorndike et al. [] concluded that online support was not effective.
Viester et al. [] concluded that these actions could have promising long-term effects, but differences between the intervention and control groups were not significant. The study by Østbye et al. [] found no differences related to the implementation of an educational program.
The use of economic incentives as the main intervention influenced the weight loss of participants [] and even decreased attrition []. It was also effective in stimulating change toward healthier attitudes, reducing the tendency to increase body weight []. However, no study showed results related to the period after the incentive ceases.
Other multicomponent actions [] (combination of mindfulness, e-coaching and the addition of fruits and vegetables) did not show clear causal effects at 6 and 12 weeks.
Exclusive dietary action (a low-fat vegan diet) [] produced an improvement in body weight at 18 weeks, but results for the maintenance period and long-term results were not indicated.
For an intervention focused on physical exercise [], beneficial effects on body composition were observed in the short term (12 weeks), but postintervention results were not included.
3.3. Main Results Derived of Meta-Analysis
For the meta-analysis, 35 groups of 22 articles were included.
- Effect size
The effect sizes calculated from the meta-analysis are shown in Figure 2 as well as tests for the presence of heterogeneity.
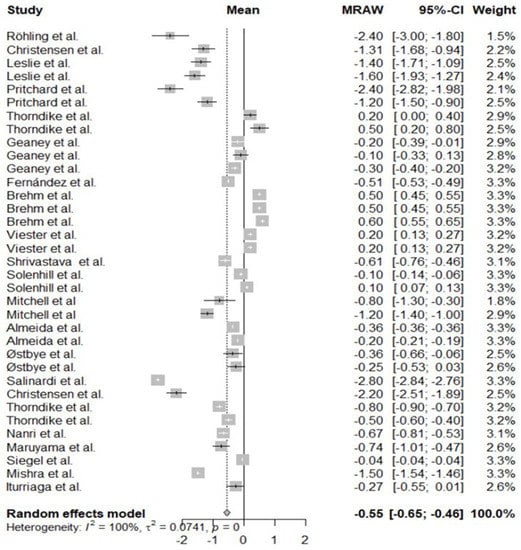
Figure 2.
Forest plot for Body Mass Index.
- Heterogeneity of included studies
The included studies show strong heterogeneity (100%). Table 3 shows the effect of each study on the total heterogeneity. We observe that none of them is very influential. Similarly, we can see in Figure 3 of the Baujat graph that no study is in the upper right corner.

Table 3.
Summary leave-one-out, Baseline of Body Mass Index and interventions.
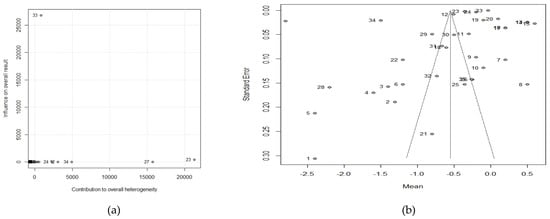
Figure 3.
(a) Baujat plot for Body Mass Index (b) Funnel plot for Body Mass Index.
The Bajujat graph (Figure 3a) shows that no single group has a decisive weight on the outcome of the meta-analysis. In fact, in the leave-one-out test, no study varied heterogeneity by more than 1%.
- Heterogeneity of non-included studies (publication bias)
Another source of heterogeneity could come from publication bias. For this purpose, we analyze the symmetry of the Funnel-polt (Figure 3b).
As can be seen, there is not much symmetry, so publication bias may be high. The results of the Trim-fill and Copas techniques suggest that many unpublished studies, between 12 and 48 respectively, would be needed to compensate for this lack of symmetry. The model proposed by Copas would reduce the size of the effect on BMI but still be significant, in the case of the Trim-fill adjustment this reduction would end up not being statistically significant.
- Moderator analysis (meta-regression)
Other sources of possible heterogeneity may be the influence of covariates or moderators. Table 4 studies the effects of the five types of interventions and the baseline BMI.

Table 4.
Moderator analysis, adjusted meta-regression by the baseline of Body Mass Index and interventions.
There is variation in the effect size of BMI by baseline. Interventions give better results on obese groups than on groups with overweight or normal weight. As for the interventions, 1 and 2 were statistically significant in the multivariate model but with opposite directions. Intervention 1 decreases BMI and intervention 2 increases BMI.
4. Discussion
Following the recommendations regarding the objectives of a systematic review [], the current review synthesized the relevant information related to nutrition, food and diet interventions implemented in occupational health to provide the scientific community with relevant information that can help promote new interventions for workers protection. In addition, this study is part of the strategy of the World Health Organization that emphasizes the importance of establishing primary prevention and interventions aimed at improving occupational health [].
It could be considered that the most prevalent occupational disease (although it is not considered as such) is undoubtedly obesity (and overweight) because it affects many workers [] and those who are overweight or obese are more likely to suffer injuries than normal-weight workers [].
The analysis of the actuality of the reviewed studies demonstrated the full validity of the selected studies because the data obtained showed greater relevance than what was calculated for the bibliometric studies in fields related to the sciences of nutrition and occupational health [] and more current than that found for recent systematic reviews related to occupational health [,].
