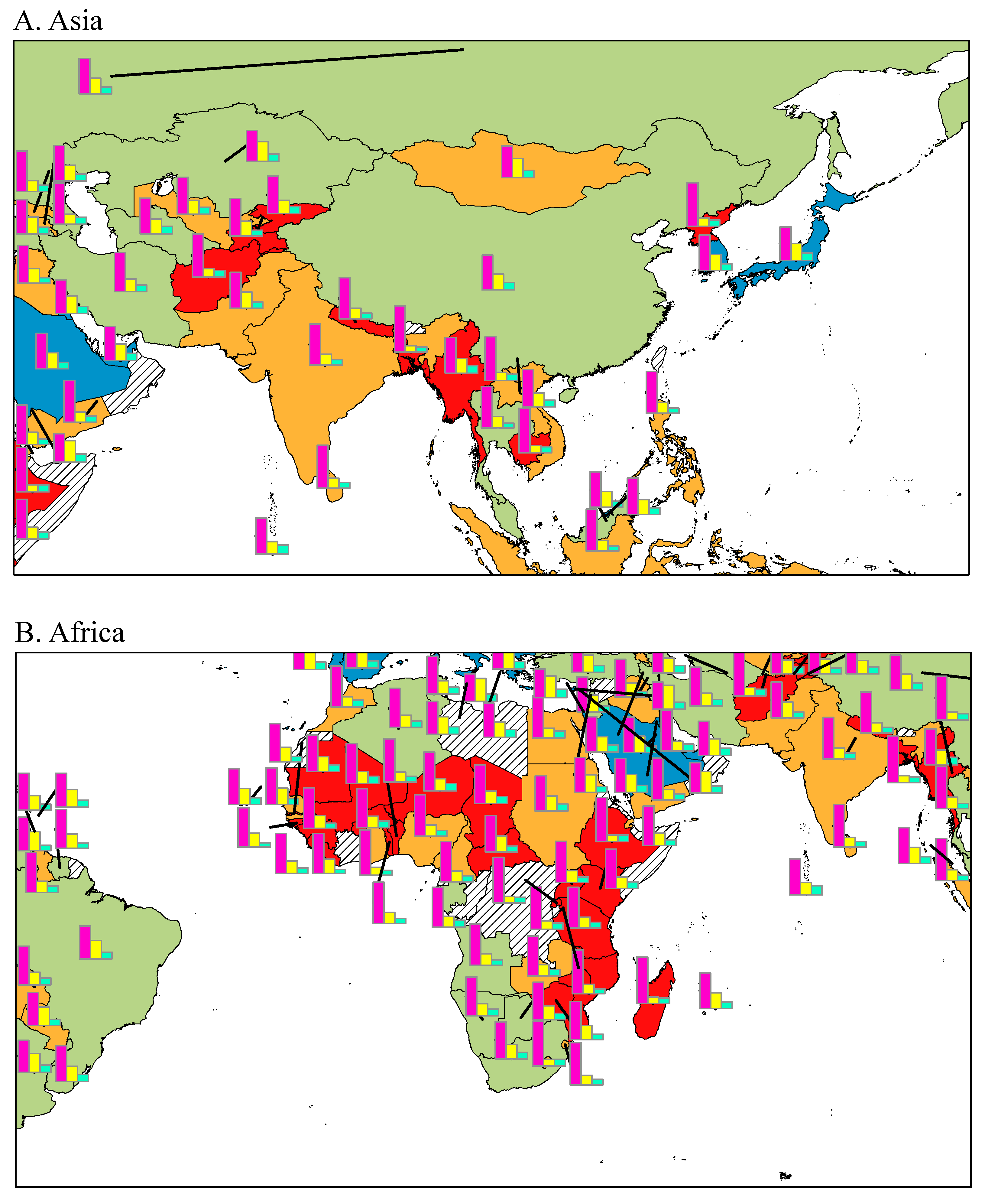
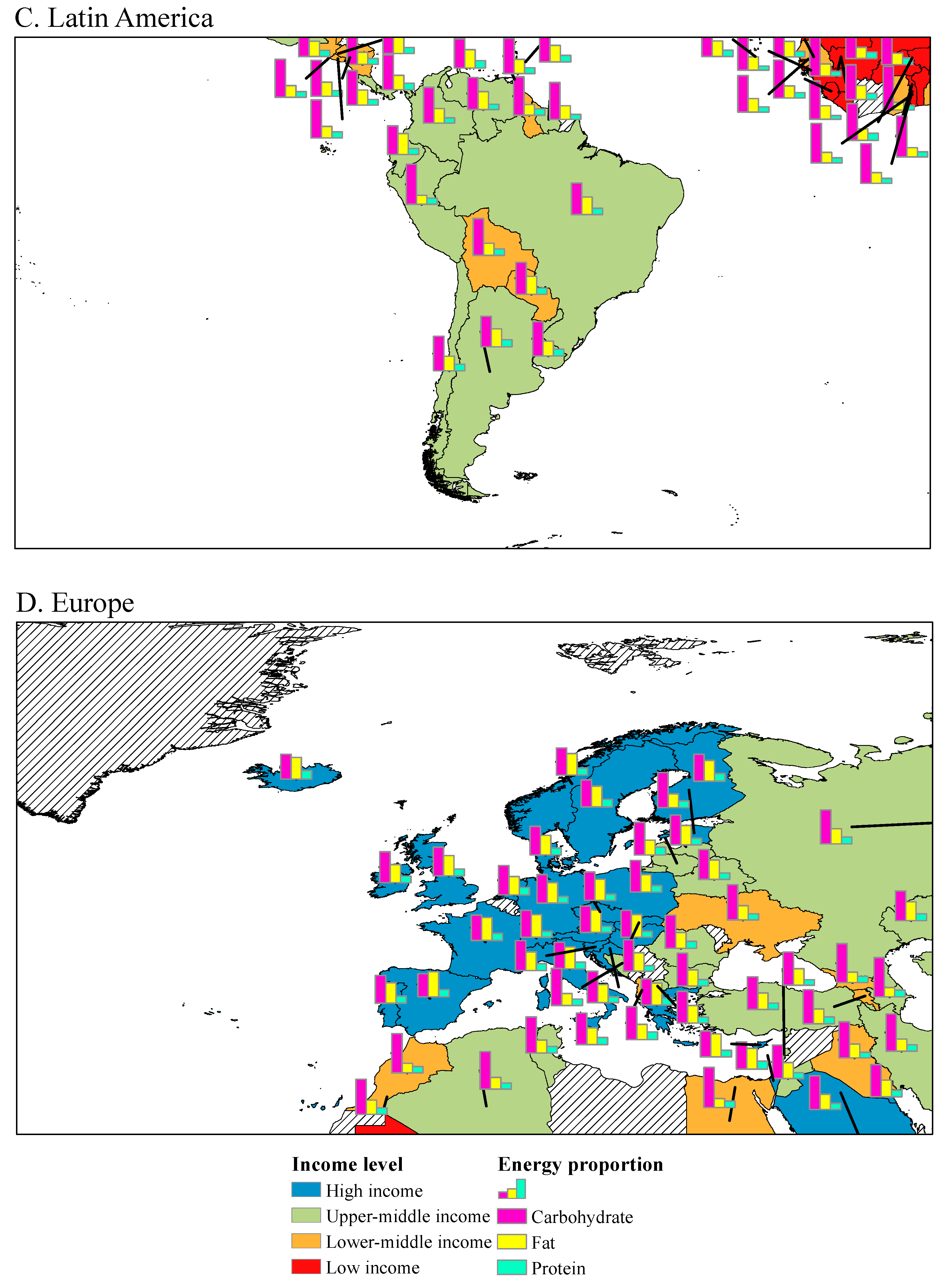
Global and Regional Patterns in Noncommunicable Diseases and Dietary Factors across National Income Levels
Abstract
:1. Introduction
2. Subjects and Methods
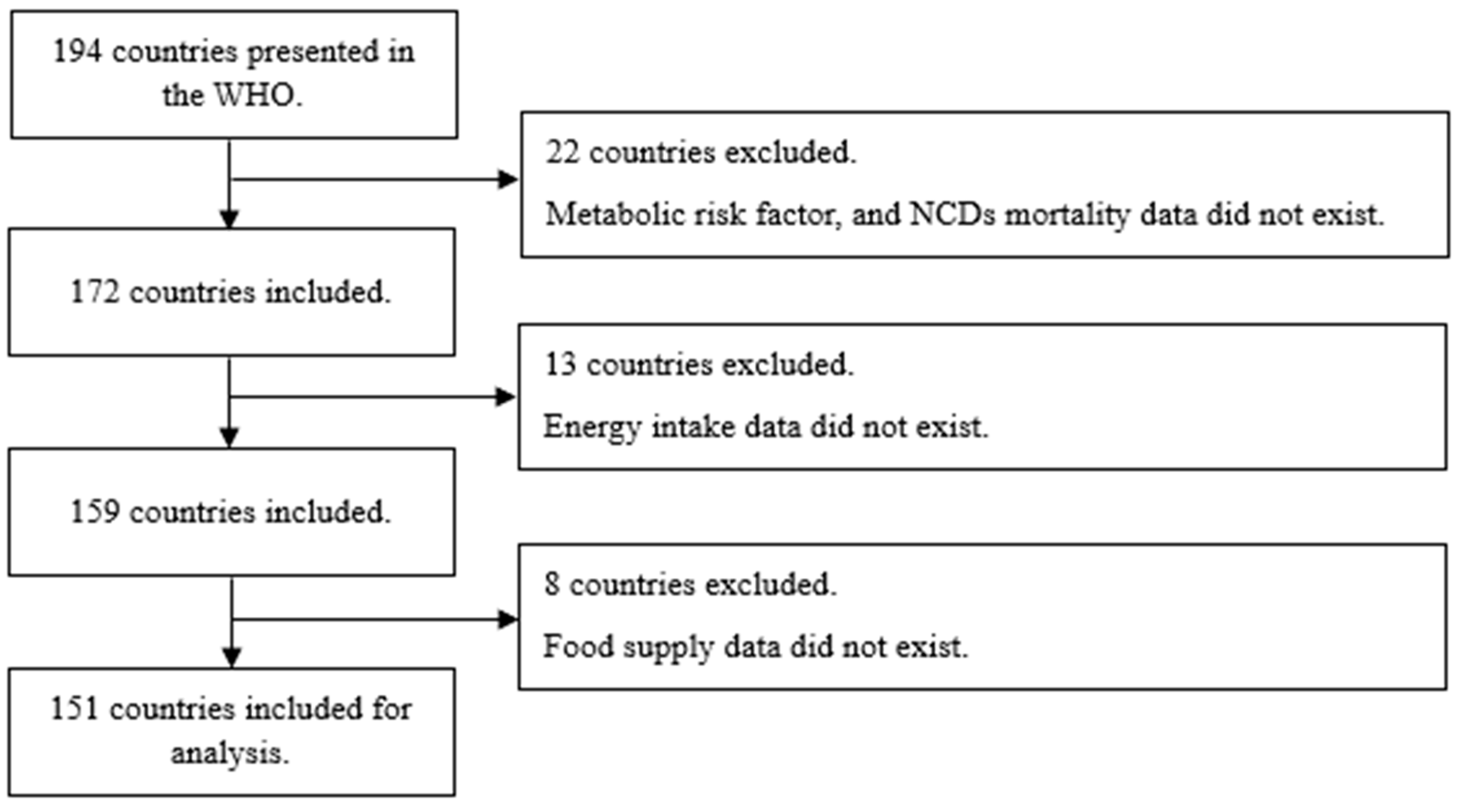
2.1. Study Population
2.2. Classifications
2.3. Data Collection
2.3.1. NCDs Mortality, Metabolic Risk Factors, and Health-Related Factors
2.3.2. Food Supply
2.4. Statistical Analyses
3. Results
4. Discussion
Author Contributions
Funding
Conflicts of Interest
References
- Renzella, J.; Townsend, N.; Jewell, J.; Breda, J.; Roberts, N.; Rayner, M.; Wickramasinghe, K. What National and Subnational Interventions and Policies Based on Mediterranean and Nordic Diets Are Recommended or Implemented in the WHO European Region, and Is There Evidence of Effectiveness in Reducing Noncommunicable Diseases? World Health Organization; WHO Regional Office for Europe: Copenhagen, Denmark, 2018. [Google Scholar]
