Change in Micronutrient Intake among People with Relapsing-Remitting Multiple Sclerosis Adapting the Swank and Wahls Diets: An Analysis of Weighed Food Records
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants and Study Design
2.2. Study Procedures
2.3. Intervention Diets
2.4. Food Records and Analysis
2.5. Statistical Analysis
3. Results
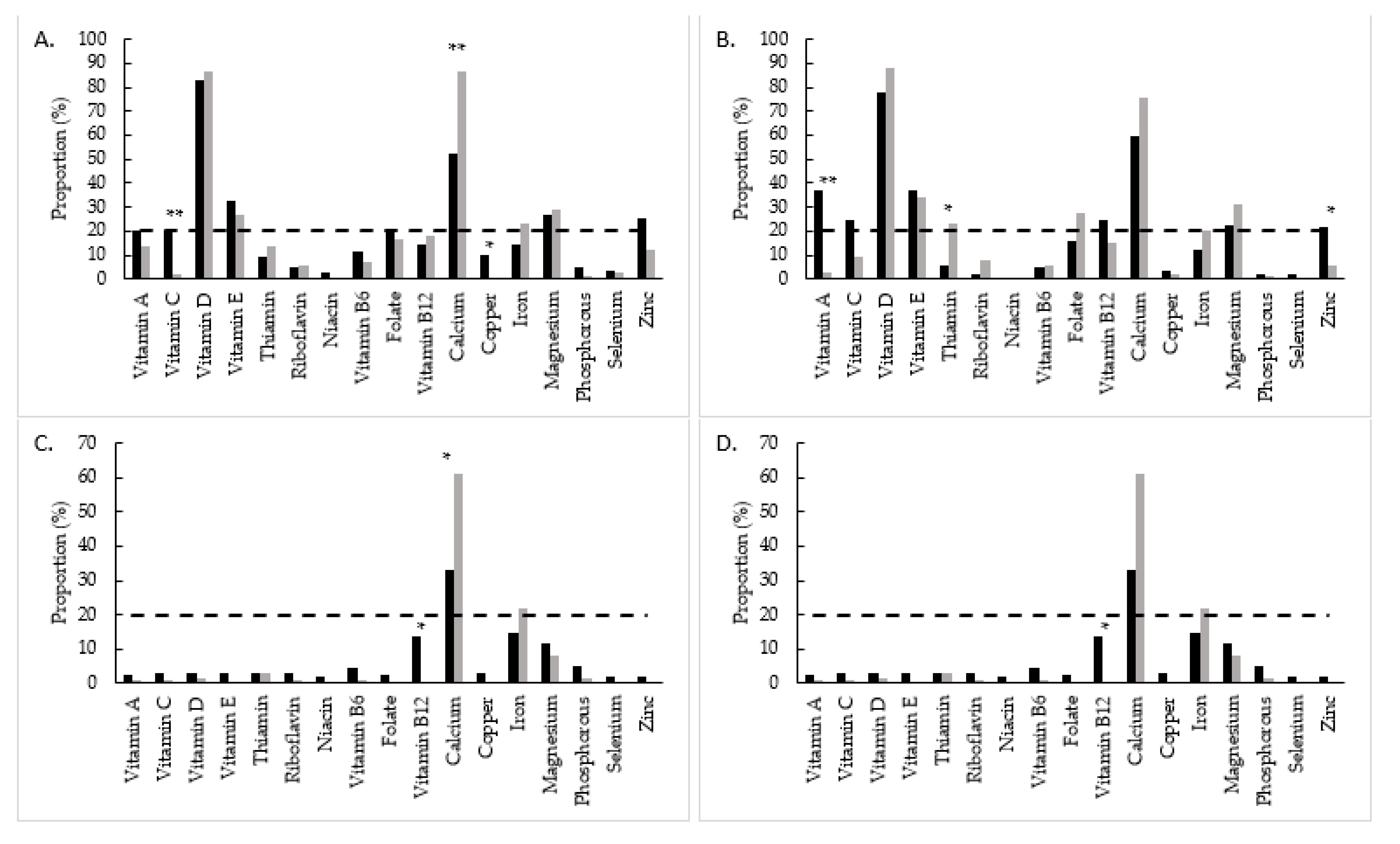
Micronutrient Inadequate Intake
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Trial Registration
References
- Wallin, M.T.; Culpepper, W.J.; Campbell, J.D.; Nelson, L.M.; Langer-Gould, A.; Marrie, R.A.; Cutter, G.R.; Kaye, W.E.; Wagner, L.; Tremlett, H.; et al. The prevalence of MS in the United States: A population-based estimate using health claims data. Neurology 2019, 92, e1029–e1040. [Google Scholar] [CrossRef] [Green Version]
- Fitzgerald, K.C.; Tyry, T.; Salter, A.; Cofield, S.S.; Cutter, G.; Fox, R.J.; Marrie, R.A. A survey of dietary characteristics in a large population of people with multiple sclerosis. Mult. Scler. Relat. Disord. 2018, 22, 12–18. [Google Scholar] [CrossRef] [PubMed]
- Russell, R.D.; Lucas, R.M.; Brennan, V.; Sherriff, J.L.; Begley, A.; Ausimmune Investigator, G.; Black, L.J. Reported Changes in Dietary Behavior Following a First Clinical Diagnosis of Central Nervous System Demyelination. Front. Neurol. 2018, 9, 161. [Google Scholar] [CrossRef] [Green Version]
- Russell, R.D.; Black, L.J.; Sherriff, J.L.; Begley, A. Dietary responses to a multiple sclerosis diagnosis: A qualitative study. Eur. J. Clin. Nutr. 2019, 73, 601–608. [Google Scholar] [CrossRef] [PubMed]
- Beckett, J.M.; Bird, M.L.; Pittaway, J.K.; Ahuja, K.D. Diet and Multiple Sclerosis: Scoping Review of Web-Based Recommendations. Interact. J. Med. Res. 2019, 8, e10050. [Google Scholar] [CrossRef] [PubMed]
- Evans, E.; Levasseur, V.; Cross, A.H.; Piccio, L. An overview of the current state of evidence for the role of specific diets in multiple sclerosis. Mult. Scler. Relat. Disord. 2019, 36, 101393. [Google Scholar] [CrossRef]
- Wahls, T.L.; Chenard, C.A.; Snetselaar, L.G. Review of Two Popular Eating Plans within the Multiple Sclerosis Community: Low Saturated Fat and Modified Paleolithic. Nutrients 2019, 11, 352. [Google Scholar] [CrossRef] [Green Version]
- Swank, R.L. Multiple sclerosis; a correlation of its incidence with dietary fat. Am. J. Med. Sci. 1950, 220, 421–430. [Google Scholar] [CrossRef]
- Swank, R.L. Treatment of multiple sclerosis with low-fat diet. AMA Arch. Neurol. Psychiatry 1953, 69, 91–103. [Google Scholar] [CrossRef]
