Body Composition Changes after a Weight Loss Intervention: A 3-Year Follow-Up Study
Abstract
1. Introduction
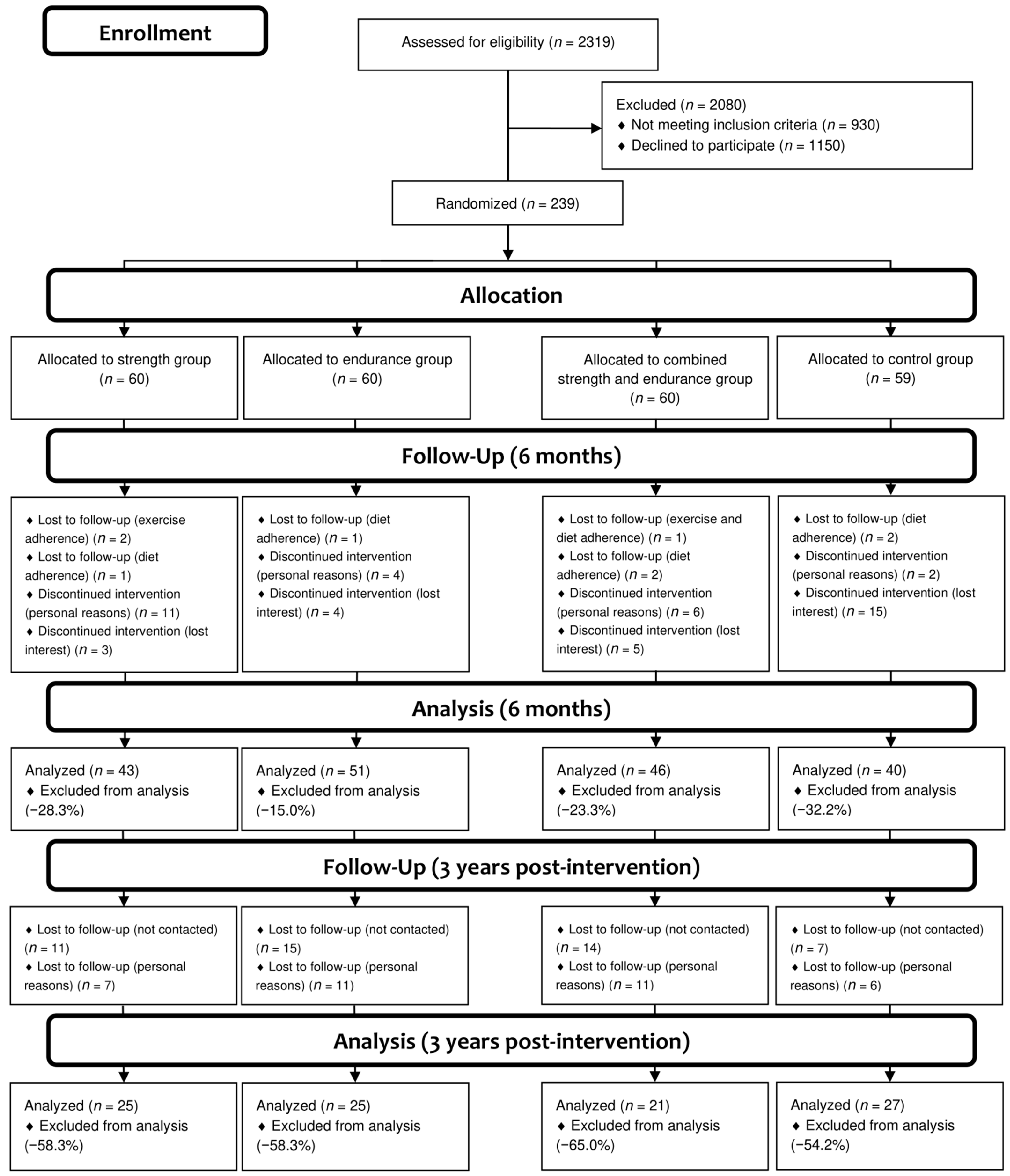
2. Materials and Methods
2.1. Design
2.2. Patient and Public Involvement
2.3. Procedures
2.4. Diet Intervention
2.5. Exercise Intervention
2.6. Control Group
2.7. Outcome Measures
2.8. Primary Outcomes
2.9. Secondary Outcomes
2.10. Statistical Analyses
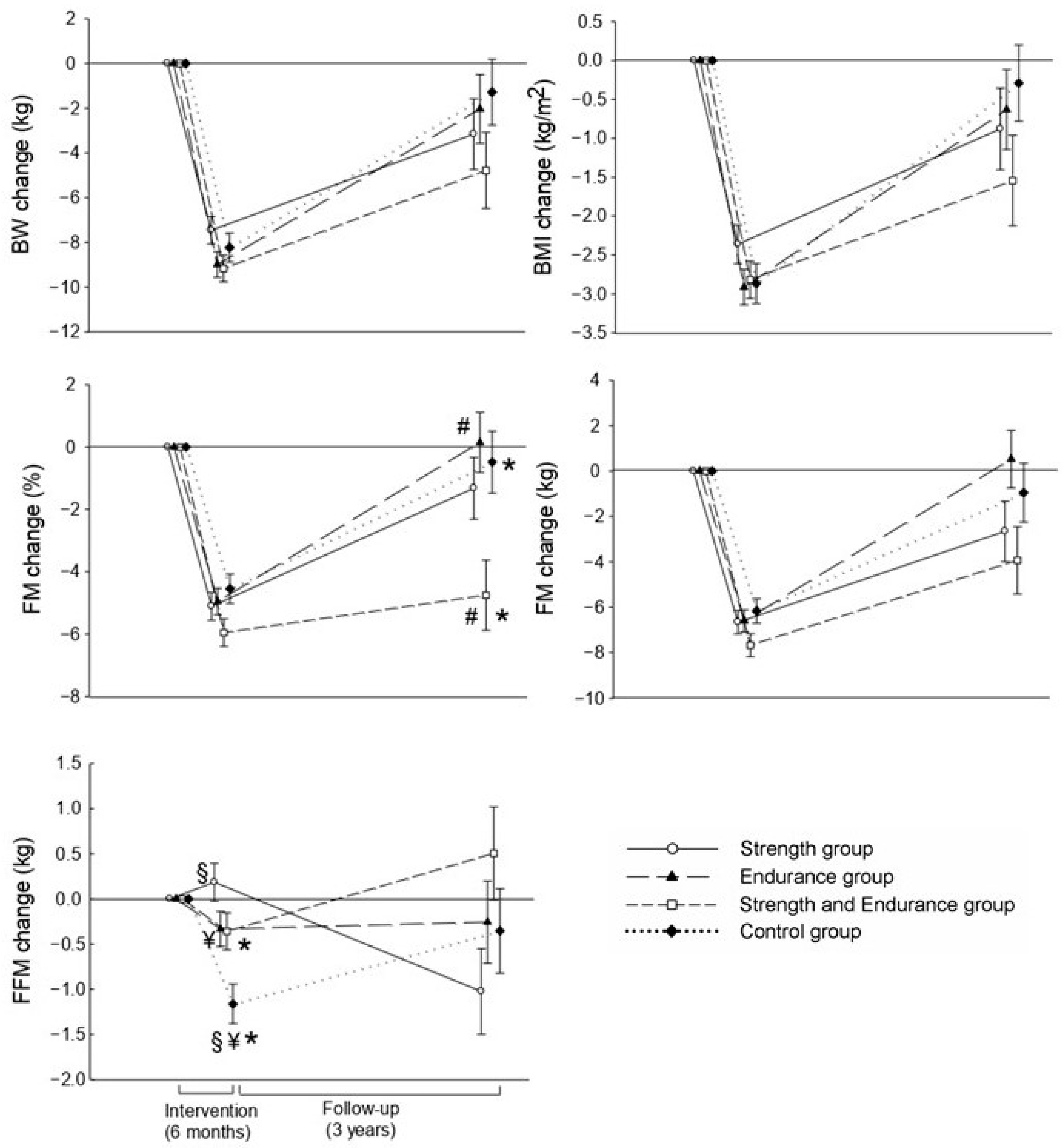
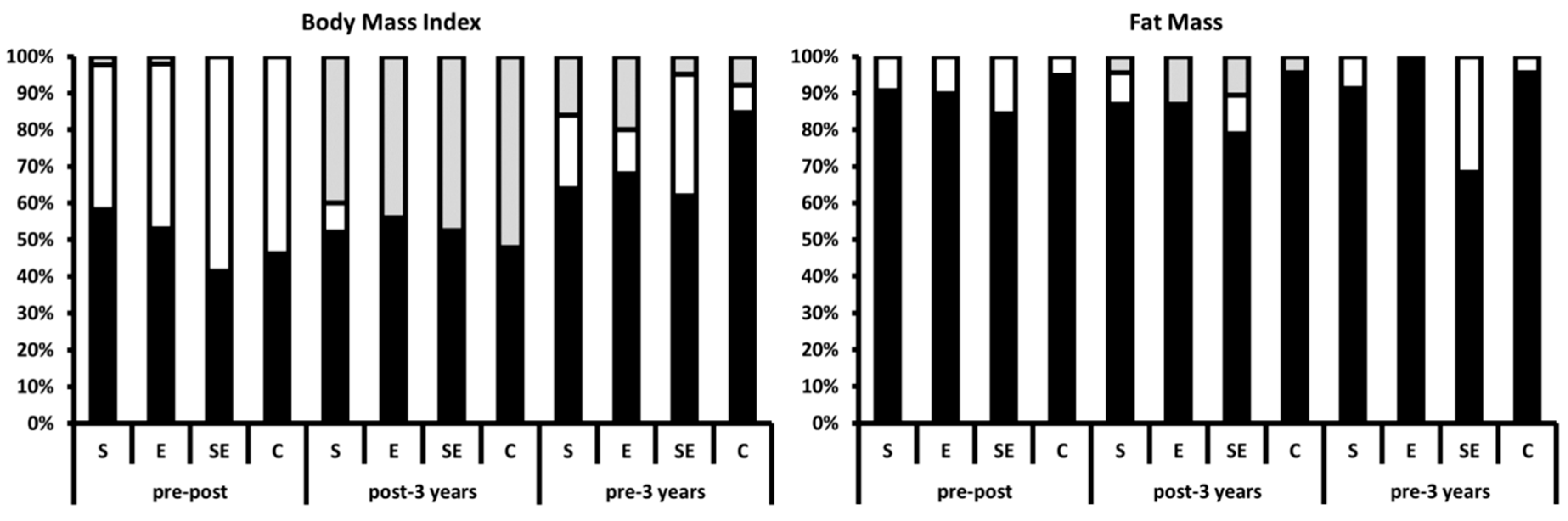
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ostendorf, D.M.; Caldwell, A.; Creasy, S. Physical Activity Energy Expenditure and Total Daily Energy Expenditure in Successful Weight Loss Maintainers. Obesity 2019, 27, 496–504. [Google Scholar] [CrossRef] [PubMed]
- Leung, W.Y.; Chan, R.S.M.; Sea, M.M.M.; Woo, J. An Overview of Factors Associated with Adherence to Lifestyle Modification Programs for Weight Management in Adults. Int. J. Environ. Res. Public Health 2017, 14, 922. [Google Scholar] [CrossRef] [PubMed]
- Franz, M.J.; VanWormer, J.J.; Crain, A.L.; Boucher, J.L.; Histon, T.; Caplan, W.; Bowman, J.D.; Pronk, N.P. Weight-loss outcomes: A systematic review and meta-analysis of weight-loss clinical trials with a minimum 1-year follow-up. J. Am. Diet. Assoc. 2007, 107, 1755–1767. [Google Scholar] [CrossRef] [PubMed]
- Curioni, C.; Lourenco, P.M. Long-term weight loss after diet and exercise: A systematic review. Int. J. Obes. 2005, 29, 1168–1174. [Google Scholar] [CrossRef] [PubMed]
- Quinn, D.M.; Puhl, R.M.; Reinka, M.A. Trying again (and again): Weight cycling and depressive symptoms in U.S. adults. PLoS ONE 2020, 15, e0239004. [Google Scholar] [CrossRef]
- Tsigos, C.; Hainer, V.; Basdevant, A.; Finer, N.; Fried, M.; Mathus-Vliegen, E.; Micic, D.; Maislos, M.; Roman, G.; Schutz, Y.; et al. Management of obesity in adults: European clinical practice guidelines. Obes. Facts 2008, 1, 106–116. [Google Scholar] [CrossRef]
