Association between Milk Intake and Incident Stroke among Japanese Community Dwellers: The Iwate-KENCO Study
Abstract
:1. Introduction
2. Materials and Methods
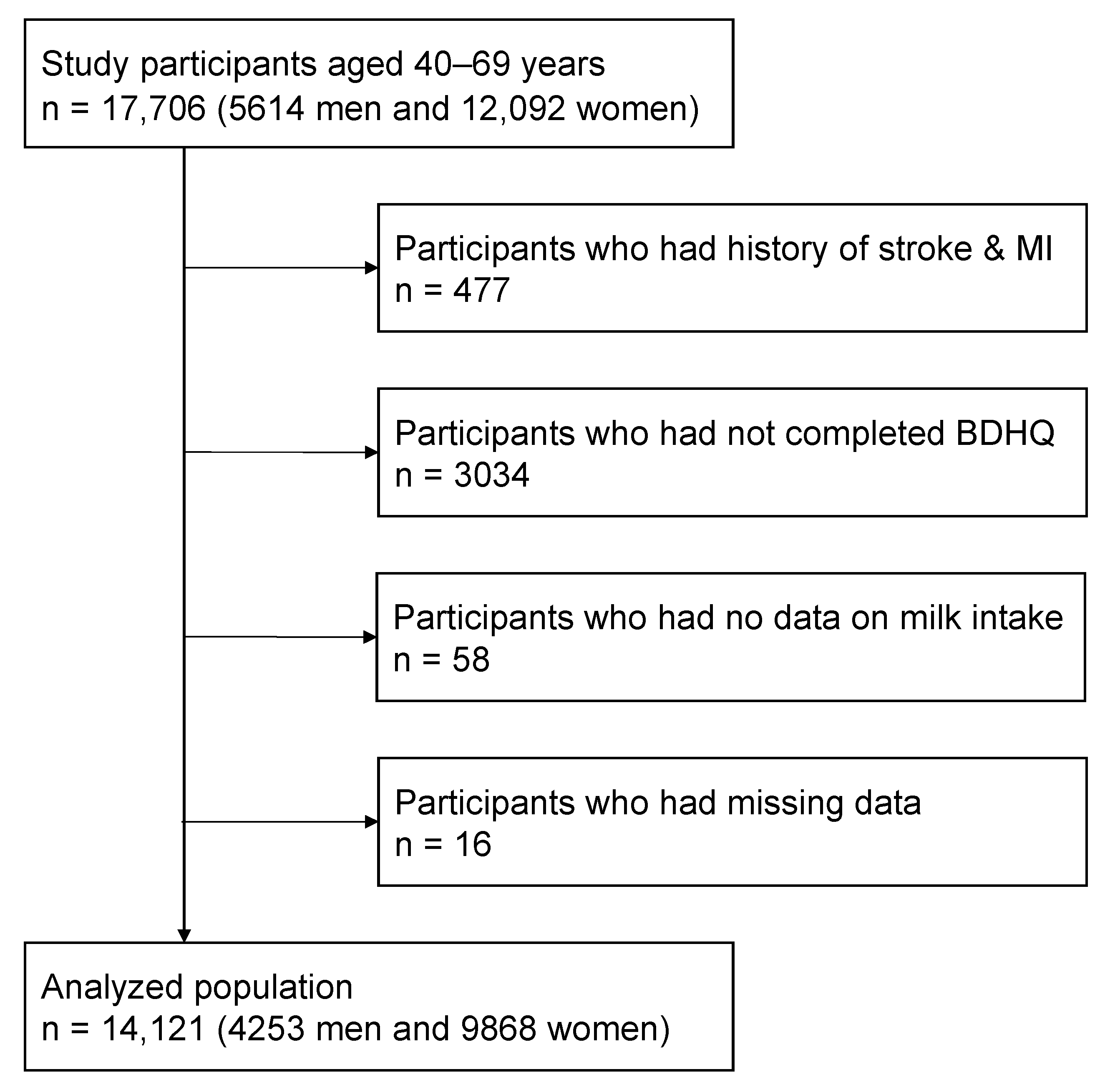
2.1. Study Population
2.2. Frequency of Milk Intake and Other Foods
2.3. Stroke Event Ascertainment
2.4. Other Measurements
2.5. Statistical Analysis
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Willett, W.C.; Ludwig, D.S. Milk and Health. N. Engl. J. Med. 2020, 382, 644–654. [Google Scholar] [CrossRef]
- FAOSTAT. New Food Balances. Available online: http://www.fao.org/faostat/en/#data/FBS (accessed on 19 December 2020).
- Ministry of Health; Labour and Welfare. National Health and Nutrition Survey Japan 2016. Available online: http://www.mhlw.go.jp/bunya/kenkou/eiyou/h28-houkoku.html (accessed on 6 October 2018).
