Abstract
Suboptimal dietary intake is a critical cause of poor maternal nutrition, with several adverse consequences both for mothers and for their children. This study aimed to (1) assess maternal dietary patterns in India; (2) examine enablers and barriers in adopting recommended diets; (3) review current policy and program strategies to improve dietary intakes. We used mixed methods, including empirical analysis, compiling data from available national and subnational surveys, and reviewing literature, policy, and program strategies. Diets among pregnant women are characterized by low energy, macronutrient imbalance, and inadequate micronutrient intake. Supply- and demand-side constraints to healthy diets include food unavailability, poor economic situation, low exposure to nutrition counselling, food restrictions and taboos, adverse family influence and gender norms, and gaps in knowledge. Intervention strategies with potential to improve maternal diets include food-based programs, behavior change communication, and nutrition-sensitive agriculture interventions. However, strategies face implementation bottlenecks and limited effectiveness in real-world at-scale impact evaluations. In conclusion, investments in systems approaches spanning health, nutrition, and agriculture sectors, with evaluation frameworks at subnational levels, are needed to promote healthy diets for women.
1. Introduction
Poor maternal nutrition before and during pregnancy is a significant public health concern due to adverse consequences both for mothers and for their children. Maternal malnutrition is associated with increased risk of maternal morbidity, preterm deliveries, and small-for-gestational-age babies [1,2]. Maternal undernutrition remains a global concern, with 24% of women in South Asia having low body mass index (BMI) [1]. Further, 30% of women of reproductive age and 37% of pregnant women are anemic [3]. Overweight/obesity among women is an emerging issue affecting most low–middle-income countries [4].
Adequate dietary quantity and quality is an established determinant of poor maternal nutrition. In 2017, the Global Burden of Disease Study found that poor diets caused more deaths than did all other risk factors, attributable to a total of 11 million deaths, with 3 million deaths each due to high sodium intake and low intake of whole grains, and 2 million deaths due to low intake of fruits [5]. Poor diet during pregnancy has been associated with adverse pregnancy outcomes [2], which, in turn, increase child susceptibility to cardiometabolic diseases in later life [6]. Despite this evidence, maternal diets in low- and middle-income countries (LMICs) suffer from macronutrient and micronutrient imbalance, and are predominantly plant-based [7]. Many women have concurrent deficiencies of essential micronutrients such as iron, zinc, vitamins B12 and D, and iodine through their reproductive years [1]. A study from Guatemala, India, Pakistan, and Democratic Republic of the Congo reported that more than 80% of women had inadequate intakes of essential micronutrients [8].
In India, more than half of women are anemic [9], nearly 40% of women 15–49 years are underweight [10], and nearly 25% of women are overweight/obese [10]. Cereals and millets form the bulk of rural diets, as indicated by the National Nutrition Monitoring Bureau (NNMB) surveys in 10 Indian states, with only about half of pregnant women consuming adequate quantities of protein and energy [11]. NNMB also showed that intakes of iron, vitamins A and C, and folic acid were less than 50% of recommended levels for most pregnant women. Suboptimal diets, together with other factors, including early and multiple pregnancies, poverty, caste discrimination, and gender inequality, contribute to poor maternal nutrition in India [12]. Increased marketing of unhealthy and cheap foods along with high carbohydrate and sugar in public procurement systems have contributed to rising overweight/obesity and other noncommunicable diseases. High rates of death and years of life lost due to ill health, disability, or early death related to diet were also reported in the 2017 Global Burden of Disease Study [5].
The World Health Organization (WHO) guidelines on antenatal care (ANC) recommend 49 interventions, of which 14 are nutrition interventions [13]. The national guidelines in India follow global recommendations on a package of essential nutrition interventions for pregnant women, among them, improving diets. India’s flagship National Nutrition Mission, POSHAN Abhiyaan, aims to improve maternal nutrition through capacity building, leveraging technology, behavior change communication, community mobilization, and cross-sectoral convergence [14]. Current intervention strategies in India to improve maternal diets include a rich portfolio of programs and policies that address dietary intakes through take-home rations and hot cooked meals for pregnant and lactating women, micronutrient supplements, food fortification, delivery of subsidized staples through the public distribution system, cash transfers, nutrition-sensitive agriculture, and diet education and counseling. However, weak delivery systems, logistical gaps, resource scarcity, poor utilization, and wide disparities in access to food and health resources continue to hamper progress in improving diets among pregnant women [12].
This paper aims to (1) assess maternal dietary patterns in India; (2) examine enablers and barriers in adopting recommended diets; (3) review current policy and program strategies in India to improve dietary intakes and assess their effectiveness. Findings from this study will highlight policy, program, and research gaps, and will be used to offer recommendations for future action.
2. Materials and Methods
We used mixed methods for the study, including (1) reviewing data from available national surveys on food and nutrient intakes among pregnant women; (2) examining data on dietary intakes from the latest available national representative surveys to document dietary patterns and identify determinants of dietary patterns; (3) conducting a literature review to identify enablers and barriers to adopting recommended diets; (4) reviewing policy and program strategies to improve dietary intakes and their effectiveness; (5) integrating insights to offer recommendations for future action.
2.1. Review of Dietary Data from National Surveys
At the national level, the NNMB was established in 1972 by the National Institute of Nutrition and Indian Council of Medical Research to collect data on food and nutrient intakes in rural and tribal populations across 10 states (Kerala, Tamil Nadu, Karnataka, Andhra Pradesh, Maharashtra, Gujarat, Madhya Pradesh, Orissa, West Bengal, and Uttar Pradesh). Data were collected approximately every 10 years, with the latest round available in 2012 [15]. A special survey was also conducted in 2015, but only for the urban population and among nonpregnant and nonlactating women. The 2012 survey included a 24-h dietary recall with a small sample of pregnant women (n = 322) to collect information on average food and nutrient intakes. We extracted relevant data from the report to summarize dietary intakes among pregnant women.
2.2. Empirical Analysis of Publicly Available Data
We used data from National Family Health Survey 2005–06 (NFHS-3) [16] and 2015–16 (NFHS-4) [17]. NFHS-3 included data from 109,041 households and was representative at the state level. NHFS-4 was representative at both state and district levels, with data from 601,509 households. This analysis used data from pregnant women (n = 38,339). Dietary intake was collected using self-reported information on the frequency (daily, weekly, occasionally, and never) of 9 food groups (milk or curd, pulses or beans, dark green leafy vegetables, fruits, eggs, fish, chicken or meat, fried foods, and aerated drinks). We first compared changes in daily food group consumption from 2006 to 2016. We then used maps to visualize state-level variation in food intake in 2016. To examine inequalities in dietary intake, we used equity plots disaggregated by residence, wealth quintile, and caste group. Finally, we performed multivariable regression analyses to assess the association between a select set of determinants and food group consumption. Because the proportion of women who consumed fish, meat, and eggs daily was very low, we used an indicator of daily consumption of any animal source foods. We were not be able to compute minimum dietary diversity for women due to limited available data. The variables selected for regression models include maternal age, early marriage (defined as age at first marriage <18 years), early birth (defined as age at first birth <19 years), education, caste status, occupation, decision-making power, and household socioeconomic status (SES). Household SES was constructed using a principal component extracted from multiple variables, including household ownership of fifteen assets. All analyses were performed using Stata version 16.1. All regression models were adjusted for the cluster sampling design and sampling weights used in the survey.