The evaluation of the reporting transparency of the studies included in the review articles, as assessed by the CONSORT criteria, was similar to that for other review articles [,]. The analysis of the progression of documentary adequacy that was observed in the most current articles was mainly due to the implementation of CONSORT criteria. In fact, the oldest works did not usually follow these quality guidelines; for example, the first documents that used the CONSORT criteria date back to 1996 [], and their use was progressive. If clinical trials have an inadequate methodology or, especially, if the final description of the trial does not contain certain information, readers cannot adequately judge the validity of the study, and the scientific evidence related to the results is very limited [].
The level of evidence and grade of recommendation for this study, as determined using the SIGN criteria, were consistent or even better than those observed in previous studies. Despite seeking a consistent cause-effect relationship, because intervention studies were sought, some were subject to more bias than others and therefore, more weakly support the conclusions []. The conclusions of many studies of occupational health and safety are still not based on the greatest possible evidence []. This may be due to the experimental design of primary studies, such as clinical trials, which are considered robust but may not be adequate to evaluate interventions in occupational health when presenting, generally, very long-term effects; furthermore, as in this review, nutritional interventions were not the most studied mediations in relation to work and were more oriented to combat certain diseases.
All the studies focused primarily on overweight and/or obese populations, except for the studies by Nanri et al. [], which focused on a population with metabolic syndrome, that by Maruyama et al. [], which focused on metabolic disease in general and that by Baer [], which focused on heart disease.
BMI was provided in the vast majority of the studies, and it was considered that those that did not provide a clear measure to evaluate interventions [,,,] could not have adequately reported their results. This inadequate description of clinical studies can be, in any case, a waste of time for those who seek valid information derived from clinical trials []. The lack of information in a publication can result in the work being excluded when carrying out a systematic review on a certain intervention. Approximately one-third of clinical trials can be excluded from systematic reviews because relevant data are lacking []. In this review, it was decided to retain these four clinical trials to provide as much information as possible but not dismiss the lack of relevant results.
Dietary-nutritional interventions within companies are always complex due to the idiosyncrasy of the workforce and, generally, the short period available to perform these interventions []. Thus, the follow-up period must be adequate to assess the results of the intervention, a requirement that all the selected trials met. A period of several weeks, even months, is considered necessary to assess the results [,].
In general, interventions using any mode of interaction (face-to-face, telephone, internet, etc.), directed by a trained professional, were effective in improving outcomes related to overweight and obesity.
From the interventions observed, it was possible to deduce that the actions that included several strategies achieved adequate results in the working population. This statement is consistent with the results reported by Upadhyaya et al. [], who concluded that occupational health professionals should continue to be creative in the development of multicomponent interventions (combining behavioral/educational, environmental and organizational support).
The effectiveness of dietary interventions associated with other actions (mainly physical exercise) is a well-known topic. Their effectiveness in the management of obesity and overweight in the work environment has already been demonstrated [,]. However, the structures and cultures of the workplace should always be considered when planning interventions. The negotiation and flexibility of stakeholders play essential roles in overcoming resistance to change [].
Among the combined strategies, environmental interventions have been proposed as appropriate actions for the promotion of healthy habits, although they were not considered sufficient, by themselves, to improve the weight and health of workers [,]. Thus, the review by Chu et al. [], confirmed the consistency of the effectiveness of multicomponent environmental interventions.
The results obtained showed a causal relationship when implementing educational measures in the workplace focused on decreasing body weight, resulting in improvements in metabolic parameters [], cardiometabolic risk factors [] and prevalence of metabolic syndrome []. This type of intervention was shown to be valid in improving the risks associated with coronary disease []. However, the review by Wolfenden et al. [] concluded that it was not clear whether such strategies were profitable or generated unintended adverse consequences, thus justifying more research to seek more evidence.
The strategies that included financial incentives (generally discounts for healthy items on the menu for the company cafeteria) when choosing the healthiest menu items were shown to be effective in preventing obesity and improving eating habits. However, the study by Sawada et al. [] expressed the need to carry out interventions that focus exclusively on financial incentives versus no intervention to determine if this strategy has a clear impact. Combined actions could mask these results.
In line with what was stated by Peñalvo et al. [], it is important to highlight the generally short/moderate duration (between 6 months and 1 year) of the vast majority of workplace health interventions and programs, as well as the limited evaluation of the sustainability of the change in habits after the end of the program, which may raise doubts about the long-term effectiveness of these interventions. However, in relation to the failure of interventions focused on overweight and obese patients carried out in the workplace, Park and King [] argue that there is evidence indicating that the duration of the intervention is a determining factor, with short-term programs (less than 6 months) being more effective than long-term programs.
Most of the identified studies came from high-income countries, mainly the United States, where the problem of obesity and overweight has become a heavy burden in economic and health terms for the state and companies []. In this sense, and as indicated by Peñalvo et al. [], occupational health programs and their evaluation are scarce in other geographic and socioeconomic contexts (a single study from India included in the review) where non-communicable diseases are increasing rapidly.