- Quann, E.E.; Fulgoni, V.L., 3rd; Auestad, N. Consuming the daily recommended amounts of dairy products would reduce the prevalence of inadequate micronutrient intakes in the United States: Diet modeling study based on NHANES 2007–2010. Nutr. J. 2015, 14, 90. [Google Scholar] [CrossRef] [Green Version]
- National Institute for Public Health and the Environment. DNFCS 2012–2016, 1–79 Years. Available online: https://www.rivm.nl/en/dutch-national-food-consumption-survey/overview-surveys/dnfcs-2012-2016 (accessed on 19 September 2021).
- Hirahatake, K.M.; Astrup, A.; Hill, J.O.; Slavin, J.L.; Allison, D.B.; Maki, K.C. Potential Cardiometabolic Health Benefits of Full-Fat Dairy: The Evidence Base. Adv. Nutr. 2020, 11, 533–547. [Google Scholar] [CrossRef]
- Yu, E.; Hu, F.B. Dairy Products, Dairy Fatty Acids, and the Prevention of Cardiometabolic Disease: A Review of Recent Evidence. Curr. Atheroscler. Rep. 2018, 20, 24. [Google Scholar] [CrossRef]
- Drouin-Chartier, J.P.; Brassard, D.; Tessier-Grenier, M.; Cote, J.A.; Labonte, M.E.; Desroches, S.; Couture, P.; Lamarche, B. Systematic Review of the Association between Dairy Product Consumption and Risk of Cardiovascular-Related Clinical Outcomes. Adv. Nutr. 2016, 7, 1026–1040. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hata, J.; Kiyohara, Y. Epidemiology of stroke and coronary artery disease in Asia. Circ. J. 2013, 77, 1923–1932. [Google Scholar] [CrossRef] [Green Version]
- Aburto, N.J.; Hanson, S.; Gutierrez, H.; Hooper, L.; Elliott, P.; Cappuccio, F.P. Effect of increased potassium intake on cardiovascular risk factors and disease: Systematic review and meta-analyses. BMJ 2013, 346, f1378. [Google Scholar] [CrossRef] [Green Version]
- Jayedi, A.; Zargar, M.S. Dietary calcium intake and hypertension risk: A dose-response meta-analysis of prospective cohort studies. Eur. J. Clin. Nutr. 2019, 73, 969–978. [Google Scholar] [CrossRef] [PubMed]
- Kass, L.; Weekes, J.; Carpenter, L. Effect of magnesium supplementation on blood pressure: A meta-analysis. Eur. J. Clin. Nutr. 2012, 66, 411–418. [Google Scholar] [CrossRef] [PubMed]
- Soedamah-Muthu, S.S.; Verberne, L.D.; Ding, E.L.; Engberink, M.F.; Geleijnse, J.M. Dairy consumption and incidence of hypertension: A dose-response meta-analysis of prospective cohort studies. Hypertension 2012, 60, 1131–1137. [Google Scholar] [CrossRef] [Green Version]
- Hidayat, K.; Du, H.Z.; Yang, J.; Chen, G.C.; Zhang, Z.; Li, Z.N.; Qin, L.Q. Effects of milk proteins on blood pressure: A meta-analysis of randomized control trials. Hypertens. Res. 2017, 40, 264–270. [Google Scholar] [CrossRef]
- Soedamah-Muthu, S.S.; de Goede, J. Dairy Consumption and Cardiometabolic Diseases: Systematic Review and Updated Meta-Analyses of Prospective Cohort Studies. Curr. Nutr. Rep. 2018, 7, 171–182. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alexander, D.D.; Bylsma, L.C.; Vargas, A.J.; Cohen, S.S.; Doucette, A.; Mohamed, M.; Irvin, S.R.; Miller, P.E.; Watson, H.; Fryzek, J.P. Dairy consumption and CVD: A systematic review and meta-analysis. Br. J. Nutr. 2016, 115, 737–750. [Google Scholar] [CrossRef] [Green Version]
- Mullie, P.; Pizot, C.; Autier, P. Daily milk consumption and all-cause mortality, coronary heart disease and stroke: A systematic review and meta-analysis of observational cohort studies. BMC Public Health 2016, 16, 1236. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- de Goede, J.; Soedamah-Muthu, S.S.; Pan, A.; Gijsbers, L.; Geleijnse, J.M. Dairy Consumption and Risk of Stroke: A Systematic Review and Updated Dose-Response Meta-Analysis of Prospective Cohort Studies. J. Am. Heart Assoc. 2016, 5, e002787. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hu, D.; Huang, J.; Wang, Y.; Zhang, D.; Qu, Y. Dairy foods and risk of stroke: A meta-analysis of prospective cohort studies. Nutr. Metab. Cardiovasc. Dis. 2014, 24, 460–469. [Google Scholar] [CrossRef]
- Kinjo, Y.; Beral, V.; Akiba, S.; Key, T.; Mizuno, S.; Appleby, P.; Yamaguchi, N.; Watanabe, S.; Doll, R. Possible protective effect of milk, meat and fish for cerebrovascular disease mortality in Japan. J. Epidemiol. 1999, 9, 268–274. [Google Scholar] [CrossRef] [Green Version]