- Swank, R.L.; Goodwin, J. Review of MS patient survival on a Swank low saturated fat diet. Nutrition 2003, 19, 161–162. [Google Scholar] [CrossRef]
- Swank, R.L. Multiple sclerosis: Twenty years on low fat diet. Arch. Neurol. 1970, 23, 460–474. [Google Scholar] [CrossRef]
- Swank, R.L. Treatment of multiple sclerosis with low-fat diet; results of five and one-half years’ experience. AMA Arch. Neurol. Psychiatry 1955, 73, 631–644. [Google Scholar] [CrossRef]
- Reese, D.; Shivapour, E.T.; Wahls, T.L.; Dudley-Javoroski, S.D.; Shields, R. Neuromuscular electrical stimulation and dietary interventions to reduce oxidative stress in a secondary progressive multiple sclerosis patient leads to marked gains in function: A case report. Cases J. 2009, 2, 7601. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wahls, T.L.; Reese, D.; Kaplan, D.; Darling, W.G. Rehabilitation with neuromuscular electrical stimulation leads to functional gains in ambulation in patients with secondary progressive and primary progressive multiple sclerosis: A case series report. J. Altern Complement. Med. 2010, 16, 1343–1349. [Google Scholar] [CrossRef] [PubMed]
- Wahls, T.L. The seventy percent solution. J. Gen. Intern. Med. 2011, 26, 1215–1216. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bisht, B.; Darling, W.G.; Shivapour, E.T.; Lutgendorf, S.K.; Snetselaar, L.G.; Chenard, C.A.; Wahls, T.L. Multimodal intervention improves fatigue and quality of life in subjects with progressive multiple sclerosis: A pilot study. Degener. Neurol. Neuromuscul. Dis. 2015, 5, 19–35. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Irish, A.K.; Erickson, C.M.; Wahls, T.L.; Snetselaar, L.G.; Darling, W.G. Randomized control trial evaluation of a modified Paleolithic dietary intervention in the treatment of relapsing-remitting multiple sclerosis: A pilot study. Degener. Neurol. Neuromuscul. Dis. 2017, 7, 1–18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, J.E.; Titcomb, T.J.; Bisht, B.; Rubenstein, L.M.; Louison, R.; Wahls, T.L. A Modified MCT-Based Ketogenic Diet Increases Plasma beta-Hydroxybutyrate but Has Less Effect on Fatigue and Quality of Life in People with Multiple Sclerosis Compared to a Modified Paleolithic Diet: A Waitlist-Controlled, Randomized Pilot Study. J. Am. Coll. Nutr. 2020, 40, 13–25. [Google Scholar] [CrossRef] [PubMed]
- Wahls, T.L.; Titcomb, T.J.; Bisht, B.; Ten Eyck, P.; Rubenstein, L.M.; Carr, L.J.; Darling, W.G.; Hoth, K.F.; Kamholz, J.; Snetselaar, L.G. Impact of the Swank and Wahls Elimination Dietary Interventions on Fatigue and Quality of Life in Relapsing-remitting Multiple Sclerosis: The WAVES Randomized Parallel-arm Clinical Trial. Mult. Scler. J. Exp. Transl. Clin. 2021, in press. [Google Scholar]
