Precision Food Parenting: A Proposed Conceptual Model and Research Agenda
Abstract
1. Introduction
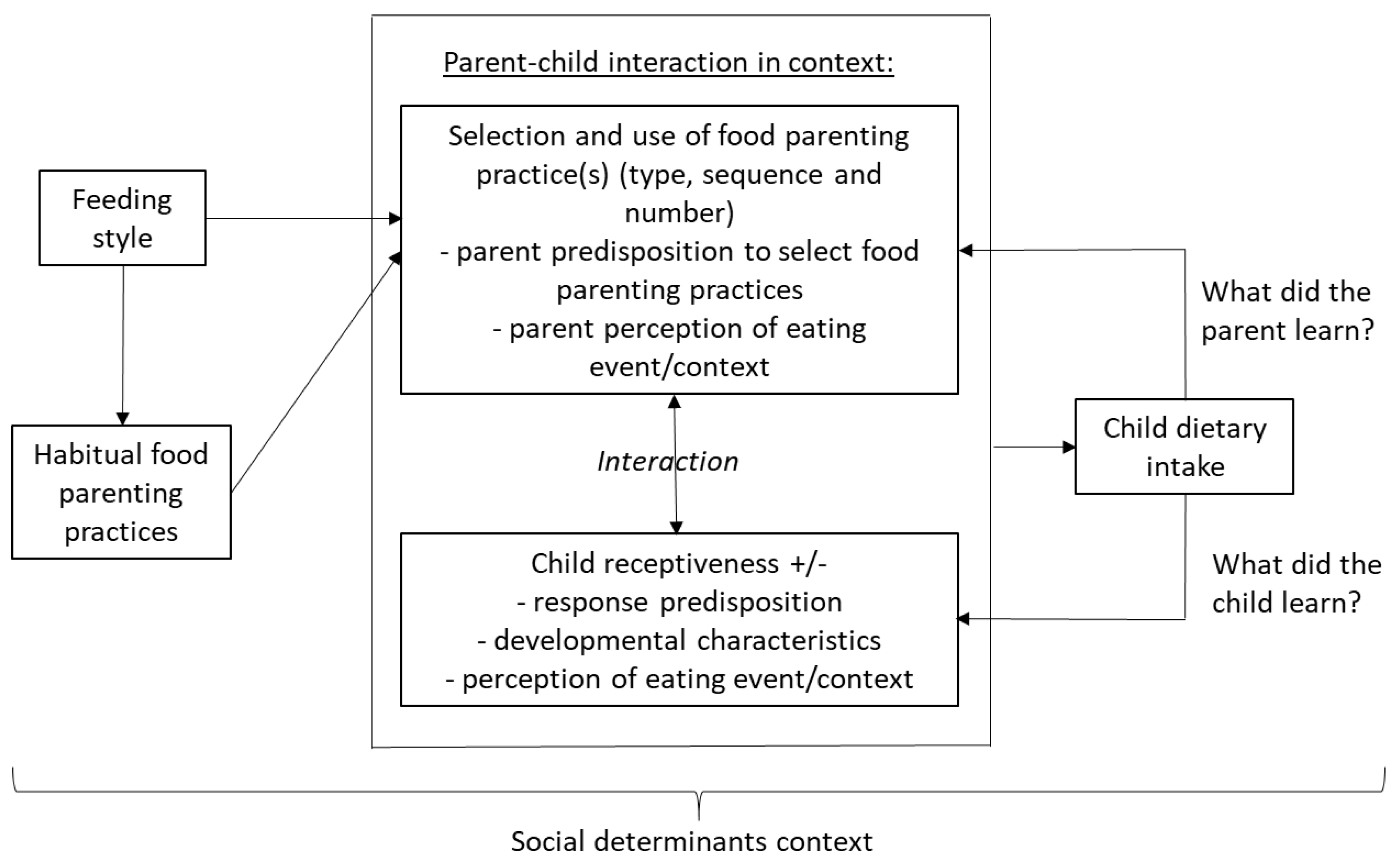
2. Feeding Styles
| Construct | Relationship to PFP | What Is Known? | What Research Is Needed? |
|---|---|---|---|
| Feeding styles | The complex interplay between the parent and the child defined by two dimensions: the parents’ demaningness and responsiveness, both in regard to the child’s food behavior | Crossing the two dimensions yields four categories of relationship: authoritative, authoritarian, permissive and uninvolved [29]. Indulgent practices lead to worse outcomes (diet, BMI) [30]. Authoritarian practices lead to the lowest BMI [31]. | How consistently are the categories related to FPP, especially among goal oriented FPP? Are there critical other dimensions of this relationship? |
| Habitual FPP | The specific behaviors that parents use without forethought with the intent to influence their child to eat specific foods, whether successful or not. | There are 17 proposed categories of FPP [23]. Some practices are likely to increase child intake of parent specified foods, and some are not [32,33]. | To what extent do FPP reflect habit, and require a habit modification approach to change? Under what circumstances do FPP result in desired child intake? What are the longer term consequences of consistent or frequent use of FPP? What are the interrelationships among use of FPP? |
| Parent predisposition to select FPP | Diverse variables may predict a parent’s use of FPP. Among these are personality characteristics and models of behavior, e.g., model of goal directed behavior. | The model of goal directed behavior predicted use of categories of effective and ineffective FPP [34,35,36]. Little other research has addressed prediction of parent selection of FPP. | Which variable or combinations of variables predict parent use of FPP? What are the limiting factors (e.g., stress, time constraints, depression, lack of financial resources) on the predictiveness of these variables? |
| Selection and use of FPP | Parents must select and use specific FPP in specific contexts/situations to influence child dietary intake | Parents tend to select FPP that are easy to use, provide benefit for their child, and/or have worked in the past [37]. | Under what circumstances do parents select to use specific FPP? How consistent are parents in use of joint FPP and what are the implications of consistency/inconsistency for child intake? |
| Parent perception of eating event/context | Parents may vary in their perception of the context of an eating event (e.g., a special or usual event) and the extent to which the event dictates specific FPP. | Little research has addressed parent perception of eating events or FPP appropriate to the perception [37]. | What are the most common categories of parents’ perception of eating events? What do parents perceive as the most appropriate FPP for each category of eating event? |
| Child receptiveness | Some children are receptive to any/all/some FPP, and some are not | Children are not passive recipients of FPP [37,38]. | Are there effective FPP to which children are universally receptive? |