- Sustainabledevelopment.un.org. The Future Is Now-Science for Achieving Sustainable Development. 2019. Available online: https://sustainabledevelopment.un.org/gsdr2019 (accessed on 11 October 2021).
- World Health Organization. Noncommunicable Diseases Country Profiles. 2018. Available online: https://apps.who.int/iris/handle/10665/274512 (accessed on 11 October 2021).
- World Health Organization. Global Status Report on Noncommunicable Diseases. 2014. Available online: https://apps.who.int/iris/handle/10665/148114 (accessed on 11 October 2021).
- World Health Organization Scaling up Action against NCDs: How Much Will It Cost; World Health Organization: Geneva, Switzerland, 2011.
- Clark, H. NCDs: A challenge to sustainable human development. Lancet 2013, 381, 510–511. [Google Scholar] [CrossRef]
- Roth, G.A.; Huffman, M.D.; Moran, A.E.; Feigin, V.; Mensah, G.A.; Naghavi, M.; Murray, C.J. Global and regional patterns in cardiovascular mortality from 1990 to 2013. Circulation 2015, 132, 1667–1678. [Google Scholar] [CrossRef] [Green Version]
- Wu, F.; Guo, Y.; Chatterji, S.; Zheng, Y.; Naidoo, N.; Jiang, Y.; Biritwum, R.; Yawson, A.; Minicuci, N.; Salinas-Rodriguez, A.; et al. Common risk factors for chronic non-communicable diseases among older adults in China, Ghana, Mexico, India, Russia and South Africa: The study on global AGEing and adult health (SAGE) wave 1. BMC Public Health 2015, 15, 88. [Google Scholar] [CrossRef] [Green Version]
- Brown, G. Mapping spatial attributes in survey research for natural resource management: Methods and applications. Soc. Nat. Resour. 2004, 18, 17–39. [Google Scholar] [CrossRef]
- World Health Organization. Available online: https://www.who.int/data/gho/indicator-metadata-registry/imr-details/523 (accessed on 11 October 2021).
- World Bank. Available online: https://data.worldbank.org/ (accessed on 11 October 2021).
- World Health Organization, Global Health Statistics. 2014. Available online: http://apps.who.int/gho/data/ (accessed on 11 October 2021).
- Singh, G.M.; Micha, R.; Khatibzadeh, S.; Shi, P.; Lim, S.; Andrews, K.G.; Engell, R.E.; Ezzati, M.; Mozaffarian, D. Global Burden of Diseases Nutrition and Chronic Diseases Expert Group (NutriCoDE) Global, regional, and national consumption of sugar-sweetened beverages, fruit juices, and milk: A systematic assessment of beverage intake in 187 countries. PLoS ONE 2015, 10, e0124845. [Google Scholar] [CrossRef] [Green Version]
- Wang, X.; Ouyang, Y.; Liu, J.; Zhu, M.; Zhao, G.; Bao, W.; Hu, F.B. Fruit and vegetable consumption and mortality from all causes, cardiovascular disease, and cancer: Systematic review and dose-response meta-analysis of prospective cohort studies. BMJ 2014, 349, g4490. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Micha, R.; Khatibzadeh, S.; Shi, P.; Fahimi, S.; Lim, S.; Andrews, K.G.; Engell, R.E.; Powles, J.; Ezzati, M.; Mozaffarian, D. Global, regional, and national consumption levels of dietary fats and oils in 1990 and 2010: A systematic analysis including 266 country-specific nutrition surveys. BMJ 2014, 348, g2272. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stevens, G.A.; Singh, G.M.; Lu, Y.; Danaei, G.; Lin, J.K.; Finucane, M.M.; Bahalim, A.N.; McIntire, R.K.; Gutierrez, H.R.; Cowan, M.; et al. National, regional, and global trends in adult overweight and obesity prevalences. Popul. Health Metr. 2012, 10, 22. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- The WHO Recommendations for the Diagnostic Criteria. 2017. Available online: http://apps.who.int/gho/data/ (accessed on 11 October 2021).
- Food and Agriculture Organization of the United Nations. Available online: http://www.fao.org/home/en/ (accessed on 11 October 2021).
- World Health Organization The Global Burden of Disease: 2004 Update. 2008. Available online: https://apps.who.int/iris/handle/10665/43942 (accessed on 11 October 2021).
- Danaei, G.; Finucane, M.M.; Lin, J.K.; Singh, G.M.; Paciorek, C.J.; Cowan, M.J.; Farzadfar, F.; Stevens, G.A.; Lim, S.S.; Riley, L.M.; et al. National, regional, and global trends in systolic blood pressure since 1980: Systematic analysis of health examination surveys and epidemiological studies with 786 country-years and 5· 4 million participants. Lancet 2011, 377, 568–577. [Google Scholar] [CrossRef]
- Min, J.; Zhao, Y.; Slivka, L.; Wang, Y. Double burden of diseases worldwide: Coexistence of undernutrition and overnutrition-related non-communicable chronic diseases. Obes. Rev. 2018, 19, 49–61. [Google Scholar] [CrossRef]
- Danaei, G.; Lu, Y.; Singh, G.M.; Carnahan, E.; Stevens, G.A.; Cowan, M.J.; Farzadfar, F.; Lin, J.K.; Finucane, M.M.; Rao, M.; et al. Cardiovascular disease, chronic kidney disease, and diabetes mortality burden of cardiometabolic risk factors from 1980 to 2010: A comparative risk assessment. Lancet Diabetes Endocrinol. 2014, 2, 634–647. [Google Scholar]
- Niessen, L.W.; Mohan, D.; Akuoku, J.K.; Mirelman, A.J.; Ahmed, S.; Koehlmoos, T.P.; Trujillo, A.; Khan, J.; Peters, D.H. Tackling socioeconomic inequalities and non-communicable diseases in low-income and middle-income countries under the Sustainable Development agenda. Lancet 2018, 391, 2036–2046. [Google Scholar] [CrossRef] [Green Version]
- Stringhini, S.; Bovet, P. Socioeconomic status and risk factors for non-communicable diseases in low-income and lower-middle-income countries. Lancet Glob. Health 2017, 5, e230–e231. [Google Scholar] [CrossRef] [Green Version]
- Hyseni, L.; Atkinson, M.; Bromley, H.; Orton, L.; Lloyd-Williams, F.; McGill, R.; Capewell, S. The effects of policy actions to improve population dietary patterns and prevent diet-related non-communicable diseases: Scoping review. Eur. J. Clin. Nutr. 2017, 71, 694–711. [Google Scholar] [CrossRef] [Green Version]
- Hayashi, F.; Takemi, Y. Why Is Creating a Healthy Food Environment So Crucial to Making Improvements in Diet-Related NCDs? J. Nutr. Sci. Vitaminol. 2015, 61, S36–S38. [Google Scholar] [CrossRef] [Green Version]
- Ronto, R.; Wu, J.H.; Singh, G.M. The global nutrition transition: Trends, disease burdens and policy interventions. Public Health Nutr. 2018, 21, 2267–2270. [Google Scholar] [CrossRef] [Green Version]
- Afshin, A.; Sur, P.J.; Fay, K.A.; Cornaby, L.; Ferrara, G.; Salama, J.S.; Mullany, E.C.; Abate, K.H.; Abbafati, C.; Abebe, Z.; et al. Health effects of dietary risks in 195 countries, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019, 393, 1958–1972. [Google Scholar] [CrossRef] [Green Version]
- Hall, J.N.; Moore, S.; Harper, S.B.; Lynch, J.W. Global variability in fruit and vegetable consumption. Am. J. Prev. Med. 2009, 36, 402–409.e5. [Google Scholar] [CrossRef]
- Fonseca-Junior, S.J.; Sá, C.G.; Rodrigues, P.A.; Fernandes-Filho, A.J. Physical exercise and morbid obesity: A systematic review. Arq. Bras. Cir. Dig. 2013, 26, 67–73. [Google Scholar] [CrossRef] [Green Version]
- Moodie, R.; Stuckler, D.; Monteiro, C.; Sheron, N.; Neal, B.; Thamarangsi, T.; Lincoln, P.; Casswell, S. Lancet NCD Action Group. Profits and pandemics: Prevention of harmful effects of tobacco, alcohol, and ultra-processed food and drink industries. Lancet 2013, 381, 670–679. [Google Scholar] [CrossRef]
- World Health Organization. Noncommunicable Diseases Global Monitoring Framework: Indicator Definitions and Specifications. 2014. Available online: https://www.who.int/publications/i/item/ncd-gmf-indicator-definitions-and-specifications (accessed on 11 October 2021).
- Benziger, C.P.; Roth, G.A.; Moran, A.E. The global burden of disease study and the preventable burden of NCD. Glob. Heart 2016, 11, 393–397. [Google Scholar] [CrossRef] [PubMed]
- Estimé, M.S.; Lutz, B.; Strobel, F. Trade as a structural driver of dietary risk factors for noncommunicable diseases in the Pacific: An analysis of household income and expenditure survey data. Glob. Health 2014, 10, 48. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Finucane, M.M.; Stevens, G.A.; Cowan, M.J.; Danaei, G.; Lin, J.K.; Paciorek, C.J.; Singh, G.M.; Gutierrez, H.R.; Lu, Y.; Bahalim, A.N.; et al. National, regional, and global trends in body-mass index since 1980: Systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9· 1 million participants. Lancet 2011, 377, 557–567. [Google Scholar] [CrossRef] [Green Version]
- Habib, A.; Alam, M.M.; Hussain, I.; Nasir, N.; Almuthebi, M. Erratic Behavioral Attitude Leads to Noncommunicable Diseases: A Cross-Sectional Study. Biomed Res. Int. 2020, 2020, 7257052. [Google Scholar]
- Popkin, B.M. The nutrition transition: An overview of world patterns of change. Nutr. Rev. 2004, 62, S140–S143. [Google Scholar] [CrossRef]

| Income Levels (n = 151) | ||||||
|---|---|---|---|---|---|---|
| High Income (n = 39) | Upper-Middle Income (n = 43) | Lower-Middle Income (n = 38) | Low Income (n = 31) | p for Trend 2 | ||
