A Call to Action: Now Is the Time to Screen Elderly and Treat Osteosarcopenia, a Position Paper of the Italian College of Academic Nutritionists MED/49 (ICAN-49)
Abstract
:1. Introduction
2. Sarcopenia and Its Different Phenotypes as Predictors of Adverse Outcomes
2.1. Definition and Assessment of Sarcopenia
2.2. Epidemiology of Sarcopenia and Its Phenotypes
2.3. Sarcopenia-Related Outcomes
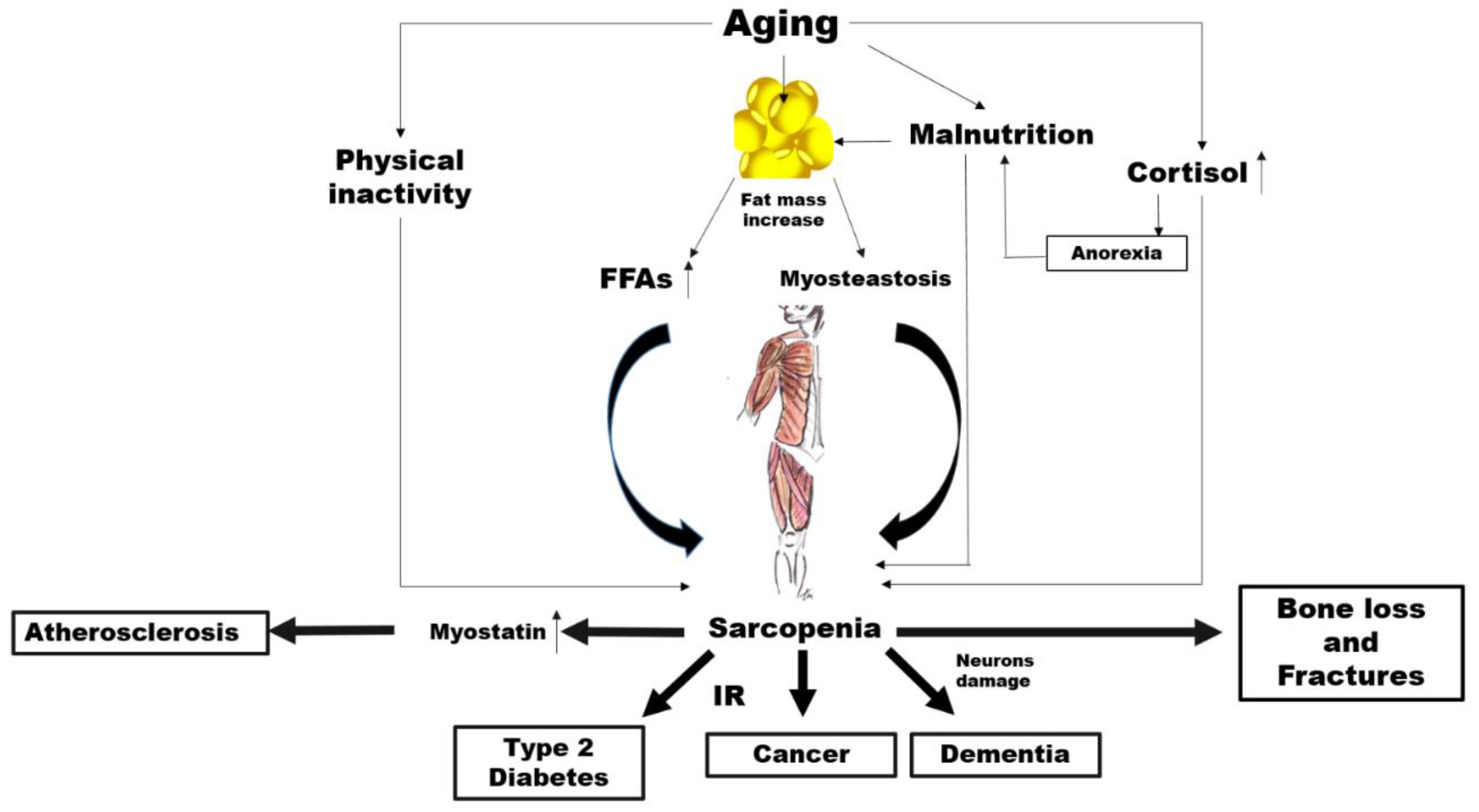
3. Potential Mechanisms Linking Sarcopenia to NCDs and Mortality
4. Now Is the Time to Screen for Sarcopenia
5. Recommendations
- Nutritionists are encouraged to screen for sarcopenia using a combination of DXA plus BIA as screening tools for secondary prevention.
- General practitioners (GPs) as well as other health care professionals should suggest a screening for sarcopenia in elderly individuals.
- Nutritionists as well as other health care professionals (as geriatrics, internists, neurologists and cardiologists) should ask National health authorities to plan screening for the early diagnosis of sarcopenia and its various phenotypes in the elderly.
- Nutritionists are encouraged to ask National health authorities for provide DXA and BIA equipment to the nutritional units and to reimburse the costs of all the treatments for those diagnosed with sarcopenia including where it is a secondary condition to chronic diseases.
- Nutritionists should collaborate with health care policy makers and health care providers regarding medical claims and common standards of screening technologies.
- Promotion of centralized data collections in epidemiological studies on older adults.
- Development of RCTs on new treatments for sarcopenia in individuals with either primary or secondary sarcopenia.
- GPs should receive continuing medical training regarding sarcopenia.
- The government should fund information and prevention campaigns, in collaboration with patient associations and scientific research groups.
- A protein intake of 1.2–1.5 g∙kg−1∙day−1 or higher for elderly adults, according to the nutrient intake, renal function and severity of sarcopenia, with at least 20–35 g/daily of whey protein, in conjunction with resistance exercise for a person with sarcopenia. Higher doses of protein (up to 2 g/day) may be appropriate in persons with severe illness or a catabolic status
- Vitamin D, from dietary and supplemental sources, to any older person with vitamin D deficiency of insufficiency (at least 800 UI per day or more according to serum concentrations).
- Calcium, from dietary and supplemental sources, should be in adequate amounts (i.e., at least 1200 mg per day).
- Patients/older individuals at risk of or with established sarcopenia should be encouraged to be involved in regular physical activity.
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- World Health Organization. Noncommunicable Diseases Country Profiles 2018; License: CC BY-NC-SA 3.0 IGO; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Eurostat. Eurostat Database. Available online: https://ec.europa.eu/eurostat/en/web/products-eurostat-news/-/DDN-20181026-1 (accessed on 26 October 2018).
- OECD/European Observatory on Health Systems and Policies. Italy: Country Health Profile 2017, State of Health in the EU; OECD Publishing: Paris, France; European Observatory on Health Systems and Policies: Brussels, Belgium, 2017. [Google Scholar]
- GBD 2017 Italy Collaborators. Italy’s health performance, 1990–2017: Findings from the Global Burden of Disease Study 2017. Lancet Public Health 2019, 4, e645–e657. [Google Scholar] [CrossRef]
- Clegg, A.; Young, J.; Iliffe, S.; Rikkert, M.O.; Rockwood, K. Frailty in elderly people. Lancet 2013, 381, 752–762. [Google Scholar] [CrossRef] [Green Version]
- COVID-19 Surveillance Group. Characteristics of COVID-19 Patients Dying in Italy: Report Based on Available Data on July 9th, 2020. Instituto Superiore Di Sanità. Available online: https://www.epicentro.iss.it/en/coronavirus/bollettino/Report-COVID-2019_9_july_2020.pdf (accessed on 9 July 2020).