In short, given the substantial period of time that adults spend in their workplaces each day, workplaces provide an opportune environment for interventions relating to healthy habits and can be effective if such interventions combine several strategies (diet, lifestyle, physical activity, reduction in alcohol and tobacco consumption, rewards, adherence to the intervention, etc.) The identification of strategies that are effective in improving the implementation of interventions in the workplace has the potential to improve health outcomes.
However, from the results observed in the clinical trials reviewed, employees acquired a greater awareness of the relationship between diet and health. Additionally, they considered the actions taken a positive experience for themselves and the company. These statements had already been noted in a previous study by Munar-Gelabert et al. [].
The results of the meta-regression and the little-observed effect derived from the interventions are in line with other previous works. The findings of LaCaille et al. [], showed that ecological approaches in the workplace have had little or no effect on preventing weight gain. Similarly, Allan et al. [], in a 2017 systematic review, noted that there was no convincing evidence that this type of intervention resulted in weight or BMI changes. Another limitation of environmental interventions is the cost and levels of administrative approval necessary for modifying the work environment since they can pose a barrier to the implementation and success of environmental strategies. In addition, there may be reluctance regarding healthy alternatives available in the cafeteria and portion size reduction among workers []. Moreover, Vermeer et al. [], noted the importance of assessing the existence of workers’ compensatory eating behaviors after eating less in the workplace.
4.1. Limitations of the Review
The results of this review are limited by the shortcomings of each work included in it. The level of evidence and recommendation values reached did not ensure that the clinical trials reviewed did not have a high risk of bias. Numerous studies did not specify whether they controlled for confounding factors that could affect the results.
In addition, to raise the level of evidence and recommendation of this review, it would be necessary for all the trials to have taken into account the existence of adverse consequences, an item not observed in any of the included studies. Thus, the low-certainty evidence suggests that such strategies can make little or no difference in the measures of the consistency of implementation or in the different health behavior outcomes of the employees, a circumstance already reported by Wolfenden et al. [].
4.2. Critical Analysis of the Authors
While the majority of clinical trials found that the different interventions observed provided opportunities to establish different programs in the workplace, other studies contradicted this possibility by not finding an association between the intervention group and the control group. Additionally, and without doubting the favorable results obtained, many of the trials did not report effects since the intervention ended.
It would have been desirable to have considered the impact that shift work had when implementing the different interventions. This issue was not clear in the documents reviewed.
Another issue that was missed was the absence of information on adherence to the different interventions. As stated by Abbate et al. [], the follow-up of any strategy is fundamental because it is directly related to health outcomes.
From the meta-regression study, it was observed that the interventions give better results in people who presented high BMI values (obesity). In contrast, intervention 2 (interventions related to workplace environment) would not give the expected results (it would increase the BMI). In addition, although the characteristics of the workplace can generate an obesogenic environment, changes in this environment may be necessary but not enough to modify the obesity-related health behaviors of workers.
Importantly, methodologically rigorous studies are considered necessary to carry out adequate nutritional interventions in the workplace.
5. Conclusions
Given that most people spend a large part of their time in the workplace and, therefore, eat at least one of their daily meals there, well-planned interventions—preferably including several strategies—have been shown to be useful for reducing weight, improving healthy behaviors and preventing overweight and obesity.
Author Contributions
Conceptualization, L.M.-F., C.W.-B. and J.S.-V.; methodology, L.M.-F., M.S.-L., P.C. and J.S.-V.; validation, C.W.-B. and J.S.-V.; formal analysis, Á.F.-P., P.C. and M.S.-L.; data curation, L.M.-F., Á.F.-P., P.C. and M.S.-L.; writing—original draft preparation, L.M.-F., C.W.-B. and J.S.-V.; writing—review and editing, L.M.-F., Á.F.-P., M.S.-L., P.C., C.W.-B. and J.S.-V.; supervision, C.W.-B. and J.S.-V. All authors have read and agreed to the published version of the manuscript.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article. The protocol of this systematic review has not been registered.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Shearer, J.; Graham, T.E.; Skinner, T.L. Nutra-Ergonomics: Influence of Nutrition on Physical Employment Standards and the Health of Workers. Appl. Physiol. Nutr. Metab. 2016, 41, S165–S174. [Google Scholar] [CrossRef] [PubMed]
- Angeles-Agdeppa, I.; Custodio, M.R.S. Food Sources and Nutrient Intakes of Filipino Working Adults. Nutrients 2020, 12, 1009. [Google Scholar] [CrossRef] [PubMed]
- Anderson, L.M.; Quinn, T.A.; Glanz, K.; Ramirez, G.; Kahwati, L.C.; Johnson, D.B.; Buchanan, L.R.; Archer, W.R.; Chattopadhyay, S.; Kalra, G.P.; et al. The Effectiveness of Worksite Nutrition and Physical Activity Interventions for Controlling Employee Overweight and Obesity: A Systematic Review. Am. J. Prev. Med. 2009, 37, 340–357. [Google Scholar] [CrossRef]
- Melián-Fleitas, L.; Franco-Pérez, Á.M.; Sanz-Valero, J. Bibliometric and Thematic Analysis of Scientific Production on Occupational Health Related to Nutrition, Food and Diet, Indexed in MEDLINE. Med. Segur. Trab. 2019, 65, 10–23. [Google Scholar] [CrossRef]
- World Health Organization. Obesity and Overweight. Available online: https://bit.ly/3gIGYwb (accessed on 20 August 2021).
