Health-Related Lifestyle Profiles in Healthy Adults: Associations with Sociodemographic Indicators, Dispositional Optimism, and Sense of Coherence
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Procedure
2.2. Sociodemographic Indicators
2.3. Lifestyle Measures
2.3.1. Diet
2.3.2. Alcohol Consumption
2.3.3. Physical Activity
2.3.4. Cigarette Smoking Behavior
2.3.5. Cardiovascular Screening
2.4. Psychological Measures
2.4.1. Dispositional Optimism
2.4.2. Sense of Coherence
2.5. Data Analysis
3. Results
3.1. Study Sample
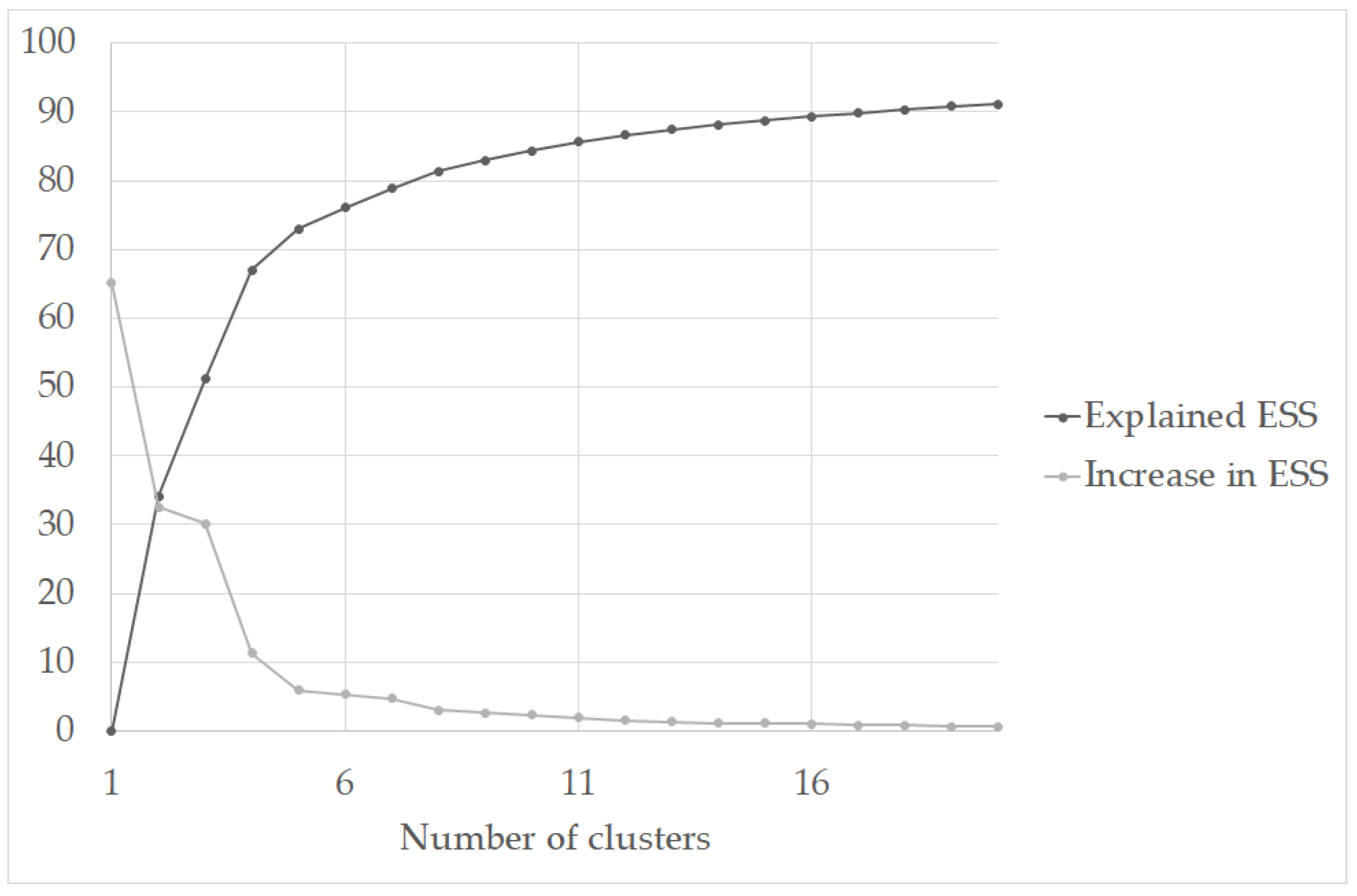
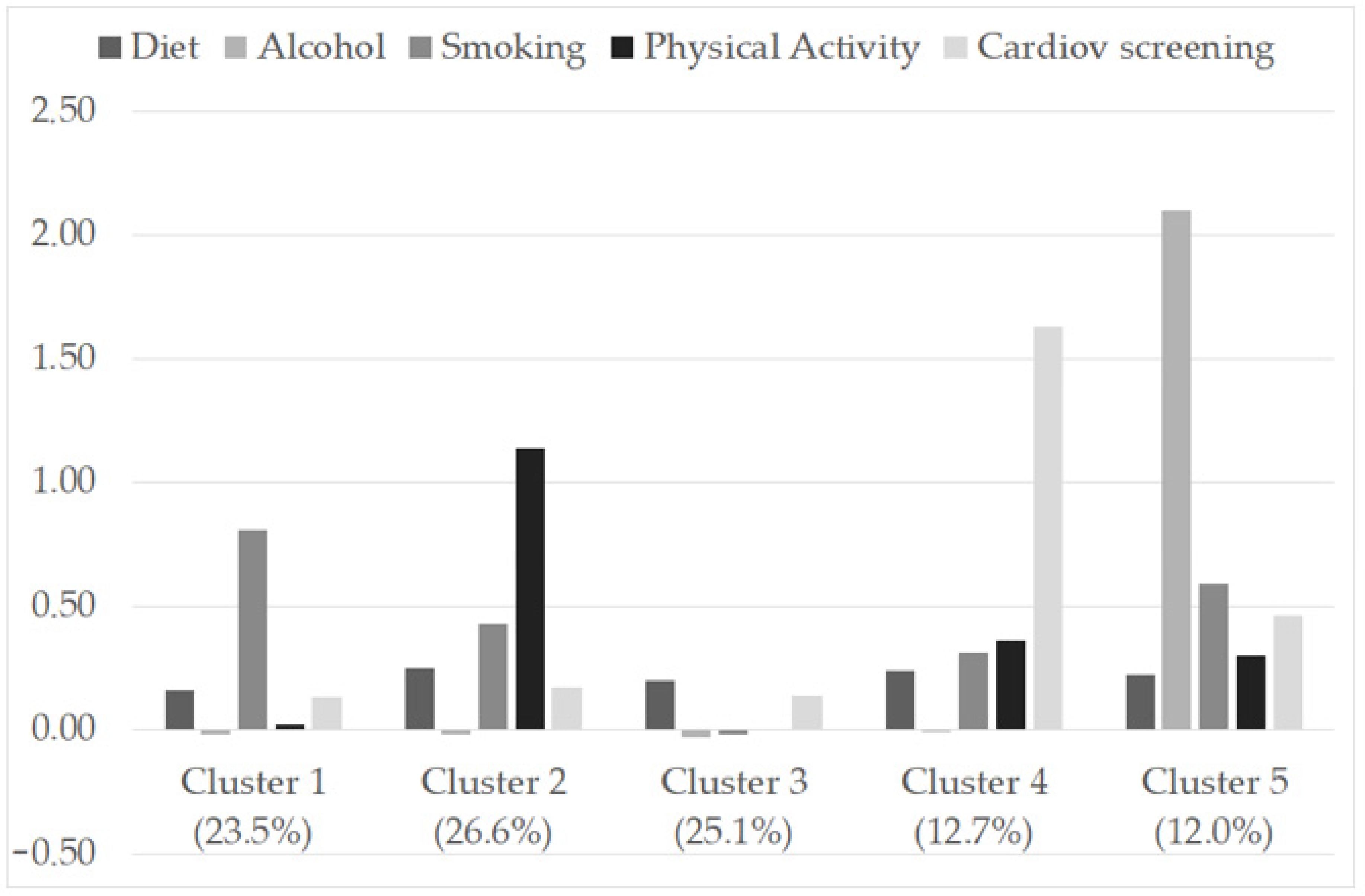
3.2. Identification of Lifestyle Profiles
3.3. Associations between Lifestyle Profile, Sociodemographic, and Psychological Variables
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Arnett, D.K.; Blumenthal, R.S.; Albert, M.A.; Buroker, A.B.; Goldberger, Z.D.; Hahn, E.J.; Himmelfarb, C.D.; Khera, A.; Lloyd-Jones, D.; McEvoy, J.W.; et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: Executive summary. J. Am. Coll. Cardiol. 2019, 74, 1376–1414. [Google Scholar] [CrossRef] [PubMed]
- Timmis, A.; Townsend, N.; Gale, C.P.; Torbica, A.; Lettino, M.; Petersen, S.E.; Mossialos, E.A.; Maggioni, A.P.; Kazakiewicz, D.; May, H.T.; et al. European Society of Cardiology: Cardiovascular disease statistics 2019. Eur. Heart J. 2020, 41, 12–85. [Google Scholar] [CrossRef] [PubMed]
- Claas, S.A.; Arnett, D.K. The role of healthy lifestyle in the primordial prevention of cardiovascular disease. Curr. Cardiol. Rep. 2016, 18, 56. [Google Scholar] [CrossRef]
- De Backer, G. Epidemiology and prevention of cardiovascular disease: Quo vadis? Eur. J. Prev. Cardiol. 2017, 24, 768–772. [Google Scholar] [CrossRef] [PubMed]
- Piepoli, M.F.; Hoes, A.W.; Agewall, S.; Albus, C.; Brotons, C.; Catapano, A.L.; Cooney, M.-T.; Corrà, U.; Cosyns, B.; Deaton, C.; et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The sixth joint task force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in clinical practice (constituted by representatives of 10 societies and by invited experts) developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur. Heart J. 2016, 37, 2315–2381. [Google Scholar] [CrossRef]
- Scicchitano, P.; Cameli, M.; Maiello, M.; Modesti, P.A.; Muiesan, M.L.; Novo, S.; Palmiero, P.; Saba, P.S.; Pedrinelli, R.; Ciccone, M.M. Nutraceuticals and dyslipidaemia: Beyond the common therapeutics. J. Funct. Foods 2014, 6, 11–32. [Google Scholar] [CrossRef]
- Mawditt, C.; Sacker, A.; Britton, A.; Kelly, Y.; Cable, N. The clustering of health-related behaviours in a british population sample: Testing for cohort differences. Prev. Med. 2016, 88, 95–107. [Google Scholar] [CrossRef] [PubMed]
- Meader, N.; King, K.; Moe-Byrne, T.; Wright, K.; Graham, H.; Petticrew, M.; Power, C.; White, M.; Sowden, A.J. A systematic review on the clustering and co-occurrence of multiple risk behaviours. BMC Public Health 2016, 16, 657. [Google Scholar] [CrossRef]