- Inciardi, R.M.; Adamo, M.; Lupi, L.; Cani, D.S.; Di Pasquale, M.; Tomasoni, D.; Italia, L.; Zaccone, G.; Tedino, C.; Fabbricatore, D.; et al. Characteristics and outcomes of patients hospitalized for COVID-19 and cardiac disease in Northern Italy. Eur. Heart J. 2020, 41, 1821–1829. [Google Scholar] [CrossRef] [PubMed]
- Office for National Statistics; National Records of Scotland; Northern Ireland Statistics and Research Agency. 2011 Census Aggregate Data; Edition: June 2016; UK Data Service: Colchester, UK, 2016. [Google Scholar]
- Yancy, C.W. COVID-19 and African Americans. JAMA 2020, 323, 1891–1892. [Google Scholar] [CrossRef] [Green Version]
- Garg, S.; Kim, L.; Whitaker, M.; O’Halloran, A.; Cummings, C.; Holstein, R.; Prill, M.; Chai, S.J.; Kirley, P.D.; Alden, N.B.; et al. Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019—COVID-NET, 14 States, March 1–30, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 458–464. [Google Scholar] [CrossRef]
- Pauly, L.; Stehle, P.; Volkert, D. Nutritional situation of elderly nursing home residents. Z. Gerontol. Geriatr. 2007, 40, 3–12. [Google Scholar] [CrossRef]
- Valmorbida, E.; Trevisan, C.; Imoscopi, A.; Mazzochin, M.; Manzato, E.; Sergi, G. Malnutrition is associated with increased risk of hospital admission and death in the first 18 months of institutionalization. Clin. Nutr. 2020. [Google Scholar] [CrossRef]
- GBD 2017 Diet Collaborators. Health effects of dietary risks in 195 countries, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019, 393, 1958–1972. [Google Scholar]
- Gingrich, A.; Volkert, D.; Kiesswetter, E.; Thomanek, M.; Bach, S.; Sieber, C.C.; Zopf, Y. Prevalence and overlap of sarcopenia, frailty, cachexia and malnutrition in older medical inpatients. BMC Geriatr. 2019, 19, 120. [Google Scholar] [CrossRef] [Green Version]
- Pacifico, J.; Geerlings, M.A.; Reijnierse, E.M.; Phassouliotis, C.; Lim, W.K.; Maier, A.B. Prevalence of sarcopenia as a comorbid disease: A systematic review and meta-analysis. Exp. Gerontol. 2020, 131, 110801. [Google Scholar] [CrossRef]
- Mijnarends, D.M.; Schols, J.M.; Meijers, J.M.; Tan, F.E.; Verlaan, S.; Luiking, Y.C.; Morley, J.E.; Halfens, R.J. Instruments to assess sarcopenia and physical frailty in older people living in a community (care) setting: Similarities and discrepancies. J. Am. Med. Dir. Assoc. 2015, 16, 301–308. [Google Scholar] [CrossRef] [PubMed]
- Reijnierse, E.M.; Trappenburg, M.C.; Blauw, G.J.; Verlaan, S.; de van der Schueren, M.A.; Meskers, C.G.; Maier, A.B. Common ground? The concordance of sarcopenia and frailty definitions. J. Am. Med. Dir. Assoc. 2016, 17, 371–377. [Google Scholar] [CrossRef] [PubMed]
- Marty, E.; Liu, Y.; Samuel, A.; Or, O.; Lane, J. A review of sarcopenia: Enhancing awareness of an increasingly prevalent disease. Bone 2017, 105, 276–286. [Google Scholar] [CrossRef] [PubMed]
- Montero-Fernandez, N.; Serra-Rexach, J. Role of exercise on sarcopenia in the elderly. Eur. J. Phys. Rehabil Med. 2013, 49, 131–143. [Google Scholar]
- Atkins, J.L.; Whincup, P.H.; Morris, R.W.; Lennon, L.T.; Papacosta, O.; Wannamethee, S.G. Sarcopenic obesity and risk of cardiovascular disease and mortality: A population-based cohort study of older men. J. Am. Geriatr. Soc. 2014, 62, 253–260. [Google Scholar] [CrossRef] [Green Version]
- Baumgartner, R.N.; Koehler, K.M.; Gallagher, D.; Romero, L.; Heymsfield, S.B.; Ross, R.R.; Garry, P.J.; Lindeman, R.D. Epidemiology of sarcopenia among the elderly in New Mexico. Am. J. Epidemiol. 1998, 147, 755–763. [Google Scholar] [CrossRef]
- Melton, L.J., 3rd; Khosla, S.; Crowson, C.S.; O’Connor, M.K.; O’Fallon, W.M.; Riggs, B.L. Epidemiology of sarcopenia. J. Am. Geriatr. Soc. 2000, 48, 625–630. [Google Scholar] [CrossRef]
- Janssen, I.; Heymsfield, S.B.; Ross, R. Low relative skeletal muscle mass (sarcopenia) in older persons is associated with functional impairment and physical disability. J. Am. Geriatr. Soc. 2002, 50, 889–896. [Google Scholar] [CrossRef] [Green Version]
- Prynn, J.E.; Kuper, H. Perspectives on Disability and Non-Communicable Diseases in Low-and Middle-Income Countries, with a Focus on Stroke and Dementia. Int. J. Environ. Res. Public Health 2019, 16, 3488. [Google Scholar] [CrossRef] [Green Version]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef] [Green Version]
- Morley, J.E.; Abbatecola, A.M.; Argiles, J.M.; Baracos, V.; Bauer, J.; Bhasin, S.; Cederholm, T.; Coats, A.J.S.; Cummings, S.R.; Evans, W.J.; et al. Sarcopenia with limited mobility: An international consensus. J. Am. Med. Dir. Assoc. 2011, 12, 403–409. [Google Scholar] [CrossRef] [Green Version]
- Studenski, S.A.; Peters, K.W.; Alley, D.E.; Cawthon, P.M.; McLean, R.R.; Harris, T.B.; Ferrucci, L.; Guralnik, J.M.; Fragala, M.S.; Kenny, A.M.; et al. The FNIH sarcopenia project: Rationale, study description, conference recommendations, and final estimates. J. Gerontol. Ser. A Biomed. Sci. Med. Sci. 2014, 69, 547–558. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.-K.; Liu, L.-K.; Woo, J.; Assantachai, P.; Auyeung, T.-W.; Bahyah, K.S.; Chou, M.-Y.; Chen, L.-Y.; Hsu, P.-S.; Krairit, O.; et al. Sarcopenia in Asia: Consensus report of the Asian Working Group for Sarcopenia. J. Am. Med. Dir. Assoc. 2014, 15, 95–101. [Google Scholar] [CrossRef] [PubMed]
- Cooper, C.; Dere, W.; Evans, W.; Kanis, J.A.; Rizzoli, R.; Sayer, A.A.; Sieber, C.; Kaufman, J.-M.; Van Kan, G.A.; Boonen, S.; et al. Frailty and sarcopenia: Definitions and outcome parameters. Osteoporos. Int. 2012, 23, 1839–1848. [Google Scholar] [CrossRef] [PubMed]
- Buckinx, F.; Landi, F.; Cesari, M.; Fielding, R.A.; Visser, M.; Engelke, K.; Maggi, S.; Dennison, E.; Al-Daghri, N.M.; Allepaerts, S.; et al. Pitfalls in the measurement of muscle mass: A need for a reference standard. J. Cachexia Sarcopenia Muscle 2018, 9, 269–278. [Google Scholar] [CrossRef]
- Kyle, U.G.; Bosaeus, I.; De Lorenzo, A.D.; Deurenberg, P.; Elia, M.; Gómez, J.M.; Heitmann, B.L.; Kent-Smith, L.; Melchior, J.-C.; Pirlich, M.; et al. Bioelectrical impedance analysis—Part I: Review of principles and methods. Clin. Nutr. 2004, 23, 1226–1243. [Google Scholar] [CrossRef]
- Houtkooper, L.B.; Lohman, T.G.; Going, S.B.; Howell, W.H. Why bioelectrical impedance analysis should be used for estimating adiposity. Am. J. Clin. Nutr. 1996, 64, 436S–448S. [Google Scholar] [CrossRef]
- Beaudart, C.; Bruyère, O.; Geerinck, A.; Hajaoui, M.; Scafoglieri, A.; Perkisas, S.; Bautmans, I.; Gielen, E.; Reginster, J.-Y.; Buckinx, F. Equation models developed with bioelectric impedance analysis tools to assess muscle mass: A systematic review. Clin. Nutr. ESPEN 2020, 35, 47–62. [Google Scholar] [CrossRef] [Green Version]
- Sergi, G.; De Rui, M.; Stubbs, B.; Veronese, N.; Manzato, E. Measurement of lean body mass using bioelectrical impedance analysis: A consideration of the pros and cons. Aging Clin. Exp. Res. 2017, 29, 591–597. [Google Scholar] [CrossRef]
- Marra, M.; Sammarco, R.; De Lorenzo, A.; Iellamo, F.; Siervo, M.; Pietrobelli, A.; Donini, L.M.; Santarpia, L.; Cataldi, M.; Pasanisi, F.; et al. Assessment of body composition in health and disease using bioelectrical impedance analysis (BIA) and dual energy X-ray absorptiometry (DXA): A critical overview. Contrast Media Mol. Imaging 2019, 2019, 3548284. [Google Scholar] [CrossRef]