2.3. Literature Review
The literature review aimed to (1) identify enablers and barriers in adopting recommended diets and (2) review policies/programs and assess the effectiveness of current intervention strategies to improve dietary intakes. Between 7 June and 17 July2021, we searched PubMed, MEDLINE, and Google Scholar with the following search terms ((Dietary intake OR diet OR Food consumption) AND (maternal OR pregnancy) AND (India)) with no language restriction but limited to “humans”, “Adolescent: 13–18 years”, “Adult: 19+ years”, and time between January 2000 and June 2021. In addition, we sourced grey literature from the last 10 years, including interventions, program evaluations, and unpublished literature from the government or organizational websites. The abstracts of all potential publications were reviewed independently by the first and second authors, then the full text of potentially eligible studies was obtained for in-depth review. We extracted data using a standardized template including authors, publication year, state, study objective, study design and sample size, enablers and/or barriers, and key findings of interventions.
The literature review of key enablers and barriers influencing maternal dietary intakes identified 20 studies across 13 states, including from Tamil Nadu, Karnataka, West Bengal, Maharashtra, Andhra Pradesh, Sikkim, Uttar Pradesh, Delhi, Bihar, Rajasthan, Chhattisgarh, Odisha, and Madhya Pradesh. Most studies (n = 18) aimed to understand maternal dietary beliefs and practices, and two studies aimed to assess affordability and access to nutritious diets. Studies varied in design and methods and included qualitative ethnographic studies (in-depth interview and focus group discussion), quantitative cross-sectional surveys, and market surveys.
The literature review of interventions identified a total of 14 studies from 10 states, including Andhra Pradesh, Telangana, Karnataka, Odisha, Rajasthan, Punjab, Tamil Nadu, Haryana, Uttar Pradesh, and Kerala. Most studies aimed to assess the effects of different strategies to improve maternal nutrition and used various methods and study designs: cluster-randomized control trials, quasi-experimental studies, cross-sectional surveys, and qualitative methods (focused group discussions and in-depth interviews).
3. Results
3.1. Current Situation of Maternal Diets in India
3.1.1. Maternal Diets at the National Level
The review of NNMB data showed that energy and macronutrient intakes were lower than recommended (Table 1). The median intake of energy was 1736 Kcal [15], compared to the estimated average requirement (EAR) of 2010 Kcal, and the median intake of protein was 45 g, compared to the EAR of 54 g for sedentary pregnant women [18]; about half of pregnant women had inadequate intakes of energy, 35% had inadequate protein intake, and 20% had inadequate fat intake. Intakes of essential micronutrients such as iron, vitamin A, riboflavin, vitamin C, and folic acid were less than 50% of RDA among most pregnant women (~50–80%) [15]. The average intake of several food groups (cereals and millets, nuts and seeds, milk and milk products, and sugar) decreased over time between 1997 and 2012 among pregnant women. Daily intakes of all nutrients except vitamin A, thiamine, and niacin also declined from 1997 to 2012 (data not shown).

Table 1.
Macro- and micronutrient intakes.
Analysis of NFHS data revealed no improvement in dietary intakes among PW between 2006 and 2016, except for dairy, which increased marginally over time (8 percentage points, pp) (Figure 1). Consumption of pulses and vegetables reduced over time (6 and 16 pp, respectively). In 2016, diets among PW remained suboptimal for most food groups: less than 10% of PW consumed meat, fish, and/or eggs, a fifth consumed fruits, and about half consumed pulses, dairy, and vegetables daily. Unhealthy food consumption including aerated beverages and fried foods was 4–8% among PW in 2016.
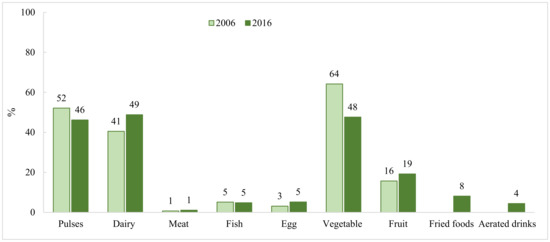
Figure 1.
Dietary intake among pregnant women in India between 2006 and 2016 1. 1 National data comes from National Family Health Surveys in 2005–2006 and 2015–2016.
Food group consumption was higher among wealthier compared with poorer households, with the highest gap being in dairy consumption (35 percentage points, pp), followed by fruits (21 pp), pulses (12 pp), and green vegetables (11 pp) (Figure 2). Similar inequity in dietary intakes was observed between residential areas and among caste groups; women living in rural areas or belonging to backward castes had lower intakes compared with their counterparts.
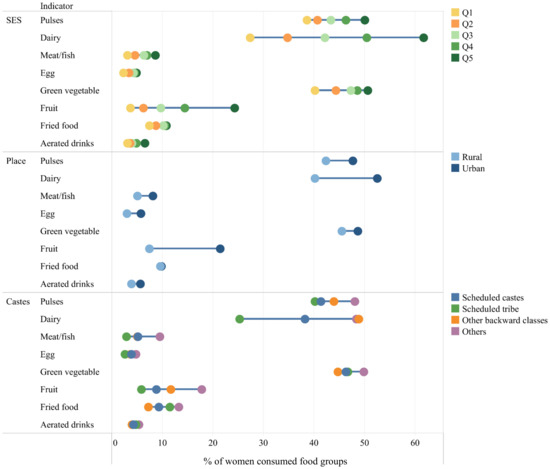
Figure 2.
Socioeconomic 1, residential, and caste inequality in dietary intake among Indian pregnant women. SES: socioeconomic status; Q: quintile. Data are from National Family Health Survey 2015–2016. 1 Household SES was constructed using the principal component analysis method. The first principal component was used to divide household SES into quintiles; the lowest quintile (Q1) represented the poorest 20% of the population and the highest quintile (Q5) represented the richest 20%.
3.1.2. Maternal Diets at the Subnational Level
Subnational data on dietary intake showed a low percent of PW consuming animal-source foods in most states in 2015–2016 (<30%), with the exception of Kerala where 65% of women consumed meat or fish (Figure 3). Similarly, low consumption of fruits was observed for most states. There were substantial subnational variations across states in consumption of pulses, dairy, and green vegetables (ranging from 3% to 80%). Consumption of unhealthy foods was higher in some Eastern states, particularly Odisha (69%) and Mizoram (86%).
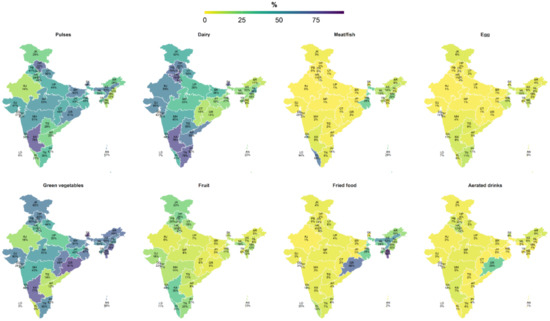
Figure 3.
Subnational variation in dietary intake among pregnant women in India 1. 1 Data comes from the National Family Health Survey in 2015–2016. Values are percentages of women consuming these food groups. AN: Andaman and Nicobar Island; AP: Andhra Pradesh; AR: Arunachal Pradesh; AS: Assam; BR: Bihar; CH: Chandigarh; CT: Chhattisgarh; DD: Daman and Diu; DH: Dadara and Nagar Havelli; DL: NCT of Delhi; GA: Goa; GJ: Gujarat; HP: Himachal Pradesh; HR: Haryana; JH: Jharkhand; JK: Jammu and Kashmir; KA: Karnataka; KL: Kerala; LD: Lakshadweep; MH: Maharashtra; ML: Meghalaya; MN: Manipur; MP: Madhya Pradesh; MZ: Mizoram; NL: Nagaland; OR: Odisha; PB: Punjab; PY: Puducherry; RJ: Rajasthan; SK: Sikkim; TG: Telangana; TN: Tamil Nadu; TR: Tripura; UP: Uttar Pradesh; UT: Uttarakhand; WB: West Bengal.