- Clark, J.E. Diet, exercise or diet with exercise: Comparing the effectiveness of treatment options for weight-loss and changes in fitness for adults (18–65 years old) who are overfat, or obese; systematic review and meta-analysis. J. Diabetes Metab. Disord. 2015, 14, 31. [Google Scholar] [CrossRef]
- Hunter, G.R.; Brock, D.W.; Byrne, N.M.; Chandler-Laney, P.C.; Del Corral, P.; Gower, B.A. Exercise Training Prevents Regain of Visceral Fat for 1 Year Following Weight Loss. Obesity 2010, 18, 690–695. [Google Scholar] [CrossRef]
- Zapico, A.G.; Benito, P.J.; González-Gross, M.; Peinado, A.B.; Morencos, E.; Romero, B.; Rojo-Tirado, M.A.; Cupeiro, R.; Szendrei, B.; Butragueño, J.; et al. Nutrition and physical activity programs for obesity treatment (PRONAF study): Methodological approach of the project. BMC Public Health 2012, 12, 1100. [Google Scholar] [CrossRef]
- Acharya, S.D.; Elci, O.U.; Sereika, S.M.; Music, E.; Styn, M.A.; Turk, M.W.; Burke, L.E. Adherence to a behavioral weight loss treatment program enhances weight loss and improvements in biomarkers. Patient Prefer. Adherence 2009, 3, 151–160. [Google Scholar] [CrossRef]
- Spanish Society of Community Nutrition (SENC). Healthy Nutrition Guide; Everest-SENC: Madrid, Spain, 2004. [Google Scholar]
- Wycherley, T.P.; Moran, L.J.; Clifton, P.M.; Noakes, M.; Brinkworth, G.D. Effects of energy-restricted high-protein, low-fat compared with standard-protein, low-fat diets: A meta-analysis of randomized controlled trials. Am. J. Clin. Nutr. 2012, 96, 1281–1298. [Google Scholar] [CrossRef] [PubMed]
- Donnelly, J.E.; Blair, S.N.; Jakicic, J.M.; Manore, M.M.; Rankin, J.W.; Smith, B.K. Appropriate Physical Activity Intervention Strategies for Weight Loss and Prevention of Weight Regain for Adults. Med. Sci. Sport Exerc. 2009, 41, 459–471. [Google Scholar] [CrossRef] [PubMed]
- Okorodudu, D.O.; Jumean, M.F.; Montori, V.M.; Romero-Corral, A.; Somers, V.K.; Erwin, P.J.; Lopez-Jimenez, F.D. Diagnostic performance of body mass index to identify obesity as defined by body adiposity: A systematic review and meta-analysis. Int. J. Obes. 2010, 34, 791–799. [Google Scholar] [CrossRef] [PubMed]