| Child response predisposition | Children may be receptive to a FPP or not, based on appetitive, temperament, taste sensitivities and other characteristics. | A large number of factors (e.g., child social/cultural, neighborhood) influence child dietary intake [39]. | How do children with different response predispositions respond to different FPP in different situations? |
| Developmental characteristics | Influences on FPP and child intake vary by age and age-related characteristics of the child/adolescent. | Child temperament and appetitive and food avoidant characteristics were related to BMI [40]. Some child developmental characteristics, e.g., food neophobia or picky eating were not related to child BMI [41]. | More precise definitions and operationalizations of developmental characteristics are needed. Under what circumstances are child developmental characteristics related to dietary intake and BMI, at what ages? |
| Child perception of eating event/context | Children may vary in their perception of the context of the eating event (e.g., a special or usual event) and the extent to which the event dictates specific behavior | Little research has addressed child perception of eating events or child behaviors appropriate to the perception. | What are the most common categories of child perception of eating events? What do children perceive as the most appropriate behavior for each category of eating event? |
| Child dietary intake | This objective of PFP is to enable children to consume a healthier diet. | While many possible influences on child dietary intake have been proposed, and some supported, there is no consistent findings on the relation of FPP and child dietary intake [42]. | Under what circumstances do FPP influence child dietary intake? |
| What did the parent learn? | As a result of the use of one or more FPP on a particular occasion, the parent will have learned one or more things, and this will serve to confirm or induce change in the parent predisposition to select and employ FPP. | Little research has addressed what parents learn from employing FPP or how it influences their predispositions to use FPP in the future. | How does use of FPP in interaction with their child, peers, or other sources of parenting information influence their predisposition to select, and how to employ FPP in the future? |
| What did the child learn? | As a result of being on the receiving end of one or more FPP, the child could be oblivious, or adapt/modify some aspect of their receptiveness, including defensive behaviors for future attempts. It is likely that different children will respond to the same FPP in different ways. | Little research has addressed what children learn from receiving FPP or how the experience results in changes in their receptiveness. | Under what circumstances, what and how does a child learn from a parent’s use of FPP, and how does this experience of related comments from peers and the media impact their future receptiveness. |
| Social determinants context | All parent and child behaviors and their interactions are performed in cultural and socioeconomic-demographic context. | There are inconsistent findings in regard to how context influences any of the above, perhaps due to complexity [43]. | How, and under what circumstances, do any of the above outcomes, relationships or other vary by cultural and socioeconomic-demographic context? |