| Prevalence | ||||||
| Raised fasting blood glucose 3 | % | 8.2 ± 2.2 | 10.0 ± 1.7 | 9.5 ± 2.1 | 7.7 ± 1.1 | <0.001 |
| Raised total cholesterol 4 | % | 16.3 ± 3.7 | 9.1 ± 2.8 | 6.0 ± 1.8 | 4.1 ± 0.7 | <0.001 |
| Overweight 5 | % | 57.6 ± 12.8 | 43.2 ± 12.2 | 26.7 ± 10.4 | 22.1 ± 4.3 | <0.001 |
| Obesity 6 | % | 24.1 ± 9.2 | 13.3 ± 8.5 | 7.3 ± 5.5 | 5.3 ± 2.1 | <0.001 |
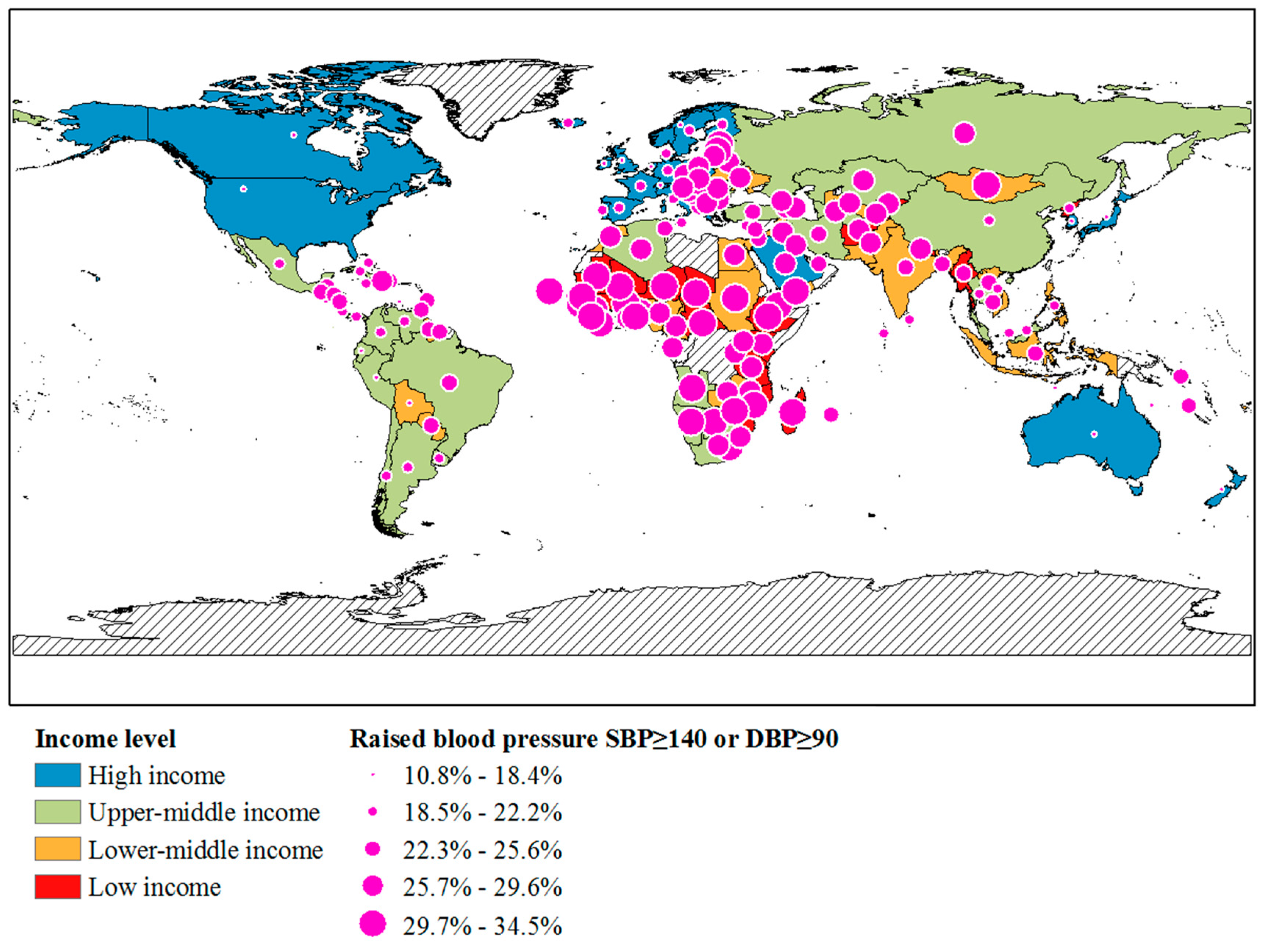
| Raised blood pressure 7 | % | 18.9 ± 5.4 | 20.8 ± 3.2 | 25.6 ± 2.1 | 29.7 ± 2.9 | <0.001 |
| Deaths8 | ||||||
| Risk of premature death from target NCDs 9 | % | 14.6 ± 6.1 | 18.9 ± 3.1 | 23.6 ± 3.5 | 20.3 ± 4.5 | <0.001 |
| NCDs deaths under age 70 10 | % (Male) | 36.6 ± 9.7 | 44.3 ± 6.8 | 60.4 ± 7.3 | 65.6 ± 6.3 | <0.001 |
| NCDs deaths under age 70 | % (Female) | 22.0 ± 8.1 | 35.7 ± 6.6 | 51.6 ± 9.8 | 60 ± 8.2 | <0.001 |
| Deaths (per 100,000) | ||||||
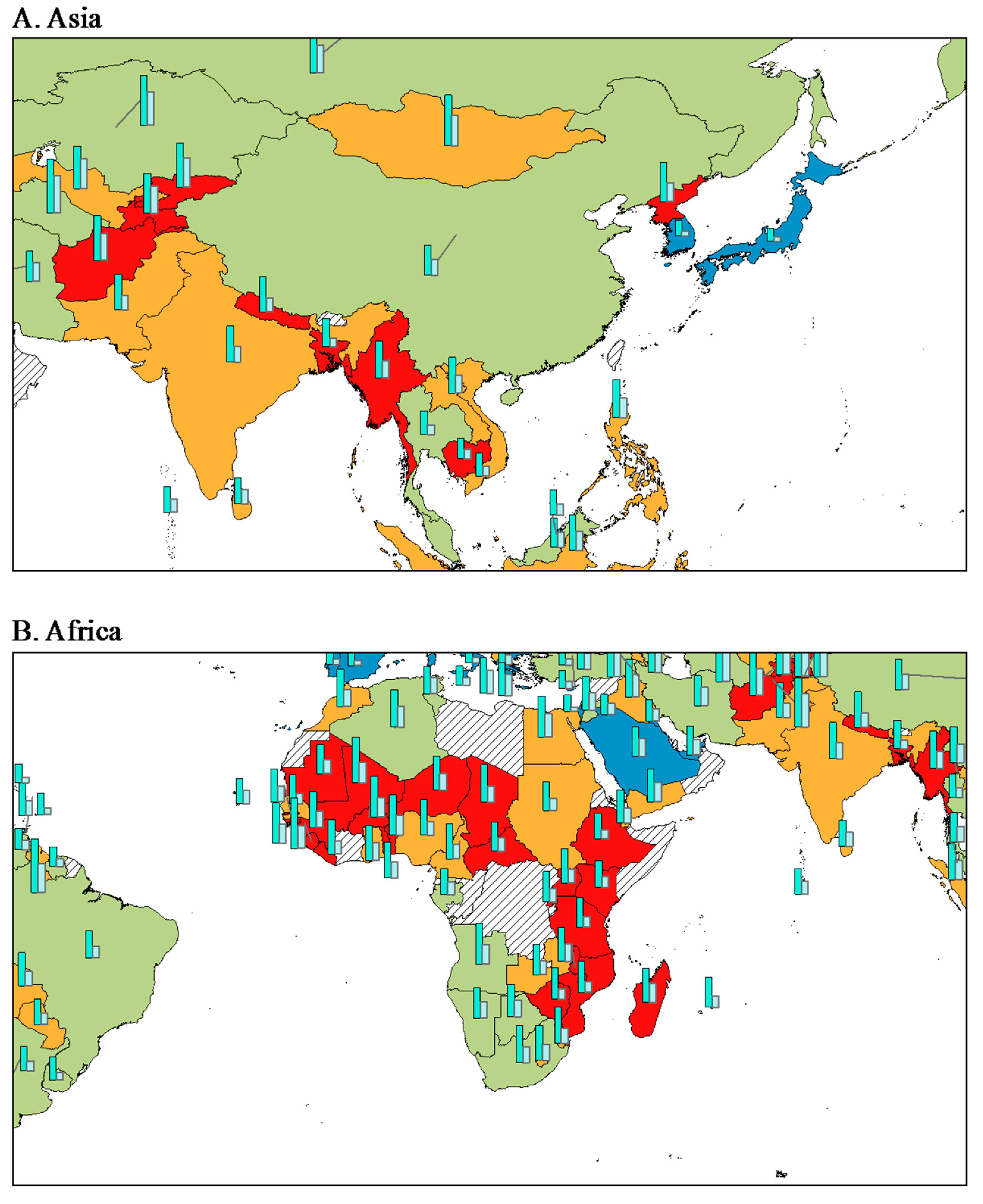
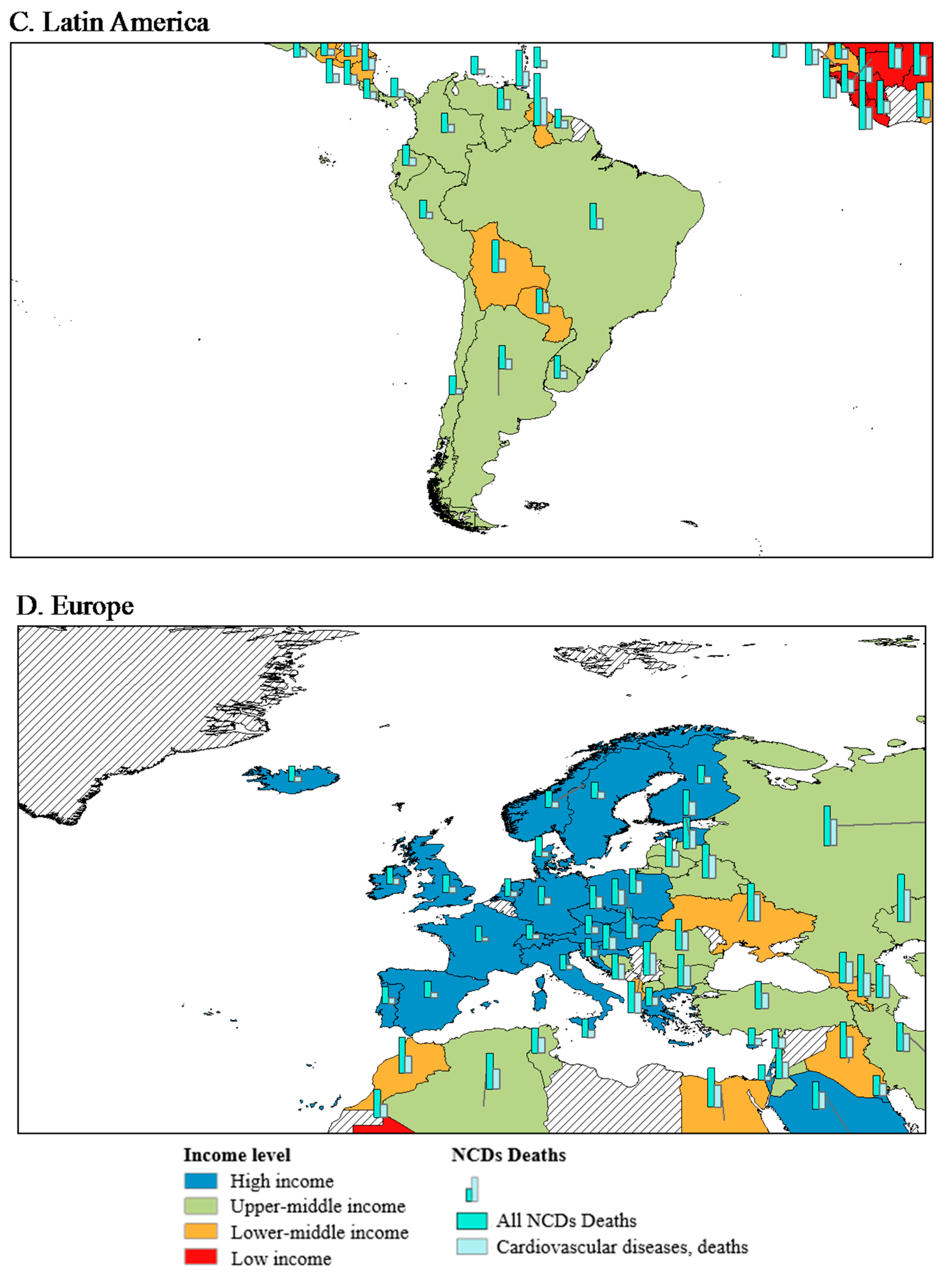
| All NCDs 11 | Numbers | 416 ± 149 | 564 ± 81 | 663 ± 73 | 636 ± 124 | <0.001 |
| Cancers | Numbers | 122 ± 17 | 127 ± 23 | 88 ± 19 | 104 ± 29 | <0.001 |
| Cardiovascular diseases | Numbers | 178 ± 134 | 285 ± 73 | 306 ± 74 | 277 ± 97 | <0.001 |
| Diabetes | Numbers | 11 ± 8 | 25 ± 22 | 35 ± 16 | 36 ± 13 | <0.001 |
| Chronic respiratory diseases | Numbers | 24 ± 8 | 60 ± 20 | 101 ± 52 | 57 ± 33 | <0.001 |