- Wing, R.R.; Hill, J.O. Successful Weight Loss Maintenance. Annu. Rev. Nutr. 2001, 21, 323–341. [Google Scholar] [CrossRef] [PubMed]
- Milsom, V.; Ross, K.; Perri, M. Successful long-term weight loss maintenance in a rural population. Clin. Interv. Aging 2011, 1, 303. [Google Scholar] [CrossRef]
- Rojo-Tirado, M.A.; Benito, P.J.; Atienza, D.; Rincón, E.; Calderón, F.J. Effects of age, sex, and treatment on weight-loss dynamics in overweight people. Appl. Physiol. Nutr. Metab. 2013, 38, 967–976. [Google Scholar] [CrossRef]
- Magkos, F. On adaptive thermogenesis: Just another weight-loss tale? Am. J. Clin. Nutr. 2020, 112, 1157–1159. [Google Scholar] [CrossRef]
- Santarpia, L.; Contaldo, F.; Pasanisi, F. Body composition changes after weight-loss interventions for overweight and obesity. Clin. Nutr. 2013, 32, 157–161. [Google Scholar] [CrossRef]
- Martins, C.; Gower, B.A.; Hill, J.O.; Hunter, G.R. Metabolic adaptation is not a major barrier to weight-loss maintenance. Am. J. Clin. Nutr. 2020, 112, 558–565. [Google Scholar] [CrossRef]
- Melby, C.; Paris, H.; Foright, R.; Peth, J. Attenuating the Biologic Drive for Weight Regain Following Weight Loss: Must What Goes Down Always Go Back Up? Nutrients 2017, 9, 468. [Google Scholar] [CrossRef]
- Colleluori, G.; Aguirre, L.; Phadnis, U.; Fowler, K.; Armamento-Villareal, R.; Sun, Z.; Brunetti, L.; Hyoung Park, J.; Abraham Kaipparettu, B.; Putluri, N.; et al. Aerobic Plus Resistance Exercise in Obese Older Adults Improves Muscle Protein Synthesis and Preserves Myocellular Quality Despite Weight Loss. Cell Metab. 2019, 30, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Hwaung, P.; Bosy-Westphal, A.; Muller, M.J.; Geisler, C.; Heo, M.; Thomas, D.M.; Kennedy, S.; Heymsfield, S. Obesity Tissue: Composition, Energy Expenditure, and Energy Content in Adult Humans. Obesity 2019, 27, oby.22557. [Google Scholar] [CrossRef] [PubMed]