3. Habitual Food Parenting Practices
4. Parent Predisposition to Select FPP
5. Selection and Use of Food Parenting Practices
Parent Perception of Eating Event/Context
6. Child Receptiveness
6.1. Child Response Predisposition
6.2. Developmental Characteristics
6.3. Child Perception of Eating Event/Context
7. Parent–Child Interaction
8. Child Dietary Intake
9. What Did the Parent Learn?
10. What Did the Child Learn?
11. Social Determinants
12. Limitations
13. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Ahmad, F.B.; Anderson, R.N. The Leading Causes of Death in the US for 2020. JAMA 2021, 325, 1829–1830. [Google Scholar] [CrossRef]
- Zupo, R.; Sardone, R.; Donghia, R.; Castellana, F.; Lampignano, L.; Bortone, I.; Misciagna, G.; De Pergola, G.; Panza, F.; Lozupone, M.; et al. Traditional Dietary Patterns and Risk of Mortality in a Longitudinal Cohort of the Salus in Apulia Study. Nutrients 2020, 12, 1070. [Google Scholar] [CrossRef]
- Johansson, U.; Lindberg, L.; Öhlund, I.; Hernell, O.; Lönnerdal, B.; Lundén, S.; Sandell, M.; Lind, T. Acceptance of a Nordic, Protein-Reduced Diet for Young Children during Complementary Feeding—A Randomized Controlled Trial. Foods 2021, 10, 275. [Google Scholar] [CrossRef] [PubMed]
- Petty, S.; Salame, C.; Mennella, J.A.; Pepino, M.Y. Relationship between Sucrose Taste Detection Thresholds and Preferences in Children, Adolescents, and Adults. Nutrients 2020, 12, 1918. [Google Scholar] [CrossRef] [PubMed]
- Van Der Veek, S.M.C.; De Graaf, C.; De Vries, J.H.M.; Jager, G.; Vereijken, C.M.J.L.; Weenen, H.; Van Winden, N.; Van Vliet, M.S.; Schultink, J.M.; De Wild, V.W.T.; et al. Baby’s first bites: A randomized controlled trial to assess the effects of vegetable-exposure and sensitive feeding on vegetable acceptance, eating behavior and weight gain in infants and toddlers. BMC Pediatr. 2019, 19, 266. [Google Scholar] [CrossRef] [PubMed]
- Brennan, L.; de Roos, B. Nutrigenomics: Lessons learned and future perspectives. Am. J. Clin. Nutr. 2021, 113, 503–516. [Google Scholar] [CrossRef]
- Mehta, S.; Huey, S.L.; McDonald, D.; Knight, R.; Finkelstein, J.L. Nutritional interventions and the gut microbiome in children. Annu. Rev. Nutr. 2021, 41, 479–510. [Google Scholar] [CrossRef]
- Rodgers, G.P.; Collins, F.S. Precision Nutrition—The Answer to “What to Eat to Stay Healthy”. JAMA 2020, 324, 735–736. [Google Scholar] [CrossRef]
- Grimaldi, K.A.; van Ommen, B.; Ordovas, J.M.; Parnell, L.D.; Mathers, J.C.; Bendik, I.; Brennan, L.; Celis-Morales, C.; Cirillo, E.; Daniel, H.; et al. Proposed guidelines to evaluate scientific validity and evidence for genotype-based dietary advice. Genes Nutr. 2017, 12, 35. [Google Scholar] [CrossRef]
- Al-Awadhi, B.; Fallaize, R.; Franco, R.Z.; Hwang, F.; Lovegrove, J.A. Insights Into the Delivery of Personalized Nutrition: Evidence From Face-To-Face and Web-Based Dietary Interventions. Front. Nutr. 2020, 7, 570531. [Google Scholar] [CrossRef]
- Chevance, G.; Perski, O.; Hekler, E.B. Innovative methods for observing and changing complex health behaviors: Four propositions. Transl. Behav. Med. 2021, 11, 676–685. [Google Scholar] [CrossRef]
- Motevalli, M.; Drenowatz, C.; Tanous, D.R.; Khan, N.A.; Wirnitzer, K. Management of Childhood Obesity—Time to Shift from Generalized to Personalized Intervention Strategies. Nutrients 2021, 13, 1200. [Google Scholar] [CrossRef] [PubMed]