| Income Levels | |||||
|---|---|---|---|---|---|
| High Income | Upper-Middle Income | Lower-Middle Income | Low Income | p for Trend 3 | |
| Nutrition consumption | |||||
| Total energy intake (kcal/capita/day) | 3355 ± 287 | 3067 ± 206 | 2561 ± 254 | 2274 ± 210 | <0.001 |
| Fat (g/capita/day) | 132.9 ± 28.4 | 92.6 ± 14.2 | 55.7 ± 11.0 | 42.8 ± 12.8 | <0.001 |
| Fat (%) 4 | 35.4 ± 5.7 | 27.1 ± 3.2 | 19.6 ± 3.6 | 16.7 ± 4.2 | <0.001 |
| Protein (g/capita/day) | 101.8 ± 9.8 | 90.8 ± 10.6 | 64.3 ± 10.0 | 59.4 ± 9.4 | <0.001 |
| Protein (%) 5 | 12.1 ± 0.7 | 11.8 ± 0.9 | 10.0 ± 1.0 | 10.5 ± 1.3 | <0.001 |
| Carbohydrates (%) 6 | 52.5 ± 5.8 | 61.1 ± 3.6 | 70.4 ± 4.3 | 72.8 ± 4.0 | <0.001 |
| Food supply | |||||
| Fruit | 108.2 ± 35.2 | 108.4 ± 38.7 | 80.3 ± 41.9 | 69.5 ± 83.2 | <0.001 |
| Vegetable | 80.0 ± 24.7 | 151.3 ± 82.1 | 54.8 ± 24.8 | 30.4 ± 23.1 | <0.001 |
| Cereal | 934.5 ± 197 | 1329.9 ± 211.4 | 1406.5 ± 235.7 | 1352.8 ± 390.5 | <0.001 |
| Meat | 370.5 ± 89.5 | 369.9 ± 120.3 | 69 ± 90.8 | 68.6 ± 52.8 | <0.001 |
| Animal fat | 134.6 ± 85.8 | 48 ± 24.3 | 53 ± 30.8 | 15.4 ± 9.8 | <0.001 |
| Vegetable oil | 538.8 ± 154.2 | 262.7 ± 102.8 | 216.7 ± 59.2 | 156.5 ± 71.3 | <0.001 |
| Milk | 286.7 ± 106.7 | 122.8 ± 95.4 | 109.7 ± 80.5 | 62.5 ± 57.2 | <0.001 |
| Stimulant | 24.8 ± 12.2 | 5.7 ± 6.8 | 2.9 ± 4.4 | 2.4 ± 4 | <0.001 |
| Sugar and sweetener | 415.4 ± 119.4 | 213.1 ± 167 | 208 ± 74.2 | 98.7 ± 48.7 | <0.001 |
| Health-related behaviors | |||||
| Smoking 7 | 32.1 ± 12.8 | 41.3 ± 11.7 | 33.1 ± 16.7 | 23.5 ± 11.9 | <0.001 |
| Insufficient activity 8 | 28.2 ± 10.1 | 27.3 ± 8.4 | 18.3 ± 6.1 | 14.4 ± 6.9 | <0.001 |
| Alcohol consumers, past 12 months 9 | 38.5 ± 27.8 | 36.3 ± 13.7 | 25.3 ± 29.3 | 41.0 ± 23.6 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kang, S.; Kang, M.; Lim, H. Global and Regional Patterns in Noncommunicable Diseases and Dietary Factors across National Income Levels. Nutrients 2021, 13, 3595. https://doi.org/10.3390/nu13103595
Kang S, Kang M, Lim H. Global and Regional Patterns in Noncommunicable Diseases and Dietary Factors across National Income Levels. Nutrients. 2021; 13(10):3595. https://doi.org/10.3390/nu13103595
Chicago/Turabian StyleKang, Sooyoung, Minji Kang, and Hyunjung Lim. 2021. "Global and Regional Patterns in Noncommunicable Diseases and Dietary Factors across National Income Levels" Nutrients 13, no. 10: 3595. https://doi.org/10.3390/nu13103595
APA StyleKang, S., Kang, M., & Lim, H. (2021). Global and Regional Patterns in Noncommunicable Diseases and Dietary Factors across National Income Levels. Nutrients, 13(10), 3595. https://doi.org/10.3390/nu13103595