- Heymsfield, S.B.; Peterson, C.M.; Bourgeois, B.; Thomas, D.M.; Gallagher, D.; Strauss, B.; Müller, M.J.; Bosy-Westphal, A.S. Human energy expenditure: Advances in organ-tissue prediction models. Obes. Rev. 2018, 19, 1177–1188. [Google Scholar] [CrossRef] [PubMed]
- Sillanpaa, E.; Laaksonen, D.E.; Hakkinen, A.; Karavirta, L.; Jensen, B.; Kraemer, W.J.; Nyman, K.; Hakkinen, K. Body composition, fitness, and metabolic health during strength and endurance training and their combination in middle-aged and older women. Eur. J. Appl. Physiol. 2009, 106, 285–296. [Google Scholar] [CrossRef]
- Benito, P.J.; Alvarez-Sanchez, M.; Diaz, V.; Morencos, E.; Peinado, A.B.; Cupeiro, R.; Maffulli, N.P. Cardiovascular Fitness and Energy Expenditure Response during a Combined Aerobic and Circuit Weight Training Protocol. PLoS ONE 2016, 11, e0164349. [Google Scholar] [CrossRef]
- Reyes, N.R.; Oliver, T.L.; Klotz, A.A.; Lagrotte, C.A.; Vander Veur, S.S.; Virus, A.; Bailer, B.A.; Foster, G. Similarities and differences between weight loss maintainers and regainers: A qualitative analysis. J. Acad. Nutr. Diet. 2012, 112, 499–505. [Google Scholar] [CrossRef]
- Xu, S.; Zhang, J.; Dong, Y.; Chen, R.; Xu, W.; Tan, Z.; Gao, L.; Shang, L. The PROMOTE study (High-protein and resistance-training combination in overweight and obesity) for short-term weight loss and long-term weight maintenance for Chinese people: A protocol for a pilot randomized controlled trial. Trials 2020, 21, 47. [Google Scholar] [CrossRef]
- Wing, R.R.; Phelan, S. Long-term weight loss maintenance. Am. J. Clin. Nutr. 2005, 82, 222S–225S. [Google Scholar] [CrossRef]
- Perri, M.G. Effects of behavioral treatment on long-term weight loss: Lessons learned from the look AHEAD trial. Obesity 2014, 22, 3–4. [Google Scholar] [CrossRef]
- Jakicic, J.M.; Marcus, B.H.; Lang, W.; Janney, C. Effect of exercise on 24-month weight loss maintenance in overweight women. Arch. Intern. Med. 2008, 168, 1550–1560. [Google Scholar] [CrossRef]