Subnational data on dietary intake among PW based on 24-h recall of 10 food groups were available for some states (Uttar Pradesh [21], Bihar, Odisha, and Chhattisgarh [22] (Figure S1). In Uttar Pradesh, only about a fifth of PW achieved dietary diversity (consumed ≥5 food groups in a day), while about third of PW in Bihar and more than half of PW in Odisha and Chhattisgarh consumed diverse diets.
Data on macro- and micronutrient intakes at the subnational level were available in Uttar Pradesh only [21] (Table 1). Energy intakes were lower than recommended, and macronutrient intakes were imbalanced. Per capita mean energy intake was 1759 kcal in Uttar Pradesh, far below the individual requirement of 2322 kcal/day. Over 75% of energy came from carbohydrates (recommendation: 45–65%), 12% from protein (recommendation: 10–35%), and 11% from fat (recommendation: 20–35%). In addition, >80% of PW had inadequate intakes for 9 of 11 essential micronutrients.
3.2. Enablers of and Barriers to Adopting Recommended Diets in India
Key enablers of and barriers to maternal diets identified through empirical analysis (Table 2) and the literature review (Table 3) are presented by theme below.

Table 2.
Factors associated with dietary intake among pregnant women, NFHS-4 data 2015–16.

Table 3.
Summary of enablers of and barriers to optimal diets from subnational data.
3.2.1. Food Availability and Accessibility
The review found mixed results on the role of food availability and accessibility in influencing maternal diets. Findings from an ethnographic study in Tamil Nadu found that women reduced consumption of millets and switched to rice due to lack of availability [28]. Another study in Maharashtra similarly found that with easier food access, consumption of staple foods reduced and of other foods increased [29]. In addition, qualitative in-depth interviews in Uttar Pradesh showed that pregnant women were constrained by limited food items in their markets and travel limitations for women [30]. In contrast, a cost-of-diet survey found that food availability in markets was not a key barrier to nutritious diets [31], but other factors that may affect availability, such as seasonality and market access, were not reported.
3.2.2. Economic Constraint and Affordability
Both the empirical analysis and the literature review highlighted the important role of higher economic status as an enabler and financial constraints as a barrier in adopting recommended diets. Regression analysis showed that, compared to the poorest households, the richest households were 3.7 times more likely to consume dairy, nearly twice as likely to consume animal-source foods, and 5 times more likely to consume dark green leafy vegetables. Larger households (≥7 people) were less likely to consume animal-source foods and dark green leafy vegetables, but more likely to consume pulses.
Findings from studies identified during the literature review corroborated findings from the empirical analysis [21,22,24,30,31,32,35,36]. Mothers belonging to richer households were about two times more likely to consume a diverse diet (≥5 food groups) [21,36]. Nutritious diets were unaffordable for ~65–75% of households [31,35]. Women did not consume recommended foods due to lack of money [38]. Higher parity was associated with less consumption of special foods during pregnancy, such as milk, animal protein, pulses, and fruits [34], and was associated with lower diet diversity [21,34,36].
3.2.3. Exposure to Health and Nutrition Services
Receipt of health and nutrition services and counseling on diet was associated with a 1.5–3 times greater likelihood of higher dietary diversity and consuming more food groups [21,39,40]. Dietary diversity was lower among women who had no prior contact with a health professional (OR = 0.6) [36]. In addition, interventions of home production, subsidized grains, and food supplementation improved the affordability of nutritious diets by 10–35% [31]. Although overall use of food supplementation increased between 2006 and 2016 from 19% to 53%, marginalized groups such as lower castes and tribes, the poorest quintiles, or those with low schooling levels were still left behind [27].
3.2.4. Maternal Education
In our empirical analysis, compared to illiterate mothers, those with high school or higher education were nearly twice as likely to consume pulses, 3 times more likely to consume dairy and animal source foods, and 5.6 times more likely to consume dark green leafy vegetables.
Studies from the literature review showed that mothers with higher education or at least 6 years of education were more likely to have higher dietary diversity compared with illiterate mothers [21,36]. Higher literacy was associated with consuming special foods such as milk and animal source foods during pregnancy [34].
3.2.5. Maternal Knowledge
The review found that higher maternal knowledge was associated with higher diet diversity (OR = 2.2) and greater number of food groups consumed [21]. Qualitative interviews also confirmed that high awareness and high knowledge of diet diversity recommendations were the key enablers affecting behavioral adoption for diet diversity [30]. Additional enablers included knowing that nutritious foods included fruits, vegetables, egg, and animal-source foods; 60% of women believed that these foods were beneficial for health and should be consumed during pregnancy [28,32,33].
3.2.6. Food Taboos and Restrictions during Pregnancy
Food taboos and restrictions during pregnancy were mentioned in several qualitative studies across different states [24,25,26,28,33,34,38]. Most mothers (65% to 82%) believed that some food items should be restricted during pregnancy [33,34]. Various fruits (banana, papaya, jackfruit, and coconut), vegetables (brinjal and leafy vegetables), meat, fish, and eggs were believed to be heat-producing or sour, thus should be restricted during pregnancy to prevent miscarriage and fetal malformations, and promote easy delivery [25,26,28,38]. Other beliefs associated with the type of food given to pregnant women included “casting an evil eye” or “color of the baby” [25]. Most food avoidance was based on advice from elders and family members [28]. Mothers who had strong likes and dislikes during pregnancy and experienced nausea were less likely to follow diet recommendations [30].
3.2.7. Family Influence
The review yielded mixed findings on the role of family members in influencing maternal diets. Qualitative in-depth interviews in one study showed that family members had high levels of awareness and motivation to ensure nutritious diets for pregnant women [30]. Specifically, husbands supported pregnant women by procuring nutritious foods from the market and reminding them to eat recommended foods. In contrast, another study reported that family elders restricted certain foods during pregnancy [28].
3.2.8. Gender Norms
Strong gendered social norms affected many aspects of women’s health and well-being, including nutrition behavior and practices [37]. From childhood to adulthood, women’s health and nutrition is given lower priority than is men’s health and nutrition. Women are usually the last to eat in the household and eat the least amount of food [37]. In many households, men were responsible for procurement of food from the market, often themselves deciding what food items to buy or buying food items as decided by the mother-in-law while women had limited access to markets and minimal ability in exercising their choices for food items [23].
3.2.9. Other Demographic Factors
Our regression analysis showed that households in urban areas were 1.7 times more likely to consume dairy and 2.7 times more likely to consume dark green leafy vegetables than were those in rural areas. Belonging to scheduled caste/tribe or other backward classes was associated with lower consumption of pulses (OR = 0.85) and dairy (OR = 0.79). Early marriage was associated with 17% and 32% lower consumption of dairy and dark green leafy vegetables, respectively. The literature review confirmed that women belonging to lower caste (OR = 0.9) and rural households (OR = 6.9) were more likely to have lower diversity [21,39,40].