- Bitarafan, S.; Harirchian, M.H.; Nafissi, S.; Sahraian, M.A.; Togha, M.; Siassi, F.; Saedisomeolia, A.; Alipour, E.; Mohammadpour, N.; Chamary, M.; et al. Dietary intake of nutrients and its correlation with fatigue in multiple sclerosis patients. Iran. J. Neurol. 2014, 13, 28–32. [Google Scholar]
- Bromley, L.; Horvath, P.J.; Bennett, S.E.; Weinstock-Guttman, B.; Ray, A.D. Impact of Nutritional Intake on Function in People with Mild-to-Moderate Multiple Sclerosis. Int. J. MS Care 2019, 21, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chenard, C.A.; Rubenstein, L.M.; Snetselaar, L.G.; Wahls, T.L. Nutrient Composition Comparison between the Low Saturated Fat Swank Diet for Multiple Sclerosis and Healthy U.S.-Style Eating Pattern. Nutrients 2019, 11, 616. [Google Scholar] [CrossRef] [Green Version]
- Chenard, C.A.; Rubenstein, L.M.; Snetselaar, L.G.; Wahls, T.L. Nutrient Composition Comparison between a Modified Paleolithic Diet for Multiple Sclerosis and the Recommended Healthy U.S.-Style Eating Pattern. Nutrients 2019, 11, 537. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wahls, T.; Scott, M.O.; Alshare, Z.; Rubenstein, L.; Darling, W.; Carr, L.; Smith, K.; Chenard, C.A.; LaRocca, N.; Snetselaar, L. Dietary approaches to treat MS-related fatigue: Comparing the modified Paleolithic (Wahls Elimination) and low saturated fat (Swank) diets on perceived fatigue in persons with relapsing-remitting multiple sclerosis: Study protocol for a randomized controlled trial. Trials 2018, 19, 309. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Hopewell, S.; Schulz, K.F.; Montori, V.; Gotzsche, P.C.; Devereaux, P.J.; Elbourne, D.; Egger, M.; Altman, D.G. CONSORT 2010 Explanation and Elaboration: Updated guidelines for reporting parallel group randomised trials. J. Clin. Epidemiol. 2010, 63, e1–e37. [Google Scholar] [CrossRef] [Green Version]
- Polman, C.H.; Reingold, S.C.; Banwell, B.; Clanet, M.; Cohen, J.A.; Filippi, M.; Fujihara, K.; Havrdova, E.; Hutchinson, M.; Kappos, L.; et al. Diagnostic criteria for multiple sclerosis: 2010 revisions to the McDonald criteria. Ann. Neurol. 2011, 69, 292–302. [Google Scholar] [CrossRef] [Green Version]
- Tooze, J.A.; Kipnis, V.; Buckman, D.W.; Carroll, R.J.; Freedman, L.S.; Guenther, P.M.; Krebs-Smith, S.M.; Subar, A.F.; Dodd, K.W. A mixed-effects model approach for estimating the distribution of usual intake of nutrients: The NCI method. Stat. Med. 2010, 29, 2857–2868. [Google Scholar] [CrossRef] [Green Version]