- Wright, S.M.; Aronne, L.J. Causes of Obesity. Abdom. Imaging 2012, 37, 730–732. [Google Scholar] [CrossRef]
- Organisation for Economic Co-Operation and Development (OECD) The Heavy Burden of Obesity: The Economics of Prevention; OECD Health Policy Studies; OECD: Paris, France, 2019; ISBN 978-92-64-33004-7.
- Engin, A. The Definition and Prevalence of Obesity and Metabolic Syndrome. Adv. Exp. Med. Biol. 2017, 960, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Goettler, A.; Grosse, A.; Sonntag, D. Productivity Loss Due to Overweight and Obesity: A Systematic Review of Indirect Costs. BMJ Open 2017, 7, e014632. [Google Scholar] [CrossRef] [PubMed]
- Melián-Fleitas, L. Occupational Health New Paradigm: Food, Nutrition and Diet. Med. Segur. Trab. 2019, 65, 73–75. [Google Scholar] [CrossRef][Green Version]
- Lang, J.; Cluff, L.; Payne, J.; Matson-Koffman, D.; Hampton, J. The Centers for Disease Control and Prevention: Findings From The National Healthy Worksite Program. J. Occup. Environ. Med. 2017, 59, 631–641. [Google Scholar] [CrossRef] [PubMed]
- Pelletier, K.R. A Review and Analysis of the Clinical and Cost-Effectiveness Studies of Comprehensive Health Promotion and Disease Management Programs at the Worksite: Update VIII 2008 to 2010. J. Occup. Environ. Med. 2011, 53, 1310–1331. [Google Scholar] [CrossRef]
- Piepoli, M.F.; Hoes, A.W.; Agewall, S.; Albus, C.; Brotons, C.; Catapano, A.L.; Cooney, M.-T.; Corrà, U.; Cosyns, B.; Deaton, C.; et al. 2016 European Guidelines on Cardiovascular Disease Prevention in Clinical Practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (Constituted by Representatives of 10 Societies and by Invited Experts) Developed with the Special Contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur. Heart J. 2016, 37, 2315–2381. [Google Scholar] [CrossRef] [PubMed]
- Schröer, S.; Haupt, J.; Pieper, C. Evidence-Based Lifestyle Interventions in the Workplace—An Overview. Occup. Med. Oxf. Engl. 2014, 64, 8–12. [Google Scholar] [CrossRef] [PubMed]
- Arksey, H.; O’Malley, L. Scoping Studies: Towards a Methodological Framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Wanden-Berghe, C.; Sanz-Valero, J. Systematic Reviews in Nutrition: Standardized Methodology. Br. J. Nutr. 2012, 107, S3–S7. [Google Scholar] [CrossRef]
- Pandis, N.; Chung, B.; Scherer, R.W.; Elbourne, D.; Altman, D.G. CONSORT 2010 Statement: Extension Checklist for Reporting within Person Randomised Trials. BMJ 2017, 357, j2835. [Google Scholar] [CrossRef] [PubMed]
- Harbour, R.; Miller, J. A New System for Grading Recommendations in Evidence Based Guidelines. BMJ 2001, 323, 334–336. [Google Scholar] [CrossRef]
- Duval, S.; Tweedie, R. Trim and Fill: A Simple Funnel-Plot-Based Method of Testing and Adjusting for Publication Bias in Meta-Analysis. Biometrics 2000, 56, 455–463. [Google Scholar] [CrossRef] [PubMed]
- Copas, J.; Shi, J. A Sensitivity Analysis for Publication Bias in Systematic Reviews. Stat. Methods Med. Res. 2001, 10, 251–265. [Google Scholar] [CrossRef]
- Schwarzer, G.; Carpenter, J.R.; Rucker, G. Metasens: Statistical Methods for Sensitivity Analysis in Meta-Analysis. Available online: https://cran.r-project.org/package=metasens (accessed on 26 October 2021).