3.2.10. Indigenous Foods
Trends in the use of indigenous foods also affect PW’s diets. Being a country with the largest tribal population in the world, India is composed of 705 distinct tribal groups who make up nearly one-tenth of the country’s population (104 million). Tribal people cultivate local foods and collect uncultivated foods from forests; thus, they are able to eat nutritious food [41]. However, several barriers affecting this population included experiencing discrimination in access to agricultural inputs or economic opportunities, expulsion from their lands, and displacement to urban settlements where they lose access to their cultural heritage and their traditional foods, practices, and languages [42]. The introduction of modern technologies has improved their lives but has also brought other challenges, including altering the nutritive value of indigenous foods due to chemical use, or reducing diversity of traditional foods through degradation of forest and agro-biodiversity [43].
3.3. Policies to Improve Maternal Diet
Selected policies to improve maternal diet are summarized in Figure 4. The National Nutrition Policy (NNP) 1993, formulated in the national development context, positioned nutrition as a complex development problem linked to agriculture, food production, and poverty. The NNP recommended both direct and indirect nutrition interventions that include nutrition-specific and nutrition-sensitive interventions. India’s nutrition policies recognize the multifaceted nature of interventions necessary to accelerate progress in nutrition. Various programs and schemes have been launched and expanded over the years to improve maternal diets and nutritional status. Schemes in India are largely delivered through flagship programs of two ministries: (1) the Integrated Child Development Services (ICDS) scheme under the Ministry of Women and Child Development provides micronutrient-fortified supplementary food and/or energy-dense take-home rations for pregnant women and breast-feeding mothers; (2) the Ministry of Health and Family Welfare delivers micronutrient supplements (IFA and calcium), deworming, weight gain monitoring, and dietary counseling to pregnant women as part of antenatal care services.
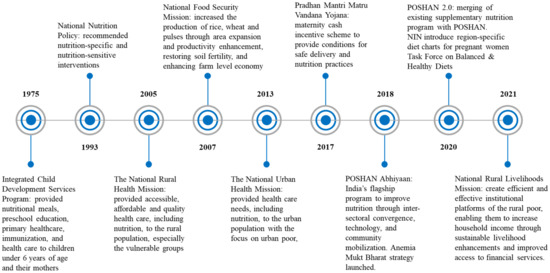
Figure 4.
Summary of key policies to improve maternal nutrition and maternal diets.
One of the notable current programs is POSHAN Abhiyaan, (Prime Minister’s overarching scheme for holistic nutrition), India’s flagship program that was launched in 2018, with an aim to improve nutritional outcomes for children, pregnant women, and lactating mothers. The core components of the POSHAN Abhiyan include a focus on inter-sectoral convergence, use of technology, and Jan Andolan (people’s movement). The current program is being strengthened in the form of POSHAN 2.0, where an existing Supplementary Nutrition Program and the POSHAN Abhiyan will be merged to increase nutritional content, delivery, outreach, and outcomes. Another important program is a maternity benefit program titled “Pradhan Mantri Matru Vandana Yojana (PMMVY)”. The cash incentive helps to improve safe delivery and good nutrition and feeding practices. Other programs, including the National Health Mission, Anemia Mukt Bharat program, National Rural Livelihoods Mission, and Task Force on Healthy and Balanced Diets, also indirectly or directly aim to improve maternal nutrition. However, despite evidence of rising overweight and obesity among women, the current policy guidelines lack specific recommendations on improving diets for pregnant women in different body mass index (BMI) categories ranging from thin to obese. In 2020, the Ministry of Women and Child Development started sharing region-specific diet charts, which were prepared by Indian Council for Medical Research—National Institute of Nutrition [44]. These charts have been created for six regions—North, South Central, East, West, and North East—to guide pregnant women on their nutritional requirements, keeping different dietary habits and cultures in mind. The current implementation status of the region-specific diet chart is unknown.
3.4. Current Intervention Strategies in India to Improve Dietary Intakes and Their Effectiveness
Several intervention strategies have been implemented to improve maternal diets in India, including hot cooked meals, food innovations in take-home rations (THR), maternal cash transfer programs, food fortification of staples, behavior change communication (BCC) strategies, and nutrition-sensitive agriculture interventions (Table 4).

Table 4.
Studies on program strategies in India to improve maternal diets.
3.4.1. Hot Cooked Meals
The review identified three studies on hot cooked meals, which found some improvements in the proportion of women consuming diverse diets post-intervention (~60%), consumption of specific food groups (eggs and milk—74% to 96%), and energy and protein intake among pregnant women [45,46,47]. However, several implementation issues were noted, including lower distribution of foods and fewer feeding days compared with the program protocol.
3.4.2. Food Innovations in Take-Home Rations
Three studies were found on food innovations that are applicable for THR through centralized models of production. An innovative enzyme called phytase was found to significantly improve mineral bioavailability from plant-based diets and cereal–legume foods [60,61]. Another area for innovation in THR is the role of fermented foods on gut health and nutrition status. A Lactobacillus plantarum strain isolated from the dosa has been found to inhibit the growth of a range of food-borne pathogens [48].
3.4.3. Maternal Cash Transfers
Only one study was found on maternal cash transfers, which reported a decline of 0.84 on the household food insecurity access scale following receipt of cash transfer [49]. The key bottlenecks were smaller transfers than expected and delays in payment to beneficiaries.
3.4.4. Food Fortification of Staples
Two studies were identified on fortification of staples, which reported low levels of fortification of wheat flour (6%), edible oil (24%), and salt (66%) [50,51]. Key challenges related to food fortification were low demand given low consumption of wheat in many predominantly rice-eating regions in the South and most households purchasing whole grain and milling produce locally (82%) in the North. The other barrier was lack of monitoring of compliance to fortification protocols.
3.4.5. Behavior Change Communication
Strategies of BCC were reported in six studies, which included nutrition counseling and visual tools to improve maternal diets. Most studies reported positive impacts on dietary intake, including increased quantity, frequency (from 2–3 to 3–4 meals), and quality of diets (increased intake of vitamin A-rich fruits, other vegetables, and higher protein intake), however few studies reported impacts on overall dietary diversity [52,53,54,55,56]. Despite improvements, dietary intakes did not meet recommended levels for most micronutrients. The key factors associated with adoption of recommended behaviors were maternal perceptions, role of family members, food preferences, and limited resources. Many research gaps remain, however, on evidence of BCC complemented by systems strengthening efforts to improve quality and sustainability. The Alive & Thrive maternal nutrition study is the only study that included evidence on integrating multiple strategies as part of BCC interventions in existing antenatal care [54]. Other studies documented the development and feasibility of integrating a maternal service package for mothers of children with severe acute malnutrition admitted to nutrition rehabilitation centers in Delhi and Uttar Pradesh [57,62].
3.4.6. Nutrition-Sensitive Agriculture Interventions: Empowerment through Income and Access to Nutritious Foods
A model of improving socioeconomic and nutrition conditions through women’s empowerment is a poultry cooperative in central India—Madhya Pradesh Women Poultry Producers’ Company Limited (MPWPCL) [58]. MPWPCL is an all-women-owned and -managed farmer co-operative that promotes smallholder poultry women farmers in difficult-to-reach areas, by aggregating them in clusters. Based on market principles, MPWCL generates wealth leading to their socioeconomic upliftment. Women are trained in poultry farming and provided capital to set up small farms. All farms are supported with high-quality and a steady supply of affordable inputs, with regular supervision. By doing so, good poultry management practices are reinforced, resulting in improved farm operational efficiency and safety from disease outbreaks. As a result, income increased by eight times per household and more eggs became available in the community. Another study reported on nutrition-sensitive agriculture interventions and found positive impacts on maternal dietary diversity through exposure to videos and participatory learning activities [59].
