Changes in Child and Adult Care Food Program (CACFP) Practices at Participating Childcare and Education Centers in the United States Following Updated National Standards, 2017–2019
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design, Survey Administration, and Study Sample
2.2. Survey Content
2.3. Measures
2.3.1. Outcome Variable Measures
Implementation Progress and Challenges
Meeting CACFP Standards and Best Practices
2.3.2. Control Variable Measures
2.4. Statistical Analysis
3. Results
3.1. Characteristics of the Centers
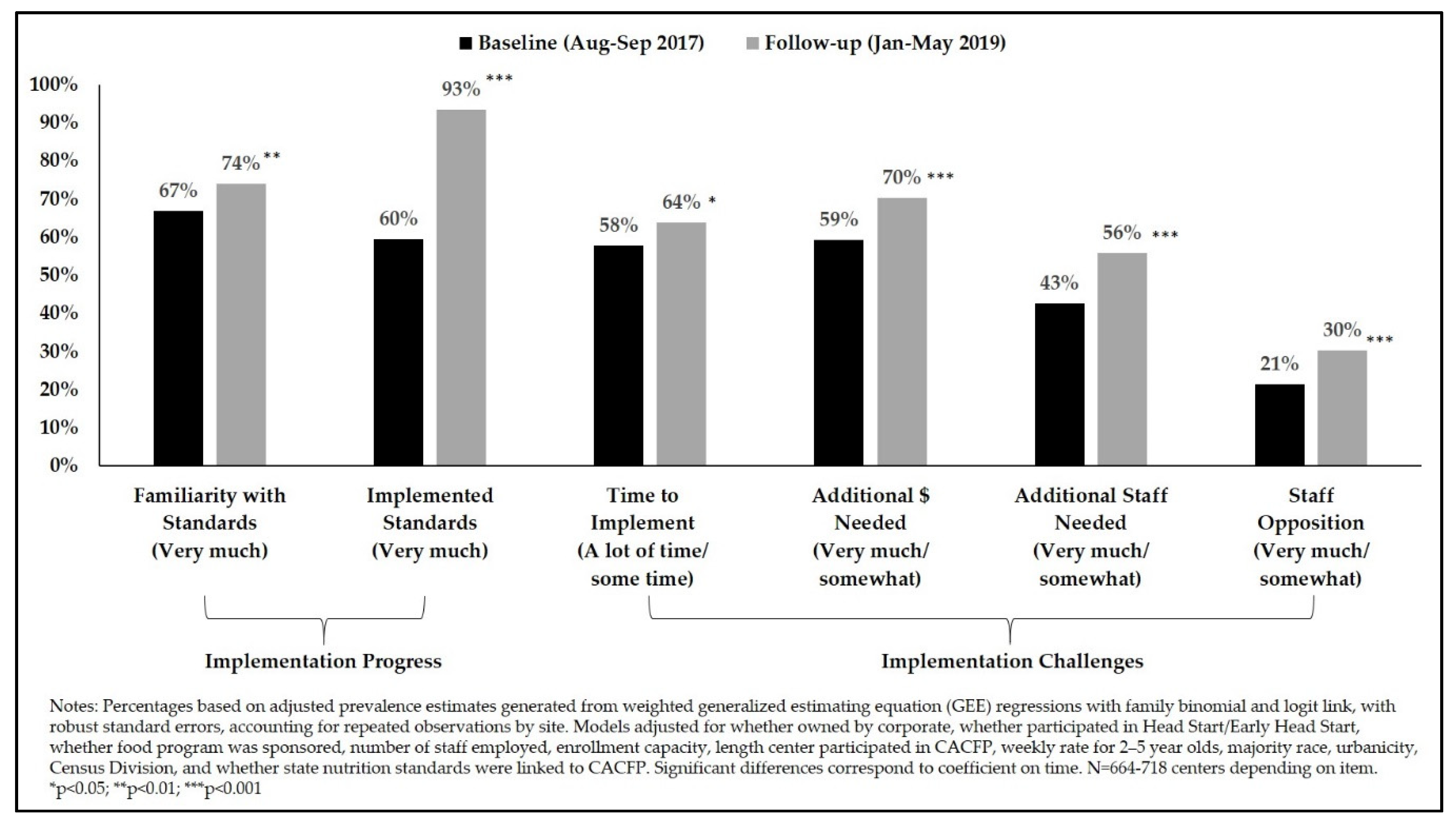
3.2. Implementation Progress and Challenges
3.3. Progress in Meeting CACFP Standards
3.4. Progress in Meeting Selected CACFP Best Practices
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A. Supplementary Tables
| Characteristic | Unweighted Responders | Unweighted Non-Responders | p-Value (Responders vs. Non-Responders) |
|---|---|---|---|
| Center characteristics | |||
| Corporate-owned (baseline) | 29.60 | 31.34 | 0.51 |
| Participated in Head Start/Early Head Start (baseline) | 33.57 | 34.43 | 0.75 |
| Food program sponsored (baseline) | 36.52 | 39.92 | 0.22 |
| Number of staff employed | |||
| 1–10 employees | 32.36 | 34.02 | 0.24 |
| 11–20 employees | 37.63 | 41.08 | |
| 21–30 employees | 16.65 | 14.32 | |
| ≥31 employees | 13.36 | 10.58 | |
| Enrolment capacity | |||
| 1–25 children | 7.13 | 8.54 | 0.33 |
| 26–50 children | 19.14 | 15.42 | |
| 51–100 children | 39.24 | 40.63 | |
| 101–499 children | 34.48 | 35.42 | |
| Length of center’s participation in CACFP | |||
| <10 years | 35.28 | 40.10 | 0.10 |
| 10+ years | 64.72 | 59.90 | |
| Weekly rate for 2–5-year-old | |||
| Free/no cost or state subsidized | 22.03 | 21.80 | 0.64 |
| $1–$100.99 | 12.38 | 12.36 | |
| $101–$200.99 | 45.30 | 48.31 | |
| ≥$201 | 20.30 | 17.53 | |
| Zip code-level characteristics | |||
| % Urban (Mean) | 80.24 | 80.98 | 0.66 |
| Majority (≥50%) race | |||
| Non-Hispanic White | 68.30 | 63.71 | 0.28 |
| Non-Hispanic Black | 7.46 | 9.69 | |
| Hispanic | 11.07 | 12.99 | |
| Mixed | 13.17 | 13.61 | |