- Sauvaget, C.; Nagano, J.; Allen, N.; Grant, E.J.; Beral, V. Intake of animal products and stroke mortality in the Hiroshima/Nagasaki Life Span Study. Int. J. Epidemiol. 2003, 32, 536–543. [Google Scholar] [CrossRef]
- Kondo, I.; Ojima, T.; Nakamura, M.; Hayasaka, S.; Hozawa, A.; Saitoh, S.; Ohnishi, H.; Akasaka, H.; Hayakawa, T.; Murakami, Y.; et al. Consumption of dairy products and death from cardiovascular disease in the Japanese general population: The NIPPON DATA80. J. Epidemiol. 2013, 23, 47–54. [Google Scholar] [CrossRef] [Green Version]
- Ohsawa, M.; Itai, K.; Tanno, K.; Onoda, T.; Ogawa, A.; Nakamura, M.; Kuribayashi, T.; Yoshida, Y.; Kawamura, K.; Sasaki, S.; et al. Cardiovascular risk factors in the Japanese northeastern rural population. Int. J. Cardiol. 2009, 137, 226–235. [Google Scholar] [CrossRef]
- Ohsawa, M.; Itai, K.; Onoda, T.; Tanno, K.; Sasaki, S.; Nakamura, M.; Ogawa, A.; Sakata, K.; Kawamura, K.; Kuribayashi, T.; et al. Dietary intake of n-3 polyunsaturated fatty acids is inversely associated with CRP levels, especially among male smokers. Atherosclerosis 2008, 201, 184–191. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, S.; Murakami, K.; Sasaki, S.; Okubo, H.; Hirota, N.; Notsu, A.; Fukui, M.; Date, C. Comparison of relative validity of food group intakes estimated by comprehensive and brief-type self-administered diet history questionnaires against 16 d dietary records in Japanese adults. Public Health Nutr. 2011, 14, 1200–1211. [Google Scholar] [CrossRef] [PubMed]
- Makita, S.; Nakamura, M.; Satoh, K.; Tanaka, F.; Onoda, T.; Kawamura, K.; Ohsawa, M.; Tanno, K.; Itai, K.; Sakata, K.; et al. Serum C-reactive protein levels can be used to predict future ischemic stroke and mortality in Japanese men from the general population. Atherosclerosis 2009, 204, 234–238. [Google Scholar] [CrossRef] [PubMed]
- Omama, S.; Yoshida, Y.; Ogasawara, K.; Ogawa, A.; Ishibashi, Y.; Ohsawa, M.; Tanno, K.; Onoda, T.; Itai, K.; Sakata, K.; et al. Incidence rate of cerebrovascular diseases in northern Japan determined from the Iwate Stroke Registry with an inventory survey system. J. Stroke Cerebrovasc. Dis. 2013, 22, e317–e322. [Google Scholar] [CrossRef]
- National Cardiovascular Center. Study Project of Monitoring System for Cardiovascular Disease commissioned by the Ministry of Health and Welfare. In Manual for the Registry and Follow-Up of Stroke; National Cardiovascular Center: Osaka, Japan, 1988. [Google Scholar]
- World Health Organization; World Health Organization MONICA Project. Event Registration Data Component, MONICA Manual Version 1.1. Document for Meeting of MONICA Principal Investigators; World Health Organization: Geneva, Switzerland, 1986. [Google Scholar]
- Mazidi, M.; Mikhailidis, D.P.; Sattar, N.; Howard, G.; Graham, I.; Banach, M.; Lipid and Blood Pressure Meta-Analysis Collaboration Group. Consumption of dairy product and its association with total and cause specific mortality—A population-based cohort study and meta-analysis. Clin. Nutr. 2019, 38, 2833–2845. [Google Scholar] [CrossRef] [PubMed]
- Dehghan, M.; Mente, A.; Rangarajan, S.; Sheridan, P.; Mohan, V.; Iqbal, R.; Gupta, R.; Lear, S.; Wentzel-Viljoen, E.; Avezum, A.; et al. Association of dairy intake with cardiovascular disease and mortality in 21 countries from five continents (PURE): A prospective cohort study. Lancet 2018, 392, 2288–2297. [Google Scholar] [CrossRef]
- Dalmeijer, G.W.; Struijk, E.A.; van der Schouw, Y.T.; Soedamah-Muthu, S.S.; Verschuren, W.M.; Boer, J.M.; Geleijnse, J.M.; Beulens, J.W. Dairy intake and coronary heart disease or stroke--a population-based cohort study. Int. J. Cardiol. 2013, 167, 925–929. [Google Scholar] [CrossRef] [Green Version]
- Praagman, J.; Franco, O.H.; Ikram, M.A.; Soedamah-Muthu, S.S.; Engberink, M.F.; van Rooij, F.J.; Hofman, A.; Geleijnse, J.M. Dairy products and the risk of stroke and coronary heart disease: The Rotterdam Study. Eur. J. Nutr. 2015, 54, 981–990. [Google Scholar] [CrossRef]
- Larsson, S.C.; Virtamo, J.; Wolk, A. Dairy consumption and risk of stroke in Swedish women and men. Stroke 2012, 43, 1775–1780. [Google Scholar] [CrossRef] [Green Version]
- Johansson, I.; Esberg, A.; Nilsson, L.M.; Jansson, J.H.; Wennberg, P.; Winkvist, A. Dairy Product Intake and Cardiometabolic Diseases in Northern Sweden: A 33-Year Prospective Cohort Study. Nutrients 2019, 11, 284. [Google Scholar] [CrossRef] [Green Version]
- Yoshiike, N.; Hayashi, F.; Takemi, Y.; Mizoguchi, K.; Seino, F. A new food guide in Japan: The Japanese food guide Spinning Top. Nutr. Rev. 2007, 65, 149–154. [Google Scholar] [CrossRef]
- Okuda, N.; Miura, K.; Okayama, A.; Okamura, T.; Abbott, R.D.; Nishi, N.; Fujiyoshi, A.; Kita, Y.; Nakamura, Y.; Miyagawa, N.; et al. Fruit and vegetable intake and mortality from cardiovascular disease in Japan: A 24-year follow-up of the NIPPON DATA80 Study. Eur. J. Clin. Nutr. 2015, 69, 482–488. [Google Scholar] [CrossRef]
- Miyagawa, N.; Miura, K.; Okuda, N.; Kadowaki, T.; Takashima, N.; Nagasawa, S.Y.; Nakamura, Y.; Matsumura, Y.; Hozawa, A.; Fujiyoshi, A.; et al. Long-chain n-3 polyunsaturated fatty acids intake and cardiovascular disease mortality risk in Japanese: A 24-year follow-up of NIPPON DATA80. Atherosclerosis 2014, 232, 384–389. [Google Scholar] [CrossRef]
- Nakamura, Y.; Ueshima, H.; Okamura, T.; Kadowaki, T.; Hayakawa, T.; Kita, Y.; Abbott, R.D.; Okayama, A.; National Integrated Project for Prospective Observation of Non-Communicable Diseases and Its Trends in the Aged, 1980 Research Group. A Japanese diet and 19-year mortality: National integrated project for prospective observation of non-communicable diseases and its trends in the aged, 1980. Br. J. Nutr. 2009, 101, 1696–1705. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Larsson, S.C.; Orsini, N.; Wolk, A. Dietary potassium intake and risk of stroke: A dose-response meta-analysis of prospective studies. Stroke 2011, 42, 2746–2750. [Google Scholar] [CrossRef]
- Larsson, S.C.; Orsini, N.; Wolk, A. Dietary magnesium intake and risk of stroke: A meta-analysis of prospective studies. Am. J. Clin. Nutr. 2012, 95, 362–366. [Google Scholar] [CrossRef] [Green Version]
- Larsson, S.C.; Orsini, N.; Wolk, A. Dietary calcium intake and risk of stroke: A dose-response meta-analysis. Am. J. Clin. Nutr. 2013, 97, 951–957. [Google Scholar] [CrossRef] [Green Version]
- Umesawa, M.; Iso, H.; Date, C.; Yamamoto, A.; Toyoshima, H.; Watanabe, Y.; Kikuchi, S.; Koizumi, A.; Kondo, T.; Inaba, Y.; et al. Dietary intake of calcium in relation to mortality from cardiovascular disease: The JACC Study. Stroke 2006, 37, 20–26. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marcone, S.; Belton, O.; Fitzgerald, D.J. Milk-derived bioactive peptides and their health promoting effects: A potential role in atherosclerosis. Br. J. Clin. Pharmacol. 2017, 83, 152–162. [Google Scholar] [CrossRef] [Green Version]
- Mena-Sanchez, G.; Becerra-Tomas, N.; Babio, N.; Salas-Salvado, J. Dairy Product Consumption in the Prevention of Metabolic Syndrome: A Systematic Review and Meta-Analysis of Prospective Cohort Studies. Adv. Nutr. 2019, 10, S144–S153. [Google Scholar] [CrossRef] [PubMed]
- Talaei, M.; Pan, A.; Yuan, J.M.; Koh, W.P. Dairy intake and risk of type 2 diabetes. Clin. Nutr. 2018, 37, 712–718. [Google Scholar] [CrossRef]
- Muto, M.; Ezaki, O. High Dietary Saturated Fat is Associated with a Low Risk of Intracerebral Hemorrhage and Ischemic Stroke in Japanese but not in Non-Japanese: A Review and Meta-Analysis of Prospective Cohort Studies. J. Atheroscler. Thromb. 2018, 25, 375–392. [Google Scholar] [CrossRef] [Green Version]
- Yamagishi, K.; Iso, H.; Tsugane, S. Saturated fat intake and cardiovascular disease in Japanese population. J. Atheroscler. Thromb. 2015, 22, 435–439. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ministry of Health; Labour and Welfare. National Health and Nurtrional Survey 2003. Available online: https://www.mhlw.go.jp/bunya/kenkou/eiyou-chosa2-01/index.html (accessed on 26 February 2021).