4. Discussion
Maternal diets affect women’s immediate well-being and livelihoods as well as the health, cognition, and productivity of the next generation [1]. Through literature review and empirical analysis with multiple data sources, this mixed methods study assessed trends in maternal diets in India, identified enablers of and barriers to adopting diets, and documented program interventions and policies in India. Dietary intakes among pregnant women were suboptimal with low energy, imbalanced macronutrients, and inadequate micronutrient intakes, and varied substantially across states. Economic constraints, food taboos, and social norms play an important role, with family members emerging as key influential persons. Interventions that can improve maternal diets in India are not well evaluated but highlight the importance of ICDS food-based programs, BCC strategies, and nutrition-sensitive agriculture interventions.
4.1. Data Gaps on Maternal Dietary Practices and Evaluation Impacts of Programs and Interventions
This study highlighted critical data gaps regarding maternal dietary practices and evaluation impacts of programs and interventions. The Global Nutrition Report in 2017 recognized the importance of high-quality, regular, disaggregated data to ensure accountability and progress towards improving nutrition universally [63]. However, nationally representative data on maternal diets in India are very limited. The most recent NFHS data collected dietary information using food frequency questions that did not include sufficient food groups to calculate maternal dietary diversity, macro- or micronutrient intakes, or food security status to help understand consumption patterns of families affected by food insecurity. The NNMB data used a 24-h dietary recall of food and nutrient intakes but was limited by a small sample of pregnant women in rural areas (n = 322 for all 10 states), and the most recent round available is from 2012. The NNMB data collected in urban areas in 2015–2016 did not include data for pregnant women [64]. Although fish is recommended as a source of essential nutrients during pregnancy in the national guideline [65], we did not identify any studies that specifically evaluated meat or fish separately, nor any that reported on omega-3 or omega-6 fatty acids. The evidence review also found limited available research on impacts of programs and interventions. For example, although food supplementation under ICDS scheme has been widely implemented, only a few studies exist on the hot cooked meal and THR program. These small-scale studies mainly focus on implementation issues and lack impact evaluation to assess the extent of the program’s impact on maternal nutrition outcomes [66]. Rigorous evaluations are needed to test successful innovations and models to harmonize THR recipes and standards across all states.
4.2. Factors Influencing Maternal Diets in India
Multiple supply- and demand-side factors influence maternal diets in India. The predominant factors include food unavailability, economic constraints, low exposure to nutrition services and counselling, food restrictions and taboos during pregnancy, family influence, gender norms, and gaps in maternal knowledge. There is, however, limited information on how household budgets can be adjusted to procure specific nutrient-rich foods for meeting the needs of pregnant women. The evaluations in India identified intervention-specific limitations in implementation, such as inadequate food distributed and fewer days of distribution in hot meals programs, small amounts and delayed payments in cash transfer programs, and low coverage of foods selected for fortification and inadequate fortification levels. Thus, investments to improve nutrition, including maternal diet, must be fundamentally multisectoral in nature and focus on strengthening the delivery, reach, and utilization of nutrition-specific interventions.
4.3. Intervention Strategies with Potential to Improve Maternal Diets in India
The literature review also found few intervention strategies with potential to improve maternal diets in India. Specifically, food supplementation and cash transfer program evaluations suggest improvements in affordability of diets by reducing economic constraints in obtaining recommended foods [67]. Lack of food availability is a complex problem with many potential factors, including access to markets, diversity and types of food available in markets, low agriculture production, postharvest losses, and seasonality. Strategies to improve food availability include kitchen gardens, homestead production, women cooperatives, and nutrition-sensitive agriculture interventions [68]. Food systems approach (from Farm to Fork) needs to be strengthened to ensure affordability, availability, accessibility, food security, sustainability, and resilience in production and promotion of diverse nutrient-rich foods and safe diets for pregnant women.
BCC, along with community sensitization and engagement, can be an effective strategy to improve maternal knowledge, motivate family members (especially husbands and mothers-in-law) to support maternal diets, and clarify misconceptions about food taboos during pregnancy where foods are available but not utilized optimally [69]. BCC needs to be complemented by efforts to address the gender-based power differentials within the family related to decision making on choice of food items, procurement, preparation, and food distribution, and efforts to improve women’s informed decision-making power, agency, and access to resources. Multiple platforms (at home, community, and facility levels) across multiple sectors (health, nutrition, rural development/self-help groups) need to be engaged to ensure coverage, intensity, continuity, and quality. Experience from the maternal nutrition study in Uttar Pradesh, India [54] and Bangladesh [69] highlighted the crucial roles of investing in systems strengthening efforts of capacity building (knowledge and skills for counselling, and supportive supervision of frontline workers and providers across multiple sectors), use of data to review and track progress, setting up of convergent action planning and review mechanisms, and ensuring accountability of program managers. Regular mass media campaigns using existing social media platforms of all stakeholders are needed to disseminate accurate and uniform information about the importance of healthy and balanced diets for pregnant women.
Over the past two decades, there have been several experiments in the THR program. Dedicated government bodies, frontline workers, and supporting organizations have led to better recipes, viable production models, and mechanisms for women’s participation, as well as better governance and accountability. The initiatives have been further strengthened by the Supreme Court’s ruling emphasizing quality and safety standards during THR production and the role of automated machines for assuring food safety and quality. Fermented food has emerged as an innovation in THR. While there is limited evidence on the health benefits of fermented foods during pregnancy, India is among very few countries that encourage the consumption of fermented foods during pregnancy in its national food guide [70]. There are more than 350 types of fermented foods in India [71], and these foods are common in every food culture—modern or traditional; rural or urban or tribal. They can be prepared at home or through self-help groups and are convenient to produce through the decentralized THR production models. It would be worth exploring the effect of fermented foods on maternal health.
4.4. Policy Implication
Our findings highlight policy, program, and research gaps, and offer recommendations for future action. Policy and program guidelines across multiple health, nutrition, and agriculture sectors need to prioritize and invest sufficiently in resource allocation towards accelerating efforts to improve maternal diets. Operational guidelines need to be strengthened and updated. Guidelines should include micronutrient supplement formulations, locally adapted food supplements, the required number of counseling sessions and counseling guidelines on diet, and management of special dietary requirements for at-risk groups of pregnant women, including overweight and obese pregnant women, and should clarify roles among functionaries across different sectors. Strategies need to be both universal and targeted to address special requirements and must be contextualized to local environments to integrate local food and diet patterns and sociocultural norms around dietary practices of pregnant women. Emphasis should be on combined packages across health and food systems, social safety nets, and women’s empowerment with social and behavior change integral to all interventions.
5. Conclusions
Poor diets in pregnancy have wide-ranging and long-lasting detrimental impacts [1,2]. Investments are urgently needed in ongoing tracking of dietary patterns of PW, investigating factors influencing diets, addressing barriers through interventions, and development of quality standards for implementing programs. Priority should be placed on commitment to research for closing data gaps and strengthening existing platforms reaching pregnant women in all socioeconomic classes. Social behavior change interventions should be developed and adapted for specific locations as a part of existing programs. Other broader programs should be considered, including strengthening an ANC package, community mobilization for empowering women through self-help groups, and ICDS food-based programs combined with community awareness.
Supplementary Materials
The following are available online at www.mdpi.com/article/10.3390/nu13103534/s1, Figure S1: Dietary intake among pregnant women in selected states.