- Institute of Medicine. Dietary Reference Intakes. Applications in Dietary Assessment; National Academy Press: Washington, DC, USA, 2000. [Google Scholar]
- Institute of Medicine. Dietary Reference Intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc. In Dietary Reference Intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc; National Academy Press: Washington, DC, USA, 2001. [Google Scholar]
- Agarwal, S.; Reider, C.; Brooks, J.R.; Fulgoni, V.L., 3rd. Comparison of prevalence of inadequate nutrient intake based on body weight status of adults in the United States: An analysis of NHANES 2001–2008. J. Am. Coll. Nutr. 2015, 34, 126–134. [Google Scholar] [CrossRef]
- Ramsaransing, G.S.; Mellema, S.A.; De Keyser, J. Dietary patterns in clinical subtypes of multiple sclerosis: An exploratory study. Nutr. J. 2009, 8, 36. [Google Scholar] [CrossRef] [Green Version]
- Rosjo, E.; Myhr, K.M.; Loken-Amsrud, K.I.; Bakke, S.J.; Beiske, A.G.; Bjerve, K.S.; Hovdal, H.; Lilleas, F.; Midgard, R.; Pedersen, T.; et al. Increasing serum levels of vitamin A, D and E are associated with alterations of different inflammation markers in patients with multiple sclerosis. J. Neuroimmunol. 2014, 271, 60–65. [Google Scholar] [CrossRef] [Green Version]
- Loken-Amsrud, K.I.; Holmoy, T.; Bakke, S.J.; Beiske, A.G.; Bjerve, K.S.; Bjornara, B.T.; Hovdal, H.; Lilleas, F.; Midgard, R.; Pedersen, T.; et al. Vitamin D and disease activity in multiple sclerosis before and during interferon-beta treatment. Neurology 2012, 79, 267–273. [Google Scholar] [CrossRef]
- Loken-Amsrud, K.I.; Myhr, K.M.; Bakke, S.J.; Beiske, A.G.; Bjerve, K.S.; Bjornara, B.T.; Hovdal, H.; Lilleas, F.; Midgard, R.; Pedersen, T.; et al. Retinol levels are associated with magnetic resonance imaging outcomes in multiple sclerosis. Mult. Scler. 2013, 19, 451–457. [Google Scholar] [CrossRef] [PubMed]
- Loken-Amsrud, K.I.; Myhr, K.M.; Bakke, S.J.; Beiske, A.G.; Bjerve, K.S.; Bjornara, B.T.; Hovdal, H.; Lilleas, F.; Midgard, R.; Pedersen, T.; et al. Alpha-tocopherol and MRI outcomes in multiple sclerosis--association and prediction. PLoS ONE 2013, 8, e54417. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Masullo, L.; Papas, M.A.; Cotugna, N.; Baker, S.; Mahoney, L.; Trabulsi, J. Complementary and alternative medicine use and nutrient intake among individuals with multiple sclerosis in the United States. J. Community Health 2015, 40, 153–160. [Google Scholar] [CrossRef] [PubMed]
- Titcomb, T.J.; Bisht, B.; Moore, D.D., 3rd; Chhonker, Y.S.; Murry, D.J.; Snetselaar, L.G.; Wahls, T.L. Eating Pattern and Nutritional Risks among People with Multiple Sclerosis Following a Modified Paleolithic Diet. Nutrients 2020, 12, 1844. [Google Scholar] [CrossRef] [PubMed]
