The Effect of Supportive Implementation of Healthier Canteen Guidelines on Changes in Dutch School Canteens and Student Purchase Behaviour
Abstract
1. Introduction
2. Materials and Methods
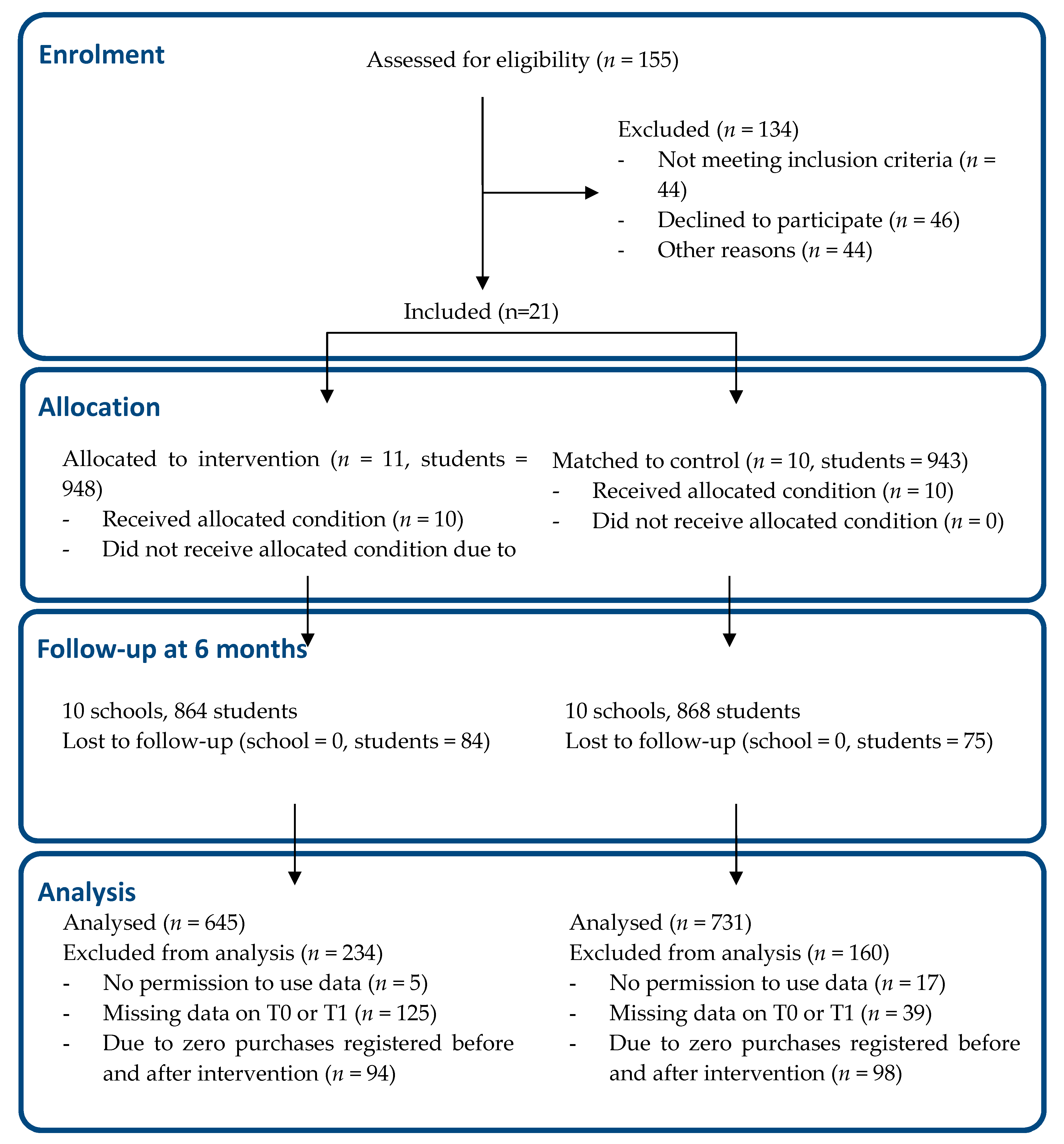
2.1. Study Design
2.2. Study Population
2.3. Intervention
2.4. Measurements
2.4.1. Health Level of the School Canteen
2.4.2. Self-Reported Purchase Behaviour of Students
2.4.3. Other Student Variables
2.5. Sample Size
2.6. Statistical Analyses
3. Results
3.1. Baseline Characteristics
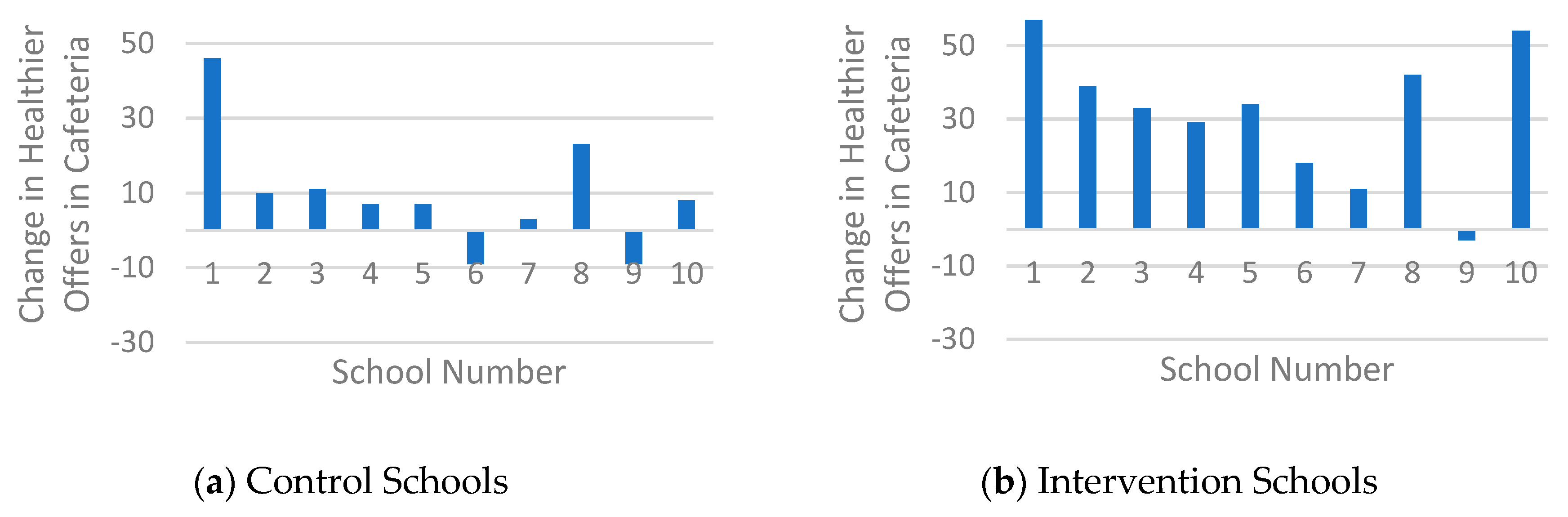
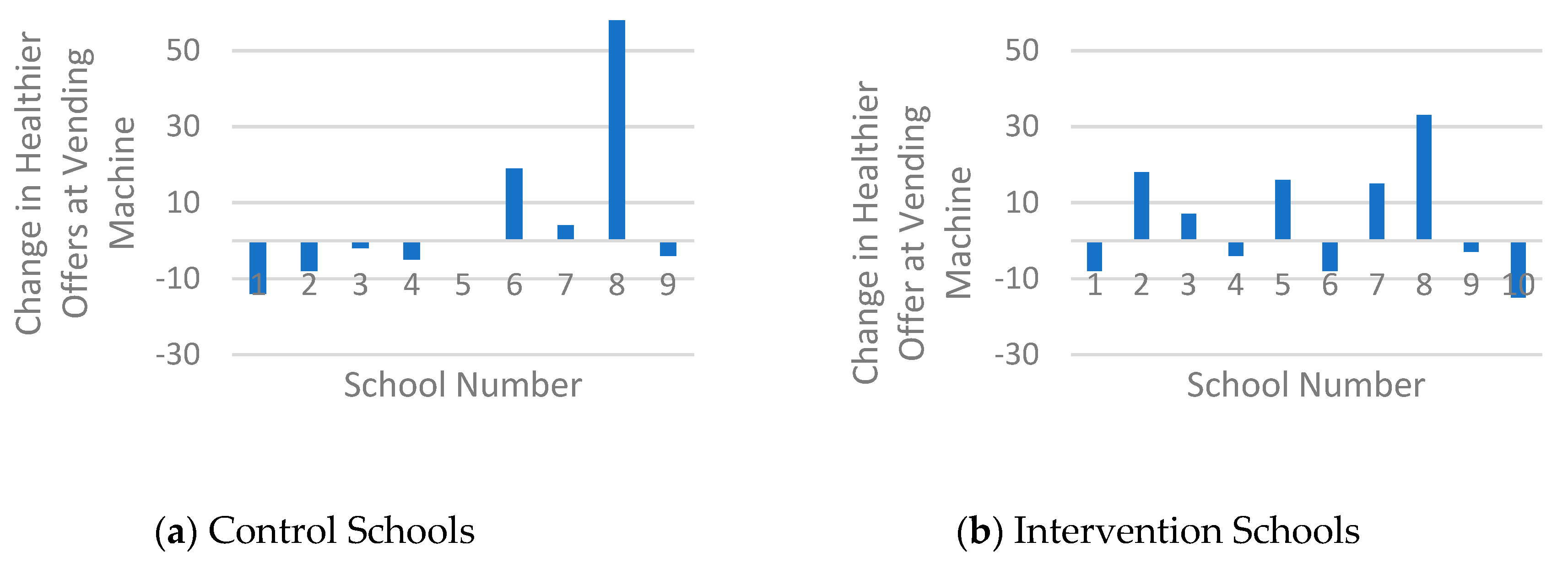
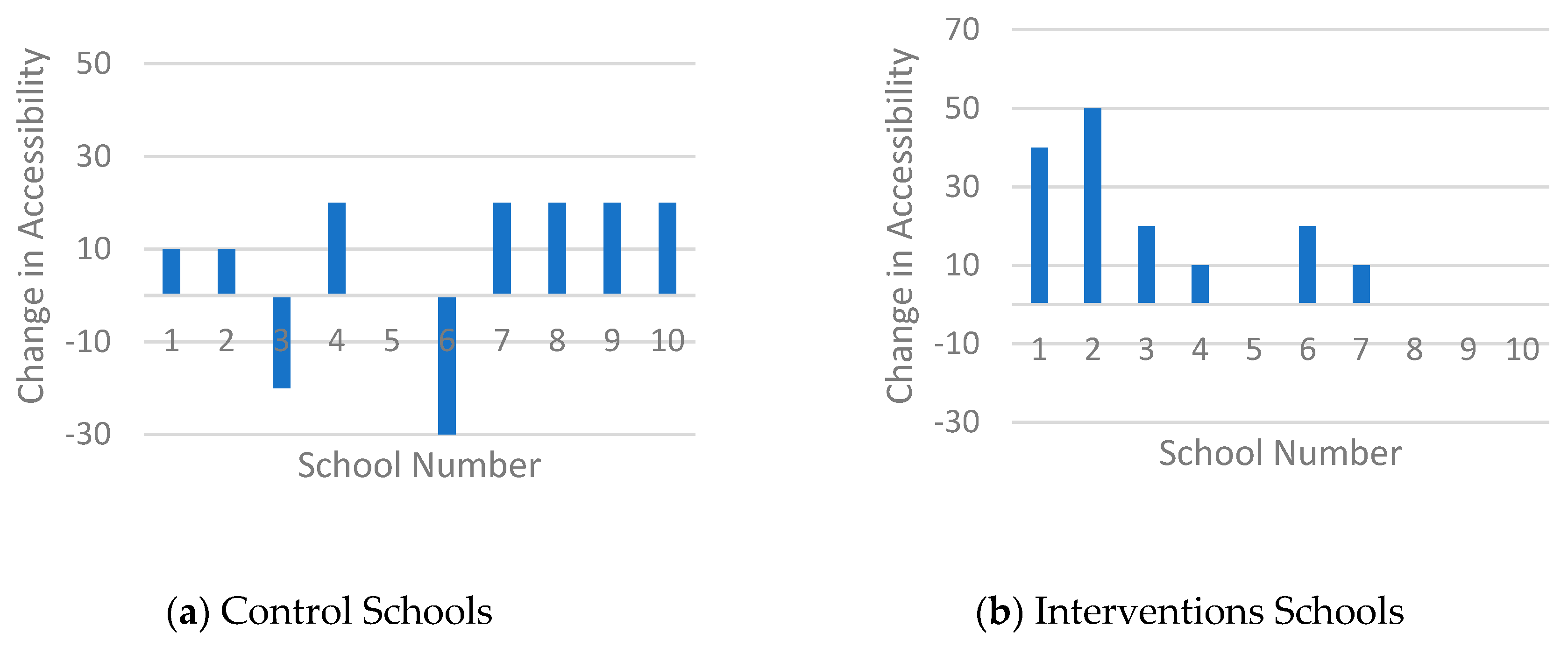
3.2. Intervention Effect on Health Level of the Canteen
3.3. Purchases in the Cafeteria
3.4. Purchases at the Vending Machines
3.5. Purchase Behaviour Analysed by Mixed Logistic Regression Analyses
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Storcksdieck, S.; Kardakis, T.; Wollgast, J.; Nelson, M.; Caldeira, S. Mapping of National School Food