Author Contributions
P.H.N.: conceptualization, methodology, data curation, formal analysis, original draft preparation, and final draft revision. S.K.: data curation, formal analysis, and original draft preparation. L.M.T.: data curation, validation, and visualization. T.S., S.G., B.K., and K.B.: data interpretation and its implications, original draft preparation, and review and editing manuscript. P.M.: funding acquisition, investigation, and review and editing manuscript. V.S.: investigation, data interpretation and its implications, and review and editing manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the Bill & Melinda Gates Foundation through Partnerships and Opportunities to Strengthen and Harmonize Actions for Nutrition in India (POSHAN, grant numbers: OPP1150189), led by International Food Policy Research Institute.
Institutional Review Board Statement
Ethical approval was not required for this study as anonymized data used for secondary data analysis were from existing surveys, which all had prior ethical clearance from international and national institutional review boards.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data availability statement: The data that support the findings of this study are available in the tables/figures and in the Supplementary Materials of this article.
Acknowledgments
We would like to thank Sam Scott, Research Fellow at IFPRI, for his support to edit the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Victora, C.G.; Christian, P.; Vidaletti, L.P.; Gatica-Dominguez, G.; Menon, P.; Black, R.E. Revisiting maternal and child undernutrition in low-income and middle-income countries: Variable progress towards an unfinished agenda. Lancet 2021, 397, 1388–1399. [Google Scholar] [CrossRef]
- Ramakrishnan, U.; Grant, F.; Goldenberg, T.; Zongrone, A.; Martorell, R. Effect of women’s nutrition before and during early pregnancy on maternal and infant outcomes: A systematic review. Paediatr. Perinat. Epidemiol. 2012, 26 (Suppl. 1), 285–301. [Google Scholar] [CrossRef] [PubMed]
- WHO. Global Health Observatory. Data on Anemia. Available online: https://www.who.int/data/gho/data/themes/topics/anaemia_in_women_and_children (accessed on 4 May 2021).
- Popkin, B.M.; Corvalan, C.; Grummer-Strawn, L.M. Dynamics of the double burden of malnutrition and the changing nutrition reality. Lancet 2020, 395, 65–74. [Google Scholar] [CrossRef]
- GBD Diet Collaborators. Health effects of dietary risks in 195 countries, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019, 393, 1958–1972. [Google Scholar] [CrossRef]
- Barker, D.J.P. Mothers, Babies and Health in Later Life; Churchill Livingstone: Edinburgh, UK, 1998. [Google Scholar]
- Lee, S.E.; Talegawkar, S.A.; Merialdi, M.; Caulfield, L.E. Dietary intakes of women during pregnancy in low- and middle-income countries. Public Health Nutr. 2013, 16, 1340–1353. [Google Scholar] [CrossRef] [PubMed]
- Lander, R.L.; Hambidge, K.M.; Westcott, J.E.; Tejeda, G.; Diba, T.S.; Mastiholi, S.C.; Khan, U.S.; Garces, A.; Figueroa, L.; Tshefu, A.; et al. Pregnant women in four low-middle income countries have a high prevalence of inadequate dietary intakes that are improved by dietary diversity. Nutrients 2019, 11, 1560. [Google Scholar] [CrossRef]
- Nguyen, P.H.; Scott, S.; Avula, R.; Tran, L.M.; Menon, P. Trends and drivers of change in the prevalence of anaemia among 1 million women and children in India, 2006 to 2016. BMJ Glob. Health 2018, 3, e001010. [Google Scholar] [CrossRef]
- Young, M.F.; Nguyen, P.; Tran, L.M.; Avula, R.; Menon, P. A double edged sword? Improvements in economic conditions over a decade in India led to declines in undernutrition as well as increases in overweight among adolescents and women. J. Nutr. 2020, 150, 364–372. [Google Scholar] [CrossRef]
- Shankar, B.; Agrawal, S.; Beaudreault, A.R.; Avula, L.; Martorell, R.; Osendarp, S.; Prabhakaran, D.; McLean, M.S. Dietary and nutritional change in India: Implications for strategies, policies, and interventions. Ann. N. Y. Acad. Sci. 2017, 1395, 49–59. [Google Scholar] [CrossRef]
- Ramakrishnan, U.; Lowe, A.; Vir, S.; Kumar, S.; Mohanraj, R.; Chaturvedi, A.; Noznesky, E.A.; Martorell, R.; Mason, J.B. Public health interventions, barriers, and opportunities for improving maternal nutrition in India. Food Nutr. Bull. 2012, 33, S71–S92. [Google Scholar] [CrossRef]
- WHO. WHO Recommendations on Antenatal Care for a Positive Pregnancy Experience; World Health Organization: Geneva, Switzerland, 2016. [Google Scholar]
- Abhiyaan, P. PM’s Overarching Scheme for Holistic Nourishment. Available online: http://poshanabhiyaan.gov.in/#/ (accessed on 10 July 2021).
- National Nutrition Monitoring Bureau. Diet and Nutritional Status of Rural Population, Prevalence of Hypertension & Diabetes Among Adults and Infant & Young Child Feeding Practices—Report of Third Repeat Survey; NNMB Technical Report No 26; National Institute of Nutrition; Indian Council of Medical Research: Hyderabad, India, 2012.
- IIPS—International Institute for Population Sciences and Macro International. National Family Health Survey (NFHS-3), 2005–06; IIPS: Mumbai, India, 2007; Volume 1. [Google Scholar]
- IIPS—International Institute for Population Sciences and ICF. National Family Health Survey (NFHS-4), 2015–16; IIPS: Mumbai, India, 2017. [Google Scholar]
- ICMR-National Institute of Nutrition. Recommended Dietary Allowances and Estimated Average Requirements Nutrient Requirements for Indians-2020: A Report of the Expert Group Indian Council of Medical Research National Institute of Nutrition; National Institute of Nutrition: Hyderabad, India, 2020.