- Wood, A.C.; Blissett, J.M.; Brunstrom, J.M.; Carnell, S.; Faith, M.S.; Fisher, J.O.; Hayman, L.L.; Khalsa, A.S.; Hughes, S.O.; Miller, A.L.; et al. Caregiver Influences on Eating Behaviors in Young Children: A scientific statement from the American Heart Association. J. Am. Heart Assoc. 2020, 9, e014520. [Google Scholar] [CrossRef] [PubMed]
- Birch, L.L.; Doub, A.E. Learning to eat: Birth to age 2 y. Am. J. Clin. Nutr. 2014, 99, 723S–728S. [Google Scholar] [CrossRef] [PubMed]
- Thompson, D.; Callender, C.; Velazquez, D.; Adera, M.; Dave, J.M.; Olvera, N.; Chen, T.-A.; Goldsworthy, N. Perspectives of Black/African American and Hispanic Parents and Children Living in Under-Resourced Communities Regarding Factors That Influence Food Choices and Decisions: A Qualitative Investigation. Children 2021, 8, 236. [Google Scholar] [CrossRef] [PubMed]
- Savage, J.S.; Fisher, J.O.; Birch, L.L. Parental Influence on Eating Behavior: Conception to Adolescence. J. Law Med. Ethics 2007, 35, 22–34. [Google Scholar] [CrossRef]
- Nader, P.R.; Baranowski, T.; Vanderpool, N.A.; Dunn, K.; Dworkin, R.; Ray, L. The Family Health Project: Cardiovascular risk reduction education for children and parents. J. Dev. Behav. Pediatr. 1983, 4, 3–10. [Google Scholar] [CrossRef]
- Perdew, M.; Liu, S.; Naylor, P.-J. Family-based nutrition interventions for obesity prevention among school-aged children: A systematic review. Transl. Behav. Med. 2021, 11, 709–723. [Google Scholar] [CrossRef]
- Hingle, M.D.; O’Connor, T.M.; Dave, J.M.; Baranowski, T. Parental involvement in interventions to improve child dietary intake: A systematic review. Prev. Med. 2010, 51, 103–111. [Google Scholar] [CrossRef]
- Hoelscher, D.M.; Kirk, S.; Ritchie, L.; Cunningham-Sabo, L. Position of the Academy of Nutrition and Dietetics: Interventions for the Prevention and Treatment of Pediatric Overweight and Obesity. J. Acad. Nutr. Diet. 2013, 113, 1375–1394. [Google Scholar] [CrossRef]
- O’Connor, T.M.; Pham, T.; Watts, A.; Tu, A.W.; Hughes, S.O.; Beauchamp, M.R.; Baranowski, T.; Mâsse, L. Development of an item bank for food parenting practices based on published instruments and reports from Canadian and US parents. Appetite 2016, 103, 386–395. [Google Scholar] [CrossRef]
- O’Connor, T.M.; Mâsse, L.C.; Tu, A.W.; Watts, A.W.; Hughes, S.O.; Beauchamp, M.R.; Baranowski, T.; Pham, T.; Berge, J.M.; Fiese, B.; et al. Food parenting practices for 5 to 12 year old children: A concept map analysis of parenting and nutrition experts input. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 122. [Google Scholar] [CrossRef] [PubMed]
- Mâsse, L.C.; O’Connor, T.M.; Lin, Y.; Hughes, S.O.; Tugault-Lafleur, C.N.; Baranowski, T.; Beauchamp, M.R. Calibration of the food parenting practice (FPP) item bank: Tools for improving the measurement of food parenting practices of parents of 5–12-year-old children. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 140. [Google Scholar] [CrossRef] [PubMed]
- Olstad, D.L.; McIntyre, L. Reconceptualising precision public health. BMJ Open 2019, 9, e030279. [Google Scholar] [CrossRef] [PubMed]
- Darling, N.; Steinberg, L. Parenting style as context: An intergrative model. Psychol. Bull. 1993, 113, 487–496. [Google Scholar] [CrossRef]
- Hoerr, S.L.; Hughes, S.O.; Fisher, J.O.; Nicklas, T.A.; Liu, Y.; Shewchuk, R.M. Associations among parental feeding styles and children’s food intake in families with limited incomes. Int. J. Behav. Nutr. Phys. Act. 2009, 6, 55. [Google Scholar] [CrossRef]