- Evans, E.; Piccio, L.; Cross, A.H. Use of Vitamins and Dietary Supplements by Patients With Multiple Sclerosis: A Review. JAMA Neurol. 2018, 75, 1013–1021. [Google Scholar] [CrossRef] [PubMed]
- Van der Mei, I.A.; Ponsonby, A.L.; Dwyer, T.; Blizzard, L.; Taylor, B.V.; Kilpatrick, T.; Butzkueven, H.; McMichael, A.J. Vitamin D levels in people with multiple sclerosis and community controls in Tasmania, Australia. J. Neurol. 2007, 254, 581–590. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Swank | Wahls | p-Value 2 |
|---|---|---|---|
| n | 38 | 39 | - |
| Age (years) | 46.9 ± 1.7 | 46.4 ± 1.5 | 0.84 |
| Gender (female) | 35 (92.1) | 32 (82.1) | 0.31 |
| MS duration (years) | 12.1 ± 1.6 | 9.3 ± 1.0 | 0.14 |
| Disease modifying drug use | 0.83 | ||
| None | 13 | 10 | |
| Oral | 11 | 11 | |
| Injectable | 10 | 12 | |
| Infused | 4 | 6 | |
| Race (Caucasian) | 36 (94.7) | 38 (97.4) | 0.99 |
| Education | 0.32 | ||
| High school | 0 (0.0) | 3 (7.7) | - |
| Some college | 12 (31.6) | 10 (25.6) | - |
| 4-year degree | 11 (28.9) | 8 (20.5) | - |
| Advanced degree | 15 (39.5) | 18 (46.2) | - |
| Smoking status | 0.13 | ||
| Never | 29 (76.3) | 23 (59.0) | - |
| Former | 3 (7.9) | 2 (5.1) | - |
| Current | 6 (15.8) | 14 (35.9) | - |
| Alcohol drinks per month 3 | 0.99 | ||
| None | 6 (15.8) | 7 (17.9) | - |
| Within recommendations | 29 (76.3) | 29 (74.4) | - |
| Above recommendations | 3 (7.9) | 3 (7.7) | - |
| BMI (kg/m2) | 27.6 ± 0.9 | 30.2 ± 1.3 | 0.11 |
| Diet Component | Swank | Wahls |
|---|---|---|
| Energy, kilocalories | Adjust to meet energy needs | Adjust to achieve and maintain a healthy body mass index |
| Fruits and vegetables, cup equivalents per day | 2+ fruit 2+ vegetables | 2–3+ dark green leafy vegetables 2–3+ sulfur-rich vegetables 2–3+ deeply colored fruits and vegetables White fruits and vegetables limited Nightshade vegetables/spices avoided |
| Protein, ounces per day | Adequate in quantity and quality - Beef, pork, organ meat, egg yolks, and dark meat poultry and skin avoided - White meat poultry, white fish, shellfish, and egg whites as desired - ≤1.75 fatty fish - Nuts and legumes allowed if low in saturated fat | 6–12+ meat/fish - Beef, pork, poultry, game, fish, shellfish, organ meat as desired - Eggs and legumes not allowed - 16 fatty fish per week - 12 organ meat per week - 4 nuts, soaked and rinsed |
| Grains, ounce equivalents per day | 4, whole grains preferred | Not allowed |
| Dairy, cup equivalents per day | 2 if <1% dairy fat | Cow, goat, mare, soy not allowed |
| Fats | - ≤15 g saturated fat per day - 20–50 g oil per day | As desired for satiety and weight maintenance - Clarified butter, animal fats, coconut oil, avocado oil, extra virgin olive oil, sesame oil, sunflower oil as desired - ≤30 g flax, hemp, and walnut oil per day - All other fats and oils not allowed |
| Sweeteners | Minimal for taste | ≤1tsp allowed sweeteners per day |
| Salt | As desired | As desired |
| Alcohol, standard drinks per day | 1 wine or mixed drink in evening | ≤1 for women, ≤2 for men |
| Caffeine | ≤3 cups caffeinated beverages per day | As desired |
| Seaweed, algae, nutritional yeast, fermented foods | No recommendation, must be low in saturated fat | 1 serving each per day |
| Swank | Wahls | |||||
|---|---|---|---|---|---|---|
| Micronutrient | Baseline | 12 Weeks | 24 Weeks | Baseline | 12 Weeks | 24 Weeks |
| Vitamins | ||||||
| Vitamin A | 19.3 | 2.2 * | 1.4 * | 30.9 | 0.8 * | 0.0 * |
| Vitamin C | 28.6 | 2.9 * | 2.6 * | 29.6 | 0.7 * | 1.4 * |
| Vitamin D | 27.7 | 2.8 * | 0.7 * | 16.9 | 1.0 * | 0.3 * |
| Vitamin E | 31.9 | 2.5 * | 0.5 * | 38.7 | 0.3 * | 0.4 * |
| Thiamin | 9.6 | 2.8 | 0.0 * | 15.9 | 2.8 * | 0.8 * |
| Riboflavin | 6.2 | 2.6 | 0.0 | 12.5 | 0.8 * | 0.2 * |
| Niacin | 2.7 | 1.6 | 0.0 | 5.9 | 0.0 | 0.0 |
| Vitamin B6 | 17.1 | 4.2 * | 3.9 * | 24.3 | 0.8 * | 3.9 * |
| Folate | 9.9 | 2.1 | 0.5 | 19.7 | 0.3 * | 0.2 * |
| Vitamin B12 | 14.0 | 13.4 | 12.6 | 28.6 | 0.1 * | 0.1 * |
| Minerals | ||||||
| Calcium | 33.7 | 32.6 | 38.1 | 35.9 | 60.7 * | 55.4 * |
| Copper | 12.6 | 2.7 | 0.2 * | 7.8 | 0.0 | 0.1 |
| Iron | 11.5 | 14.4 | 11.4 | 11.5 | 21.4 | 19.2 |
| Magnesium | 32.2 | 11.5 * | 6.5 * | 44.9 | 7.9 * | 12.8 * |
| Phosphorous | 3.4 | 4.6 | 1.7 | 5.5 | 1.3 | 1.3 |
| Selenium | 3.4 | 1.7 | 0.1 | 6.2 | 0.0 | 0.0 |
| Zinc | 14.6 | 1.9 * | 0.4 * | 19.5 | 0.0 * | 0.2 * |
| Swank | Wahls | |||||
|---|---|---|---|---|---|---|
| Micronutrient | Baseline | 12 Weeks | 24 Weeks | Baseline | 12 Weeks | 24 Weeks |
| Vitamins | ||||||
| Vitamin A | 20.7 | 19.8 | 36.6 *,** | 44.3 | 13.1 * | 2.3 * |
| Vitamin C | 44.6 | 19.8 * | 24.1 * | 50.0 | 1.5 * | 9.3 *,** |
| Vitamin D | 96.3 | 82.3 * | 77.6 * | 99.9 | 86.6 * | 87.8 * |
| Vitamin E | 50.1 | 32.3 * | 37.0 | 56.1 | 26.7 * | 34.0 * |
| Thiamin | 11.5 | 8.7 | 5.2 | 5.7 | 13.6 * | 22.8 * |
| Riboflavin | 5.3 | 4.5 | 1.9 | 4.5 | 5.3 | 7.8 |
| Niacin | 2.8 | 2.4 | 0.0 | 5.3 | 0.0 | 0.0 |
| Vitamin B6 | 23.1 | 11.3 | 4.8 * | 15.3 | 7.1 | 5.7 |
| Folate | 21.6 | 20.9 | 15.9 | 26.4 | 16.1 | 26.9 |
| Vitamin B12 | 14.0 | 13.9 | 24.3 | 5.3 | 17.4 * | 14.6 * |
| Minerals | ||||||
| Calcium | 47.4 | 51.7 | 59.5 | 54.7 | 86.5 * | 75.5 * |
| Copper | 8.7 | 9.9 | 3.4 | 6.4 | 0.1 | 1.4 ** |