| State/regional characteristics | |||
| State nutrition standards linked to CACFP | |||
| Not mentioned | 40.33 | 42.06 | 0.53 |
| Standards linked to CACFP | 59.67 | 57.94 | |
| Census division | |||
| New England | 5.59 | 3.09 | 0.39 |
| Middle Atlantic | 10.72 | 13.40 | |
| East North Central | 16.90 | 14.43 | |
| West North Central | 8.62 | 7.84 | |
| South Atlantic | 16.90 | 17.53 | |
| East South Central | 6.64 | 7.84 | |
| West South Central | 8.39 | 9.28 | |
| Mountain | 7.93 | 8.25 | |
| Pacific | 18.30 | 18.35 |
| Standard | Unadjusted OR (95% CI) | Unadjusted p-Value | Unadjusted Prevalence, % (SE) | |
|---|---|---|---|---|
| Pre | Post | |||
| Beverage Standards | ||||
| Water availability, milk flavor, 100% juice all meet requirements, and site does not serve juice drinks or soda | 1.47 * (1.04–2.08) | 0.031 | 88.90 (1.30) | 92.12 (1.09) |
| Only 1% or skim milk served, and no flavored milk | 0.83 (0.67–1.04) | 0.102 | 80.23 (1.58) | 77.16 (1.69) |
| Flavored milk is never served | 1.83 * (1.11–3.01) | 0.018 | 93.30 (1.01) | 96.20 (0.76) |
| Serves 100% juice less than twice a day | NC | NC | 97.03 (0.72) | 99.36 (0.28) |
| Sugar in Cereals Standard | ||||
| No sugar cereals served | 1.92 *** (1.52–2.43) | <0.001 | 70.14 (1.80) | 81.50 (1.57) |
| Frosted Flakes | 0.77 (0.52–1.14) | 0.190 | 7.97 (1.05) | 6.25 (0.94) |
| Apple Jacks | 0.68 (0.41–1.16) | 0.158 | 5.79 (0.94) | 4.06 (0.82) |
| Froot Loops | 0.48 *** (0.31–0.73) | <0.001 | 9.58 (1.19) | 4.88 (0.88) |
| Sugar Smacks/Honey Smacks | NC | NC | 0.41 (0.21) | 1.80 (0.51) |
| Lucky Charms | 0.58 * (0.36–0.94) | 0.027 | 5.02 (0.84) | 3.01 (0.67) |
| Honey Nut Cheerios | 0.55 *** (0.43–0.71) | <0.001 | 21.49 (1.62) | 13.28 (1.37) |
| Sugar in Yogurt | ||||
| Only plain/unflavored yogurt served | 1.15 (0.98–1.35) | 0.094 | 33.36 (1.91) | 36.51 (1.95) |
| Best Practice | Unadjusted OR (95% CI) | Unadjusted p-Value | Unadjusted Prevalence, % (SE) | |
|---|---|---|---|---|
| Pre | Post | |||
| Beverage Best Practices | ||||
| Type of milk typically served is 1% or skim | 0.67 *** (0.53–0.85) | <0.001 | 85.51 (1.40) | 79.87 (1.62) |