- Ministry of Agriculture; Forestry and Fisheries. Statistical Survey on Milk and Dairy Products 2003. Available online: https://www.e-stat.go.jp/stat-search/files?page=1&layout=datalist&toukei=00500225&tstat=000001015114&cycle=7&year=20030&month=0&tclass1=000001015842&tclass2=000001033340 (accessed on 7 August 2021).
- Japan Dairy Association. Survey on Consumption Trends of Milk and Dairy Products. Available online: https://www.j-milk.jp/report/trends/f13cn00000000xc8-att/9fgd1p0000023zn9.pdf (accessed on 26 February 2021).
- Kobayashi, S.; Honda, S.; Murakami, K.; Sasaki, S.; Okubo, H.; Hirota, N.; Notsu, A.; Fukui, M.; Date, C. Both comprehensive and brief self-administered diet history questionnaires satisfactorily rank nutrient intakes in Japanese adults. J. Epidemiol. 2012, 22, 151–159. [Google Scholar] [CrossRef] [Green Version]
- Brown, I.J.; Tzoulaki, I.; Candeias, V.; Elliott, P. Salt intakes around the world: Implications for public health. Int. J. Epidemiol. 2009, 38, 791–813. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ng, M.; Fleming, T.; Robinson, M.; Thomson, B.; Graetz, N.; Margono, C.; Mullany, E.C.; Biryukov, S.; Abbafati, C.; Abera, S.F.; et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014, 384, 766–781. [Google Scholar] [CrossRef] [Green Version]
| Milk Intake Frequency | <2 Cups/Week | 2 to <7 Cups/Week | 7 to <12 Cups/Week | ≥12 Cups/week | p for Trend | |
|---|---|---|---|---|---|---|
| Men | ||||||
| Number of participants | 1072 | 1129 | 1508 | 544 | ||
| Age (years) | 56.7 (8.6) | 57.9 (8.1) | 60.4 (7.1) | 60.1 (7.5) | <0.001 | |
| SBP (mmHg) | 128.9 (19.0) | 129.9 (19.2) | 128.3 (19.1) | 127.5 (19.3) | 0.050 | |
| HbA1c (%) | 5.06 (0.66) | 5.12 (0.78) | 5.16 (0.74) | 5.11 (0.72) | 0.077 | |
| TC (mg/dL) | 191.2 (33.5) | 192.7 (33.1) | 195.6 (31.8) | 199.8 (32.6) | <0.001 | |
| HDLC (mg/dL) | 56.6 (15.4) | 55.2 (15.0) | 56.3 (15.5) | 58.8 (15.8) | 0.003 | |
| BMI | <18.5 kg/m2 | 18 (1.7) | 14 (1.2) | 28 (1.9) | 4 (0.7) | 0.532 |
| 18.5 to <25 kg/m2 | 687 (64.1) | 667 (59.1) | 935 (62.0) | 333 (61.2) | 0.418 | |
| 25 to <30 kg/m2 | 329 (30.7) | 407 (36.0) | 501 (33.2) | 190 (34.9) | 0.185 | |
| ≥30 kg/m2 | 38 (3.5) | 41 (3.6) | 44 (2.9) | 17 (3.1) | 0.380 | |
| Smoking status | Current smoking | 519 (48.4) | 446 (39.5) | 436 (28.9) | 143 (26.3) | <0.001 |
| Ex-smoking | 252 (23.5) | 315 (27.9) | 457 (30.3) | 170 (31.3) | <0.001 | |
| Non-smoking | 301 (28.1) | 368 (32.6) | 615 (40.8) | 231 (42.5) | <0.001 | |
| Alcohol drinking status | ≥3 drinks/day | 113 (10.5) | 80 (7.1) | 61 (4.0) | 27 (5.0) | <0.001 |
| 2 to <3 drink/day | 190 (17.7) | 149 (13.2) | 203 (13.5) | 41 (7.5) | <0.001 | |
| <2 drinks/day | 455 (42.4) | 546 (48.4) | 723 (47.9) | 250 (46.0) | 0.061 | |