- Hughes, S.O.; Power, T.G.; O’Connor, T.M.; Fisher, J.O.; Micheli, N.E.; Papaioannou, M.A. Maternal feeding style and child weight status among Hispanic families with low-income levels: A longitudinal study of the direction of effects. Int. J. Behav. Nutr. Phys. Act. 2021, 18, 30. [Google Scholar] [CrossRef]
- Hughes, S.O.; Power, T.G. Feeding styles and child eating behaviors: A multi-method approach. In Families, Food and Parenting: Integrating Research, Practice and Policy; Francis, L.A., McHale, S.M., King, V., Glick, J.E., Eds.; Springer: Cham, Switzerland, 2021; pp. 95–114. [Google Scholar]
- Wood, A.C.; Senn, M.; Beltran, A.; Pfaff, R.; Hughes, S.O.; Thompson, D.; O’Connor, T.M.; Baranowski, T. Vegetable parenting practices vary by feeding styles among middle class mothers of young children. Appetite 2021. under review. [Google Scholar]
- Olvera, N.; Power, T.G. Parenting Styles and Obesity in Mexican American Children: A Longitudinal Study. J. Pediatr. Psychol. 2010, 35, 243–249. [Google Scholar] [CrossRef]
- Larsen, J.K.; Hermans, R.C.; Sleddens, E.F.; Engels, R.C.; Fisher, J.O.; Kremers, S.P. How parental dietary behavior and food parenting practices affect children’s dietary behavior. Interacting sources of influence? Appetite 2015, 89, 246–257. [Google Scholar] [CrossRef]
- Mâsse, L.C.; Tu, A.W.; Watts, A.; Hughes, S.O.; O’Connor, T.M. What parenting practices do US and Canadian parents use to encourage or discourage healthy eating among their 5–12 year-old children? Prev. Med. Rep. 2020, 20, 101234. [Google Scholar] [CrossRef]
- Baranowski, T.; Chen, T.-A.; O’Connor, T.; Hughes, S.; Beltran, A.; Frankel, L.; Diep, C.; Baranowski, J.C. Dimensions of vegetable parenting practices among preschoolers. Appetite 2013, 69, 89–93. [Google Scholar] [CrossRef]
- Baranowski, T.; Chen, T.-A.; O’Connor, T.M.; Hughes, S.O.; Diep, C.S.; Beltran, A.; Brand, L.; Nicklas, T.; Baranowski, J. Predicting habits of vegetable parenting practices to facilitate the design of change programmes. Public Health Nutr. 2016, 19, 1976–1982. [Google Scholar] [CrossRef][Green Version]
- Baranowski, T.; Beltran, A.; Chen, T.-A.; Thompson, D.; O’Connor, T.; Hughes, S.; Diep, C.; Baranowski, J.C. Predicting use of ineffective vegetable parenting practices with the Model of Goal Directed Behavior. Public Health Nutr. 2015, 18, 1028–1035. [Google Scholar] [CrossRef]
- Diep, C.S.; Beltran, A.; Chen, T.-A.; Thompson, D.; O’Connor, T.; Hughes, S.; Baranowski, J.; Baranowski, T. Predicting use of effective vegetable parenting practices with the Model of Goal Directed Behavior. Public Health Nutr. 2015, 18, 1389–1396. [Google Scholar] [CrossRef]
- Beltran, A.; Demet, R.; Hughes, S.O.; Wood, A.C.; Thompson, D.; O’Connor, T.M.; Baranowski, T. Selection and use of vegetable parenting practices did not vary by parent feeding styles: Mixed methods investigation. Appetite 2021. under review. [Google Scholar]
- Soto, S.; Arredondo, E.M.; Ayala, G.X.; Marcus, B.H.; Shakya, H.B. Exploring how bicultural and assimilated children of Mexican origin influence their Latina mothers’ diet: Perspectives from mothers and children. Appetite 2018, 129, 217–227. [Google Scholar] [CrossRef] [PubMed]