- Otten, J.; Hellwig, J.; Meyers, L. Dietary Reference Intakes: The Essential Guide to Nutrient Requirements; The National Academies Press: Washington, DC, USA, 2006. [Google Scholar]
- Torheim, L.E.; Ferguson, E.L.; Penrose, K.; Arimond, M. Women in resource-poor settings are at risk of inadequate intakes of multiple micronutrients. J. Nutr. 2010, 140, 2051S–2058S. [Google Scholar] [CrossRef]
- Nguyen, P.H.; Kachwaha, S.; Avula, R.; Young, M.; Tran, L.M.; Ghosh, S.; Agrawal, R.; Escobar-Alegria, J.; Patil, S.; Menon, P. Maternal nutrition practices in Uttar Pradesh, India: Role of key influential demand and supply factors. Matern. Child Nutr. 2019, 15, e12839. [Google Scholar] [CrossRef] [PubMed]
- Unisa, S.; Saraswat, A.; Bhanot, A.; Jaleel, A.; Parhi, R.N.; Bhattacharjee, S.; Purty, A.; Rath, S.; Mohapatra, B.; Lumba, A.; et al. Predictors of the diets consumed by adolescent girls, pregnant women and mothers with children under age two years in rural eastern India. J. Biosoc. Sci. 2020, 53, 663–682. [Google Scholar] [CrossRef] [PubMed]
- Alive & Thrive. Nutrition Practices in Uttar Pradesh, Results of a Formative Research Study; Alive & Thrive: Uttar Pradesh, India, 2016. [Google Scholar]
- Andersen, L.T.; Thilsted, S.H.; Nielsen, B.B.; Rangasamy, S. Food and nutrient intakes among pregnant women in rural Tamil Nadu, South India. Public Health Nutr. 2003, 6, 131–137. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Catherin, N.; Rock, B.; Roger, V.; Anlita, C.; Ashish, G.; Delwin, P.; Shanbhag, D.; Goud, B. Beliefs and practices regarding nutrition during pregnancy and lactation in a rural area in Karnataka, India: A qualitative study. Int. J. Community Med. Public Health 2015, 2, 116–120. [Google Scholar] [CrossRef]
- Chakrabarti, S.; Chakrabarti, A. Food taboos in pregnancy and early lactation among women living in a rural area of West Bengal. J. Fam. Med. Prim. Care 2019, 8, 86–90. [Google Scholar] [CrossRef]
- Chakrabarti, S.; Raghunathan, K.; Alderman, H.; Menon, P.; Nguyen, P. India’s Integrated Child Development Services programme; equity and extent of coverage in 2006 and 2016. Bull. World Health Organ. 2019, 97, 270–282. [Google Scholar] [CrossRef]
- Craig, H.C.; Jeyanthi, R.; Pelto, G.; Willford, A.C.; Stoltzfus, R.J. Using a cultural-ecological framework to explore dietary beliefs and practices during pregnancy and lactation among women in Adivasi communities in the Nilgiris Biosphere Reserve, India. Ecol. Food Nutr. 2018, 57, 165–186. [Google Scholar] [CrossRef]
- Ganpule-Rao, A.V.; Roy, D.; Karandikar, B.A.; Yajnik, C.S.; Rush, E.C. Food Access and Nutritional Status of Rural Adolescents in India: Pune Maternal Nutrition Study. Am. J. Prev. Med. 2020, 58, 728–735. [Google Scholar] [CrossRef]
- Jhaveri, N.R. In-Depth Understanding of Drivers of Maternal Nutrition Behavior Change in the Context of an Ongoing Maternal Nutrition Intervention in Uttar Pradesh, India. Master’s Thesis, Emory University, Atlanta, GA, USA, 2020. Available online: https://etd.library.emory.edu/concern/etds/n296x0341?locale=en (accessed on 10 July 2021).
- Kachwaha, S.; Nguyen, P.H.; DeFreese, M.; Avula, R.; Cyriac, S.; Girard, A.; Menon, P. Assessing the Economic Feasibility of Assuring Nutritionally Adequate Diets for Vulnerable Populations in Uttar Pradesh, India: Findings from a “Cost of the Diet” Analysis. Curr. Dev. Nutr. 2020, 4, nzaa169. [Google Scholar] [CrossRef]
- Kehoe, S.H.; Dhurde, V.; Bhaise, S.; Kale, R.; Kumaran, K.; Gelli, A.; Rengalakshmi, R.; Lawrence, W.; Bloom, I.; Sahariah, S.A.; et al. Barriers and facilitators to fruit and vegetable consumption among rural indian women of reproductive age. Food Nutr. Bull. 2019, 40, 87–98. [Google Scholar] [CrossRef]
- Lakshmi, G. Food preferences and taboos during ante-natal period among the tribal women of north coastal Andhra Pradesh. J. Community Nutr. Health 2013, 2, 32. [Google Scholar]
- Mukhopadhyay, S.; Sarkar, A. Pregnancy-related food habits among women of rural Sikkim, India. Public Health Nutr. 2009, 12, 2317–2322. [Google Scholar] [CrossRef] [PubMed]
- Raghunathan, K.; Headey, D.; Herforth, A. Affordability of nutritious diets in rural India. Food Policy 2021, 99, 101982. [Google Scholar] [CrossRef] [PubMed]
- Rammohan, A.; Goli, S.; Singh, D.; Ganguly, D.; Singh, U. Maternal dietary diversity and odds of low birth weight: Empirical findings from India. Women Health 2019, 59, 375–390. [Google Scholar] [CrossRef] [PubMed]
- ROSHNI—ROSHNI-Centre of Women Collectives Led Social Action. Formative Research on Engaging Men & Boys for Advancing Gender Equality in the Swabhimaan Programme; Lady Irwin College: New Delhi, India, 2019. [Google Scholar]
- Sadhu, G.; Prusty, R.K.; Rani, V.; Nigam, S.; Bandhu, A.; Dhakad, R.; Kumar, A.; Mishra, V.K.; Sharif Gautam, S. A Study Report on “Formulation of Evidence-Based and Actionable Dietary Advice for Pregnant and Lactating Women in Rajasthan”; Institute of Health and Management Research: Rajasthan, India, 2017. [Google Scholar]
- Sarkar, A.; Sabharwal, V.; Qualitz, G.; Bader, N. Influence of Social Inequalities on Dietary Diversity and Household Food Insecurity: An In-Depth Nutrition Baseline Survey Conducted in Madhya Pradesh, India. World Rev. Nutr. Diet 2020, 121, 212–220. [Google Scholar] [PubMed]
- Sharma, S.; Akhtar, F.; Kumar Singh, R.; Mehra, S. Dietary patterns and determinants of pregnant and lactating women from marginalized communities in india: A community-based cross-sectional study. Front. Nutr. 2020, 7, 595170. [Google Scholar] [CrossRef]
- OneWorld Foundation India; UNICEF. Forest Lanterns; Penguin Random House India Pvt. Ltd.: Haryana, India, 2017; Available online: https://oneworld.net.in/wp-content/uploads/forest-lanterns.pdf (accessed on 10 July 2021).
- Stephens, C. Nutrition, Biodiversity and Traditional Knowledge. The Malnoursihed Tribal. A Symposium on the Continuing Burden of Hunger and Illness in Our Tribal Communities. 2014. Available online: https://www.india-seminar.com/2014/661/661_carolyn_stephens.htm (accessed on 10 July 2021).
- Sarangi, D.; Trustee, M.; Patra, P. Forests as a Food Producing Habitat. Nourishing Tribals. A Symposium on Nutrition Sensitive Practices in Schedule V States of India. 2016. Available online: https://www.india-seminar.com/2016/681/681_debjeet_sarangi_et_al.htm (accessed on 15 July 2021).
- ICMR; NIN; Abhiyaan, P. Area-Wise Diet Charts Developed for Pregnant Women and Malnourished Pregnant Women in Reproductive Age. 2020. Available online: https://wcd.nic.in/acts/area-wise-diet-charts-developed-pregnant-women-and-malnourished-pregnant-women-reproductive-age (accessed on 15 July 2021).
- Sethi, V.; Tiwari, K.; Sareen, N.; Singh, S.; Mishra, C.; Jagadeeshwar, M.; Sunitha, K.; Kumar, S.V.; de Wagt, A.; Sachdev, H.P.S. Delivering an Integrated Package of Maternal Nutrition Services in Andhra Pradesh and Telangana (India). Food Nutr. Bull. 2019, 40, 393–408. [Google Scholar] [CrossRef]
- National Institute of Nutrition. Assessment of Effect of ‘Anna Amrutha Hastham’ on Nutritional Status of Pregnant Women and Lactating Mothers in the State of Andhra Pradesh; Indian Council of Medical Research: Hyderabad, India, 2016.