- Thorndike, A.N.; McCurley, J.L.; Gelsomin, E.D.; Anderson, E.; Chang, Y.; Porneala, B.; Johnson, C.; Rimm, E.B.; Levy, D.E. Automated Behavioral Workplace Intervention to Prevent Weight Gain and Improve Diet: The ChooseWell 365 Randomized Clinical Trial. JAMA Netw. Open 2021, 4, e2112528. [Google Scholar] [CrossRef] [PubMed]
- Röhling, M.; Martin, K.; Ellinger, S.; Schreiber, M.; Martin, S.; Kempf, K. Weight Reduction by the Low-Insulin-Method-A Randomized Controlled Trial. Nutrients 2020, 12, 3004. [Google Scholar] [CrossRef]
- Iturriaga, T.; Barcelo, O.; Diez-Vega, I.; Cordero, J.; Pulgar, S.; Fernandez-Luna, A.; Perez-Ruiz, M. Effects of a Short Workplace Exercise Program on Body Composition in Women: A Randomized Controlled Trial. Health Care Women Int. 2020, 41, 133–146. [Google Scholar] [CrossRef]
- Day, R.S.; Jahnke, S.A.; Haddock, C.K.; Kaipust, C.M.; Jitnarin, N.; Poston, W.S.C. Occupationally Tailored, Web-Based, Nutrition and Physical Activity Program for Firefighters: Cluster Randomized Trial and Weight Outcome. J. Occup. Environ. Med. 2019, 61, 841–848. [Google Scholar] [CrossRef]
- Kempf, K.; Röhling, M.; Martin, S.; Schneider, M. Telemedical Coaching for Weight Loss in Overweight Employees: A Three-Armed Randomised Controlled Trial. BMJ Open 2019, 9, e022242. [Google Scholar] [CrossRef] [PubMed]
- Tene, L.; Shelef, I.; Schwarzfuchs, D.; Gepner, Y.; Yaskolka Meir, A.; Tsaban, G.; Zelicha, H.; Bilitzky, A.; Komy, O.; Cohen, N.; et al. The Effect of Long-Term Weight-Loss Intervention Strategies on the Dynamics of Pancreatic-Fat and Morphology: An MRI RCT Study. Clin. Nutr. ESPEN 2018, 24, 82–89. [Google Scholar] [CrossRef]
- Viester, L.; Verhagen, E.A.L.M.; Bongers, P.M.; van der Beek, A.J. Effectiveness of a Worksite Intervention for Male Construction Workers on Dietary and Physical Activity Behaviors, Body Mass Index, and Health Outcomes: Results of a Randomized Controlled Trial. Am. J. Health Promot. 2018, 32, 795–805. [Google Scholar] [CrossRef]
- Shrivastava, U.; Fatma, M.; Mohan, S.; Singh, P.; Misra, A. Randomized Control Trial for Reduction of Body Weight, Body Fat Patterning, and Cardiometabolic Risk Factors in Overweight Worksite Employees in Delhi, India. J. Diabetes Res. 2017, 2017, 7254174. [Google Scholar] [CrossRef]
- Gepner, Y.; Shelef, I.; Schwarzfuchs, D.; Zelicha, H.; Tene, L.; Yaskolka Meir, A.; Tsaban, G.; Cohen, N.; Bril, N.; Rein, M.; et al. Effect of Distinct Lifestyle Interventions on Mobilization of Fat Storage Pools: CENTRAL Magnetic Resonance Imaging Randomized Controlled Trial. Circulation 2018, 137, 1143–1157. [Google Scholar] [CrossRef]
- Faghri, P.D.; Simon, J.; Huedo-Medina, T.; Gorin, A. Perceived Self-Efficacy and Financial Incentives: Factors Affecting Health Behaviors and Weight Loss in a Workplace Weight Loss Intervention. J. Occup. Environ. Med. 2017, 59, 453–460. [Google Scholar] [CrossRef]
- Geaney, F.; Kelly, C.; Di Marrazzo, J.S.; Harrington, J.M.; Fitzgerald, A.P.; Greiner, B.A.; Perry, I.J. The Effect of Complex Workplace Dietary Interventions on Employees’ Dietary Intakes, Nutrition Knowledge and Health Status: A Cluster Controlled Trial. Prev. Med. 2016, 89, 76–83. [Google Scholar] [CrossRef]
- Solenhill, M.; Grotta, A.; Pasquali, E.; Bakkman, L.; Bellocco, R.; Trolle Lagerros, Y. The Effect of Tailored Web-Based Feedback and Optional Telephone Coaching on Health Improvements: A Randomized Intervention Among Employees in the Transport Service Industry. J. Med. Internet Res. 2016, 18, e158. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, D.C.; Andrews, T.; Schenker, M.B. Pasos Saludables: A Pilot Randomized Intervention Study to Reduce Obesity in an Immigrant Farmworker Population. J. Occup. Environ. Med. 2015, 57, 1039–1046. [Google Scholar] [CrossRef]
- Fernandez, I.D.; Chin, N.P.; Devine, C.M.; Dozier, A.M.; Martina, C.A.; McIntosh, S.; Thevenet-Morrison, K.; Yang, H. Images of a Healthy Worksite: A Group-Randomized Trial for Worksite Weight Gain Prevention With Employee Participation in Intervention Design. Am. J. Public Health 2015, 105, 2167–2174. [Google Scholar] [CrossRef] [PubMed]