| Iron | 12.6 | 14.4 | 11.7 | 18.3 | 23.0 | 19.7 |
| Magnesium | 37.7 | 26.7 | 22.2 | 50.8 | 28.5 * | 31.1 * |
| Phosphorous | 3.5 | 4.7 | 1.8 | 5.6 | 1.3 | 1.3 |
| Selenium | 2.7 | 2.9 | 1.8 | 6.3 | 2.3 | 0.3 |
| Zinc | 17.4 | 25.2 | 21.7 | 12.5 | 11.8 | 5.0 |
| Swank | Wahls | |||||
|---|---|---|---|---|---|---|
| Micronutrient | Baseline | 12 Weeks | 24 Weeks | Baseline | 12 Weeks | 24 Weeks |
| Vitamins | ||||||
| Vitamin A | 1.2 | 0.0 | 0.0 | 0.1 | 0.1 | 0.1 |
| Vitamin C | 0.0 | 0.0 | 0.0 | 4.6 | 5.5 | 2.5 |
| Vitamin D | 20.8 | 71.9 * | 55.4 *,** | 33.9 | 72.2 * | 76.4 * |
| Vitamin E | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Niacin | 5.5 | 44.8 * | 44.8 * | 8.6 | 30.6 * | 6.5 ** |
| Vitamin B6 | 1.9 | 0.0 | 0.0 | 2.8 | 2.8 | 2.5 |
| Folate | 4.5 | 9.7 | 9.8 | 0.3 | 0.0 | 0.0 |
| Minerals | ||||||
| Calcium | 1.1 | 1.0 | 3.0 | 0.0 | 0.0 | 0.4 |
| Copper | 0.0 | 0.0 | 0.0 | 0.0 | 0.5 | 0.0 |
| Iron | 4.9 | 2.9 | 6.2 | 9.3 | 0.1 | 0.1 |
| Magnesium | 2.6 | 2.6 | 10.7 *,** | 0.9 | 0.2 | 0.3 |
| Phosphorous | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Selenium | 0.0 | 0.1 | 0.1 | 0.0 | 0.0 | 0.0 |
| Zinc | 4.2 | 0.3 | 4.4 ** | 0.4 | 0.0 | 1.4 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Titcomb, T.J.; Brooks, L.; Smith, K.L.; Ten Eyck, P.; Rubenstein, L.M.; Wahls, T.L.; Snetselaar, L.G. Change in Micronutrient Intake among People with Relapsing-Remitting Multiple Sclerosis Adapting the Swank and Wahls Diets: An Analysis of Weighed Food Records. Nutrients 2021, 13, 3507. https://doi.org/10.3390/nu13103507
Titcomb TJ, Brooks L, Smith KL, Ten Eyck P, Rubenstein LM, Wahls TL, Snetselaar LG. Change in Micronutrient Intake among People with Relapsing-Remitting Multiple Sclerosis Adapting the Swank and Wahls Diets: An Analysis of Weighed Food Records. Nutrients. 2021; 13(10):3507. https://doi.org/10.3390/nu13103507
Chicago/Turabian StyleTitcomb, Tyler J., Lisa Brooks, Karen L. Smith, Patrick Ten Eyck, Linda M. Rubenstein, Terry L. Wahls, and Linda G. Snetselaar. 2021. "Change in Micronutrient Intake among People with Relapsing-Remitting Multiple Sclerosis Adapting the Swank and Wahls Diets: An Analysis of Weighed Food Records" Nutrients 13, no. 10: 3507. https://doi.org/10.3390/nu13103507
APA StyleTitcomb, T. J., Brooks, L., Smith, K. L., Ten Eyck, P., Rubenstein, L. M., Wahls, T. L., & Snetselaar, L. G. (2021). Change in Micronutrient Intake among People with Relapsing-Remitting Multiple Sclerosis Adapting the Swank and Wahls Diets: An Analysis of Weighed Food Records. Nutrients, 13(10), 3507. https://doi.org/10.3390/nu13103507