Policies across the EU28 Plus Norway and Switzerland; European Commission, EUR 26621 EN, Joint Research Centre, Institute for Health and Consumer Protection: Luxembourg, 2014; ISSN 18319–42. [Google Scholar]
- Thaler, R.H.; Sunstein, C.R. Nudge: Improving Decisions about Health, Wealth, and Happiness; Yale University Press: Connecticut, CT, USA, 2008. [Google Scholar]
- Powell, L.M.; Chriqui, J.F.; Khan, T.; Wada, R.; Chaloupka, F.J. Assessing the potential effectiveness of food and beverage taxes and subsidies for improving public health: A systematic review of prices, demand and body weight outcomes. Obes. Rev. 2013, 14, 110–128. [Google Scholar] [CrossRef] [PubMed]
- Grech, A.; Allman-Farinelli, M.A. Systematic literature review of nutrition interventions in vending machines that encourage consumers to make healthier choices. Obes. Rev. 2015, 16, 1030–1041. [Google Scholar] [CrossRef] [PubMed]
- Driessen, C.E.; Cameron, A.J.; Thornton, L.E.; Lai, S.K.; Barnett, L.M. Effect of changes to the school food environment on eating behaviours and/or body weight in children: A systematic review. Obes. Rev. 2014, 15, 968–982. [Google Scholar] [CrossRef] [PubMed]
- Kessler, H.S. Simple interventions to improve healthy eating behaviors in the school cafeteria. Nutr. Rev. 2016, 74, 198–209. [Google Scholar] [CrossRef]
- Micha, R.; Karageorgou, D.; Bakogianni, I.; Trichia, E.; Whitsel, L.P.; Story, M.; Penalvo, J.L.; Mozaffarian, D. Effectiveness of school food environment policies on children’s dietary behaviors: A systematic review and meta-analysis. PLoS ONE 2018, 13, e0194555. [Google Scholar] [CrossRef]
- Masse, L.C.; Naiman, D.; Naylor, P.J. From policy to practice: Implementation of physical activity and food policies in schools. Int. J. Behav. Nutr. Phys. Act. 2013, 10, 71. [Google Scholar] [CrossRef]