- Bianchi, L.; Abete, P.; Bellelli, G.; Bo, M.; Cherubini, A.; Corica, F.; Di Bari, M.; Maggio, M.; Manca, G.M.; Rizzo, M.R.; et al. Prevalence and clinical correlates of sarcopenia, identified according to the EWGSOP definition and diagnostic algorithm, in hospitalized older people: The GLISTEN study. J. Gerontol. Ser. A Biomed. Sci. Med. Sci. 2017, 72, 1575–1581. [Google Scholar] [CrossRef] [PubMed]
- Reijnierse, E.M.; Trappenburg, M.C.; Leter, M.J.; Blauw, G.J.; Sipilä, S.; Sillanpää, E.; Narici, M.V.; Hogrel, J.-Y.; Butler-Browne, G.; McPhee, J.S.; et al. The impact of different diagnostic criteria on the prevalence of sarcopenia in healthy elderly participants and geriatric outpatients. Gerontology 2015, 61, 491–496. [Google Scholar] [CrossRef]
- Churilov, I.; Churilov, L.; MacIsaac, R.J.; Ekinci, E.I. Systematic review and meta-analysis of prevalence of sarcopenia in post acute inpatient rehabilitation. Osteoporos. Int. 2018, 29, 805–812. [Google Scholar] [CrossRef] [PubMed]
- Verschueren, S.; Gielen, E.; O’neill, T.; Pye, S.; Adams, J.; Ward, K.; Wu, F.; Szulc, P.; Laurent, M.; Claessens, F.; et al. Sarcopenia and its relationship with bone mineral density in middle-aged and elderly European men. Osteoporos. Int. 2013, 24, 87–98. [Google Scholar] [CrossRef] [PubMed]
- Fiatarone Singh, M.A.; Singh, N.A.; Hansen, R.D.; Finnegan, T.P.; Allen, B.J.; Diamond, T.H.; Diwan, A.D.; Lloyd, B.D.; Williamson, D.A.; Smith, E.U.; et al. Methodology and baseline characteristics for the Sarcopenia and Hip Fracture study: A 5-year prospective study. J. Gerontol. Ser. A Biomed. Sci. Med. Sci. 2009, 64, 568–574. [Google Scholar] [CrossRef] [Green Version]
- Hida, T.; Ishiguro, N.; Shimokata, H.; Sakai, Y.; Matsui, Y.; Takemura, M.; Terabe, Y.; Harada, A. High prevalence of sarcopenia and reduced leg muscle mass in Japanese patients immediately after a hip fracture. Geriatr. Gerontol. Int. 2013, 13, 413–420. [Google Scholar] [CrossRef]
- Iolascon, G.; Giamattei, M.; Moretti, A.; Di Pietro, G.; Gimigliano, F.; Gimigliano, R. Sarcopenia in women with vertebral fragility fractures. Aging Clin. Exp. Res. 2013, 25, S129–S131. [Google Scholar] [CrossRef]
- Nielsen, B.R.; Abdulla, J.; Andersen, H.E.; Schwarz, P.; Suetta, C. Sarcopenia and osteoporosis in older people: A systematic review and meta-analysis. Eur. Geriatr. Med. 2018, 9, 419–434. [Google Scholar] [CrossRef]
- Fahimfar, N.; Tajrishi, F.Z.; Gharibzadeh, S.; Shafiee, G.; Tanha, K.; Heshmat, R.; Nabipour, I.; Raeisi, A.; Jalili, A.; Larijani, B.; et al. Prevalence of osteosarcopenia and its association with cardiovascular risk factors in Iranian older people: Bushehr elderly health (BEH) program. Calcif. Tissue Int. 2020, 106, 364–370. [Google Scholar] [CrossRef]
- Koliaki, C.; Liatis, S.; Dalamaga, M.; Kokkinos, A. Sarcopenic Obesity: Epidemiologic Evidence, Pathophysiology, and Therapeutic Perspectives. Curr. Obes. Rep. 2019, 8, 458–471. [Google Scholar] [CrossRef]
- Landi, F.; Calvani, R.; Tosato, M.; Martone, A.M.; Bernabei, R.; Onder, G.; Marzetti, E. Impact of physical function impairment and multimorbidity on mortality among community-living older persons with sarcopaenia: Results from the ilSIRENTE prospective cohort study. BMJ Open 2016, 6, e008281. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arango-Lopera, V.; Arroyo, P.; Gutiérrez-Robledo, L.M.; Perez-Zepeda, M.; Cesari, M. Mortality as an adverse outcome of sarcopenia. J. Nutr. Health Aging 2013, 17, 259–262. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Jentoft, A.J.; Landi, F.; Topinková, E.; Michel, J.P. Understanding sarcopenia as a geriatric syndrome. Curr. Opin. Clin. Nutr. Metab. Care 2010, 13, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Landi, F.; Liperoti, R.; Fusco, D.; Mastropaolo, S.; Quattrociocchi, D.; Proia, A.; Tosato, M.; Bernabei, R.; Onder, G. Sarcopenia and mortality among older nursing home residents. J. Am. Med. Dir. Assoc. 2012, 13, 121–126. [Google Scholar] [CrossRef]
- Bahat, G.; Ilhan, B. Sarcopenia and the cardiometabolic syndrome: A narrative review. Eur. Geriatr. Med. 2016, 7, 220–223. [Google Scholar] [CrossRef]
- Chang, K.V.; Hsu, T.H.; Wu, W.T.; Huang, K.C.; Han, D.S. Association between sarcopenia and cognitive impairment: A systematic review and meta-analysis. J. Am. Med. Dir. Assoc. 2016, 17, 1164–1167. [Google Scholar] [CrossRef]
- Tian, S.; Xu, Y. Association of sarcopenic obesity with the risk of all-cause mortality: A meta-analysis of prospective cohort studies. Geriatr. Gerontol. Int. 2016, 16, 155–166. [Google Scholar] [CrossRef]
- Newman, A.B.; Haggerty, C.L.; Goodpaster, B.; Harris, T.; Kritchevsky, S.; Nevitt, M.; Miles, T.P.; Visser, M. Strength and muscle quality in a well-functioning cohort of older adults: The Health, Aging and Body Composition Study. J. Am. Geriatr. Soc. 2003, 51, 323–330. [Google Scholar] [CrossRef]
- Kalinkovich, A.; Livshits, G. Sarcopenic obesity or obese sarcopenia: A cross talk between age-associated adipose tissue and skeletal muscle inflammation as a main mechanism of the pathogenesis. Ageing Res. Rev. 2017, 35, 200–221. [Google Scholar] [CrossRef]
- Stewart, S.T.; Cutler, D.M.; Rosen, A.B. Forecasting the effects of obesity and smoking on US life expectancy. N. Engl. J. Med. 2009, 361, 2252–2260. [Google Scholar] [CrossRef] [Green Version]
- Patterson, R.E.; Frank, L.L.; Kristal, A.R.; White, E. A comprehensive examination of health conditions associated with obesity in older adults. Am. J. Prev. Med. 2004, 27, 385–390. [Google Scholar] [CrossRef] [PubMed]
- Barbat-Artigas, S.; Pion, C.H.; Leduc-Gaudet, J.-P.; Rolland, Y.; Aubertin-Leheudre, M. Exploring the role of muscle mass, obesity, and age in the relationship between muscle quality and physical function. J. Am. Med. Dir. Assoc. 2014, 15, 303–313. [Google Scholar] [CrossRef] [PubMed]
- Nordström, A.; Eriksson, M.; Stegmayr, B.; Gustafson, Y.; Nordström, P. Low bone mineral density is an independent risk factor for stroke and death. Cerebrovasc. Dis. 2010, 29, 130–136. [Google Scholar] [CrossRef]
- Van Der Klift, M.; Pols, H.; Geleijnse, J.; Van der Kuip, D.; Hofman, A.; De Laet, C. Bone mineral density and mortality in elderly men and women: The Rotterdam Study. Bone 2002, 30, 643–648. [Google Scholar] [CrossRef]
- Trivedi, D.; Khaw, K. Bone mineral density at the hip predicts mortality in elderly men. Osteoporos. Int. 2001, 12, 259–265. [Google Scholar] [CrossRef] [PubMed]
- Yeung, S.S.; Reijnierse, E.M.; Pham, V.K.; Trappenburg, M.C.; Lim, W.K.; Meskers, C.G.; Maier, A.B. Sarcopenia and its association with falls and fractures in older adults: A systematic review and meta-analysis. J. Cachexia Sarcopenia Muscle 2019, 10, 485–500. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yoo, J.-I.; Kim, H.; Ha, Y.-C.; Kwon, H.-B.; Koo, K.-H. Osteosarcopenia in patients with hip fracture is related with high mortality. J. Korean Med. Sci. 2018, 33, e27. [Google Scholar] [CrossRef]
- Wang, Y.-J.; Wang, Y.; Zhan, J.-K.; Tang, Z.-Y.; He, J.-Y.; Tan, P.; Deng, H.-Q.; Huang, W.; Liu, Y.-S. Sarco-osteoporosis: Prevalence and association with frailty in Chinese community-dwelling older adults. Int. J. Endocrinol. 2015, 2015, 482940. [Google Scholar] [CrossRef] [Green Version]
- Ethgen, O.; Beaudart, C.; Buckinx, F.; Bruyère, O.; Reginster, J.-Y. The future prevalence of sarcopenia in Europe: A claim for public health action. Calcif. Tissue Int. 2017, 100, 229–234. [Google Scholar] [CrossRef] [Green Version]
- Nakanishi, R.; Oki, E.; Sasaki, S.; Hirose, K.; Jogo, T.; Edahiro, K.; Korehisa, S.; Taniguchi, D.; Kudo, K.; Kurashige, J.; et al. Sarcopenia is an independent predictor of complications after colorectal cancer surgery. Surg. Today 2018, 48, 151–157. [Google Scholar] [CrossRef]
- Cosquéric, G.; Sebag, A.; Ducolombier, C.; Thomas, C.; Piette, F.; Weill-Engerer, S. Sarcopenia is predictive of nosocomial infection in care of the elderly. Br. J. Nutr. 2006, 96, 895–901. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Altuna-Venegas, S.; Aliaga-Vega, R.; Maguiña, J.L.; Parodi, J.F.; Runzer-Colmenares, F.M. Risk of community-acquired pneumonia in older adults with sarcopenia of a hospital from Callao, Peru 2010–2015. Arch. Gerontol. Geriatr. 2019, 82, 100–105. [Google Scholar] [CrossRef] [PubMed]
- Randle, P.; Garland, P.; Hales, C.; Newsholme, E. The glucose fatty acid cycle; its role in insulin sensitivity and the metabolic disturbances of diabetes mellitus. Lancet 1963, 1, 785–789. [Google Scholar] [CrossRef]
- Ponti, F.; Santoro, A.; Mercatelli, D.; Gasperini, C.; Conte, M.; Martucci, M.; Sangiorgi, L.; Franceschi, C.; Bazzocchi, A. Aging and imaging assessment of body composition: From fat to facts. Front. Endocrinol. 2019, 10, 861. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carobbio, S.; Rodriguez-Cuenca, S.; Vidal-Puig, A. Origins of metabolic complications in obesity: Ectopic fat accumulation. The importance of the qualitative aspect of lipotoxicity. Curr. Opin. Clin. Nutr. Metab. Care 2011, 14, 520–526. [Google Scholar] [CrossRef]
- Miljkovic, I.; Cauley, J.A.; Wang, P.Y.; Holton, K.F.; Lee, C.G.; Sheu, Y.; Barrett-Connor, E.; Hoffman, A.R.; Lewis, C.B.; Orwoll, E.S.; et al. Abdominal myosteatosis is independently associated with hyperinsulinemia and insulin resistance among older men without diabetes. Obesity 2013, 21, 2118–2125. [Google Scholar] [CrossRef] [Green Version]
- Zamboni, M.; Gattazzo, S.; Rossi, A.P. Myosteatosis: A relevant, yet poorly explored element of sarcopenia. Eur. Geriatr. Med. 2019, 10, 5–6. [Google Scholar] [CrossRef] [Green Version]
- Goodpaster, B.H.; Carlson, C.L.; Visser, M.; Kelley, D.E.; Scherzinger, A.; Harris, T.B.; Stamm, E.; Newman, A.B. Attenuation of skeletal muscle and strength in the elderly: The Health ABC Study. J. Appl. Physiol. 2001, 90, 2157–2165. [Google Scholar] [CrossRef]
- Heshka, S.; Ruggiero, A.; Bray, G.A.; Foreyt, J.; Kahn, S.E.; Lewis, C.E.; Saad, M.; Schwartz, A.V. Look AHEAD Research Group. Altered body composition in type 2 diabetes mellitus. Int. J. Obes. 2008, 32, 780–787. [Google Scholar] [CrossRef] [Green Version]
- Kalyani, R.R.; Corriere, M.; Ferrucci, L. Age-related and disease-related muscle loss: The effect of diabetes, obesity, and other diseases. Lancet Diabetes Endocrinol. 2014, 2, 819–829. [Google Scholar] [CrossRef] [Green Version]
- Srikanthan, P.; Karlamangla, A.S. Relative muscle mass is inversely associated with insulin resistance and prediabetes. Findings from the third National Health and Nutrition Examination Survey. J. Clin. Endocrinol. Metab. 2011, 96, 2898–2903. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rimbert, V.; Boirie, Y.; Bedu, M.; Hocquette, J.-F.; Ritz, P.; Morio, B. Muscle fat oxidative capacity is not impaired by age but by physical inactivity: Association with insulin sensitivity. FASEB J. 2004, 18, 737–739. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reaven, G.M. The insulin resistance syndrome: Definition and dietary approaches to treatment. Annu. Rev. Nutr. 2005, 25, 391–406. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gast, K.B.; Tjeerdema, N.; Stijnen, T.; Smit, J.W.; Dekkers, O.M. Insulin resistance and risk of incident cardiovascular events in adults without diabetes: Meta-analysis. PLoS ONE 2012, 7, e52036. [Google Scholar] [CrossRef] [Green Version]
- Bjørge, T.; Lukanova, A.; Jonsson, H.; Tretli, S.; Ulmer, H.; Manjer, J.; Stocks, T.; Selmer, R.; Nagel, G.; Almquist, M.; et al. Metabolic syndrome and breast cancer in the me-can (metabolic syndrome and cancer) project. Cancer Epidemiol. Prev. Biomark. 2010, 19, 1737–1745. [Google Scholar] [CrossRef] [Green Version]
- Stocks, T.; Rapp, K.; Bjørge, T.; Manjer, J.; Ulmer, H.; Selmer, R.; Lukanova, A.; Johansen, D.; Concin, H.; Tretli, S. Blood glucose and risk of incident and fatal cancer in the metabolic syndrome and cancer project (me-can): Analysis of six prospective cohorts. PLoS Med. 2009, 6, e1000201. [Google Scholar] [CrossRef]
- Borena, W.; Strohmaier, S.; Lukanova, A.; Bjørge, T.; Lindkvist, B.; Hallmans, G.; Edlinger, M.; Stocks, T.; Nagel, G.; Manjer, J.; et al. Metabolic risk factors and primary liver cancer in a prospective study of 578,700 adults. Int. J. Cancer 2012, 131, 193–200. [Google Scholar] [CrossRef]
- Burger, E.; Klein-Nulend, J. Microgravity and bone cell mechanosensitivity. Bone 1998, 22, 127S–130S. [Google Scholar] [CrossRef]
- Lloyd, S.A.; Lang, C.H.; Zhang, Y.; Paul, E.M.; Laufenberg, L.J.; Lewis, G.S.; Donahue, H.J. Interdependence of muscle atrophy and bone loss induced by mechanical unloading. J. Bone Miner. Res. 2014, 29, 1118–1130. [Google Scholar] [CrossRef] [Green Version]
- Burr, D.B. Muscle strength, bone mass, and age-related bone loss. J. Bone Miner. Res. 1997, 12, 1547–1551. [Google Scholar] [CrossRef]
- Hamrick, M.W.; McNeil, P.L.; Patterson, S.L. Role of muscle-derived growth factors in bone formation. J. Musculoskelet. Neuronal Interact. 2010, 10, 64–70. [Google Scholar] [PubMed]
- Hamrick, M.W. A role for myokines in muscle-bone interactions. Exerc. Sport Sci. Rev. 2011, 39, 43–47. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bauman, W.A.; Spungen, A.M.; Wang, J.; Pierson, R.N., Jr.; Schwartz, E. Relationship of fat mass and serum estradiol with lower extremity bone in persons with chronic spinal cord injury. Am. J. Physiol. Endocrinol. Metab. 2006, 290, E1098–E1103. [Google Scholar] [CrossRef] [PubMed]
- Verzola, D.; Barisione, C.; Picciotto, D.; Garibotto, G.; Koppe, L. Emerging role of myostatin and its inhibition in the setting of chronic kidney disease. Kidney Int. 2019, 95, 506–517. [Google Scholar] [CrossRef]
- Léger, B.; Derave, W.; De Bock, K.; Hespel, P.; Russell, A.P. Human sarcopenia reveals an increase in SOCS-3 and myostatin and a reduced efficiency of Akt phosphorylation. Rejuvenation Res. 2008, 11, 163–175B. [Google Scholar] [CrossRef] [Green Version]
- McPherron, A.C.; Lawler, A.M.; Lee, S.-J. Regulation of skeletal muscle mass in mice by a new TGF-p superfamily member. Nature 1997, 387, 83–90. [Google Scholar] [CrossRef]
- Hill, E.W.; Gu, J.; Eivers, S.S.; Fonseca, R.G.; McGivney, B.A.; Govindarajan, P.; Orr, N.; Katz, L.M.; MacHugh, D. A sequence polymorphism in MSTN predicts sprinting ability and racing stamina in thoroughbred horses. PLoS ONE 2010, 5, e8645. [Google Scholar] [CrossRef]
- Brandt, C.; Hansen, R.H.; Hansen, J.B.; Olsen, C.H.; Galle, P.; Mandrup-Poulsen, T.; Gehl, J.; Pedersen, B.K.; Hojman, P. Over-expression of Follistatin-like 3 attenuates fat accumulation and improves insulin sensitivity in mice. Metabolism 2015, 64, 283–295. [Google Scholar] [CrossRef]
- Dschietzig, T.B. Myostatin—From the mighty mouse to cardiovascular disease and cachexia. Clin. Chim. Acta 2014, 433, 216–224. [Google Scholar] [CrossRef]
- Verzola, D.; Milanesi, S.; Bertolotto, M.; Garibaldi, S.; Villaggio, B.; Brunelli, C.; Balbi, M.; Ameri, P.; Montecucco, F.; Palombo, D. Myostatin mediates abdominal aortic atherosclerosis progression by inducing vascular smooth muscle cell dysfunction and monocyte recruitment. Sci. Rep. 2017, 7, 46362. [Google Scholar] [CrossRef]
- Yiallouris, A.; Agapidaki, E.; Ntourakis, D.; Tsioutis, C.; Zafeiri, M.; Johnson, E.O. Adrenal aging and its implications on stress responsiveness in humans. Front. Endocrinol. 2019, 10, 54. [Google Scholar] [CrossRef] [PubMed]
- Lamberts, S.W.; Van den Beld, A.W.; Van Der Lely, A.-J. The endocrinology of aging. Science 1997, 278, 419–424. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tiganescu, A.; Walker, E.A.; Hardy, R.S.; Mayes, A.E.; Stewart, P.M. Localization, age-and site-dependent expression, and regulation of 11β-hydroxysteroid dehydrogenase type 1 in skin. J. Investig. Dermatol. 2011, 131, 30–36. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Izquierdo, M.; Häkkinen, K.; Antón, A.; Garrues, M.; Ibañez, J.; Ruesta, M.; Gorostiaga, E.M. Maximal strength and power, endurance performance, and serum hormones in middle-aged and elderly men. Med. Sci. Sports Exerc. 2001, 33, 1577–1587. [Google Scholar] [CrossRef] [Green Version]
- Peeters, G.; Van Schoor, N.; Visser, M.; Knol, D.; Eekhoff, E.; De Ronde, W.; Lips, P. Relationship between cortisol and physical performance in older persons. Clin. Endocrinol. 2007, 67, 398–406. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ennis, G.E.; An, Y.; Resnick, S.M.; Ferrucci, L.; O’Brien, R.J.; Moffat, S.D. Long-term cortisol measures predict Alzheimer disease risk. Neurology 2017, 88, 371–378. [Google Scholar] [CrossRef] [Green Version]
- Maeda, K.; Tanimoto, K.; Terada, T.; Shintani, T.; Kakigi, T. Elevated urinary free cortisol in patients with dementia. Neurobiol. Aging 1991, 12, 161–163. [Google Scholar] [CrossRef]
- Mijnarends, D.; Schols, J.; Halfens, R.; Meijers, J.; Luiking, Y.; Verlaan, S.; Evers, S. Burden-of-illness of Dutch community-dwelling older adults with sarcopenia: Health related outcomes and costs. Eur. Geriatr. Med. 2016, 7, 276–284. [Google Scholar] [CrossRef]
- Tang, T.; Wu, L.; Yang, L.; Jiang, J.; Hao, Q.; Dong, B.; Yang, M. A sarcopenia screening test predicts mortality in hospitalized older adults. Sci. Rep. 2018, 8, 1–9. [Google Scholar] [CrossRef]
- Yu, S.C.; Khow, K.S.; Jadczak, A.D.; Visvanathan, R. Clinical screening tools for sarcopenia and its management. Curr. Gerontol. Geriatr. Res. 2016, 2016, 5978523. [Google Scholar] [CrossRef] [Green Version]
- Nawi, S.N.M.; Yu, S.C. Screening Tools for Sarcopenia in Community-Dwellers: A Scoping Review. Ann. Acad Med. Singap. 2019, 48, 201–216. [Google Scholar]
- Malmstrom, T.K.; Morley, J.E. SARC-F: A simple questionnaire to rapidly diagnose sarcopenia. J. Am. Med. Dir. Assoc. 2013, 14, 531–532. [Google Scholar] [CrossRef] [PubMed]
- Goodman, M.J.; Ghate, S.R.; Mavros, P.; Sen, S.; Marcus, R.L.; Joy, E.; Brixner, D.I. Development of a practical screening tool to predict low muscle mass using NHANES 1999–2004. J. Cachexia Sarcopenia Muscle 2013, 4, 187–197. [Google Scholar] [CrossRef] [PubMed]
- Visvanathan, R.; Yu, S.; Field, J.; Chapman, I.; Adams, R.; Wittert, G.; Visvanathan, T. Appendicular Skeletal Muscle Mass: Development and Validation of Anthropometric Prediction Equations. J. Frailty Aging 2012, 1, 147–151. [Google Scholar] [PubMed]
- Ishii, S.; Tanaka, T.; Shibasaki, K.; Ouchi, Y.; Kikutani, T.; Higashiguchi, T.; Obuchi, S.P.; Ishikawa-Takata, K.; Hirano, H.; Kawai, H. Development of a simple screening test for sarcopenia in older adults. Geriatr. Gerontol. Int. 2014, 14, 93–101. [Google Scholar] [CrossRef] [PubMed]
- Yu, S.; Appleton, S.; Chapman, I.; Adams, R.; Wittert, G.; Visvanathan, T.; Visvanathan, R. An anthropometric prediction equation for appendicular skeletal muscle mass in combination with a measure of muscle function to screen for sarcopenia in primary and aged care. J. Am. Med. Dir. Assoc. 2015, 16, 25–30. [Google Scholar] [CrossRef] [PubMed]
- Krzymińska-Siemaszko, R.; Tobis, S.; Lewandowicz, M.; Wieczorowska-Tobis, K. Comparison of four sarcopenia screening questionnaires in community-dwelling older adults from Poland using six sets of international diagnostic criteria of sarcopenia. PLoS ONE 2020, 15, e0231847. [Google Scholar]
- Ida, S.; Kaneko, R.; Murata, K. SARC-F for screening of sarcopenia among older adults: A meta-analysis of screening test accuracy. J. Am. Med. Dir. Assoc. 2018, 19, 685–689. [Google Scholar] [CrossRef]
- Fletcher, S.W.; Elmore, J.G. Clinical practice. Mammographic screening for breast cancer. N. Engl. J. Med. 2003, 348, 1672–1680. [Google Scholar] [CrossRef] [Green Version]
- Damilakis, J.; Adams, J.E.; Guglielmi, G.; Link, T.M. Radiation exposure in X-ray-based imaging techniques used in osteoporosis. Eur. Radiol. 2010, 20, 2707–2714. [Google Scholar] [CrossRef] [Green Version]
- Blake, G.M.; Naeem, M.; Boutros, M. Comparison of effective dose to children and adults from dual X-ray absorptiometry examinations. Bone 2006, 38, 935–942. [Google Scholar] [CrossRef]
- Elmore, J.G.; Barton, M.B.; Moceri, V.M.; Polk, S.; Arena, P.J.; Fletcher, S.W. Ten-year risk of false positive screening mammograms and clinical breast examinations. N. Engl. J. Med. 1998, 338, 1089–1096. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Paskett, E.D.; Rimer, B.K. Psychosocial effects of abnormal Pap tests and mammograms: A review. J. Womens Health 1995, 4, 73–82. [Google Scholar] [CrossRef]
- Elmore, J.G.; Nakano, C.Y.; Koepsell, T.D.; Desnick, L.M.; D’orsi, C.J.; Ransohoff, D.F. International variation in screening mammography interpretations in community-based programs. J. Natl. Cancer Inst. 2003, 95, 1384–1393. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hansen, N.J.; Lohman, T.G.; Going, S.B.; Hall, M.C.; Pamenter, R.W.; Bare, L.A.; Boyden, T.W.; Houtkooper, L.B. Prediction of body composition in premenopausal females from dual-energy X-ray absorptiometry. J. Appl. Physiol. 1993, 75, 1637–1641. [Google Scholar] [CrossRef]
- Wellens, R.; Chumlea, W.C.; Guo, S.; Roche, A.F.; Reo, N.V.; Siervogel, R.M. Body composition in white adults by dual-energy x-ray absorptiometry, densitometry, and total body water. Am. J. Clin. Nutr. 1994, 59, 547–555. [Google Scholar]
- Picaud, J.-C.; Rigo, J.; Nyamugabo, K.; Milet, J.; Senterre, J. Evaluation of dual-energy X-ray absorptiometry for body-composition assessment in piglets and term human neonates. Am. J. Clin. Nutr. 1996, 63, 157–163. [Google Scholar] [CrossRef]
- Svendsen, O.L.; Haarbo, J.; Hassager, C.; Christiansen, C. Accuracy of measurements of body composition by dual-energy x-ray absorptiometry in vivo. Am. J. Clin. Nutr. 1993, 57, 605–608. [Google Scholar] [CrossRef]
- Maden-Wilkinson, T.; Degens, H.; Jones, D.; McPhee, J. Comparison of MRI and DXA to measure muscle size and age-related atrophy in thigh muscles. J. Musculoskelet. Neuronal Interact. 2013, 13, 320–328. [Google Scholar]
- Bredella, M.A.; Ghomi, R.H.; Thomas, B.J.; Torriani, M.; Brick, D.J.; Gerweck, A.V.; Misra, M.; Klibanski, A.; Miller, K.K. Comparison of DXA and CT in the assessment of body composition in premenopausal women with obesity and anorexia nervosa. Obesity 2010, 18, 2227–2233. [Google Scholar] [CrossRef] [Green Version]
- Levine, J.A.; Abboud, L.; Barry, M.; Reed, J.E.; Sheedy, P.F.; Jensen, M.D. Measuring leg muscle and fat mass in humans: Comparison of CT and dual-energy X-ray absorptiometry. J. Appl. Physiol. 2000, 88, 452–456. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, W.; Wang, Z.; Faith, M.S.; Kotler, D.; Shih, R.; Heymsfield, S.B. Regional skeletal muscle measurement: Evaluation of new dual-energy X-ray absorptiometry model. J. Appl. Physiol. 1999, 87, 1163–1171. [Google Scholar] [CrossRef] [PubMed]
- Glickman, S.G.; Marn, C.S.; Supiano, M.A.; Dengel, D.R. Validity and reliability of dual-energy X-ray absorptiometry for the assessment of abdominal adiposity. J. Appl. Physiol. 2004, 97, 509–514. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Locquet, M.; Beaudart, C.; Reginster, J.-Y.; Petermans, J.; Bruyère, O. Comparison of the performance of five screening methods for sarcopenia. Clin. Epidemiol. 2018, 10, 71–82. [Google Scholar] [CrossRef] [Green Version]
- Kohrt, W.M. Dual-Energy X-ray Absorptiometry: Research Issues and Equipment; Carlson-Newberry, S.J., Costello, R.B., Eds.; National Academies Press (US): Washington, DC, USA, 1997; Volume 6, p. 151. [Google Scholar]
- Delmas, P.; Fontanges, E.; Duboeuf, F.; Boivin, G.; Chavassieux, P.; Meunier, P. Comparison of bone mass measured by histomorphometry on iliac biopsy and by dual photon absorptiometry of the lumbar spine. Bone 1988, 9, 209–213. [Google Scholar] [CrossRef]
- Wright, C.; Crawley, E.; Evans, W.; Garrahan, N.; Mellish, R.; Croucher, P.; Compston, J. The relationship between spinal trabecular bone mineral content and iliac crest trabecular bone volume. Calcif. Tissue Int. 1990, 46, 162–165. [Google Scholar] [CrossRef]
- Cosman, F.; Schnitzer, M.; McCann, P.; Parisien, M.; Dempster, D.; Lindsay, R. Relationships between quantitative histological measurements and noninvasive assessments of bone mass. Bone 1992, 13, 237–242. [Google Scholar] [CrossRef]
- Jindal, M.; Lakhwani, O.P.; Kaur, O.; Agarwal, S.; Garg, K. Bone Density versus Bone Quality as a Predictor of Bone Strength. Orthop. Rheumatol. Open Access J. 2018, 12, 555830. [Google Scholar] [CrossRef] [Green Version]
- Humadi, A.; Alhadithi, R.H.; Alkudiari, S.I. Validity of the DEXA diagnosis of involutional osteoporosis in patients with femoral neck fractures. Indian J. Orthop. 2010, 44, 73–78. [Google Scholar] [CrossRef]
- Genant, H.K.; Engelke, K.; Fuerst, T.; Glüer, C.C.; Grampp, S.; Harris, S.T.; Jergas, M.; Lang, T.; Lu, Y.; Majumdar, S.; et al. Noninvasive assessment of bone mineral and structure: State of the art. J. Bone Miner. Res. 1996, 11, 707–730. [Google Scholar] [CrossRef]
- Kabel, J.; van Rietbergen, B.; Dalstra, M.; Odgaard, A.; Huiskes, R. The role of an effective isotropic tissue modulus in the elastic properties of cancellous bone. J. Biomech. 1999, 32, 673–680. [Google Scholar] [CrossRef]
- Homminga, J.; Mccreadie, B.R.; Weinans, H.; Huiskes, R. The dependence of the elastic properties of osteoporotic cancellous bone on volume fraction and fabric. J. Biomech. 2003, 36, 1461–1467. [Google Scholar] [CrossRef]
- Berg, W.A.; Blume, J.D.; Cormack, J.B.; Mendelson, E.B.; Lehrer, D.; Böhm-Vélez, M.; Pisano, E.D.; Jong, R.A.; Evans, W.P.; Morton, M.J.; et al. Combined screening with ultrasound and mammography vs mammography alone in women at elevated risk of breast cancer. JAMA 2008, 299, 2151–2163. [Google Scholar] [CrossRef] [PubMed]
- Health Quality Ontario. Ultrasound as an adjunct to mammography for breast cancer screening: A health technology assessment. Ont. Health Technol. Assess. Ser. 2016, 16, 1–71. [Google Scholar]
- Kolb, T.M.; Lichy, J.; Newhouse, J.H. Comparison of the performance of screening mammography, physical examination, and breast US and evaluation of factors that influence them: An analysis of 27,825 patient evaluations. Radiology 2002, 225, 165–175. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ciatto, S.; Houssami, N.; Ambrogetti, D.; Bonardi, R.; Collini, G.; Del Turco, M.R. Minority report–false negative breast assessment in women recalled for suspicious screening mammography: Imaging and pathological features, and associated delay in diagnosis. Breast Cancer Res. Treat. 2007, 105, 37–43. [Google Scholar] [CrossRef]
- Buchberger, W.; Niehoff, A.; Obrist, P.; DeKoekkoek-Doll, P.; Dünser, M. Clinically and mammographically occult breast lesions: Detection and classification with high-resolution sonography. Semin. Ultrasound CT MRI 2000, 21, 325–336. [Google Scholar] [CrossRef]
- Kaplan, S.S. Clinical utility of bilateral whole-breast US in the evaluation of women with dense breast tissue. Radiology 2001, 221, 641–649. [Google Scholar] [CrossRef]
- Weigert, J.; Steenbergen, S. The Connecticut experiment: The role of ultrasound in the screening of women with dense breasts. Breast J. 2012, 18, 517–522. [Google Scholar] [CrossRef]
- Berg, W.A.; Zhang, Z.; Lehrer, D.; Jong, R.A.; Pisano, E.D.; Barr, R.G.; Böhm-Vélez, M.; Mahoney, M.C.; Evans, W.P.; Larsen, L.H. Detection of breast cancer with addition of annual screening ultrasound or a single screening MRI to mammography in women with elevated breast cancer risk. JAMA 2012, 307, 1394–1404. [Google Scholar]
- Berg, W.A.; Blume, J.D.; Cormack, J.B.; Mendelson, E.B. Operator dependence of physician-performed whole-breast US: Lesion detection and characterization. Radiology 2006, 241, 355–365. [Google Scholar] [CrossRef] [PubMed]
- Deer, R.R.; Akhverdiyeva, L.; Kuo, Y.-F.; Volpi, E. Developing a screening tool for sarcopenia in hospitalized geriatric patients: Estimation of appendicular skeletal muscle mass using bioelectrical impedance. Clin. Nutr. 2019, 39, 2233–2237. [Google Scholar] [CrossRef] [PubMed]
- Buckinx, F.; Reginster, J.-Y.; Dardenne, N.; Croisiser, J.-L.; Kaux, J.-F.; Beaudart, C.; Slomian, J.; Bruyère, O. Concordance between muscle mass assessed by bioelectrical impedance analysis and by dual energy X-ray absorptiometry: A cross-sectional study. BMC Musculoskelet. Disord. 2015, 16, 60. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Regione del Veneto. Tariffario Unico Regionale. Available online: https://www.regione.veneto.it/web/sanita/tariffario-unico-regionale (accessed on 13 December 2011).
- Lauretani, F.; Russo, C.R.; Bandinelli, S.; Bartali, B.; Cavazzini, C.; Di Iorio, A.; Corsi, A.M.; Rantanen, T.; Guralnik, J.M.; Ferrucci, L. Age-associated changes in skeletal muscles and their effect on mobility: An operational diagnosis of sarcopenia. J. Appl. Physiol. 2003, 95, 1851–1860. [Google Scholar] [CrossRef] [PubMed]
- Nabuco, H.C.; Tomeleri, C.M.; Fernandes, R.R.; Sugihara Junior, P.; Venturini, D.; Barbosa, D.S.; Deminice, R.; Sardinha, L.B.; Cyrino, E.S. Effects of pre-or post-exercise whey protein supplementation on oxidative stress and antioxidant enzymes in older women. Scand. J. Med. Sci. Sports 2019, 29, 1101–1108. [Google Scholar] [CrossRef]
- Sugihara Junior, P.; Ribeiro, A.S.; Nabuco, H.C.; Fernandes, R.R.; Tomeleri, C.M.; Cunha, P.M.; Venturini, D.; Barbosa, D.S.; Schoenfeld, B.J.; Cyrino, E.S. Effects of whey protein supplementation associated with resistance training on muscular strength, hypertrophy, and muscle quality in preconditioned older women. Int. J. Sport Nutr. Exerc. Metab. 2018, 28, 528–535. [Google Scholar] [CrossRef]
- Mori, H.; Tokuda, Y. Effect of whey protein supplementation after resistance exercise on the muscle mass and physical function of healthy older women: A randomized controlled trial. Geriatr. Gerontol. Int. 2018, 18, 1398–1404. [Google Scholar] [CrossRef] [Green Version]
- Englund, D.A.; Kirn, D.R.; Koochek, A.; Zhu, H.; Travison, T.G.; Reid, K.F.; von Berens, Å.; Melin, M.; Cederholm, T.; Gustafsson, T. Nutritional supplementation with physical activity improves muscle composition in mobility-limited older adults, the VIVE2 study: A randomized, double-blind, placebo-controlled trial. J. Gerontol. Ser. A 2017, 73, 95–101. [Google Scholar] [CrossRef]
- Fielding, R.A.; Travison, T.G.; Kirn, D.R.; Koochek, A.; Reid, K.F.; von Berens, Å.; Zhu, H.; Folta, S.C.; Sacheck, J.M.; Nelson, M.E.; et al. Effect of structured physical activity and nutritional supplementation on physical function in mobility-limited older adults: Results from the VIVE2 randomized trial. J. Nutr. Health Aging 2017, 21, 936–942. [Google Scholar] [CrossRef]
- Chalé, A.; Cloutier, G.J.; Hau, C.; Phillips, E.M.; Dallal, G.E.; Fielding, R.A. Efficacy of whey protein supplementation on resistance exercise–induced changes in lean mass, muscle strength, and physical function in mobility-limited older adults. J. Gerontol. Ser. A Biomed. Sci. Med. Sci. 2013, 68, 682–690. [Google Scholar] [CrossRef] [Green Version]
- Kirk, B.; Mooney, K.; Amirabdollahian, F.; Khaiyat, O. Exercise and Dietary-Protein as a Countermeasure to Skeletal Muscle Weakness Liverpool Hope University-Sarcopenia Ageing Trial (LHU-SAT). Front. Physiol. 2019, 10, 445. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kirk, B.; Mooney, K.; Cousins, R.; Angell, P.; Jackson, M.; Pugh, J.N.; Coyles, G.; Amirabdollahian, F.; Khaiyat, O. Effects of exercise and whey protein on muscle mass, fat mass, myoelectrical muscle fatigue and health-related quality of life in older adults: A secondary analysis of the Liverpool Hope University—Sarcopenia Ageing Trial (LHU-SAT). Eur. J. Appl. Physiol. 2020, 120, 493–503. [Google Scholar] [CrossRef] [PubMed]
- Niccoli, S.; Kolobov, A.; Bon, T.; Rafilovich, S.; Munro, H.; Tanner, K.; Pearson, T.; Lees, S.J. Whey protein supplementation improves rehabilitation outcomes in hospitalized geriatric patients: A double blinded, randomized controlled trial. J. Nutr. Gerontol. Geriatr. 2017, 36, 149–165. [Google Scholar] [CrossRef] [PubMed]
- Gade, J.; Beck, A.M.; Bitz, C.; Christensen, B.; Klausen, T.W.; Vinther, A.; Astrup, A. Protein-enriched, milk-based supplement to counteract sarcopenia in acutely ill geriatric patients offered resistance exercise training during and after hospitalisation: Study protocol for a randomised, double-blind, multicentre trial. BMJ Open 2018, 8, e019210. [Google Scholar] [CrossRef]
- Gade, J.; Beck, A.M.; Andersen, H.E.; Christensen, B.; Rønholt, F.; Klausen, T.W.; Vinther, A.; Astrup, A. Protein supplementation combined with low-intensity resistance training in geriatric medical patients during and after hospitalisation: A randomised, double-blind, multicentre trial. Br. J. Nutr. 2019, 122, 1006–1020. [Google Scholar] [CrossRef]
- Mancuso, M.; Orsucci, D.; LoGerfo, A.; Rocchi, A.; Petrozzi, L.; Nesti, C.; Galetta, F.; Santoro, G.; Murri, L.; Siciliano, G. Oxidative stress biomarkers in mitochondrial myopathies, basally and after cysteine donor supplementation. J. Neurol. 2010, 257, 774–781. [Google Scholar] [CrossRef]
- Carbone, J.W.; Pasiakos, S.M. Dietary Protein and Muscle Mass: Translating Science to Application and Health Benefit. Nutrients 2019, 11, 1136. [Google Scholar] [CrossRef] [Green Version]
- Wolfe, R.R.; Miller, S.L.; Miller, K.B. Optimal protein intake in the elderly. Clin. Nutr. 2008, 27, 675–684. [Google Scholar] [CrossRef]
- Volpi, E.; Campbell, W.W.; Dwyer, J.T.; Johnson, M.A.; Jensen, G.L.; Morley, J.E.; Wolfe, R.R. Is the optimal level of protein intake for older adults greater than the recommended dietary allowance? J. Gerontol. Ser. A Biomed. Sci. Med. Sci. 2013, 68, 677–681. [Google Scholar] [CrossRef] [Green Version]
- Fulgoni, V.L., III. Current protein intake in America: Analysis of the National Health and Nutrition Examination Survey, 2003–2004. Am. J. Clin. Nutr. 2008, 87, 1554S–1557S. [Google Scholar] [CrossRef] [Green Version]
- Pasiakos, S.M.; Agarwal, S.; Lieberman, H.R.; Fulgoni, V.L. Sources and amounts of animal, dairy, and plant protein intake of US adults in 2007–2010. Nutrients 2015, 7, 7058–7069. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Coelho-Junior, H.J.; Calvani, R.; Picca, A.; Gonçalves, I.O.; Landi, F.; Bernabei, R.; Cesari, M.; Uchida, M.C.; Marzetti, E. Association between Dietary Habits and Physical Function in Brazilian and Italian Older Women. Nutrients 2020, 12, 1635. [Google Scholar] [CrossRef] [PubMed]
- Houston, D.K.; Nicklas, B.J.; Ding, J.; Harris, T.B.; Tylavsky, F.A.; Newman, A.B.; Lee, J.S.; Sahyoun, N.R.; Visser, M.; Kritchevsky, S.B. Dietary protein intake is associated with lean mass change in older, community-dwelling adults: The Health, Aging, and Body Composition (Health ABC) Study. Am. J. Clin. Nutr. 2008, 87, 150–155. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhao, J.X.; Liu, X.D.; Li, K.; Liu, W.Z.; Ren, Y.S.; Zhang, J.X. Different dietary energy intake affects skeletal muscle development through an Akt-dependent pathway in Dorper × small thin-tailed crossbred ewe lambs. Domest. Anim. Endocrinol. 2016, 57, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, C.J.; Della Gatta, P.A.; Petersen, A.C.; Cameron-Smith, D.; Markworth, J.F. Soy protein ingestion results in less prolonged p70S6 kinase phosphorylation compared to whey protein after resistance exercise in older men. J. Int. Soc. Sports Nutr. 2015, 12, 6. [Google Scholar] [CrossRef] [Green Version]
- Phillips, S.M.; Tang, J.E.; Moore, D.R. The role of milk-and soy-based protein in support of muscle protein synthesis and muscle protein accretion in young and elderly persons. J. Am. Coll. Nutr. 2009, 28, 343–354. [Google Scholar] [CrossRef]
- Tang, J.E.; Moore, D.R.; Kujbida, G.W.; Tarnopolsky, M.A.; Phillips, S.M. Ingestion of whey hydrolysate, casein, or soy protein isolate: Effects on mixed muscle protein synthesis at rest and following resistance exercise in young men. J. Appl. Physiol. 2009, 107, 987–992. [Google Scholar] [CrossRef]
- Mattick, J.S.; Kamisoglu, K.; Ierapetritou, M.G.; Androulakis, I.P.; Berthiaume, F. Branched-chain amino acid supplementation: Impact on signaling and relevance to critical illness. Wiley Interdiscip. Rev. Syst. Biol. Med. 2013, 5, 449–460. [Google Scholar] [CrossRef] [Green Version]
- Gilmartin, S.; O’Brien, N.; Giblin, L. Whey for Sarcopenia; Can Whey Peptides, Hydrolysates or Proteins Play a Beneficial Role? Foods 2020, 9, 750. [Google Scholar] [CrossRef]
- Nabuco, H.C.; Tomeleri, C.M.; Sugihara Junior, P.; Fernandes, R.R.; Cavalcante, E.F.; Antunes, M.; Ribeiro, A.S.; Teixeira, D.C.; Silva, A.M.; Sardinha, L.B. Effects of whey protein supplementation pre-or post-resistance training on muscle mass, muscular strength, and functional capacity in pre-conditioned older women: A randomized clinical trial. Nutrients 2018, 10, 563. [Google Scholar] [CrossRef] [Green Version]
- Chanet, A.; Verlaan, S.; Salles, J.; Giraudet, C.; Patrac, V.; Pidou, V.; Pouyet, C.; Hafnaoui, N.; Blot, A.; Cano, N.; et al. Supplementing breakfast with a vitamin D and leucine–enriched whey protein medical nutrition drink enhances postprandial muscle protein synthesis and muscle mass in healthy older men. J. Nutr. 2017, 147, 2262–2271. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ascenzi, F.; Barberi, L.; Dobrowolny, G.; Villa Nova Bacurau, A.; Nicoletti, C.; Rizzuto, E.; Rosenthal, N.; Scicchitano, B.M.; Musarò, A. Effects of IGF-1 isoforms on muscle growth and sarcopenia. Aging Cell 2019, 18, e12954. [Google Scholar] [CrossRef] [PubMed]
- Rodondi, A.; Ammann, P.; Ghilardi-Beuret, S.; Rizzoli, R. Zinc increases the effects of essential amino acids-whey protein supplements in frail elderly. JNHA J. Nutr. Health Aging 2009, 13, 491–497. [Google Scholar] [CrossRef] [PubMed]
- Nabuco, H.C.; Tomeleri, C.M.; Fernandes, R.R.; Junior, P.S.; Cavalcante, E.F.; Cunha, P.M.; Antunes, M.; Nunes, J.P.; Venturini, D.; Barbosa, D.S.; et al. Effect of whey protein supplementation combined with resistance training on body composition, muscular strength, functional capacity, and plasma-metabolism biomarkers in older women with sarcopenic obesity: A randomized, double-blind, placebo-controlled trial. Clin. Nutr. ESPEN 2019, 32, 88–95. [Google Scholar] [PubMed]
- Morton, R.W.; Murphy, K.T.; McKellar, S.R.; Schoenfeld, B.J.; Henselmans, M.; Helms, E.; Aragon, A.A.; Devries, M.C.; Banfield, L.; Krieger, J.W.; et al. A systematic review, meta-analysis and meta-regression of the effect of protein supplementation on resistance training-induced gains in muscle mass and strength in healthy adults. Br. J. Sports Med. 2018, 52, 376–384. [Google Scholar] [CrossRef]
- Darling, A.; Manders, R.; Sahni, S.; Zhu, K.; Hewitt, C.E.; Prince, R.L.; Millward, D.; Lanham-New, S. Dietary protein and bone health across the life-course: An updated systematic review and meta-analysis over 40 years. Osteoporos. Int. 2019, 30, 741–761. [Google Scholar] [CrossRef] [Green Version]
- Wallace, T.C.; Frankenfeld, C.L. Dietary protein intake above the current RDA and bone health: A systematic review and meta-analysis. J. Am. Coll. Nutr. 2017, 36, 481–496. [Google Scholar] [CrossRef] [Green Version]
- Oktaviana, J.; Zanker, J.; Vogrin, S.; Duque, G. The Effect of β-hydroxy-β-methylbutyrate (HMB) on Sarcopenia and Functional Frailty in Older Persons: A Systematic Review. J. Nutr. Health Aging 2019, 23, 145–150. [Google Scholar] [CrossRef]
- Chakhtoura, M.; Chamoun, N.; Rahme, M.; Fuleihan, G.E.-H. Impact of vitamin D supplementation on falls and fractures—A critical appraisal of the quality of the evidence and an overview of the available guidelines. Bone 2020, 131, 115112. [Google Scholar] [CrossRef]
- Bruyère, O.; Cavalier, E.; Reginster, J.-Y. Vitamin D and osteosarcopenia: An update from epidemiological studies. Curr. Opin. Clin. Nutr. Metab. Care 2017, 20, 498–503. [Google Scholar] [CrossRef] [Green Version]
- Beaudart, C.; Buckinx, F.; Rabenda, V.; Gillain, S.; Cavalier, E.; Slomian, J.; Petermans, J.; Reginster, J.-Y.; Bruyère, O. The effects of vitamin D on skeletal muscle strength, muscle mass, and muscle power: A systematic review and meta-analysis of randomized controlled trials. J. Clin. Endocrinol. Metab. 2014, 99, 4336–4345. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kelley, G.A.; Kelley, K.S.; Tran, Z.V. Resistance training and bone mineral density in women: A meta-analysis of controlled trials. Am. J. Phys. Med. Rehabil. 2001, 80, 65–77. [Google Scholar] [CrossRef] [PubMed]
- Layne, J.E.; Nelson, M.E. The effects of progressive resistance training on bone density: A review. Med. Sci. Sports Exerc. 1999, 31, 25–30. [Google Scholar] [CrossRef]
- Martyn-St James, M.; Carroll, S. High-intensity resistance training and postmenopausal bone loss: A meta-analysis. Osteoporos. Int. 2006, 17, 1225–1240. [Google Scholar] [CrossRef] [PubMed]
- Senderovich, H.; Kosmopoulos, A. An insight into the effect of exercises on the prevention of osteoporosis and associated fractures in high-risk individuals. Rambam Maimonides Med. J. 2018, 9, e0005. [Google Scholar] [CrossRef] [Green Version]
- Nelson, M.E.; Fiatarone, M.A.; Morganti, C.M.; Trice, I.; Greenberg, R.A.; Evans, W.J. Effects of high-intensity strength training on multiple risk factors for osteoporotic fractures: A randomized controlled trial. JAMA 1994, 272, 1909–1914. [Google Scholar] [CrossRef]
- Souza, D.; Barbalho, M.; Ramirez-Campillo, R.; Martins, W.; Gentil, P. High and low-load resistance training produce similar effects on bone mineral density of middle-aged and older people: A systematic review with meta-analysis of randomized clinical trials. Exp. Gerontol. 2020, 138, 110973. [Google Scholar] [CrossRef]
- Daly, R.M.; Gianoudis, J.; Kersh, M.E.; Bailey, C.A.; Ebeling, P.R.; Krug, R.; Nowson, C.A.; Hill, K.; Sanders, K.M. Effects of a 12-month supervised, community-based, multimodal exercise program followed by a 6-month research-to-practice transition on bone mineral density, trabecular microarchitecture, and physical function in older adults: A randomized controlled trial. J. Bone Miner. Res. 2020, 35, 419–429. [Google Scholar] [CrossRef]
- Hita-Contreras, F.; Bueno-Notivol, J.; Martínez-Amat, A.; Cruz-Díaz, D.; Hernandez, A.V.; Pérez-López, F.R. Effect of exercise alone or combined with dietary supplements on anthropometric and physical performance measures in community-dwelling elderly people with sarcopenic obesity: A meta-analysis of randomized controlled trials. Maturitas 2018, 116, 24–35. [Google Scholar] [CrossRef] [Green Version]
- Martínez-Amat, A.; Aibar-Almazán, A.; Fábrega-Cuadros, R.; Cruz-Díaz, D.; Jiménez-García, J.D.; Pérez-López, F.R.; Achalandabaso, A.; Barranco-Zafra, R.; Hita-Contreras, F. Exercise alone or combined with dietary supplements for sarcopenic obesity in community-dwelling older people: A systematic review of randomized controlled trials. Maturitas 2018, 110, 92–103. [Google Scholar] [CrossRef]
- Yin, Y.-H.; Liu, J.Y.W.; Välimäki, M. Effectiveness of non-pharmacological interventions on the management of sarcopenic obesity: A systematic review and meta-analysis. Exp. Gerontol. 2020, 135, 110937. [Google Scholar] [CrossRef] [PubMed]
- Hsu, K.J.; Liao, C.D.; Tsai, M.W.; Chen, C.N. Effects of Exercise and Nutritional Intervention on Body Composition, Metabolic Health, and Physical Performance in Adults with Sarcopenic Obesity: A Meta-Analysis. Nutrients 2019, 11, 2163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Muscariello, E.; Nasti, G.; Siervo, M.; Di Maro, M.; Lapi, D.; D’Addio, G.; Colantuoni, A. Dietary protein intake in sarcopenic obese older women. Clin. Interv. Aging 2016, 11, 133–140. [Google Scholar] [CrossRef] [PubMed] [Green Version]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Montalcini, T.; Pujia, A.; Donini, L.M.; Frittitta, L.; Galvano, F.; Natali, A.; Pironi, L.; Porrini, M.; Riso, P.; Rivellese, A.A.; et al. A Call to Action: Now Is the Time to Screen Elderly and Treat Osteosarcopenia, a Position Paper of the Italian College of Academic Nutritionists MED/49 (ICAN-49). Nutrients 2020, 12, 2662. https://doi.org/10.3390/nu12092662
Montalcini T, Pujia A, Donini LM, Frittitta L, Galvano F, Natali A, Pironi L, Porrini M, Riso P, Rivellese AA, et al. A Call to Action: Now Is the Time to Screen Elderly and Treat Osteosarcopenia, a Position Paper of the Italian College of Academic Nutritionists MED/49 (ICAN-49). Nutrients. 2020; 12(9):2662. https://doi.org/10.3390/nu12092662
Chicago/Turabian StyleMontalcini, Tiziana, Arturo Pujia, Lorenzo M. Donini, Lucia Frittitta, Fabio Galvano, Andrea Natali, Loris Pironi, Marisa Porrini, Patrizia Riso, Angela Albarosa Rivellese, and et al. 2020. "A Call to Action: Now Is the Time to Screen Elderly and Treat Osteosarcopenia, a Position Paper of the Italian College of Academic Nutritionists MED/49 (ICAN-49)" Nutrients 12, no. 9: 2662. https://doi.org/10.3390/nu12092662