- Jakicic, J.M.; Winters, C.; Lang, W.; Wing, R.R. Effects of Intermittent Exercise and Use of Home Exercise Equipment on Adherence, Weight Loss, and Fitness in Overweight Women. JAMA 1999, 282, 1554. [Google Scholar] [CrossRef] [PubMed]
- Melin, I.; Reynisdottir, S.; Berglund, L.; Zamfir, M.; Karlström, B. Conservative treatment of obesity in an academic obesity unit. Long-term outcome and drop-out. Eat. Weight Disord. Stud. Anorex. Bulim. Obes. 2006, 11, 22–30. [Google Scholar] [CrossRef] [PubMed]
| Group | Pre (95% CI) | Post (95% CI) | 3 Years (95% CI) | p-Group | η2 | p-Time | η2 | p-Interaction | η2 | |
|---|---|---|---|---|---|---|---|---|---|---|
| Body Weight (kg) | S | 92.3 (2.0) (88.3–96.3) | 83.7 (2.0) (79.8–87.65) | 89.1 (2.5) (84.1–94.1) | 0.019 | 0.102 | 0.139 | 0.024 | 0.435 | 0.029 |
| E | 85.9 (2.0) (81.8–89.9) | 77.0 (2.0) (73.0–80.9) | 83.8 (2.5) (78.8–88.9) | |||||||
| SE | 83.3 (2.2) (79.0–87.7) | 74.4 (2.2) (70.1–78.7) | 78.6 (2.7) (73.1–84.1) | |||||||
| C | 86.8 (1.9) (82.9–90.6) | 79.0 (1.9) (75.2–82.7) | 85.5 (2.4) (80.7–90.3) | |||||||
| Body Mass Index (kg/m2) | S | 31.6 (0.5) (30.6–32.6) | 29.0 (0.5) (27.9–30.0) | 30.7 (0.7) (29.3–32.1) | 0.002 | 0.150 | 0.102 | 0.029 | 0.382 | 0.033 |
| E | 30.4 (0.5) (29.5–31.4) | 27.3 (0.5) (26.3–28.4) | 29.8 (0.7) (28.4–31.2) | |||||||
| SE | 29.0 (0.5) (27.9–30.0) | 25.9 (0.6) (24.7–27.1) | 27.4 (0.8) (25.9–28.9) | |||||||
| C | 30.7 (0.5) (29.8–31.6) | 28.1 (0.5) (27.1–29.1) | 30.4 (0.7) (29.1–31.8) | |||||||
| Fat Mass (%) | S | 41.5 (0.9) (39.8–43.3) | 36.1 † (1.0) (34.0–38.1) | 40.1 § (1.3) (37.6–42.7) | 0.001 | 0.187 | 0.586 | 0.004 | 0.017 | 0.116 |
| E | 40.5 (0.9) (38.7–42.3) | 35.2 † (1.0) (33.1–37.2) | 40.6 § (1.3) (38.1–43.1) | |||||||
| SE | 38.1 (1.0) (36.1–40.0) | 31.0 ¶,◊,#,† (1.1) (28.8–33.3) | 33.6 ¶,◊,#,¥ (1.4) (30.8–36.3) | |||||||
| C | 41.5 (0.9) (39.7–43.2) | 36.6 † (1.0) (34.5–38.6) | 40.9 § (1.3) (38.4–43.4) | |||||||
| Fat Mass (kg) | S | 36.3 (1.3) (33.8–38.9) | 28.7 (1.3) (26.1–31.2) | 33.9 (1.9) (30.1–37.6) | 0.005 | 0.144 | 0.282 | 0.015 | 0.238 | 0.047 |