- Almeida, F.A.; You, W.; Harden, S.M.; Blackman, K.C.A.; Davy, B.M.; Glasgow, R.E.; Hill, J.L.; Linnan, L.A.; Wall, S.S.; Yenerall, J.; et al. Effectiveness of a Worksite-Based Weight Loss Randomized Controlled Trial: The Worksite Study. Obesity 2015, 23, 737–745. [Google Scholar] [CrossRef]
- Østbye, T.; Stroo, M.; Brouwer, R.J.N.; Peterson, B.L.; Eisenstein, E.L.; Fuemmeler, B.F.; Joyner, J.; Gulley, L.; Dement, J.M. Steps to Health Employee Weight Management Randomized Control Trial: Short-Term Follow-up Results. J. Occup. Environ. Med. 2015, 57, 188–195. [Google Scholar] [CrossRef]
- Van Berkel, J.; Boot, C.R.L.; Proper, K.I.; Bongers, P.M.; van der Beek, A.J. Effectiveness of a Worksite Mindfulness-Based Multi-Component Intervention on Lifestyle Behaviors. Int. J. Behav. Nutr. Phys. Act. 2014, 11, 9. [Google Scholar] [CrossRef]
- Mishra, S.; Xu, J.; Agarwal, U.; Gonzales, J.; Levin, S.; Barnard, N.D. A Multicenter Randomized Controlled Trial of a Plant-Based Nutrition Program to Reduce Body Weight and Cardiovascular Risk in the Corporate Setting: The GEICO Study. Eur. J. Clin. Nutr. 2013, 67, 718–724. [Google Scholar] [CrossRef] [PubMed]
- Salinardi, T.C.; Batra, P.; Roberts, S.B.; Urban, L.E.; Robinson, L.M.; Pittas, A.G.; Lichtenstein, A.H.; Deckersbach, T.; Saltzman, E.; Das, S.K. Lifestyle Intervention Reduces Body Weight and Improves Cardiometabolic Risk Factors in Worksites. Am. J. Clin. Nutr. 2013, 97, 667–676. [Google Scholar] [CrossRef]
- Christensen, J.R.; Overgaard, K.; Carneiro, I.G.; Holtermann, A.; Søgaard, K. Weight Loss among Female Health Care Workers-a 1-Year Workplace Based Randomized Controlled Trial in the FINALE-Health Study. BMC Public Health 2012, 12, 625. [Google Scholar] [CrossRef]
- Thorndike, A.N.; Sonnenberg, L.; Healey, E.; Myint-U, K.; Kvedar, J.C.; Regan, S. Prevention of Weight Gain Following a Worksite Nutrition and Exercise Program: A Randomized Controlled Trial. Am. J. Prev. Med. 2012, 43, 27–33. [Google Scholar] [CrossRef]
- Linde, J.A.; Nygaard, K.E.; MacLehose, R.F.; Mitchell, N.R.; Harnack, L.J.; Cousins, J.M.; Graham, D.J.; Jeffery, R.W. HealthWorks: Results of a Multi-Component Group-Randomized Worksite Environmental Intervention Trial for Weight Gain Prevention. Int. J. Behav. Nutr. Phys. Act. 2012, 9, 14. [Google Scholar] [CrossRef]
- Nanri, A.; Tomita, K.; Matsushita, Y.; Ichikawa, F.; Yamamoto, M.; Nagafuchi, Y.; Kakumoto, Y.; Mizoue, T. Effect of Six Months Lifestyle Intervention in Japanese Men with Metabolic Syndrome: Randomized Controlled Trial. J. Occup. Health 2012, 54, 215–222. [Google Scholar] [CrossRef]
- Brehm, B.J.; Gates, D.M.; Singler, M.; Succop, P.A.; D’Alessio, D.A. Environmental Changes to Control Obesity: A Randomized Controlled Trial in Manufacturing Companies. Am. J. Health Promot. 2011, 25, 334–340. [Google Scholar] [CrossRef]
- Christensen, J.R.; Faber, A.; Ekner, D.; Overgaard, K.; Holtermann, A.; Søgaard, K. Diet, Physical Exercise and Cognitive Behavioral Training as a Combined Workplace Based Intervention to Reduce Body Weight and Increase Physical Capacity in Health Care Workers—A Randomized Controlled Trial. BMC Public Health 2011, 11, 671. [Google Scholar] [CrossRef]
- Barham, K.; West, S.; Trief, P.; Morrow, C.; Wade, M.; Weinstock, R.S. Diabetes Prevention and Control in the Workplace: A Pilot Project for County Employees. J. Public Health Manag. Pract. 2011, 17, 233–241. [Google Scholar] [CrossRef]
- Ferdowsian, H.R.; Barnard, N.D.; Hoover, V.J.; Katcher, H.I.; Levin, S.M.; Green, A.A.; Cohen, J.L. A Multicomponent Intervention Reduces Body Weight and Cardiovascular Risk at a GEICO Corporate Site. Am. J. Health Promot. 2010, 24, 384–387. [Google Scholar] [CrossRef]
- Maruyama, C.; Kimura, M.; Okumura, H.; Hayashi, K.; Arao, T. Effect of a Worksite-Based Intervention Program on Metabolic Parameters in Middle-Aged Male White-Collar Workers: A Randomized Controlled Trial. Prev. Med. 2010, 51, 11–17. [Google Scholar] [CrossRef]