| Ex-drinking | 58 (5.4) | 47 (4.2) | 96 (6.4) | 40 (7.4) | 0.035 | |
| Non-drinking | 256 (23.9) | 307 (27.2) | 425 (28.2) | 186 (34.2) | <0.001 | |
| Regular exercise | 113 (10.5) | 141 (12.5) | 310 (20.6) | 113 (20.8) | <0.001 | |
| Use of antihypertensives | 188 (17.5) | 210 (18.6) | 301 (20.0) | 92 (16.9) | 0.591 | |
| Women | ||||||
| Number of participants | 1370 | 2624 | 4257 | 1617 | ||
| Age (years) | 56.3 (8.2) | 56.0 (8.0) | 58.4 (7.5) | 59.0 (7.5) | <0.001 | |
| SBP (mmHg) | 124.9 (19.9) | 121.8 (18.9) | 123.5 (19.4) | 123.3 (19.1) | 0.135 | |
| HbA1c (%) | 5.05 (0.65) | 5.06 (0.63) | 5.09 (0.63) | 5.09 (0.53) | 0.026 | |
| TC (mg/dL) | 202.2 (32.6) | 204.7 (32.8) | 208.9 (32.3) | 208.4 (30.8) | <0.001 | |
| HDLC (mg/dL) | 60.1 (14.2) | 61.9 (14.4) | 62.2 (14.2) | 63.1 (14.5) | <0.001 | |
| BMI | <18.5 kg/m2 | 52 (3.8) | 72 (2.7) | 129 (3.0) | 41 (2.5) | 0.343 |
| 18.5 to <25 kg/m2 | 779 (56.9) | 1614 (61.5) | 2682 (63.0) | 1025 (63.4) | 0.008 | |
| 25 to <30 kg/m2 | 438 (32.0) | 785 (29.9) | 1251 (29.4) | 486 (30.1) | 0.465 | |
| ≥30 kg/m2 | 101 (7.4) | 153 (5.8) | 195 (4.6) | 65 (4.0) | <0.001 | |
| Smoking status | Current smoking | 79 (5.8) | 92 (3.5) | 86 (2.0) | 37 (2.3) | <0.001 |
| Ex-smoking | 32 (2.3) | 46 (1.8) | 53 (1.2) | 16 (1.0) | <0.001 | |
| Non-smoking | 1259 (91.9) | 2486 (94.7) | 4118 (96.7) | 1564 (96.7) | <0.001 | |
| Alcohol drinking status | ≥2 drinks/day | 59 (4.3) | 64 (2.4) | 57 (1.3) | 12 (0.7) | <0.001 |
| <2 drinks/day | 200 (14.6) | 398 (15.2) | 513 (12.1) | 163 (10.1) | <0.001 | |
| Ex-drinking | 32 (2.3) | 38 (1.4) | 54 (1.3) | 31 (1.9) | 0.284 | |
| Non-drinking | 1119 (81.7) | 2171 (82.7) | 3679 (86.4) | 1421 (87.9) | <0.001 | |
| Regular exercise | 135 (9.9) | 266 (10.1) | 525 (12.3) | 215 (13.3) | <0.001 | |
| Use of antihypertensives | 268 (19.6) | 444 (16.9) | 771 (18.1) | 311 (19.2) | 0.728 | |
| Postmenopausal state | 977 (71.3) | 1872 (71.3) | 3439 (80.8) | 1326 (82.0) | <0.001 | |
| Milk Intake Frequency | <2 Cups/Week | 2 to <7 Cups/Week | 7 to <12 Cups/Week | ≥12 Cups/Week | p for Trend |
|---|---|---|---|---|---|
| Men | |||||
| Number of participants | 1072 | 1129 | 1508 | 544 | |
| Starchy foods (portion/week) | 29.8 (11.3) | 30.0 (11.0) | 29.0 (10.6) | 30.1 (12.0) | 0.443 |
| Fish (times/week) | 9.3 (6.8) | 10.1 (6.6) | 10.5 (7.1) | 11.2 (8.2) | <0.001 |
| Soy products (times/week) | 7.6 (4.5) | 7.9 (4.1) | 9.2 (4.7) | 9.8 (5.0) | <0.001 |
| Meat (times/week) | 8.3 (2.5) | 8.7 (2.5) | 8.6 (2.8) | 9.1 (3.5) | <0.001 |
| Protein foods, (fish + soy)/meats ratio | 2.1 (1.2) | 2.1 (1.2) | 2.3 (1.2) | 2.5 (1.4) | <0.001 |
| Vegetable (times/week) | 26.2 (14.3) | 27.3 (14.2) | 30.7 (15.4) | 32.0 (17.1) | <0.001 |
| Fruit (times/week) | 4.0 (4.5) | 5.2 (4.9) | 6.8 (5.8) | 7.4 (6.4) | <0.001 |