| E | 33.0 (1.3) (30.4–35.5) | 26.2 (1.3) (23.7–28.8) | 33.4 (1.9) (29.6–37.1) | |||||||
| SE | 29.9 (1.4) (27.1–32.7) | 22.0 (1.4) (19.2–24.9) | 25.8 (2.1) (21.7–29.9) | |||||||
| C | 34.0 (1.3) (31.5–36.6) | 27.8 (1.3) (25.2–30.3) | 33.1 (1.9) (29.4–36.8) | |||||||
| Fat-Free Mass (kg) | S | 51.7 (1.1) (49.5–53.8) | 51.5 (1.1) (49.3–53.7) | 50.7 (1.2) (48.3–53.1) | 0.198 | 0.055 | <0.001 | 0.144 | 0.205 | 0.054 |
| E | 48.7 (1.1) (46.6–50.9) | 48.5 (1.1) (46.3–50.7) | 48.3 (1.2) (45.9–50.7) | |||||||
| SE | 49.1 (1.2) (46.7–51.5) | 49.1 (1.2) (46.6–51.5) | 49.6 (1.3) (47.0–52.3) | |||||||
| C | 48.5 (1.1) (46.4–50.7) | 47.7 (1.1) (45.4–49.9) | 48.1 (1.2) (45.7–50.5) |
| Pre | Post | 3 Years | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Group | Freq. (%) | Mean (SD) | Freq. (%) | Mean (SD) | Freq. (%) | Mean (SD) | ||||||||
| Body Mass Index (kg/m2) | Normal Weight (20–24.9) | S | - | - | 2 | (7.4) | 23.7 | (0.3) | 2 | (18.2) | 24.2 | (0.5) | ||
| E | - | - | 6 | (22.2) | 23.5 | (0.8) | - | - | ||||||
| SE | - | - | 13 | (48.2) | 23.9 | (0.7) | 7 | (63.6) | 23.6 | (1.2) | ||||
| C | - | - | 6 | (22.2) | 23.6 | (1.2) | 2 | (18.2) | 24.3 | (0.6) | ||||
| Overweight (25–29.9) | S | 21 | (23.9) | 28.8 | (1.1) | 30 | (27.3) | 27.7 | (1.2) | 9 | (23.6) | 28.2 | (1.1) | |
| E | 26 | (29.5) | 28.4 | (1.3) | 36 | (32.7) | 27.3 | (1.4) | 13 | (34.2) | 27.5 | (1.1) | ||
| SE | 23 | (26.1) | 27.8 | (1.2) | 20 | (18.2) | 27.3 | (1.4) | 8 | (21.1) | 27.3 | (1.2) | ||
| C | 18 | (20.5) | 28.3 | (1.3) | 24 | (21.8) | 27.4 | (1.1) | 8 | (21.1) | 27.9 | (1.5) | ||
| Obese (30–34.9) | S | 21 | (23.1) | 32.5 | (1.6) | 9 | (24.3) | 31.9 | (1.9) | 14 | (29.2) | 33.2 | (2.1) | |
| E | 25 | (27.5) | 32.4 | (1.8) | 9 | (24.3) | 31.2 | (0.8) | 12 | (25.0) | 32.5 | (3.1) | ||
| SE | 23 | (25.3) | 32.9 | (2.0) | 11 | (29.7) | 32.5 | (1.9) | 6 | (12.5) | 32.0 | (1.7) | ||
| C | 22 | (24.1) | 32.5 | (1.7) | 8 | (21.7) | 32.2 | (2.3) | 16 | (33.3) | 32.8 | (2.3) | ||
| Fat Mass (%) | Normal Fat (♂ < 25%; ♀ < 30%) | S | - | - | 4 | (22.2) | 22.0 | (1.7) | 2 | (22.2) | 22.9 | (0.9) | ||
| E | - | - | 5 | (27.8) | 24.4 | (0.3) | - | - | ||||||
| SE | - | - | 7 | (38.9) | 21.7 | (3.6) | 6 | (66.7) | 19.2 | (5.8) | ||||
| C | - | - | 2 | (11.1) | 22.5 | (2.1) | 1 | (11.1) | 23.9 | |||||
| Overfat (♂ < 25%; ♀ < 30%) | S | 43 | (23.9) | 41.2 | (6.2) | 39 | (24.7) | 37.5 | (5.7) | 21 | (26.3) | 42.1 | (5.9) | |
| E | 51 | (28.3) | 41.3 | (6.0) | 44 | (27.8) | 37.8 | (5.6) | 24 | (30.0) | 40.0 | (7.4) | ||
| SE | 46 | (25.6) | 40.5 | (7.3) | 38 | (24.1) | 36.7 | (7.2) | 13 | (16.3) | 38.0 | (7.9) | ||
| C | 40 | (22.2) | 41.2 | (5.4) | 37 | (23.4) | 37.2 | (5.8) | 22 | (27.4) | 43.0 | (6.0) | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rojo-Tirado, M.A.; Benito, P.J.; Ruiz, J.R.; Ortega, F.B.; Romero-Moraleda, B.; Butragueño, J.; Bermejo, L.M.; Castro, E.A.; Gómez-Candela, C. Body Composition Changes after a Weight Loss Intervention: A 3-Year Follow-Up Study. Nutrients 2021, 13, 164. https://doi.org/10.3390/nu13010164
Rojo-Tirado MA, Benito PJ, Ruiz JR, Ortega FB, Romero-Moraleda B, Butragueño J, Bermejo LM, Castro EA, Gómez-Candela C. Body Composition Changes after a Weight Loss Intervention: A 3-Year Follow-Up Study. Nutrients. 2021; 13(1):164. https://doi.org/10.3390/nu13010164
Chicago/Turabian StyleRojo-Tirado, Miguel A., Pedro J. Benito, Jonatan R. Ruiz, Francisco B. Ortega, Blanca Romero-Moraleda, Javier Butragueño, Laura M. Bermejo, Eliane A. Castro, and Carmen Gómez-Candela. 2021. "Body Composition Changes after a Weight Loss Intervention: A 3-Year Follow-Up Study" Nutrients 13, no. 1: 164. https://doi.org/10.3390/nu13010164
APA StyleRojo-Tirado, M. A., Benito, P. J., Ruiz, J. R., Ortega, F. B., Romero-Moraleda, B., Butragueño, J., Bermejo, L. M., Castro, E. A., & Gómez-Candela, C. (2021). Body Composition Changes after a Weight Loss Intervention: A 3-Year Follow-Up Study. Nutrients, 13(1), 164. https://doi.org/10.3390/nu13010164