| Whole milk is one of milks typically served | 1.94 *** (1.38–2.72) | <0.001 | 6.53 (0.95) | 11.87 (1.28) |
| Site never serves fruit drinks | 0.83 (0.49–1.40) | 0.487 | 97.28 (0.62) | 96.75 (0.72) |
| Vegetable and Fruit Best Practices | ||||
| Dark green vegetables provided at least 1x/week | 0.97 (0.81–1.15) | 0.690 | 63.36 (1.89) | 62.55 (1.94) |
| Red/orange vegetables provided at least 1x/week | 0.84 (0.67–1.05) | 0.126 | 77.33 (1.67) | 74.19 (1.76) |
| Starchy vegetables provided at least 1x/week | 1.00 (0.82–1.22) | 0.992 | 69.12 (1.84) | 69.09 (1.86) |
| Other vegetables provided at least 1x/week | 0.80 * (0.64–1.00) | 0.046 | 82.99 (1.46) | 79.66 (1.61) |
| Fruit or vegetable is a component of a snack at least once a day, or every snack includes vegetable or fruit | 1.09 (0.89–1.33) | 0.393 | 60.96 (1.97) | 62.94 (1.96) |
| Other Best Practices | ||||
| Serves 100% whole grains | 2.07 * (1.05–4.06) | 0.035 | 96.51 (0.72) | 98.27 (0.54) |
| Only low fat/reduced fat cheese, or cheese not served | 1.33 ** (1.09–1.61) | 0.005 | 33.54 (2.01) | 39.96 (2.11) |
| Processed meats served less than once a week | 1.29 * (1.03–1.61) | 0.026 | 74.68 (1.75) | 79.08 (1.63) |
| Any processed meats served | 0.19 *** (0.15–0.25) | <0.001 | 90.97 (1.09) | 66.59 (1.87) |
References
- U.S. Department of Agriculture. Child and Adult Care Food Program Participation, Meals, and Costs. Available online: https://fns-prod.azureedge.net/pd/child-nutrition-tables (accessed on 15 September 2020).
- U.S. Department of Agriculture. Child and Adult Care Food Program: Meal Pattern Revisions Related to the Healthy, Hunger-Free Kids Act of 2010. Final rule. Fed. Regist. 2016, 81, 24347–24383. [Google Scholar]
- U.S. Department of Agriculture. Transition period for the updated Child and Adult Care Food Program meal program and the updated National School Lunch Program and School Breakfast Program Infants and Preschool Meal Patterns. Available online: https://www.fns.usda.gov/transition-period-updated-cacfp-infant-preschool-meal-patterns (accessed on 10 October 2019).
- Food Research & Action Center. Child & Adult Care Food Program: Participation Trends 2018. Available online: https://frac.org/wp-content/uploads/CACFP-participation-trends-2018.pdf (accessed on 17 May 2020).
- Andreyeva, T.; Henderson, K.E. Center-Reported Adherence to Nutrition Standards of the Child and Adult Care Food Program. Child. Obes. 2018, 14, 421–428. [Google Scholar] [CrossRef] [PubMed]
- Cotwright, C.J.; Bradley, H.; Celestin, N.; Drake, S.; Love, K.; Birch, L. Beverage Policy Implementation by Child and Adult Care Food Program Participation and Program Type: A Statewide Examination in Georgia. Child. Obes. 2019, 15, 185–193. [Google Scholar] [CrossRef] [PubMed]
- Dev, D.A.; Garcia, A.S.; Dzewaltowski, D.A.; Sisson, S.; Franzen-Castle, L.; Rida, Z.; Williams, N.A.; Hillburn, C.; Dinkel, D.; Srivastava, D.; et al. Provider reported implementation of nutrition-related practices in childcare centers and family childcare homes in rural and urban Nebraska. Prev. Med. Rep. 2020, 17, 101021. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.L.; Gurzo, K.; Yoshida, S.; Vitale, E.H.; Hecht, K.; Ritchie, L.D. Compliance with the New 2017 Child and Adult Care Food Program Standards for Infants and Children before Implementation. Child. Obes. 2018, 14, 393–402. [Google Scholar] [CrossRef] [PubMed]
- Gurzo, K.; Lee, D.L.; Ritchie, K.; Yoshida, S.; Vitale, E.H.; Hecht, K.; Ritchie, L.D. Child Care Sites Participating in the Federal Child and Adult Care Food Program Provide More Nutritious Foods and Beverages. J. Nutr. Educ. Behav. 2020. [Google Scholar] [CrossRef]
- Lee, D.L.; Gurzo, K.; Nhan, L.A.; Vitale, E.H.; Yoshida, S.; Hecht, K.; Ritchie, L.D. Status of Beverages Served to Young Children in Child Care After Implementation of California Policy, 2012–2016. Prev. Chronic Dis. 2020, 17, 190296. [Google Scholar] [CrossRef]
- Lessard, L. Implementation of Revised Nutrition Standards in US Department of Agriculture’s Child and Adult Care Food Program. J. Nutr. Educ. Behav. 2019. [Google Scholar] [CrossRef]
- Chriqui, J.F.; Leider, J.; Schermbeck, R.M. Early Childhood Education Centers’ Reported Readiness to Implement the Updated Child and Adult Care Food Program Meal Pattern Standards in the United States, 2017. Child. Obes. 2018, 14, 412–420. [Google Scholar] [CrossRef]
- UIC Center for Clinical and Translational Science. REDCap: Research Electronic Data Capture. Available online: https://ccts.uic.edu/tools/redcap/ (accessed on 1 September 2020).
- American Association for Public Opinion Research. Response Rates-An Overview. Available online: http://www.aapor.org/Education-Resources/For-Researchers/Poll-Survey-FAQ/Response-Rates-An-Overview.aspx (accessed on 20 February 2018).
- Machin, D.; Campbell, M.J.; Fayers, P.; Pinol, A. Sample Size Tables for Clinical Studies, 2nd ed.; Blackwell Science: London, UK, 1997. [Google Scholar]
- U.S. Census Bureau. 2011–2015 ACS 5-Year Estimates. Available online: http://www2.census.gov/programs-surveys/acs/summary_file/2015/data/5_year_by_state/ (accessed on 15 September 2020).
- U.S. Census Bureau. 2010 Census Summary File 1. Available online: https://factfinder.census.gov/faces/nav/jsf/pages/index.xhtml (accessed on 15 October 2017).
- Public Health Law Center. Child Care Regulations. Available online: https://www.publichealthlawcenter.org/heal/ChildCareMap2016.html (accessed on 16 July 2019).
- U.S. Census Bureau. Census Regions and Divisions. Available online: https://www2.census.gov/geo/pdfs/maps-data/maps/reference/us_regdiv.pdf (accessed on 1 October 2019).
- Muller, C.J.; MacLehose, R.F. Estimating predicted probabilities from logistic regression: Different methods correspond to different target populations. Int. J. Epidemiol. 2014, 43, 962–970. [Google Scholar] [CrossRef]
- Zaltz, D.A.; Hecht, A.A.; Pate, R.R.; Neelon, B.; O’Neill, J.R.; Benjamin-Neelon, S.E. Participation in the Child and Adult Care Food Program is associated with fewer barriers to serving healthier foods in early care and education. BMC Public Health 2020, 20, 856. [Google Scholar] [CrossRef]
- Asada, Y.; Ziemann, M.; Zatz, L.; Chriqui, J. Successes and Challenges in School Meal Reform: Qualitative Insights from Food Service Directors. J. Sch. Health 2017, 87, 608–615. [Google Scholar] [CrossRef] [PubMed]
- Tabak, R.G.; Moreland-Russell, S. Food Service Perspectives on National School Lunch Program Implementation. Health Behav. Policy Rev. 2015, 2, 362–371. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J.F.; Gorski, M.T.; Hoffman, J.A.; Rosenfeld, L.; Chaffee, R.; Smith, L.; Catalano, P.J.; Rimm, E.B. Healthier Standards for School Meals and Snacks: Impact on School Food Revenues and Lunch Participation Rates. Am. J. Prev. Med. 2016, 51, 485–492. [Google Scholar] [CrossRef] [PubMed]
- Lott, M.; Callahan, E.; Welker, E.; Story, M.; Daniels, S. Healthy Beverage Consumption in Early Childhood: Recommendations from Key National Health and Nutrition Organizations, Consensus Statement. Consens. Statement 2019. Available online: http://healthyeatingresearch.org/ (accessed on 1 September 2020).
- Howard, F. Consumers More Often Turn To Whole Milk. 2019. Available online: https://www.milkbusiness.com/article/consumers-more-often-turn-to-whole-milk (accessed on 4 September 2020).
- U.S. Department of Agriculture. Choose my plate: All About the Dairy Group. Available online: https://www.choosemyplate.gov/eathealthy/dairy (accessed on 1 September 2020).
- Schermbeck, R.M.; Leider, J.; Chriqui, J.F. Sugary Cereals at Early Childhood Education Centers Participating in the Child and Adult Care Food Program, 2017. Prev. Chronic Dis. 2019, 16, E34. [Google Scholar] [CrossRef] [PubMed]
- U.S Department of Agriculture. CACFP Halftime Webinar: Choose Breakfast Cereals That Are Lower in Added Sugars. 2017. Available online: https://www.fns.usda.gov/tn/thirty-thursdays-choose-breakfast-cereals-lower-added-sugars (accessed on 1 September 2020).
- Center for Science in the Public Interest. Milkshakes, Sugary Cereals, Candy: What Nickelodeon is Peddling to Kids; Center for Science in the Public Interest: Washington, DC, USA, 2016; Available online: https://cspinet.org/sites/default/files/attachment/Nickelodeon%20brief.pdf (accessed on 20 August 2020).
- U.S. Department of Health and Human Services; U.S. Department of Agriculture. 2015–2020 Dietary Guidelines for Americans, 8th ed.; Government Printing Office: Washington, DC, USA, 2015.
- Neelon, S.E.B.; Vaughn, A.; Ball, S.C.; McWilliams, C.; Ward, D.S. Nutrition practices and mealtime environments of North Carolina child care centers. Child. Obes. 2012, 8, 216–223. [Google Scholar] [CrossRef]
- Ervin, R.B.; Kit, B.K.; Carroll, M.D.; Ogden, C.L. Consumption of Added Sugar among U.S. Children and Adolescents, 2005–2008; Department of Health and Human Services: Washington, DC, USA, 2012. [Google Scholar]
- Maalouf, J.; Evers, S.C.; Griffin, M.; Lyn, R. Assessment of mealtime environments and nutrition practices in child care centers in Georgia. Child. Obes. 2013, 9, 437–445. [Google Scholar] [CrossRef]
- Ritchie, L.D.; Boyle, M.; Chandran, K.; Spector, P.; Whaley, S.E.; James, P.; Samuels, S.; Hecht, K.; Crawford, P. Participation in the Child and Adult Care Food Program Is Associated with More Nutritious Foods and Beverages in Child Care. Child. Obes. 2012, 8, 224–229. [Google Scholar] [CrossRef]
- Ritchie, L.D.; Sharma, S.; Gildengorin, G.; Yoshida, S.; Braff-Guajardo, E.; Crawford, P. Policy Improves What Beverages Are Served to Young Children in Child Care. J. Acad. Nutr. Diet. 2015, 115, 724–730. [Google Scholar] [CrossRef]
- Tovar, A.; Risica, P.; Mena, N.; Lawson, E.; Ankoma, A.; Gans, K.M. An Assessment of Nutrition Practices and Attitudes in Family Child-Care Homes: Implications for Policy Implementation. Prev. Chronic Dis. 2015, 12, E88. [Google Scholar] [CrossRef][Green Version]
- Erinosho, T.; Vaughn, A.; Hales, D.; Mazzucca, S.; Gizlice, Z.; Ward, D. Participation in the Child and Adult Care Food Program is Associated with Healthier Nutrition Environments at Family Child Care Homes in Mississippi. J. Nutr. Educ. Behav. 2018, 50, 441–450. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | % or Mean (SE) |
|---|---|
| Center characteristics | |
| Corporate-owned (follow-up; n = 858) | 30.45 (1.83) |
| Participated in Head Start/Early Head Start (follow-up; n = 858) | 33.03 (1.84) |
| Food program sponsored (follow-up; n = 856) | 41.40 (1.94) |
| Number of staff employed (n = 853) | |
| 1–10 employees | 33.73 (1.84) |
| 11–20 employees | 38.98 (1.93) |
| 21–30 employees | 15.00 (1.36) |
| ≥31 employees | 12.29 (1.21) |
| Enrolment capacity (n = 841) | |
| 1–25 children | 7.00 (1.00) |
| 26–50 children | 17.45 (1.44) |
| 51–100 children | 40.28 (1.95) |
| 101–499 children | 35.27 (1.85) |
| Length of center’s participation in CACFP (n = 771) | |
| <10 years | 36.92 (1.99) |
| 10+ years | 63.08 (1.99) |
| Weekly rate for 2–5-year-old children (n = 808) | |
| Free/no cost or state subsidized | 20.86 (1.58) |
| $1–$100.99 | 12.83 (1.34) |
| $101–$200.99 | 49.16 (1.96) |
| ≥$201 | 17.15 (1.33) |
| Zip code-level characteristics | |
| Majority (≥50%) race (n = 858) | |
| Non-Hispanic White | 58.53 (1.96) |
| Non-Hispanic Black | 11.55 (1.38) |
| Hispanic | 14.12 (1.43) |
| Mixed | 15.81 (1.47) |
| % Urban (Mean) (n = 858) | 82.02 (1.07) |
| State/regional characteristics | |
| State nutrition standards linked to CACFP (n = 858) | |
| Not mentioned | 42.25 (1.88) |
| Standards linked to CACFP | 57.75 (1.88) |
| Census division (n = 858) | |
| New England | 3.51 (0.17) |
| Middle Atlantic | 11.79 (0.58) |
| East North Central | 12.95 (0.49) |
| West North Central | 6.82 (0.44) |
| South Atlantic | 23.13 (0.61) |
| East South Central | 6.76 (0.55) |
| West South Central | 12.50 (0.65) |
| Mountain | 5.46 (0.42) |
| Pacific | 17.08 (0.64) |
| Standard | Adjusted OR (95% CI) | Adjusted p-Value | Adjusted Prevalence (%) | |
|---|---|---|---|---|
| Pre | Post | |||
| Beverage Standards | ||||
| Water availability, milk flavor, 100% juice all meet requirements, and site does not serve juice drinks or soda | 1.41 (0.94–2.10) | 0.094 | 88.98 | 91.76 |
| Only 1% or skim milk served, and no flavored milk | 0.85 (0.66–1.10) | 0.222 | 80.54 | 78.10 |
| Flavored milk is never served | 1.88 * (1.03–3.41) | 0.038 | 93.53 | 96.32 |
| Sugar in Cereals Standard | ||||
| No sugar cereals served | 2.08 *** (1.60–2.72) | <0.001 | 67.56 | 80.36 |
| Frosted Flakes | 0.74 (0.47–1.15) | 0.184 | 8.32 | 6.38 |
| Apple Jacks | 0.58 (0.31–1.09) | 0.091 | 6.17 | 3.76 |
| Froot Loops | 0.45 ** (0.28–0.73) | 0.001 | 9.42 | 4.62 |
| Sugar Smacks/Honey Smacks | NC | NC | NC | NC |
| Lucky Charms | 0.47 ** (0.28–0.80) | 0.005 | 5.63 | 2.79 |
| Honey Nut Cheerios | 0.51 *** (0.38–0.68) | <0.001 | 23.83 | 14.42 |
| Best Practice | Adjusted OR (95% CI) | Adjusted p-Value | Adjusted Prevalence (%) | |
|---|---|---|---|---|
| Pre | Post | |||
| Beverage Best Practices | ||||
| Type of milk typically served is 1% or skim | 0.66 ** (0.50–0.86) | 0.002 | 86.19 | 80.76 |
| Whole milk is one of milks typically served | 2.09 *** (1.43–3.03) | <0.001 | 6.16 | 11.81 |
| Site never serves fruit drinks | 0.73 (0.40–1.32) | 0.301 | 97.20 | 96.27 |
| Other Best Practices | ||||
| Serves 100% whole grains | 2.02 * (1.02–4.00) | 0.043 | 96.05 | 97.99 |
| Cheese not served, or only low fat/reduced fat cheese | 1.35 * (1.07–1.69) | 0.010 | 31.96 | 38.25 |
| Processed meats served less than once a week | 1.41 ** (1.10–1.80) | 0.007 | 72.66 | 78.48 |
| Any processed meats served | 0.16 *** (0.12–0.23) | <0.001 | 91.79 | 68.49 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chriqui, J.F.; Leider, J.; Schermbeck, R.M.; Sanghera, A.; Pugach, O. Changes in Child and Adult Care Food Program (CACFP) Practices at Participating Childcare and Education Centers in the United States Following Updated National Standards, 2017–2019. Nutrients 2020, 12, 2818. https://doi.org/10.3390/nu12092818
Chriqui JF, Leider J, Schermbeck RM, Sanghera A, Pugach O. Changes in Child and Adult Care Food Program (CACFP) Practices at Participating Childcare and Education Centers in the United States Following Updated National Standards, 2017–2019. Nutrients. 2020; 12(9):2818. https://doi.org/10.3390/nu12092818
Chicago/Turabian StyleChriqui, Jamie F., Julien Leider, Rebecca M. Schermbeck, Anmol Sanghera, and Oksana Pugach. 2020. "Changes in Child and Adult Care Food Program (CACFP) Practices at Participating Childcare and Education Centers in the United States Following Updated National Standards, 2017–2019" Nutrients 12, no. 9: 2818. https://doi.org/10.3390/nu12092818
APA StyleChriqui, J. F., Leider, J., Schermbeck, R. M., Sanghera, A., & Pugach, O. (2020). Changes in Child and Adult Care Food Program (CACFP) Practices at Participating Childcare and Education Centers in the United States Following Updated National Standards, 2017–2019. Nutrients, 12(9), 2818. https://doi.org/10.3390/nu12092818