| Miso soup (cups/day) | 2.5 (1.3) | 2.5 (1.2) | 2.5 (1.1) | 2.5 (1.2) | 0.870 |
| Sugary drink (drinks/week) | 3.0 (4.7) | 2.7 (4.2) | 2.6 (4.4) | 3.1 (4.7) | 0.487 |
| Women | |||||
| Number of participants | 1370 | 2624 | 4257 | 1617 | |
| Starchy foods (portion/week) | 25.2 (8.1) | 25.7 (8.0) | 25.2 (7.9) | 26.2 (8.6) | 0.042 |
| Fish (times/week) | 9.1 (7.0) | 10.3 (7.0) | 10.7 (7.1) | 12.3 (8.6) | <0.001 |
| Soy products (times/week) | 8.2 (4.9) | 8.9 (4.6) | 9.7 (4.7) | 10.7 (5.2) | <0.001 |
| Meat (times/week) | 8.4 (2.5) | 8.8 (2.6) | 8.6 (2.6) | 8.9 (3.1) | 0.008 |
| Protein foods, (fish + soy)/meats ratio | 2.1 (1.4) | 2.2 (1.2) | 2.4 (1.4) | 2.7 (2.1) | <0.001 |
| Vegetable (times/week) | 30.2 (16.1) | 32.4 (15.4) | 35.2 (16.7) | 38.2 (18.1) | <0.001 |
| Fruit (times/week) | 5.9 (5.7) | 7.2 (5.9) | 8.6 (6.3) | 9.8 (7.2) | <0.001 |
| Miso soup (cups/day) | 2.1 (1.0) | 2.2 (1.0) | 2.1 (1.0) | 2.2 (1.0) | 0.399 |
| Sugary drink (drinks/week) | 1.6 (3.4) | 1.5 (2.8) | 1.4 (3.0) | 1.6 (3.4) | 0.648 |
| Milk Intake Frequency | <2 Cups/Week | 2 to <7 Cups/Week | 7 to <12 Cups/Week | ≥12 Cups/Week | p for Trend |
|---|---|---|---|---|---|
| Men | |||||
| Person-years | 11,268 | 11,848 | 15,986 | 5764 | |
| Total stroke | |||||
| Number of cases | 49 | 64 | 70 | 25 | |
| Crude incidence rate | 4.35 | 5.40 | 4.38 | 4.34 | |
| HR (95% CI) | |||||
| Model 1 | 1 | 1.18 (0.81–1.71) | 0.84 (0.58–1.21) | 0.83 (0.51–1.35) | 0.500 |
| Model 2 | 1 | 1.22 (0.84–1.77) | 0.92 (0.63–1.33) | 0.93 (0.57–1.51) | 0.885 |
| Model 3 | 1 | 1.24 (0.84–1.82) | 0.93 (0.63–1.36) | 0.95 (0.57–1.57) | 0.985 |
| Model 4 | 1 | 1.21 (0.83–1.79) | 0.99 (0.67–1.46) | 0.97 (0.59–1.61) | 0.810 |
| Ischemic stroke | |||||
| Number of cases | 31 | 42 | 50 | 11 | |
| Crude incidence rate | 2.75 | 3.54 | 3.13 | 1.91 | |
| HR (95% CI) | |||||
| Model 1 | 1 | 1.21 (0.76–1.93) | 0.92 (0.58–1.44) | 0.56 (0.28–1.12) | 0.165 |
| Model 2 | 1 | 1.24 (0.78–1.98) | 0.99 (0.62–1.56) | 0.61 (0.31–1.23) | 0.289 |
| Model 3 | 1 | 1.28 (0.80–2.06) | 1.01 (0.63–1.62) | 0.61 (0.30–1.27) | 0.364 |
| Model 4 | 1 | 1.27 (0.79–2.05) | 1.07 (0.66–1.71) | 0.64 (0.31–1.34) | 0.491 |
| Haemorrhagic stroke | |||||
| Number of cases | 18 | 21 | 20 | 13 | |
| Crude incidence rate | 1.60 | 1.77 | 1.25 | 2.26 | |
| HR (95% CI) | |||||
| Model 1 | 1 | 1.06 (0.57–2.00) | 0.68 (0.36–1.29) | 1.23 (0.60–2.53) | 0.586 |
| Model 2 | 1 | 1.12 (0.59–2.11) | 0.77 (0.40–1.47) | 1.42 (0.69–2.95) | 0.331 |
| Model 3 | 1 | 1.09 (0.56–2.10) | 0.76 (0.39–1.49) | 1.44 (0.68–3.04) | 0.295 |
| Model 4 | 1 | 1.04 (0.53–2.01) | 0.82 (0.42–1.61) | 1.39 (0.66–2.94) | 0.281 |
| Women | |||||
| Person-years | 14,657 | 28,098 | 45,822 | 17,218 | |
| Total stroke | |||||
| Number of cases | 50 | 61 | 104 | 55 | |
| Crude incidence rate | 3.41 | 2.17 | 2.27 | 3.19 | |