- Siegel, J.M.; Prelip, M.L.; Erausquin, J.T.; Kim, S.A. A Worksite Obesity Intervention: Results from a Group-Randomized Trial. Am. J. Public Health 2010, 100, 327–333. [Google Scholar] [CrossRef]
- Van Wier, M.F.; Ariëns, G.A.M.; Dekkers, J.C.; Hendriksen, I.J.M.; Smid, T.; van Mechelen, W. Phone and E-Mail Counselling Are Effective for Weight Management in an Overweight Working Population: A Randomized Controlled Trial. BMC Public Health 2009, 9, 6. [Google Scholar] [CrossRef]
- Leslie, W.S.; Lean, M.E.J.; Baillie, H.M.; Hankey, C.R. Weight Management: A Comparison of Existing Dietary Approaches in a Work-Site Setting. Int. J. Obes. Relat. Metab. Disord. J. Int. Assoc. Study Obes. 2002, 26, 1469–1475. [Google Scholar] [CrossRef] [PubMed]
- Pritchard, J.E.; Nowson, C.A.; Wark, J.D. A Worksite Program for Overweight Middle-Aged Men Achieves Lesser Weight Loss with Exercise than with Dietary Change. J. Am. Diet. Assoc. 1997, 97, 37–42. [Google Scholar] [CrossRef]
- Baer, J.T. Improved Plasma Cholesterol Levels in Men after a Nutrition Education Program at the Worksite. J. Am. Diet. Assoc. 1993, 93, 658–663. [Google Scholar] [CrossRef]
- Follick, M.J.; Fowler, J.L.; Brown, R.A. Attrition in Worksite Weight-Loss Interventions: The Effects of an Incentive Procedure. J. Consult. Clin. Psychol. 1984, 52, 139–140. [Google Scholar] [CrossRef] [PubMed]
- Hagger, M.S. What Makes a ‘Good’ Review Article? Some Reflections and Recommendations. Health Psychol. Rev. 2012, 6, 141–146. [Google Scholar] [CrossRef]
- World Health Organization. Global Strategy on Occupational Health for All: The Way to Health at Work. Available online: https://bit.ly/2Wtl0Gi (accessed on 20 August 2021).
- Gu, J.K.; Charles, L.E.; Bang, K.M.; Ma, C.C.; Andrew, M.E.; Violanti, J.M.; Burchfiel, C.M. Prevalence of Obesity by Occupation among US Workers: The National Health Interview Survey 2004–2011. J. Occup. Environ. Med. 2014, 56, 516–528. [Google Scholar] [CrossRef] [PubMed]
- Gu, J.K.; Charles, L.E.; Fekedulegn, D.; Ma, C.C.; Andrew, M.E.; Burchfiel, C.M. Prevalence of Injury in Occupation and Industry: Role of Obesity in the National Health Interview Survey 2004 to 2013. J. Occup. Environ. Med. 2016, 58, 335–343. [Google Scholar] [CrossRef]
- Muñoz-Cobo-Orosa, B.; Varela-Serrano, C.; Rodriguez-Ledott, M.; Sanz-Valero, J. Malignant Skin Neoplasms in Workers in the Fishing Industry: Systematic Review. Arch. Prev. Riesgos Labor. 2021, 24, 47–61. [Google Scholar] [CrossRef]
- Barriocanal-Gómez, P.; Del Pozo-Díez, C.M.; Kudryavtseva, O.; Portillo Chicano, I.; Sanz-Valero, J. Effects Derived from Occupational Exposure to Hazardous Substances in Pregnant Working Women: Systematic Review. Arch. Prev. Riesgos Labor. 2021, 24, 263–296. [Google Scholar] [CrossRef]
- Gea Cabrera, A.; Sanz-Lorente, M.; Sanz-Valero, J.; López-Pintor, E. Compliance and Adherence to Enteral Nutrition Treatment in Adults: A Systematic Review. Nutrients 2019, 11, 2627. [Google Scholar] [CrossRef] [PubMed]
- Comeche, J.M.; Gutierrez-Hervás, A.; Tuells, J.; Altavilla, C.; Caballero, P. Predefined Diets in Patients with Inflammatory Bowel Disease: Systematic Review and Meta-Analysis. Nutrients 2020, 13, 52. [Google Scholar] [CrossRef] [PubMed]
- Begg, C.; Cho, M.; Eastwood, S.; Horton, R.; Moher, D.; Olkin, I.; Pitkin, R.; Rennie, D.; Schulz, K.F.; Simel, D.; et al. Improving the Quality of Reporting of Randomized Controlled Trials. The CONSORT Statement. JAMA 1996, 276, 637–639. [Google Scholar] [CrossRef] [PubMed]
- González-Castro, U. Cómo mejorar la calidad de la publicación de ensayos clínicos: La declaración CONSORT. Actas Dermosifiliogr. 2002, 93, 141–142. [Google Scholar] [CrossRef]
- Manterola, C.; Asenjo-Lobos, C.; Otzen, T. Hierarchy of Evidence: Levels of Evidence and Grades of Recommendation from Current Use. Rev. Chil. Infectol. 2014, 31, 705–718. [Google Scholar] [CrossRef]