- Miller, A.L.; Miller, S.E.; Clark, K. Child, Caregiver, Family, and Social-Contextual Factors to Consider when Implementing Parent-Focused Child Feeding Interventions. Curr. Nutr. Rep. 2018, 7, 303–309. [Google Scholar] [CrossRef] [PubMed]
- Bergmeier, H.; Skouteris, H.; Horwood, S.; Hooley, M.; Richardson, B. Associations between child temperament, maternal feeding practices and child body mass index during the preschool years: A systematic review of the literature. Obes. Rev. 2014, 15, 9–18. [Google Scholar] [CrossRef] [PubMed]
- Brown, C.L.; Schaaf, E.B.V.; Cohen, G.M.; Irby, M.B.; Skelton, J.A. Association of Picky Eating and Food Neophobia with Weight: A Systematic Review. Child. Obes. 2016, 12, 247–262. [Google Scholar] [CrossRef]
- Shloim, N.; Edelson, L.R.; Martin, N.; Hetherington, M.M. Parenting Styles, Feeding Styles, Feeding Practices, and Weight Status in 4–12 Year-Old Children: A Systematic Review of the Literature. Front. Psychol. 2015, 6, 1849. [Google Scholar] [CrossRef] [PubMed]
- Sawyer, A.D.M.; van Lenthe, F.; Kamphuis, C.B.M.; Terragni, L.; Roos, G.; Poelman, M.P.; Nicolaou, M.; Waterlander, W.; Djojosoeparto, S.K.; Scheidmeir, M.; et al. Dynamics of the complex food environment underlying dietary intake in low-income groups: A systems map of associations extracted from a systematic umbrella literature review. Int. J. Behav. Nutr. Phys. Act. 2021, 18, 96. [Google Scholar] [CrossRef] [PubMed]
- Cullen, K.W.; Baranowski, T.; Rittenberry, L.; Cosart, C.; Hebert, D.; De Moor, C. Child-reported family and peer influences on fruit, juice and vegetable consumption: Reliability and validity of measures. Health Educ. Res. 2001, 16, 187–200. [Google Scholar] [CrossRef] [PubMed]
- Baumrind, D. Current patterns of parental authority. Dev. Psychol. 1971, 4 Pt 2, 1–103. [Google Scholar] [CrossRef]
- Maccoby, E.; Martin, J. Socialization in the context of the family: Parent-child interaction. In Handbook of Child Psychology: Socialization, Personality and Social Development; Hetherington, E.M., Ed.; Wiley: New York, NY, USA, 1983; pp. 1–101. [Google Scholar]
- Kwasnicka, D.; Dombrowski, S.U.; White, M.; Sniehotta, F. Theoretical explanations for maintenance of behaviour change: A systematic review of behaviour theories. Health Psychol. Rev. 2016, 10, 277–296. [Google Scholar] [CrossRef]
- Gardner, B.; Richards, R.; Lally, P.; Rebar, A.; Thwaite, T.; Beeken, R.J. Breaking habits or breaking habitual behaviours? Old habits as a neglected factor in weight loss maintenance. Appetite 2021, 162, 105183. [Google Scholar] [CrossRef]
- Gardner, B.; Rebar, A.L.; Lally, P. A matter of habit: Recognizing the multiple roles of habit in health behaviour. Br. J. Health Psychol. 2019, 24, 241–249. [Google Scholar] [CrossRef]
- Baranowski, T.; Beltran, A.; Chen, T.-A.; Thompson, D.; Connor, T.O.; Hughes, S.; Diep, C.; Baranowski, J. Psychometric assessment of scales for a Model of Goal Directed Vegetable Parenting Practices (MGDVPP). Int. J. Behav. Nutr. Phys. Act. 2013, 10, 110. [Google Scholar] [CrossRef]
- Hingle, M.; Beltran, A.; O’Connor, T.; Thompson, D.; Baranowski, J.; Baranowski, T. A model of goal directed vegetable parenting practices. Appetite 2012, 58, 444–449. [Google Scholar] [CrossRef]
- Chen, T.-A.; O’Connor, T.M.; Hughes, S.O.; Beltran, A.; Baranowski, J.; Diep, C.; Baranowski, T. Vegetable parenting practices scale. Item response modeling analyses. Appetite 2015, 91, 190–199. [Google Scholar] [CrossRef]