- Babu, G.R.; Shapeti, S.S.; Saldanha, N.; Deepa, R.; Prafully, S.; Yamuna, A. Evaluating the Effect of One Full Meal a Day in Pregnant and Lactating Women (FEEL): A Prospective Study; Indian Institute of Public Health; Public Health Foundation of India: Bangaluru, India, 2020. [Google Scholar]
- Gupta, A.; Tiwari, S.K. Probiotic Potential of Lactobacillus plantarum LD1 Isolated from Batter of Dosa, a South Indian Fermented Food. Probiotics Antimicrob. Proteins 2014, 6, 73–81. [Google Scholar] [CrossRef]
- Raghunathan, K.; Chakrabarti, S.; Avula, R.; Kim, S.S. Can conditional cash transfers improve the uptake of nutrition interventions and household food security? Evidence from Odisha’s Mamata scheme. PLoS ONE 2017, 12, e0188952. [Google Scholar] [CrossRef]
- Aaron, G.J.; Sodani, P.R.; Sankar, R.; Fairhurst, J.; Siling, K.; Guevarra, E.; Norris, A.; Myatt, M. Household coverage of fortified staple food commodities in Rajasthan, India. PLoS ONE 2016, 11, e0163176. [Google Scholar] [CrossRef] [PubMed]
- Chakrabarti, S.; Kishore, A.; Raghunathan, K.; Scott, S.P. Impact of subsidized fortified wheat on anaemia in pregnant Indian women. Matern. Child Nutr. 2019, 15, e12669. [Google Scholar] [CrossRef]
- Collison, D.K.; Kekre, P.; Verma, P.; Melgen, S.; Kram, N.; Colton, J.; Blount, W.; Girard, A.W. Acceptability and utility of an innovative feeding toolkit to improve maternal and child dietary practices in Bihar, India. Food Nutr. Bull. 2015, 36, 24–32. [Google Scholar] [CrossRef]
- Garg, A.; Kashyap, S. Effect of counseling on nutritional status during pregnancy. Indian J. Pediatr. 2006, 73, 687–692. [Google Scholar] [CrossRef]
- Nguyen, P.H.; Kachwaha, S.; Tran, L.M.; Avula, R.; Young, M.F.; Ghosh, S.; Sharma, P.K.; Escobar-Alegria, J.; Forissier, T.; Patil, S.; et al. Strengthening nutrition interventions in antenatal care services affects dietary intake, micronutrient intake, gestational weight gain, and breastfeeding in Uttar Pradesh, India: Results of a cluster-randomized program evaluation. J. Nutr. 2021, 151, 2282–2295. [Google Scholar] [CrossRef] [PubMed]
- Shivalli, S.; Srivastava, R.K.; Singh, G.P. Trials of improved practices (TIPs) to enhance the dietary and iron-folate intake during pregnancy—A quasi experimental study among rural pregnant women of Varanasi, India. PLoS ONE 2015, 10, e0137735. [Google Scholar] [CrossRef] [PubMed]
- Daivadanam, M.; Wahlstrom, R.; Ravindran, T.K.S.; Sarma, P.S.; Sivasankaran, S.; Thankappan, K.R. Changing household dietary behaviours through community-based networks: A pragmatic cluster randomized controlled trial in rural Kerala, India. PLoS ONE 2018, 13, e0201877. [Google Scholar] [CrossRef]
- Sethi, V.; Kumar, P.; Wagt, A.D. Development of a maternal service package for mothers of children with severe acute malnutrition admitted to nutrition rehabilitation centres in India. Field Exch. 2019, 59, 24–28. [Google Scholar]
- Beesabathuni, K.; Lingala, S.; Kumari, P. How Eggs and Women Transformed a Malnutrition-Prone Village. 2021. Available online: https://poshan.outlookindia.com/story/poshan-news-how-eggs-transformed-women-and-a-malnutrition-prone-tribal-village/375087 (accessed on 10 July 2021).
- Kadiyala, S.; Harris-Fry, H.; Pradhan, R.; Mohanty, S.; Padhan, S.; Rath, S.; James, P.; Fivian, E.; Koniz-Booher, P.; Nair, N.; et al. Effect of nutrition-sensitive agriculture interventions with participatory videos and women’s group meetings on maternal and child nutritional outcomes in rural Odisha, India (UPAVAN trial): A four-arm, observer-blind, cluster-randomised controlled trial. Lancet Planet Health 2021, 5, e263–e276. [Google Scholar] [CrossRef]
- Moretti, D.; Biebinger, R.; Bruins, M.J.; Hoeft, B.; Kraemer, K. Bioavailability of iron, zinc, folic acid, and vitamin A from fortified maize. Ann. N. Y. Acad. Sci. 2014, 1312, 54–65. [Google Scholar] [CrossRef] [PubMed]
- WHO; FAO. Guidelines on Food Fortification with Micronutrients; World Health Organization; Food and Agriculture Organization of the United Nations: Geneva, Switzerland, 2006. [Google Scholar]
- Choedon, T.; Dinachandra, K.; Sethi, V.; Kumar, P. Screening and management of maternal malnutrition in nutritional rehabilitation centers as a routine service: A feasibility study in kalawati saran children hospital, New Delhi. Indian J. Community Med. 2021, 46, 241–246. [Google Scholar] [PubMed]
- Development Initiatives. Global Nutrition Report 2017: Nourishing the SDGs; Development Initiatives: Bristol, UK, 2017. [Google Scholar]
- National Nutrition Monitoring Bureau. Diet and Nutritional Status of Urban Population in India and Prevalence of Obesity, Hypertension, Diabetes Among Hyperlipidemia in Urban Men and Women. A Brief Report NNMB Urban Nutrition Report; NNMB Technical Report No 27; National Institute of Nutrition; Indian Council of Medical Research: Hyderabad, India, 2017.
- National Institute of Nutrition. Dietary Guidelines for Indians: A Manual; National Institute of Nutrition: Hyderabad, India, 2011.
- Kachwaha, S.R.; Avula, P.; Menon, V.; Sethi, W.; Joe, W.; Laxmaiah, A. Improving Maternal Nutrition in India Through Integrated Hot-Cooked Meal Programs: A Review of Implementation Evidence; International Food Policy Research Institute: New Delhi, India, 2021. [Google Scholar]
- Harris-Fry, H.A.; Paudel, P.; Harrisson, T.; Shrestha, N.; Jha, S.; Beard, B.J.; Copas, A.; Shrestha, B.P.; Manandhar, D.S.; Costello, A.M.L.; et al. Participatory women’s groups with cash transfers can increase dietary diversity and micronutrient adequacy during pregnancy, whereas women’s groups with food transfers can increase equity in intrahousehold energy allocation. J. Nutr. 2018, 148, 1472–1483. [Google Scholar] [CrossRef] [PubMed]
- Olney, D.K.; Talukder, A.; Iannotti, L.L.; Ruel, M.T.; Quinn, V. Assessing impact and impact pathways of a homestead food production program on household and child nutrition in Cambodia. Food Nutr. Bull. 2009, 30, 355–369. [Google Scholar] [CrossRef]
- Nguyen, P.H.; Kim, S.S.; Sanghvi, T.; Mahmud, Z.; Tran, L.M.; Shabnam, S.; Aktar, B.; Haque, R.; Afsana, K.; Frongillo, E.A.; et al. Integrating nutrition interventions into an existing maternal, neonatal, and child health program increased maternal dietary diversity, micronutrient intake, and exclusive breastfeeding practices in Bangladesh: Results of a cluster-randomized program evaluation. J. Nutr. 2017, 147, 2326–2337. [Google Scholar] [PubMed]
- Chilton, S.N.; Burton, J.P.; Reid, G. Inclusion of fermented foods in food guides around the world. Nutrients 2015, 7, 390–404. [Google Scholar] [CrossRef]
- Tamang, J.P. History and culture of indian ethnic fermented foods and beverages. In Ethnic Fermented Foods and Beverages of India: Science History and Culture; Springer: Singapore, 2020; pp. 1–40. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).