- Noble, N.; Paul, C.; Turon, H.; Oldmeadow, C. Which modifiable health risk behaviours are related? A systematic review of the clustering of Smoking, Nutrition, Alcohol and Physical Activity (‘SNAP’) health risk factors. Prev. Med. 2015, 81, 16–41. [Google Scholar] [CrossRef]
- Morris, L.J.; D’Este, C.; Sargent-Cox, K.; Anstey, K.J. Concurrent lifestyle risk factors: Clusters and determinants in an Australian sample. Prev. Med. 2016, 84, 1–5. [Google Scholar] [CrossRef]
- Palaniappan, U.; Jacobs Starkey, L.; O’Loughlin, J.; Gray-Donald, K. Fruit and vegetable consumption is lower and saturated fat intake is higher among Canadians reporting smoking. J. Nutr. 2001, 131, 1952–1958. [Google Scholar] [CrossRef] [PubMed]
- Schuit, A.J.; van Loon, A.J.M.; Tijhuis, M.; Ocké, M. Clustering of lifestyle risk factors in a general adult population. Prev. Med. 2002, 35, 219–224. [Google Scholar] [CrossRef]
- Monzani, D.; D’Addario, M.; Fattirolli, F.; Giannattasio, C.; Greco, A.; Quarenghi, F.; Steca, P. Clustering of lifestyle risk factors in acute coronary syndrome: Prevalence and change after the first event. Appl. Psychol. Health Well-Being 2018, 10, 434–456. [Google Scholar] [CrossRef] [PubMed]
- Steca, P.; Monzani, D.; Greco, A.; Franzelli, C.; Magrin, M.E.; Miglioretti, M.; Sarini, M.; Scrignaro, M.; Vecchio, L.; Fattirolli, F.; et al. Stability and change of lifestyle profiles in cardiovascular patients after their first acute coronary event. PLoS ONE 2017, 12, e0183905. [Google Scholar] [CrossRef]
- Szlejf, C.; Suemoto, C.K.; Santos, I.S.; Brunoni, A.R.; Nunes, M.A.; Viana, M.C.; Barreto, S.M.; Lotufo, P.A.; Benseñor, I.M. Poorer cardiovascular health is associated with psychiatric comorbidity: Results from the ELSA-Brasil study. Int. J. Cardiol. 2019, 274, 358–365. [Google Scholar] [CrossRef]
- Greco, A.; Brugnera, A.; Adorni, R.; D’Addario, M.; Fattirolli, F.; Franzelli, C.; Giannattasio, C.; Maloberti, A.; Zanatta, F.; Steca, P. Protein Intake and Physical Activity in Newly Diagnosed Patients with Acute Coronary Syndrome: A 5-Year Longitudinal Study. Nutrients 2021, 13, 634. [Google Scholar] [CrossRef] [PubMed]
- Murray, J.; Craigs, C.L.; Hill, K.M.; Honey, S.; House, A. A Systematic Review of Patient Reported Factors Associated with Uptake and Completion of Cardiovascular Lifestyle Behaviour Change. BMC Cardiovasc. Disord. 2012, 12, 120. [Google Scholar] [CrossRef] [PubMed]
- Kubzansky, L.D.; Huffman, J.C.; Boehm, J.K.; Hernandez, R.; Kim, E.S.; Koga, H.K.; Feig, E.H.; Lloyd-Jones, D.M.; Seligman, M.E.P.; Labarthe, D.R. Positive Psychological Well-Being and Cardiovascular Disease: JACC Health Promotion Series. J. Am. Coll. Cardiol. 2018, 72, 1382–1396. [Google Scholar] [CrossRef]