- Peters, J.; Parletta, N.; Lynch, J.; Campbell, K. A comparison of parental views of their pre-school children’s ‘healthy’ versus ‘unhealthy’ diets. A qualitative study. Appetite 2014, 76, 129–136. [Google Scholar] [CrossRef]
- Pamungkas, R.A.; Chamroonsawasdi, K. Home-Based Interventions to Treat and Prevent Childhood Obesity: A Systematic Review and Meta-Analysis. Behav. Sci. 2019, 9, 38. [Google Scholar] [CrossRef] [PubMed]
- Carnell, S.; Cooke, L.; Cheng, R.; Robbins, A.; Wardle, J. Parental feeding behaviours and motivations. A qualitative study in mothers of UK pre-schoolers. Appetite 2011, 57, 665–673. [Google Scholar] [CrossRef] [PubMed]
- Balantekin, K.N.; Anzman-Frasca, S.; Francis, L.A.; Ventura, A.K.; Fisher, J.O.; Johnson, S.L. Positive parenting approaches and their association with child eating and weight: A narrative review from infancy to adolescence. Pediatr. Obes. 2020, 15, e12722. [Google Scholar] [CrossRef] [PubMed]
- Bergmeier, H.; Paxton, S.J.; Milgrom, J.; Anderson, S.E.; Baur, L.; Hill, B.; Lim, S.; Green, R.; Skouteris, H. Early mother-child dyadic pathways to childhood obesity risk: A conceptual model. Appetite 2020, 144, 104459. [Google Scholar] [CrossRef] [PubMed]
- Mennella, J.A.; Bobowski, N.K. The sweetness and bitterness of childhood: Insights from basic research on taste preferences. Physiol. Behav. 2015, 152 Pt B, 502–507. [Google Scholar] [CrossRef]
- Esposito, L.; Fisher, J.O.; Mennella, J.A.; Hoelscher, D.M.; Huang, T.T. Developmental Perspectives on Nutrition and Obesity from Gestation to Adolescence. Prev. Chronic Dis. 2009, 6, A94. [Google Scholar]
- Kininmonth, A.; Smith, A.; Carnell, S.; Steinsbekk, S.; Fildes, A.; Llewellyn, C. The association between childhood adiposity and appetite assessed using the Child Eating Behavior Questionnaire and Baby Eating Behavior Questionnaire: A systematic review and meta-analysis. Obes. Rev. 2021, 22, e13169. [Google Scholar] [CrossRef]
- Russell, A.; Russell, C.G. Appetite self-regulation declines across childhood while general self-regulation improves: A narrative review of the origins and development of appetite self-regulation. Appetite 2021, 162, 105178. [Google Scholar] [CrossRef]
- Russell, C.G.; Russell, A. A biopsychosocial approach to processes and pathways in the development of overweight and obesity in childhood: Insights from developmental theory and research. Obes. Rev. 2019, 20, 725–749. [Google Scholar] [CrossRef]
- Button, A.; Faith, M.S.; Berkowitz, R.I. Temperament and eating self-regulation in young children with or at risk for obesity: An exploratory report. Pediatr. Obes. 2021. [Google Scholar] [CrossRef] [PubMed]
- Gibson, E.L.; Kreichauf, S.; Wildgruber, A.; Vögele, C.; Summerbell, C.D.; Nixon, C.; Moore, H.; Douthwaite, W.; Manios, Y. ToyBox-study group A narrative review of psychological and educational strategies applied to young children’s eating behaviours aimed at reducing obesity risk. Obes. Rev. 2012, 13 (Suppl. 1), 85–95. [Google Scholar] [CrossRef]
- Tugault-Lafleur, C.N.; González, O.D.; O’Connor, T.M.; Hughes, S.O.; Mâsse, L.C. Identifying and predicting food parenting practice profiles among Canadian parents. Int. J. Behav. Nutr. Phys. Act. 2021, 18, 59. [Google Scholar] [CrossRef]
- Towner, E.K.; Reiter-Purtill, J.; Boles, R.E.; Zeller, M.H. Predictors of caregiver feeding practices differentiating persistently obese from persistently non-overweight adolescents. Appetite 2015, 84, 120–127. [Google Scholar] [CrossRef][Green Version]
- Resnicow, K.; Davis-Hearn, M.; Smith, M.; Baranowski, T.; Lin, L.S.; Baranowski, J.; Doyle, C.; Wang, D.T. Social-cognitive predictors of fruit and vegetable intake in children. Health Psychol. 1997, 16, 272–276. [Google Scholar] [CrossRef]
- Casey, R.; Rozin, P. Changing children’s food preferences: Parent opinions. Appetite 1989, 12, 171–182. [Google Scholar] [CrossRef]
- Birch, L.L.; Zimmerman, S.I.; Hind, H. The Influence of Social-Affective Context on the Formation of Children’s Food Preferences. Child Dev. 1980, 51, 856–861. [Google Scholar] [CrossRef]
- Bradshaw, C.P.; Goldweber, A.; Fishbein, D.; Greenberg, M.T. Infusing Developmental Neuroscience Into School-based Preventive Interventions: Implications and Future Directions. J. Adolesc. Health 2012, 51 (Suppl. 2), S41–S47. [Google Scholar] [CrossRef]
- Diep, C.S.; Hingle, M.; Chen, T.-A.; Dadabhoy, H.R.; Beltran, A.; Baranowski, J.; Subar, A.F.; Baranowski, T. The Automated Self-Administered 24-Hour Dietary Recall for Children, 2012 Version, for Youth Aged 9 to 11 Years: A Validation Study. J. Acad. Nutr. Diet. 2015, 115, 1591–1598. [Google Scholar] [CrossRef]
- Baranowski, T.; Islam, N.; Baranowski, J.; Martin, S.; Beltran, A.; Dadabhoy, H.; Adame, S.-H.; Watson, K.B.; Thompson, D.; Cullen, K.W.; et al. Comparison of a Web-Based versus Traditional Diet Recall among Children. J. Acad. Nutr. Diet. 2012, 112, 527–532. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.-B.; Chen, C.; Pan, X.-F.; Guo, J.; Li, Y.; Franco, O.H.; Liu, G.; Pan, A. Associations of healthy lifestyle and socioeconomic status with mortality and incident cardiovascular disease: Two prospective cohort studies. BMJ 2021, 373, n604. [Google Scholar] [CrossRef] [PubMed]
- Pinket, A.-S.; De Craemer, M.; De Bourdeaudhuij, I.; Deforche, B.; Cardon, G.; Androutsos, O.; Koletzko, B.; Moreno, L.A.; Socha, P.; Iotova, V.; et al. Can Parenting Practices Explain the Differences in Beverage Intake According to Socio-Economic Status: The Toybox-Study. Nutrients 2016, 8, 591. [Google Scholar] [CrossRef] [PubMed]
- Feinberg, E.; Kavanagh, P.L.; Young, R.L.; Prudent, N. Food Insecurity and Compensatory Feeding Practices Among Urban Black Families. Pediatrics 2008, 122, e854–e860. [Google Scholar] [CrossRef] [PubMed]
- Jago, R.; Baranowski, T.; Baranowski, J.C. Fruit and vegetable availability: A micro environmental mediating variable? Public Health Nutr. 2007, 10, 681–689. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baranowski, T.; Thompson, D.; Hughes, S.O.; O’Connor, T.M. Precision Food Parenting: A Proposed Conceptual Model and Research Agenda. Nutrients 2021, 13, 3650. https://doi.org/10.3390/nu13103650
Baranowski T, Thompson D, Hughes SO, O’Connor TM. Precision Food Parenting: A Proposed Conceptual Model and Research Agenda. Nutrients. 2021; 13(10):3650. https://doi.org/10.3390/nu13103650
Chicago/Turabian StyleBaranowski, Tom, Debbe Thompson, Sheryl O. Hughes, and Teresia M. O’Connor. 2021. "Precision Food Parenting: A Proposed Conceptual Model and Research Agenda" Nutrients 13, no. 10: 3650. https://doi.org/10.3390/nu13103650
APA StyleBaranowski, T., Thompson, D., Hughes, S. O., & O’Connor, T. M. (2021). Precision Food Parenting: A Proposed Conceptual Model and Research Agenda. Nutrients, 13(10), 3650. https://doi.org/10.3390/nu13103650