- Teufer, B.; Ebenberger, A.; Affengruber, L.; Kien, C.; Klerings, I.; Szelag, M.; Grillich, L.; Griebler, U. Evidence-Based Occupational Health and Safety Interventions: A Comprehensive Overview of Reviews. BMJ Open 2019, 9, e032528. [Google Scholar] [CrossRef] [PubMed]
- Cox, N.H.; Williams, H.C. Can You COPE with CONSORT? Br. J. Dermatol. 2000, 142, 1–3. [Google Scholar] [CrossRef]
- Munar-Gelabert, M.; Puzo-Foncillas, J.; Sanclemente, T. Dietary-Nutritional Intervention Program for Health Promotion in the Workplace in a Company of the City of Huesca, Spain. Rev. Esp. Nutr. Hum. Diet. 2015, 19, 189. [Google Scholar] [CrossRef]
- Álvarez Velásquez, S.; Sanz Valero, J. Ventajas de La Quimioterapia Domiciliaria En Los Enfermos Adultos Con Neoplasias: Revisión Sistemática. Hosp. Domic. 2020, 4, 25–41. [Google Scholar] [CrossRef]
- Upadhyaya, M.; Sharma, S.; Pompeii, L.A.; Sianez, M.; Morgan, R.O. Obesity Prevention Worksite Wellness Interventions for Health Care Workers: A Narrative Review. Workplace Health Saf. 2020, 68, 32–49. [Google Scholar] [CrossRef] [PubMed]
- Park, S.-H.; Kim, S.-Y. Effectiveness of Worksite-Based Dietary Interventions on Employees’ Obesity: A Systematic Review and Meta-Analysis. Nutr. Res. Pract. 2019, 13, 399–409. [Google Scholar] [CrossRef]
- Schliemann, D.; Woodside, J.V. The Effectiveness of Dietary Workplace Interventions: A Systematic Review of Systematic Reviews. Public Health Nutr. 2019, 22, 942–955. [Google Scholar] [CrossRef] [PubMed]
- Fitzgerald, S.; Geaney, F.; Kelly, C.; McHugh, S.; Perry, I.J. Barriers to and Facilitators of Implementing Complex Workplace Dietary Interventions: Process Evaluation Results of a Cluster Controlled Trial. BMC Health Serv. Res. 2016, 16, 139. [Google Scholar] [CrossRef]
- Chu, A.H.Y.; Ng, S.H.X.; Tan, C.S.; Win, A.M.; Koh, D.; Müller-Riemenschneider, F. A Systematic Review and Meta-Analysis of Workplace Intervention Strategies to Reduce Sedentary Time in White-Collar Workers. Obes. Rev. Off. J. Int. Assoc. Study Obes. 2016, 17, 467–481. [Google Scholar] [CrossRef]
- Wolfenden, L.; Goldman, S.; Stacey, F.G.; Grady, A.; Kingsland, M.; Williams, C.M.; Wiggers, J.; Milat, A.; Rissel, C.; Bauman, A.; et al. Strategies to Improve the Implementation of Workplace-Based Policies or Practices Targeting Tobacco, Alcohol, Diet, Physical Activity and Obesity. Cochrane Database Syst. Rev. 2018, 11, CD012439. [Google Scholar] [CrossRef] [PubMed]
- Sawada, K.; Wada, K.; Shahrook, S.; Ota, E.; Takemi, Y.; Mori, R. Social Marketing Including Financial Incentive Programs at Worksite Cafeterias for Preventing Obesity: A Systematic Review. Syst. Rev. 2019, 8, 66. [Google Scholar] [CrossRef]
- Peñalvo, J.L.; Sagastume, D.; Mertens, E.; Uzhova, I.; Smith, J.; Wu, J.H.Y.; Bishop, E.; Onopa, J.; Shi, P.; Micha, R.; et al. Effectiveness of Workplace Wellness Programmes for Dietary Habits, Overweight, and Cardiometabolic Health: A Systematic Review and Meta-Analysis. Lancet Public Health 2021, 6, e648–e660. [Google Scholar] [CrossRef]
- LaCaille, L.J.; Schultz, J.F.; Goei, R.; LaCaille, R.A.; Dauner, K.N.; de Souza, R.; Nowak, A.V.; Regal, R. Go!: Results from a Quasi-Experimental Obesity Prevention Trial with Hospital Employees. BMC Public Health 2016, 16, 171. [Google Scholar] [CrossRef] [PubMed]
- Allan, J.; Querstret, D.; Banas, K.; de Bruin, M. Environmental Interventions for Altering Eating Behaviours of Employees in the Workplace: A Systematic Review: Environmental Interventions in Eating. Obes. Rev. 2017, 18, 214–226. [Google Scholar] [CrossRef] [PubMed]
- Vermeer, W.M.; Steenhuis, I.H.M.; Leeuwis, F.H.; Heymans, M.W.; Seidell, J.C. Small Portion Sizes in Worksite Cafeterias: Do They Help Consumers to Reduce Their Food Intake? Int. J. Obes. 2011, 35, 1200–1207. [Google Scholar] [CrossRef] [PubMed]
- Abbate, M.; Gallardo-Alfaro, L.; Bibiloni, M.D.M.; Tur, J.A. Efficacy of Dietary Intervention or in Combination with Exercise on Primary Prevention of Cardiovascular Disease: A Systematic Review. Nutr. Metab. Cardiovasc. Dis. 2020, 30, 1080–1093. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).