| HR (95% CI) | |||||
| Model 1 | 1 | 0.65 (0.45–0.95) | 0.59 (0.42–0.83) | 0.80 (0.55–1.18) | 0.536 |
| Model 2 | 1 | 0.66 (0.45–0.96) | 0.60 (0.43–0.84) | 0.81 (0.55–1.20) | 0.590 |
| Model 3 | 1 | 0.66 (0.44–0.98) | 0.67 (0.47–0.95) | 0.91 (0.61–1.37) | 0.909 |
| Model 4 | 1 | 0.71 (0.47–1.05) | 0.73 (0.51–1.05 | 1.03 (0.68–1.55) | 0.567 |
| Ischemic stroke | |||||
| Number of cases | 28 | 31 | 42 | 28 | |
| Crude incidence rate | 1.91 | 1.10 | 0.92 | 1.63 | |
| HR (95% CI) | |||||
| Model 1 | 1 | 0.60 (0.36–0.999) | 0.41 (0.26–0.67) | 0.70 (0.41–1.18) | 0.153 |
| Model 2 | 1 | 0.60 (0.36–1.01) | 0.41 (0.26–0.67) | 0.70 (0.41–1.18) | 0.152 |
| Model 3 | 1 | 0.65 (0.38–1.11) | 0.48 (0.29–0.79) | 0.77 (0.44–1.35) | 0.322 |
| Model 4 | 1 | 0.69 (0.40–1.18) | 0.53 (0.32–0.88) | 0.89 (0.50–1.57) | 0.572 |
| Haemorrhagic stroke | |||||
| Number of cases | 22 | 29 | 61 | 26 | |
| Crude incidence rate | 1.50 | 1.03 | 1.33 | 1.51 | |
| HR (95% CI) | |||||
| Model 1 | 1 | 0.70 (0.40–1.22) | 0.81 (0.50–1.33) | 0.90 (0.51–1.59) | 0.664 |
| Model 2 | 1 | 0.71 (0.41–1.24) | 0.84 (0.51–1.37) | 0.93 (0.53–1.65) | 0.584 |
| Model 3 | 1 | 0.65 (0.36–1.17) | 0.91 (0.55–1.53) | 1.06 (0.58–1.93) | 0.300 |
| Model 4 | 1 | 0.70 (0.39–1.26) | 0.98 (0.59–1.64) | 1.17 (0.64–2.15) | 0.195 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tanno, K.; Yonekura, Y.; Okuda, N.; Kuribayashi, T.; Yabe, E.; Tsubota-Utsugi, M.; Omama, S.; Onoda, T.; Ohsawa, M.; Ogasawara, K.; et al. Association between Milk Intake and Incident Stroke among Japanese Community Dwellers: The Iwate-KENCO Study. Nutrients 2021, 13, 3781. https://doi.org/10.3390/nu13113781
Tanno K, Yonekura Y, Okuda N, Kuribayashi T, Yabe E, Tsubota-Utsugi M, Omama S, Onoda T, Ohsawa M, Ogasawara K, et al. Association between Milk Intake and Incident Stroke among Japanese Community Dwellers: The Iwate-KENCO Study. Nutrients. 2021; 13(11):3781. https://doi.org/10.3390/nu13113781
Chicago/Turabian StyleTanno, Kozo, Yuki Yonekura, Nagako Okuda, Toru Kuribayashi, En Yabe, Megumi Tsubota-Utsugi, Shinichi Omama, Toshiyuki Onoda, Masaki Ohsawa, Kuniaki Ogasawara, and et al. 2021. "Association between Milk Intake and Incident Stroke among Japanese Community Dwellers: The Iwate-KENCO Study" Nutrients 13, no. 11: 3781. https://doi.org/10.3390/nu13113781
APA StyleTanno, K., Yonekura, Y., Okuda, N., Kuribayashi, T., Yabe, E., Tsubota-Utsugi, M., Omama, S., Onoda, T., Ohsawa, M., Ogasawara, K., Tanaka, F., Asahi, K., Itabashi, R., Ito, S., Ishigaki, Y., Takahashi, F., Koshiyama, M., Sasaki, R., Fujimaki, D., ... Okayama, A. (2021). Association between Milk Intake and Incident Stroke among Japanese Community Dwellers: The Iwate-KENCO Study. Nutrients, 13(11), 3781. https://doi.org/10.3390/nu13113781