- Carver, C.S.; Scheier, M. On the Self-Regulation of Behavior; Cambridge University Press: Cambridge, UK; New York, NY, USA, 1998. [Google Scholar]
- Antonovsky, A. Health, Stress, and Coping: New Perspectives on Mental and Physical Well-Being; Jossey-Bass Publishers: San Francisco, CA, USA, 1979. [Google Scholar]
- Scheier, M.F.; Carver, C.S. Dispositional Optimism and Physical Health: A Long Look Back, a Quick Look Forward. Am. Psychol. 2018, 73, 1082–1094. [Google Scholar] [CrossRef] [PubMed]
- Boehm, J.K.; Chen, Y.; Koga, H.; Mathur, M.B.; Vie, L.L.; Kubzansky, L.D. Is Optimism Associated with Healthier Cardiovascular-Related Behavior? Meta-Analyses of 3 Health Behaviors. Circ. Res. 2018, 122, 1119–1134. [Google Scholar] [CrossRef] [PubMed]
- Trudel-Fitzgerald, C.; James, P.; Kim, E.S.; Zevon, E.S.; Grodstein, F.; Kubzansky, L.D. Prospective Associations of Happiness and Optimism with Lifestyle over up to Two Decades. Prev. Med. 2019, 126, 105754. [Google Scholar] [CrossRef]
- Serlachius, A.; Pulkki-Råback, L.; Elovainio, M.; Hintsanen, M.; Mikkilä, V.; Laitinen, T.T.; Jokela, M.; Rosenström, T.; Josefsson, K.; Juonala, M.; et al. Is Dispositional Optimism or Dispositional Pessimism Predictive of Ideal Cardiovascular Health? The Young Finns Study. Psychol. Health 2015, 30, 1221–1239. [Google Scholar] [CrossRef] [PubMed]
- Pänkäläinen, M.; Fogelholm, M.; Valve, R.; Kampman, O.; Kauppi, M.; Lappalainen, E.; Hintikka, J. Pessimism, Diet, and the Ability to Improve Dietary Habits: A Three-Year Follow-up Study among Middle-Aged and Older Finnish Men and Women. Nutr. J. 2018, 17, 92. [Google Scholar] [CrossRef]
- Gerend, M.A.; Aiken, L.S.; West, S.G. Personality Factors in Older Women’s Perceived Susceptibility to Diseases of Aging. J. Pers. 2004, 72, 243–270. [Google Scholar] [CrossRef]
- Hamilton, J.G.; Lobel, M. Psychosocial Factors Associated with Risk Perceptions for Chronic Diseases in Younger and Middle-Aged Women. Women Health 2015, 55, 921–942. [Google Scholar] [CrossRef]
- Mosca, L.; Mochari, H.; Christian, A.; Berra, K.; Taubert, K.; Mills, T.; Burdick, K.A.; Simpson, S.L. National study of women’s awareness, preventive action, and barriers to cardiovascular health. Circulation 2006, 113, 525–534. [Google Scholar] [CrossRef] [PubMed]
- Eriksson, M.; Lindstrom, B. Antonovsky’s Sense of Coherence Scale and the Relation with Health: A Systematic Review. J. Epidemiol. Commun. Health 2006, 60, 376–381. [Google Scholar] [CrossRef] [PubMed]
- Binkowska-Bury, M.; Iwanowicz-Palus, G.; Kruk, W.; Perenc, L.; Mazur, A.; Filip, R.; Januszewicz, P. Pro-Health Behaviours—A Sense of Coherence as the Key to a Healthy Lifestyle in Rural Areas? Ann. Agric. Environ. Med. 2016, 23, 345–349. [Google Scholar] [CrossRef][Green Version]
- Wainwright, N.W.J.; Surtees, P.G.; Welch, A.A.; Luben, R.N.; Khaw, K.-T.; Bingham, S.A. Healthy Lifestyle Choices: Could Sense of Coherence Aid Health Promotion? J. Epidemiol. Commun. Health 2007, 61, 871–876. [Google Scholar] [CrossRef]
- Riera-Sampol, A.; Bennasar-Veny, M.; Tauler, P.; Nafría, M.; Colom, M.; Aguilo, A. Association between Depression, Lifestyles, Sleep Quality, and Sense of Coherence in a Population with Cardiovascular Risk. Nutrients 2021, 13, 585. [Google Scholar] [CrossRef] [PubMed]
- Wainwright, N.W.J.; Surtees, P.G.; Welch, A.A.; Luben, R.N.; Khaw, K.-T.; Bingham, S.A. Sense of Coherence, Lifestyle Choices and Mortality. J. Epidemiol. Commun. Health 2008, 62, 829–831. [Google Scholar] [CrossRef] [PubMed]
- Thomas, K.; Nilsson, E.; Festin, K.; Henriksson, P.; Lowén, M.; Löf, M.; Kristenson, M. Associations of Psychosocial Factors with Multiple Health Behaviors: A Population-Based Study of Middle-Aged Men and Women. Int J. Environ. Res. Public Health 2020, 17, 1239. [Google Scholar] [CrossRef] [PubMed]
- Rabel, M.; Laxy, M.; Thorand, B.; Peters, A.; Schwettmann, L.; Mess, F. Clustering of Health-Related Behavior Patterns and Demographics. Results From the Population-Based KORA S4/F4 Cohort Study. Front. Public Health 2018, 6, 387. [Google Scholar] [CrossRef]
- Loef, M.; Walach, H. The Combined Effects of Healthy Lifestyle Behaviors on All Cause Mortality: A Systematic Review and Meta-Analysis. Prev. Med. 2012, 55, 163–170. [Google Scholar] [CrossRef]
- Ford, E.S.; Bergmann, M.M.; Boeing, H.; Li, C.; Capewell, S. Healthy Lifestyle Behaviors and All-Cause Mortality among Adults in the United States. Prev. Med. 2012, 55, 23–27. [Google Scholar] [CrossRef]
- Posadzki, P.; Stockl, A.; Musonda, P.; Tsouroufli, M. A Mixed-Method Approach to Sense of Coherence, Health Behaviors, Self-Efficacy and Optimism: Towards the Operationalization of Positive Health Attitudes. Scand. J. Psychol. 2010, 51, 246–252. [Google Scholar] [CrossRef]
- Antonovsky, A. The Structure and Properties of the Sense of Coherence Scale. Soc. Sci. Med. 1993, 36, 725–733. [Google Scholar] [CrossRef]
- Eriksson, M.; Lindstrom, B. A Salutogenic Interpretation of the Ottawa Charter. Health Promot. Int. 2008, 23, 190–199. [Google Scholar] [CrossRef]
- Abrahamsson, A.; Ejlertsson, G. A Salutogenic Perspective Could Be of Practical Relevance for the Prevention of Smoking amongst Pregnant Women. Midwifery 2002, 18, 323–331. [Google Scholar] [CrossRef]
- Magnusson, D. The Logic and Implications of a Person-Oriented Approach. In Methods and Models for Studying the Individual; Cairns, R.B., Bergman, L.R., Kagan, J., Eds.; Sage Publications, Inc.: Thousand Oaks, CA, USA, 1998; pp. 33–64. [Google Scholar]
- Pedretti, R.F.E.; Fattirolli, F.; Griffo, R.; Ambrosetti, M.; Angelino, E.; Brazzo, S.; Corrà, U.; Dasseni, N.; Faggiano, P.; Favretto, G.; et al. [Cardiac rehabilitation “3.0”: From the acute to the chronic stage. A position paper from the Italian Association for Cardiovascular Prevention and Rehabilitation (GICR-IACPR)]. G. Ital. Cardiol. 2018, 19 (Suppl. S3), 3S–40S. [Google Scholar] [CrossRef]
- Volpe, M.; Tocci, G.; Rubattu, S. Consensus Document and Recommendations for the Prevention of Cardiovascular Disease in Italy. G. Ital. Cardiol. 2018, 19 (Suppl. S1), 1S–95S. [Google Scholar]
- Tabachnick, B.G.; Fidell, L.S.; Ullman, J.B. Using Multivariate Statistics, 7th ed.; Pearson: New York, NY, USA, 2019. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Lawrence Erlbaum Associates Inc.: Mahwah, NJ, USA, 1988. [Google Scholar]
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G*Power 3: A Flexible Statistical Power Analysis Program for the Social, Behavioral, and Biomedical Sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Chen, H.; Cohen, P.; Chen, S. How Big Is a Big Odds Ratio? Interpreting the Magnitudes of Odds Ratios in Epidemiological Studies. Commun. Stat. Simul. Comput. 2010, 39, 860–864. [Google Scholar] [CrossRef]
- Giampaoli, S.; Krogh, V.; Grioni, S.; Palmieri, L.; Gulizia, M.M.; Stamler, J.; Vanuzzo, D.; Gruppo di ricerca dell’Osservatorio epidemiologico cardiovascolare/Health Examination Survey. [Eating behaviours of italian adults: Results of the Osservatorio epidemiologico cardiovascolare/Health Examination Survey]. Epidemiol. Prev. 2015, 39, 373–379. [Google Scholar] [PubMed]
- Rimm, E.B.; Giovannucci, E.L.; Willett, W.C.; Colditz, G.A.; Ascherio, A.; Rosner, B.; Stampfer, M.J. Prospective Study of Alcohol Consumption and Risk of Coronary Disease in Men. Lancet 1991, 338, 464–468. [Google Scholar] [CrossRef]
- Topolski, T.D.; LoGerfo, J.; Patrick, D.L.; Williams, B.; Walwick, J.; Patrick, M.B. The Rapid Assessment of Physical Activity (RAPA) among Older Adults. Prev. Chronic Dis. 2006, 3, A118. [Google Scholar] [PubMed]
- Baker, T.B.; Breslau, N.; Covey, L.; Shiffman, S. DSM Criteria for Tobacco Use Disorder and Tobacco withdrawal: A Critique and Proposed Revisions for DSM-5*: DSM Criteria Revision. Addiction 2012, 107, 263–275. [Google Scholar] [CrossRef] [PubMed]
- Scheier, M.F.; Carver, C.S.; Bridges, M.W. Distinguishing Optimism from Neuroticism (and Trait Anxiety, Self-Mastery, and Self-Esteem): A Reevaluation of the Life Orientation Test. J. Pers. Soc. Psychol. 1994, 67, 1063–1078. [Google Scholar] [CrossRef]
- Steca, P.; Monzani, D.; Pierobon, A.; Avvenuti, G.; Greco, A.; Giardini, A. Measuring dispositional optimism in patients with chronic heart failure and their healthcare providers: The validity of the life orientation test-revised. Patient Prefer. Adherence 2017, 11, 1497–1503. [Google Scholar] [CrossRef] [PubMed]
- Barni, D.; Tagliabue, S. Sense of coherence scale di Antonovsky: Un contributo alla validazione italiana. TPM. Test. Psicometria Metodol. 2005, 3, 151–166. [Google Scholar]
- Bergman, L.R.; El-Khouri, B.M. SLEIPNER: A Statistical Package for Pattern-Oriented Analyses; Version 2.1; Department of Psychology, Stockholm University: Stockholm, Sweden, 2002. [Google Scholar]
- Bergman, L.R.; Nurmi, J.-E.; von Eye, A.A. I-States-as-Objects-Analysis (ISOA): Extensions of an approach to studying short-term developmental processes by analyzing typical patterns. Int. J. Behav. Dev. 2012, 36, 237–246. [Google Scholar] [CrossRef]
- Bergman, L.R.; Magnusson, D.; El-Khouri, B.M. Studying Individual Development in an Interindividual Context: A Person-Oriented Approach; Psychology Press: New York, NY, USA; London, UK, 2003; Volume 4. [Google Scholar]
- Mahoney, J.L.; Stattin, H.; Magnusson, D. Youth recreation centre participation and criminal offending: A 20-year longitudinal study of Swedish boys. Int. J. Behav. Dev. 2001, 25, 509–520. [Google Scholar] [CrossRef]
- de Vries, H.; van ’t Riet, J.; Spigt, M.; Metsemakers, J.; van den Akker, M.; Vermunt, J.K.; Kremers, S. Clusters of Lifestyle Behaviors: Results from the Dutch SMILE Study. Prev. Med. 2008, 46, 203–208. [Google Scholar] [CrossRef]
- Rosenfeld, C.S. Sex-dependent differences in voluntary physical activity: Physical activity and sex differences. J. Neurosci. Res. 2017, 95, 279–290. [Google Scholar] [CrossRef] [PubMed]
- Sciomer, S.; Moscucci, F.; Maffei, S.; Gallina, S.; Mattioli, A. Prevention of cardiovascular risk factors in women: The lifestyle paradox and stereotypes we need to defeat. Eur. J. Prev. Cardiol. 2019, 26, 609–610. [Google Scholar] [CrossRef]
- Calabrò, P.; Gragnano, F.; Di Maio, M.; Patti, G.; Antonucci, E.; Cirillo, P.; Gresele, P.; Palareti, G.; Pengo, V.; Pignatelli, P.; et al. Epidemiology and management of patients with acute coronary syndromes in contemporary real-world practice: Evolving trends from the EYESHOT study to the START-ANTIPLATELET registry. Angiology 2018, 69, 795–802. [Google Scholar] [CrossRef]
- Di Giosia, P.; Passacquale, G.; Petrarca, M.; Giorgini, P.; Marra, A.M.; Ferro, A. gender differences in cardiovascular prophylaxis: Focus on antiplatelet treatment. Pharmacol. Res. 2017, 119, 36–47. [Google Scholar] [CrossRef]
- Maas, A.H.E.M.; Appelman, Y.E.A. Gender differences in coronary heart disease. Neth. Heart J. 2010, 18, 598–602. [Google Scholar] [CrossRef]
- Groenhof, T.K.J.; van Rijn, B.B.; Franx, A.; Roeters van Lennep, J.E.; Bots, M.L.; Lely, A.T. Preventing cardiovascular disease after hypertensive disorders of pregnancy: Searching for the how and when. Eur. J. Prev. Cardiol. 2017, 24, 1735–1745. [Google Scholar] [CrossRef]
- Bergman, E.; Malm, D.; Karlsson, J.-E.; Berterö, C. Longitudinal Study of Patients after Myocardial Infarction: Sense of Coherence, Quality of Life, and Symptoms. Heart Lung 2009, 38, 129–140. [Google Scholar] [CrossRef]
- Paulhus, D.L.; Vazire, S. The self-report method. In Handbook of Research Methods in Personality Psychology; Robins, R.W., Fraley, R.C., Krueger, R., Eds.; Guilford Press: New York, NY, USA, 2007; pp. 224–239. [Google Scholar]
- Lee, M.; Lee, H.; Kim, Y.; Kim, J.; Cho, M.; Jang, J.; Jang, H. mobile app-based health promotion programs: A systematic review of the literature. Int. J. Environ. Res. Public Health 2018, 15, 2838. [Google Scholar] [CrossRef]
| Sociodemographic Variables | |
|---|---|
| Age, mean (SD) | 34.7 (11.6) |
| Gender, n (%) | |
| Female | 363 (53.7%) |
| Male | 313 (46.3%) |
| Educational level, n (%) | |
| high school or less | 310 (45.9%) |
| higher than high school | 366 (54.1%) |
| Family history of cardiovascular disease | |
| yes | 492 (72.8%) |
| no | 184 (27.2%) |
| Goodness-of-Fit Indices | 3-Cluster | 5-Cluster |
|---|---|---|
| Explained ESS | 51.2095 | 72.9547 |
| Point-biserial correlation | 0.7850 | 0.5007 |
| C-index | 0.2028 | 0.1007 |
| Gamma index | 0.9272 | 0.8658 |
| W/B index | 0.2718 | 0.1968 |
| G+ index | 0.0175 | 0.0229 |
| Cluster | N (%) | Mean Age (SD) | % Male | % Healthy Lifestyles | ||||
|---|---|---|---|---|---|---|---|---|
| Diet | Alcohol Consumption | Physical Activity | Cigarette Smoking | Cardiovascular Screening | ||||
| 1 | 159 (23.5%) | 33.6 (11.8) | 43.4% | 23.3% | 89.9% | 0.0% | 100.0% | 50.9% |
| 2 | 180 (26.6%) | 33.0 (10.7) | 57.8% | 36.7% | 90.0% | 100.0% | 68.9% | 58.9% |
| 3 | 170 (25.1%) | 33.1 (11.0) | 38.8% | 31.8% | 86.5% | 0.0% | 28.8% | 52.4% |
| 4 | 86 (12.7%) | 38.9 (12.1) | 55.8% | 37.2% | 94.2% | 32.6% | 53.5% | 100.0% |
| 5 | 81 (12.0%) | 39.0 (11.9) | 32.1% | 38.3% | 100.0% | 29.6% | 82.7% | 70.4% |
| 95% CI | ||||||||
|---|---|---|---|---|---|---|---|---|
| Cluster | Predictor | Estimate | SE | Z | p | OR | Lower | Upper |
| 1–3 | Intercept | −0.69 | 0.68 | −1.02 | 0.306 | 0.50 | 0.13 | 1.88 |
| Age | 0.01 | 0.01 | 0.57 | 0.570 | 1.01 | 0.99 | 1.03 | |
| Gender | 0.24 | 0.24 | 1.02 | 0.308 | 1.27 | 0.80 | 2.03 | |
| Education | 0.01 | 0.24 | 0.04 | 0.971 | 1.01 | 0.64 | 1.60 | |
| Family history of CVD | −0.13 | 0.26 | −0.50 | 0.615 | 0.88 | 0.53 | 1.46 | |
| Optimism | −0.15 | 0.16 | −0.92 | 0.360 | 0.86 | 0.63 | 1.18 | |
| SOC: Comprehensibility | −0.40 | 0.18 | −2.21 | 0.027 | 0.67 | 0.47 | 0.96 | |
| SOC: Manageability | 0.36 | 0.15 | 2.33 | 0.020 | 1.43 | 1.06 | 1.93 | |
| SOC: Meaningfulness | 0.22 | 0.13 | 1.70 | 0.090 | 1.25 | 0.97 | 1.61 | |
| 2–3 | Intercept | −1.52 | 0.68 | −2.23 | 0.026 | 0.22 | 0.06 | 0.83 |
| Age | −0.00 | 0.01 | −0.36 | 0.722 | 1.00 | 0.98 | 1.02 | |
| Gender | 0.87 | 0.23 | 3.77 | <0.001 | 2.40 | 1.52 | 3.78 | |
| Education | 0.07 | 0.23 | 0.28 | 0.777 | 1.07 | 0.68 | 1.68 | |
| Family history of CVD | 0.10 | 0.24 | 0.43 | 0.667 | 1.11 | 0.69 | 1.79 | |
| Optimism | 0.26 | 0.16 | 1.66 | 0.096 | 1.30 | 0.95 | 1.78 | |
| SOC: Comprehensibility | −0.30 | 0.18 | −1.72 | 0.086 | 0.74 | 0.52 | 1.04 | |
| SOC: Manageability | 0.12 | 0.15 | 0.83 | 0.407 | 1.13 | 0.85 | 1.51 | |
| SOC: Meaningfulness | 0.22 | 0.13 | 1.72 | 0.085 | 1.25 | 0.97 | 1.60 | |
| 4–3 | Intercept | −2.24 | 0.80 | −2.80 | 0.005 | 0.11 | 0.02 | 0.51 |
| Age | 0.05 | 0.01 | 3.93 | <0.001 | 1.05 | 1.02 | 1.08 | |
| Gender | 0.74 | 0.28 | 2.59 | 0.010 | 2.09 | 1.20 | 3.65 | |
| Education | 0.17 | 0.29 | 0.59 | 0.552 | 1.18 | 0.68 | 2.07 | |
| Family history of CVD | 0.10 | 0.31 | 0.34 | 0.732 | 1.11 | 0.61 | 2.03 | |
| Optimism | −0.40 | 0.20 | −2.02 | 0.043 | 0.67 | 0.46 | 0.99 | |
| SOC: Comprehensibility | −0.29 | 0.22 | −1.33 | 0.182 | 0.75 | 0.49 | 1.15 | |
| SOC: Manageability | 0.21 | 0.18 | 1.13 | 0.257 | 1.23 | 0.86 | 1.77 | |
| SOC: Meaningfulness | 0.21 | 0.15 | 1.36 | 0.175 | 1.23 | 0.91 | 1.67 | |
| 5–3 | Intercept | −1.24 | 0.81 | −1.54 | 0.124 | 0.29 | 0.06 | 1.40 |
| Age | 0.05 | 0.01 | 3.78 | <0.001 | 1.05 | 1.02 | 1.07 | |
| Gender | −0.34 | 0.30 | −1.13 | 0.257 | 0.71 | 0.40 | 1.28 | |
| Education | −0.07 | 0.29 | −0.23 | 0.815 | 0.93 | 0.53 | 1.65 | |
| Family history of CVD | 0.02 | 0.32 | 0.07 | 0.943 | 1.02 | 0.55 | 1.91 | |
| Optimism | 8.68 × 10−4 | 0.20 | 0.00 | 0.997 | 1.00 | 0.68 | 1.48 | |
| SOC: Comprehensibility | −0.40 | 0.22 | −1.83 | 0.068 | 0.67 | 0.44 | 1.03 | |
| SOC: Manageability | 0.23 | 0.19 | 1.21 | 0.227 | 1.25 | 0.87 | 1.81 | |
| SOC: Meaningfulness | −0.05 | 0.15 | −0.30 | 0.762 | 0.95 | 0.71 | 1.29 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Adorni, R.; Zanatta, F.; D’Addario, M.; Atella, F.; Costantino, E.; Iaderosa, C.; Petarle, G.; Steca, P. Health-Related Lifestyle Profiles in Healthy Adults: Associations with Sociodemographic Indicators, Dispositional Optimism, and Sense of Coherence. Nutrients 2021, 13, 3778. https://doi.org/10.3390/nu13113778
Adorni R, Zanatta F, D’Addario M, Atella F, Costantino E, Iaderosa C, Petarle G, Steca P. Health-Related Lifestyle Profiles in Healthy Adults: Associations with Sociodemographic Indicators, Dispositional Optimism, and Sense of Coherence. Nutrients. 2021; 13(11):3778. https://doi.org/10.3390/nu13113778
Chicago/Turabian StyleAdorni, Roberta, Francesco Zanatta, Marco D’Addario, Francesca Atella, Elena Costantino, Caterina Iaderosa, Giulia Petarle, and Patrizia Steca. 2021. "Health-Related Lifestyle Profiles in Healthy Adults: Associations with Sociodemographic Indicators, Dispositional Optimism, and Sense of Coherence" Nutrients 13, no. 11: 3778. https://doi.org/10.3390/nu13113778
APA StyleAdorni, R., Zanatta, F., D’Addario, M., Atella, F., Costantino, E., Iaderosa, C., Petarle, G., & Steca, P. (2021). Health-Related Lifestyle Profiles in Healthy Adults: Associations with Sociodemographic Indicators, Dispositional Optimism, and Sense of Coherence. Nutrients, 13(11), 3778. https://doi.org/10.3390/nu13113778