- de Silva-Sanigorski, A.; Breheny, T.; Jones, L.; Lacy, K.; Kremer, P.; Carpenter, L.; Bolton, K.; Prosser, L.; Gibbs, L.; Waters, E.; et al. Government food service policies and guidelines do not create healthy school canteens. Aust. N. Z. J. Public Health 2011, 35, 117–121. [Google Scholar] [CrossRef]
- Leeman, J.; Wiecha, J.L.; Vu, M.; Blitstein, J.L.; Allgood, S.; Lee, S.; Merlo, C. School health implementation tools: A mixed methods evaluation of factors influencing their use. Implement. Sci. 2018, 13, 48. [Google Scholar] [CrossRef]
- Wolfenden, L.; Nathan, N.K.; Sutherland, R.; Yoong, S.L.; Hodder, R.K.; Wyse, R.J.; Delaney, T.; Grady, A.; Fielding, A.; Tzelepis, F.; et al. Strategies for enhancing the implementation of school-based policies or practices targeting risk factors for chronic disease. Cochrane Database Syst. Rev. 2017, 11, Cd011677. [Google Scholar] [CrossRef]
- McIsaac, J.-L.D.; Hernandez, K.J.; Kirk, S.F.L.; Curran, J.A. Interventions to Support System-level Implementation of Health Promoting Schools: A Scoping Review. Int. J. Environ. Res. Public Health 2016, 13, 200. [Google Scholar] [CrossRef]
- