Multiple Micronutrients and Docosahexaenoic Acid Supplementation during Pregnancy: A Randomized Controlled Study
Abstract
1. Introduction
2. Materials and Methods
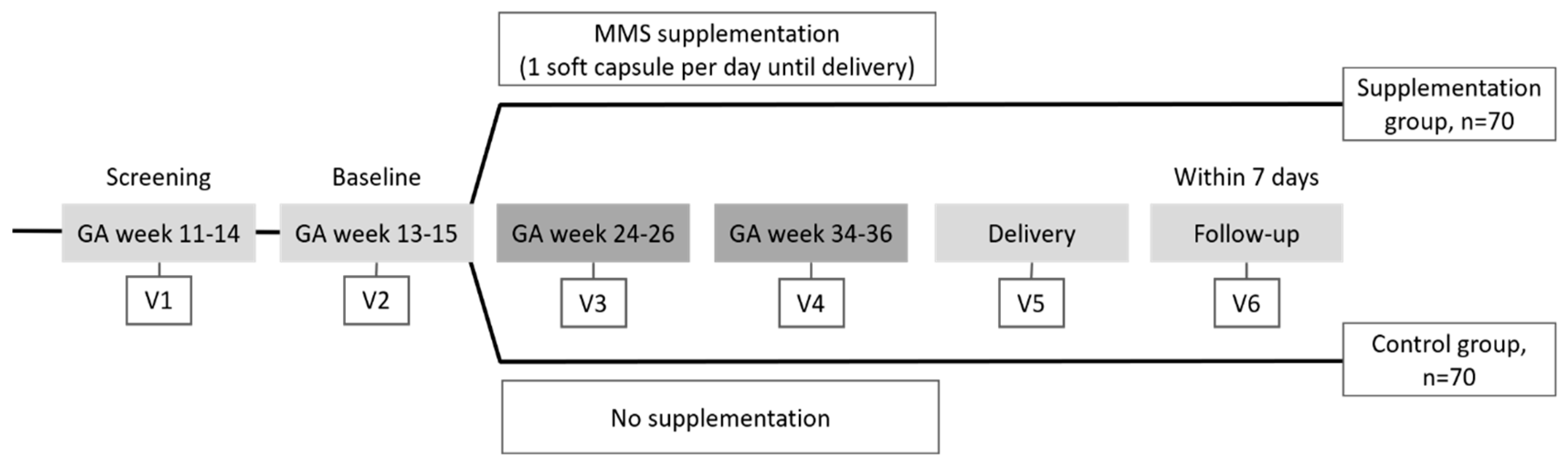
2.1. Trial Design
2.2. Study Population
2.3. Study Product
2.4. Parameters Assessed
2.5. Statistical Analysis
3. Results
3.1. Subject Characteristics
3.2. Efficacy Endpoints
3.3. Safety Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Cazzola, R.; Russo-Volpe, S.; Miles, E.A.; Rees, D.; Banerjee, T.; Roynette, C.E.; Wells, S.J.; Goua, M.; Wahle, K.W.; Calder, P.C.; et al. Age-and dose-dependent effects of an eicosapentaenoic acid-rich oil on cardiovascular risk factors in healthy male subjects. Atherosclerosis 2007, 193, 159–167. [Google Scholar] [CrossRef] [PubMed]
- Institute of Medicine. Dietary Reference Intakes for Calcium and Vitamin D; The National Academies Press: Washington, DC, USA, 2011. [Google Scholar]
- Ramakrishnan, U.; Grant, F.K.; Goldenberg, T.; Bui, V.; Imdad, A.; Bhutta, Z.A. Effect of Multiple Micronutrient Supplementation on Pregnancy and Infant Outcomes: A Systematic Review. Paediatr. Perinat. Epidemiol. 2012, 26, 153–167. [Google Scholar] [CrossRef] [PubMed]
- Cetin, I.; Bühling, K.; Demir, C.; Kortam, A.; Prescott, S.L.; Yamashiro, Y.; Yarmolinskaya, M.; Koletzko, B. Impact of Micronutrient Status during Pregnancy on Early Nutrition Programming. Ann. Nutr. Metab. 2019, 74, 269–278. [Google Scholar] [CrossRef]
- Berti, C.; Cetin, I.; Agostoni, C.; Desoye, G.; Devlieger, R.; Emmett, P.M.; Ensenauer, R.; Hauner, H.; Herrera, E.; Hoesli, I.; et al. Pregnancy and Infants’ Outcome: Nutritional and Metabolic Implications. Crit. Rev. Food Sci. Nutr. 2014, 56, 82–91. [Google Scholar] [CrossRef] [PubMed]
- Cetin, I.; Berti, C.; Calabrese, S. Role of micronutrients in the periconceptional period. Hum. Reprod. Updat. 2009, 16, 80–95. [Google Scholar] [CrossRef]
- Ramakrishnan, U.; Grant, F.; Goldenberg, T.; Zongrone, A.; Martorell, R. Effect of women’s nutrition before and during early pregnancy on maternal and infant outcomes: A systematic review. Paediatr. Perinat. Epidemiol. 2012, 26, 285–301. [Google Scholar] [CrossRef]
- Blumfield, M.L.; Hure, A.; Smith, R.; Collins, C.E.; MacDonald-Wicks, L. A systematic review and meta-analysis of micronutrient intakes during pregnancy in developed countries. Nutr. Rev. 2013, 71, 118–132. [Google Scholar] [CrossRef]
- Elmadfa, I.; Meyer, A.; Nowak, V.; Hasenegger, V.; Putz, P.; Verstraeten, R.; Remaut-DeWinter, A.M. European Nutrition and Health Report; Karger Medical and Scientific Publishers: Basel, Switzerland, 2009; Volume 62, pp. 1–405. [Google Scholar]
- Parisi, F.; Laoreti, A.; Cetin, I. Multiple Micronutrient Needs in Pregnancy in Industrialized Countries. Ann. Nutr. Metab. 2014, 65, 13–21. [Google Scholar] [CrossRef]
- Gernand, A.D.; Schulze, K.J.; Stewart, C.P.; West, K.P.; Christian, P. Micronutrient deficiencies in pregnancy worldwide: Health effects and prevention. Nat. Rev. Endocrinol. 2016, 12, 274–289. [Google Scholar] [CrossRef]
- Schaefer, E. Micronutrient Deficiency in Women Living in Industrialized Countries during the Reproductive Years: Is there a Basis for Supplementation with Multiple Micronutrients? J. Nutr. Disord. Ther. 2016, 6. [Google Scholar] [CrossRef]
- World Health Organization; e-Library of Evidence for Nutrition Actions (eLENA). Daily Iron and Folic Acid Supplementation during Pregnancy. Available online: https://www.who.int/elena/titles/guidance_summaries/daily_iron_pregnancy/en/ (accessed on 31 July 2020).
- Institute of Medicine (US) Standing Committee on the Scientific Evaluation of Dietary Reference Intakes. Dietary Reference Intakes for Calcium, Phosphorus, Magnesium, Vitamin D, and Fluoride. 7, Vitamin D; National Academies Press: Washington, DC, USA, 1997. Available online: https://www.ncbi.nlm.nih.gov/books/NBK109831/. (accessed on 31 July 2020).
- Mulligan, M.L.; Felton, S.K.; Riek, A.E.; Bernal-Mizrachi, C. Implications of vitamin D deficiency in pregnancy and lactation. Am. J. Obstet. Gynecol. 2010, 202, e421–e429. [Google Scholar] [CrossRef]
- Dovnik, A.; Mujezinović, F. The Association of Vitamin D Levels with Common Pregnancy Complications. Nutrients 2018, 10, 867. [Google Scholar] [CrossRef] [PubMed]
- Rees, A.; Sirois, S.; Wearden, A. Prenatal maternal docosahexaenoic acid intake and infant information processing at 4.5mo and 9mo: A longitudinal study. PLoS ONE 2019, 14, e0210984. [Google Scholar] [CrossRef] [PubMed]
- Agostoni, C.; Nobile, M.; Ciappolino, V.; DelVecchio, G.; Tesei, A.; Turolo, S.; Crippa, A.; Mazzocchi, A.; Altamura, C.A.; Brambilla, P. The Role of Omega-3 Fatty Acids in Developmental Psychopathology: A Systematic Review on Early Psychosis, Autism, and ADHD. Int. J. Mol. Sci. 2017, 18, 2608. [Google Scholar] [CrossRef] [PubMed]
- Echeverría, F.; Valenzuela, R.; Hernandez-Rodas, M.C.; Valenzuela, A. Docosahexaenoic acid (DHA), a fundamental fatty acid for the brain: New dietary sources. Prostaglandins Leukot. Essent. Fat. Acids 2017, 124, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Weiser, M.J.; Butt, C.M.; Mohajeri, M.H. Docosahexaenoic Acid and Cognition throughout the Lifespan. Nutrients 2016, 8, 99. [Google Scholar] [CrossRef]
- Darnell, D.; Gilbert, S.F. Neuroembryology. Wiley Interdiscip. Rev. Dev. Biol. 2016, 6, e215. [Google Scholar] [CrossRef]
- Delgado-Noguera, M.F.; Calvache, J.A.; Cosp, X.B.; Kotanidou, E.P.; Galli-Tsinopoulou, A. Supplementation with long chain polyunsaturated fatty acids (LCPUFA) to breastfeeding mothers for improving child growth and development. Cochrane Database Syst. Rev. 2015, CD007901. [Google Scholar] [CrossRef]
- Carlson, S.E.; Colombo, J. Docosahexaenoic Acid and Arachidonic Acid Nutrition in Early Development. Adv. Pediatr. 2016, 63, 453–471. [Google Scholar] [CrossRef]
- Innis, S.M. The Role of Dietary n–6 and n–3 Fatty Acids in the Developing Brain. Dev. Neurosci. 2000, 22, 474–480. [Google Scholar] [CrossRef]
- Al, M.D.M.; Van Houwelingen, A.C.; Kester, A.D.; Hasaart, T.H.; De Jong, A.E.P.; Hornstra, G. Maternal essential fatty acid patterns during normal pregnancy and their relationship to the neonatal essential fatty acid status. Br. J. Nutr. 1995, 74, 55–68. [Google Scholar] [CrossRef] [PubMed]
- Grantham-McGregor, S.; Cheung, Y.B.; Cueto, S.; Glewwe, P.; Richter, L.; Strupp, B. Developmental potential in the first 5 years for children in developing countries. Lancet 2007, 369, 60–70. [Google Scholar] [CrossRef]
- McCann, J.C.; Ames, B.N. Is docosahexaenoic acid, an n-3 long-chain polyunsaturated fatty acid, required for development of normal brain function? An overview of evidence from cognitive and behavioral tests in humans and animals. Am. J. Clin. Nutr. 2005, 82, 281–295. [Google Scholar] [CrossRef] [PubMed]
- Innis, S.M. Perinatal biochemistry and physiology of long-chain polyunsaturated fatty acids. J. Pediatr. 2003, 143, 1–8. [Google Scholar] [CrossRef]
- Englund-Ögge, L.; Brantsæter, A.; Sengpiel, V.; Haugen, M.; Birgisdottir, B.E.; Myhre, R.; Meltzer, H.M.; Jacobsson, B. Maternal dietary patterns and preterm delivery: Results from large prospective cohort study. BMJ 2014, 348, g1446. [Google Scholar] [CrossRef]
- Larqué, E.; Gil-Sánchez, A.; Prieto-Sánchez, M.T.; Koletzko, B. Omega 3 fatty acids, gestation and pregnancy outcomes. Br. J. Nutr. 2012, 107 (Suppl. 2), S77–S84. [Google Scholar] [CrossRef]
- Rogers, L.K.; Valentine, C.J.; Keim, S.A. DHA supplementation: Current implications in pregnancy and childhood. Pharmacol. Res. 2012, 70, 13–19. [Google Scholar] [CrossRef]
- Larqué, E.; Krauss-Etschmann, S.; Campoy, C.; Hartl, D.; Linde, J.; Klingler, M.; Demmelmair, H.; Caño, A.; Gil, A.; Bondy, B.; et al. Docosahexaenoic acid supply in pregnancy affects placental expression of fatty acid transport proteins. Am. J. Clin. Nutr. 2006, 84, 853–861. [Google Scholar] [CrossRef]
- Decsi, T.; Campoy, C.; Koletzko, B. Effect of N-3 Polyunsaturated Fatty Acid Supplementation in Pregnancy: The Nuheal Trial. Pharm. Biotechnol. 2005, 569, 109–113. [Google Scholar] [CrossRef]
- Keats, E.C.; Haider, B.A.; Tam, E.; Bhutta, Z. A Multiple-micronutrient supplementation for women during pregnancy. Cochrane Database Syst. Rev. 2019, 3, CD004905. [Google Scholar] [CrossRef]
- Middleton, P.; Gomersall, J.S.; Gould, J.F.; Shepherd, E.; Olsen, S.F.; Makrides, M. Omega-3 fatty acid addition during pregnancy. Cochrane Database Syst. Rev. 2018, 11, CD003402. [Google Scholar] [CrossRef] [PubMed]
- FIGO Working Group on Good Clinical Practice in Maternal-Fetal Medicine Good clinical practice advice: Micronutrients in the periconceptional period and pregnancy. Int. J. Gynecol. Obstet. 2019, 144, 317–321. [CrossRef] [PubMed]
- World Health Organization. Nutrition and Pregnancy. Available online: https://www.who.int/nutrition/publications/pregnant/en/ (accessed on 30 April 2020).
- Food Nutrition Board of the Institute of Medicine. Nutrient Recommendations: Dietary Reference Intakes (DRI). National Institutes of Health, Office of Dietary Supplements. Available online: https://ods.od.nih.gov/Health_Information/Dietary_Reference_Intakes.aspx (accessed on 1 April 2020).
- European Food Safety Authority. Dietary Reference Values for the EU: DRV Finder. Available online: https://www.efsa.europa.eu/en/interactive-pages/drvs (accessed on 25 March 2020).
- Cazzola, R.; Cestaro, B. Red wine polyphenols protect n-3 more than n-6 polyunsaturated fatty acid from lipid peroxidation. Food Res. Int. 2011, 44, 3065–3071. [Google Scholar] [CrossRef]
- Cazzola, R.; Rondanelli, M.; Faliva, M.; Cestaro, B. Effects of DHA-phospholipids, melatonin and tryptophan supplementation on erythrocyte membrane physico-chemical properties in elderly patients suffering from mild cognitive impairment. Exp. Gerontol. 2012, 47, 974–978. [Google Scholar] [CrossRef]
- Cazzola, R.; Rondanelli, M.; Trotti, R.; Cestaro, B. Effects of weight loss on erythrocyte membrane composition and fluidity in overweight and moderately obese women. J. Nutr. Biochem. 2011, 22, 388–392. [Google Scholar] [CrossRef]
- Harris, W.S.; Von Schacky, C. The Omega-3 Index: A new risk factor for death from coronary heart disease? Prev. Med. 2004, 39, 212–220. [Google Scholar] [CrossRef]
- Wang, X.; Meng, L.; Su, C.; Shapses, S.A. Low free (but not total) 25-hydroxyvitamin d levels in subjects with normocalcemic hyperparathyroidism. Endocr. Pract. 2020, 26, 174–178. [Google Scholar] [CrossRef]
- Cighetti, G.M.; Bamonti, F.; Aman, C.S.; Gregori, D.; De Giuseppe, R.; Novembrino, C.; De Liso, F.; Maiavacca, R.; Paroni, R. Oxidative status in different settings and with different methodological approaches compared by Receiver Operating Characteristic curve analysis. Clin. Biochem. 2015, 48, 73–78. [Google Scholar] [CrossRef]
- Cazzola, R.; Rondanelli, M. N-Oleoyl-Phosphatidyl-Ethanolamine and Epigallo Catechin-3-Gallate Mitigate Oxidative Stress in Overweight and Class I Obese People on a Low-Calorie Diet. J. Med. Food 2020, 23, 319–325. [Google Scholar] [CrossRef]
- Hsieh, T.-T.; Chen, S.-F.; Lo, L.-M.; Li, M.-J.; Yeh, Y.-L.; Hung, T.-H. The Association Between Maternal Oxidative Stress at Mid-Gestation and Subsequent Pregnancy Complications. Reprod. Sci. 2012, 19, 505–512. [Google Scholar] [CrossRef]
- Vioque, J.; Navarrete-Muñoz, E.M.; Gimenez-Monzo, D.; García-de-la-Hera, M.; Granado-Lorencio, F.; Young, I.S.; Ramon, R.; Ballester, F.; Murcia, M.; Rebagliato, M.; et al. Reproducibility and validity of a food frequency questionnaire among pregnant women in a Mediterranean area. Nutr. J. 2013, 12, 26. [Google Scholar] [CrossRef] [PubMed]
- Bergmann, R.L.; Haschke-Becher, E.; Klassen-Wigger, P.; Bergmann, K.E.; Richter, R.; Dudenhausen, J.W.; Grathwohl, D.; Haschke, F. Supplementation with 200 mg/day docosahexaenoic acid from mid-pregnancy through lactation improves the docosahexaenoic acid status of mothers with a habitually low fish intake and of their infants. Ann. Nutr. Metab. 2008, 52, 157–166. [Google Scholar] [CrossRef] [PubMed]
- Jackson, K.H.; Harris, W.S. A Prenatal DHA Test to Help Identify Women at Increased Risk for Early Preterm Birth: A Proposal. Nutrients 2018, 10, 1933. [Google Scholar] [CrossRef] [PubMed]
- Carlson, S.E.; Gajewski, B.J.; Valentine, C.J.; Rogers, L.K.; Weiner, C.P.; DeFranco, E.; Buhimschi, C.S. Assessment of DHA on reducing early preterm birth: The ADORE randomized controlled trial protocol. BMC Pregnancy Childbirth 2017, 17, 62. [Google Scholar] [CrossRef] [PubMed]
- Von Schacky, C. Omega-3 Fatty Acids in Pregnancy—The Case for a Target Omega-3 Index. Nutrients 2020, 12, 898. [Google Scholar] [CrossRef]
- Hoge, A.; Bernardy, F.; Donneau, A.-F.; Dardenne, N.; Degée, S.; Timmermans, M.; Nisolle, M.; Guillaume, M.; Castronovo, V. Low omega-3 index values and monounsaturated fatty acid levels in early pregnancy: An analysis of maternal erythrocytes fatty acids. Lipids Health Dis. 2018, 17, 63. [Google Scholar] [CrossRef]
- Koletzko, B.; Cetin, I.; Brenna, J.T. Group Dietary fat intakes for pregnant and lactating women. Br. J. Nutr. 2007, 98, 873–877. [Google Scholar] [CrossRef]
- Zhang, Z.; Fulgoni, V.L.; Kris-Etherton, P.M.; Mitmesser, S.H. Dietary Intakes of EPA and DHA Omega-3 Fatty Acids among US Childbearing-Age and Pregnant Women: An Analysis of NHANES 2001–2014. Nutrients 2018, 10, 416. [Google Scholar] [CrossRef]
- Hubinont, C.; Savoye, T. Maternal and fetal benefits of DHA supplementation during pregnancy. J. Pregnancy Reprod. 2017, 1, 1. [Google Scholar] [CrossRef][Green Version]
- Cetin, I.; Alvino, G.; Cardellicchio, M. Long chain fatty acids and dietary fats in fetal nutrition. J. Physiol. 2009, 587, 3441–3451. [Google Scholar] [CrossRef]
- Ramiro-Cortijo, D.; Herrera, T.; Rodríguez-Rodríguez, P.; De Pablo, Á.L.L.; De La Calle, M.; López-Giménez, M.R.; Mora-Urda, A.I.; Gutiérrez-Arzapalo, P.Y.; Gómez-Rioja, R.; Aguilera, Y.; et al. Maternal plasma antioxidant status in the first trimester of pregnancy and development of obstetric complications. Placenta 2016, 47, 37–45. [Google Scholar] [CrossRef] [PubMed]
- Ramiro-Cortijo, D.; De La Calle, M.; Rodríguez-Rodríguez, P.; De Pablo, Á.L.L.; López-Giménez, M.R.; Aguilera, Y.; Martín-Cabrejas, M.A.; Gonzalez-Granado, J.M.; Arribas, S. Maternal Antioxidant Status in Early Pregnancy and Development of Fetal Complications in Twin Pregnancies: A Pilot Study. Antioxidants 2020, 9, 269. [Google Scholar] [CrossRef] [PubMed]
- Mousa, A.; Naqash, A.; Lim, S.S. Macronutrient and Micronutrient Intake during Pregnancy: An Overview of Recent Evidence. Nutrients 2019, 11, 443. [Google Scholar] [CrossRef] [PubMed]
- Pawley, N.; Bishop, N. Prenatal and infant predictors of bone health: The influence of vitamin D. Am. J. Clin. Nutr. 2004, 80, 1748S–1751S. [Google Scholar] [CrossRef]
- Dunstan, J.A.; Mori, T.A.; Barden, A.; Beilin, L.J.; Holt, P.G.; Calder, P.C.; Taylor, A.L.; Prescott, S.L. Effects of n-3 polyunsaturated fatty acid supplementation in pregnancy on maternal and fetal erythrocyte fatty acid composition. Eur. J. Clin. Nutr. 2004, 58, 429–437. [Google Scholar] [CrossRef]
- Krauss-Etschmann, S.; Shadid, R.; Campoy, C.; Hoster, E.; Demmelmair, H.; Jimenez, M.; Gil, A.; Rivero, M.; Veszprémi, B. Effects of fish-oil and folate supplementation of pregnant women on maternal and fetal plasma concentrations of docosahexaenoic acid and eicosapentaenoic acid: A European randomized multicenter trial. Am. J. Clin. Nutr. 2007, 85, 1392–1400. [Google Scholar] [CrossRef]
- Dean, S.V.; Lassi, Z.S.; Imam, A.M.; Bhutta, Z.A. Preconception care: Nutritional risks and interventions. Reprod. Heal. 2014, 11, S3. [Google Scholar] [CrossRef]
- Czeizel, A.E. The primary prevention of birth defects: Multivitamins or folic acid? Int. J. Med Sci. 2004, 1, 50–61. [Google Scholar] [CrossRef]
- Supplementation with Multiple Micronutrients Intervention Trial (SUMMIT) Study Group. Effect of maternal multiple micronutrient supplementation on fetal loss and infant death in Indonesia: A double-blind cluster-randomised trial. Lancet 2008, 371, 215–227. [Google Scholar] [CrossRef]
- Prado, E.L.; Sebayang, S.K.; Apriatni, M.; Adawiyah, S.R.; Hidayati, N.; Islamiyah, A.; Siddiq, S.; Harefa, B.; Lum, J.; Alcock, K.J.; et al. Maternal multiple micronutrient supplementation and other biomedical and socioenvironmental influences on children’s cognition at age 9-12 years in Indonesia: Follow-up of the SUMMIT randomised trial. Lancet Glob. Health 2017, 5, e217–e228. [Google Scholar] [CrossRef]
- Wolf, H.T.; Hegaard, H.; Huusom, L.D.; Pinborg, A. Multivitamin use and adverse birth outcomes in high-income countries: A systematic review and meta-analysis. Am. J. Obstet. Gynecol. 2017, 217, 404.e1–404.e30. [Google Scholar] [CrossRef] [PubMed]
- Staudacher, H.M.; Irving, P.M.; Lomer, M.C.; Whelan, K. The challenges of control groups, placebos and blinding in clinical trials of dietary interventions. Proc. Nutr. Soc. 2017, 76, 203–212. [Google Scholar] [CrossRef] [PubMed]


| Characteristics | No Supplementation (n = 76) | MMS (n = 65) |
|---|---|---|
| Age (years) | 76 | 65 |
| 32.3 ± 4.72 | 31.4 ± 4.52 | |
| 33.0 (18–41) | 32.0 (20–40) | |
| Weight (kg) | 76 | 65 |
| 61.5 ± 9.96 | 63.2 ± 9.48 | |
| 59.0 (45–87) | 47.0 (47–95) | |
| Height (cm) | 76 | 65 |
| 164.1 ± 7.08 | 165.9 ± 5.60 | |
| 165.0 (147–184) | 165.0 (150–178) | |
| Body mass index (kg/m2) | 76 | 65 |
| 22.8 ± 3.24 | 22.9 ± 3.10 | |
| 21.7 (18.0–29.7) | 22.0 (18.1–29.9) | |
| Previous pregnancy, n (%) | ||
| No | 30 (39.5) | 30 (46.2) |
| Yes | 46 (60.5) | 35 (53.9) |
| Smoking status, n (%) | ||
| Never | 49 (64.5) | 49 (75.4) |
| Former a | 27 (35.5) | 16 (24.6) |
| Delivery information | ||
| Subjects performing delivery visit | 69 | 62 |
| Type of delivery, n (%) | ||
| Vaginal | 55 (79.7) | 49 (79.0) |
| Caesarean | 14 (20.3) | 13 (21.0) |
| Delivery complications, n (%) | ||
| No | 53 (76.8) | 54 (87.1) |
| Yes | 16 (23.2) | 8 (12.9) |
| Induced labor, n (%) | ||
| No | 56 (81.2) | 53 (85.5) |
| Yes | 13 (18.8) | 9 (14.5) |
| Infant sex, n (%) | ||
| Male | 39 (56.5) | 36 (58.1) |
| Female | 30 (43.5) | 26 (41.9) |
| No Supplementation (n = 76) | MMS (n = 65) | |||||
|---|---|---|---|---|---|---|
| Visit 1 | Visit 3 | Visit 4 | Visit 1 | Visit 3 | Visit 4 | |
| RBC DHA (wt% TFA) | 6.1 ± 1.23 (3.8–9.3) | 6.6 ± 1.30 (4.0–10.4) | 6.7 ± 1.34 (4.3–9.6) | 6.1 ± 1.26 (3.4–10.2) | 7.0 ± 1.30 (4.5–10.5) | 7.5 ± 1.48 (5.0–13.0) |
| LSMEANS difference/p value | — | — | — | — | — | 0.96 (0.61, 1.31)/ < 0.0001 * |
| RBC DHA/TFA ratio | 0.06 ± 0.01 (0.04–0.09) | 0.07 ± 0.01 (0.04–0.10) | 0.07 ± 0.01 (0.04–0.10) | 0.06 ± 0.01 (0.03–0.10) | 0.07 ± 0.01 (0.04–0.11) | 0.08 ± 0.01 (0.05–0.13) |
| LSMEANS difference/p value | — | — | — | — | — | 0.010 (0.006, 0.013)/ <0.0001 * |
| Omega 3 index (%) | 6.7 ± 1.38 (4.2–10.1) | 7.0 ± 1.43 (4.2–10.7) | 7.1 ± 1.45 (4.5–10.0) | 6.5 ± 1.40 (3.7–10.9) | 7.5 ± 1.43 (4.7–11.1) | 8.0 ± 1.59 (5.3–13.6) |
| LSMEANS difference/p value | — | — | — | — | — | 1.00 (0.64, 1.37)/ <0.0001 * |
| Calcidiol (ug/L) | 21.6 ± 8.94 (5.5–48.8) | 19.9 ± 9.87 (4.6–64.1) | 17.8 ± 9.72 (4.0–45.0) | 20.5 ± 7.54 (4.4–36.5) | 22.8 ± 8.94 (4.0–48.6) | 21.4 ± 9.07 (5.5–42.7) |
| LSMEANS difference/p value | — | — | — | — | — | 3.96 (0.88, 7.04)/ 0.0122 * |
| Parameters | No Supplementation (n = 89) | MMS (n = 87) | Total (n = 176) |
|---|---|---|---|
| Number of TEAEs pertinent to the mother | 114 | 118 | 232 |
| Any TEAEs pertinent to the mother | 64 (71.9) | 61 (70.1) | 125 (71.0) |
| At least one suspected related a | NA | 3 (3.5) | 3 (1.7) |
| At least one serious TEAE | 11 (12.4) | 12 (13.8) | 23 (13.1) |
| At least one leading to temporary treatment interruption b | NA | 1 (1.2) | 1 (0.6) |
| At least one leading to permanent treatment discontinuation c | NA | 19 (21.8) | 19 (10.8) |
| Fatal outcome | 0 | 0 | 0 |
| Number of TEAEs pertinent to fetus/child | 4 | 9 | 13 |
| Any TEAEs pertinent to fetus/child | 3 (3.4) | 7 (8.1) | 10 (5.7) |
| At least one suspected related a | NA | 0 | 0 |
| At least one serious TEAE b | 2 (2.3) | 3 (3.5) | 5 (2.8) |
| At least one leading to temporary treatment interruption c | NA | 1 (1.2) | 1 (0.6) |
| At least one leading to permanent treatment discontinuation d | NA | 1 (1.2) | 1 (0.6) |
| Fatal outcome | 0 | 1 (1.2) | 1 (0.6) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Massari, M.; Novielli, C.; Mandò, C.; Di Francesco, S.; Della Porta, M.; Cazzola, R.; Panteghini, M.; Savasi, V.; Maggini, S.; Schaefer, E.; et al. Multiple Micronutrients and Docosahexaenoic Acid Supplementation during Pregnancy: A Randomized Controlled Study. Nutrients 2020, 12, 2432. https://doi.org/10.3390/nu12082432
Massari M, Novielli C, Mandò C, Di Francesco S, Della Porta M, Cazzola R, Panteghini M, Savasi V, Maggini S, Schaefer E, et al. Multiple Micronutrients and Docosahexaenoic Acid Supplementation during Pregnancy: A Randomized Controlled Study. Nutrients. 2020; 12(8):2432. https://doi.org/10.3390/nu12082432
Chicago/Turabian StyleMassari, Maddalena, Chiara Novielli, Chiara Mandò, Stefania Di Francesco, Matteo Della Porta, Roberta Cazzola, Mauro Panteghini, Valeria Savasi, Silvia Maggini, Ella Schaefer, and et al. 2020. "Multiple Micronutrients and Docosahexaenoic Acid Supplementation during Pregnancy: A Randomized Controlled Study" Nutrients 12, no. 8: 2432. https://doi.org/10.3390/nu12082432
APA StyleMassari, M., Novielli, C., Mandò, C., Di Francesco, S., Della Porta, M., Cazzola, R., Panteghini, M., Savasi, V., Maggini, S., Schaefer, E., & Cetin, I. (2020). Multiple Micronutrients and Docosahexaenoic Acid Supplementation during Pregnancy: A Randomized Controlled Study. Nutrients, 12(8), 2432. https://doi.org/10.3390/nu12082432







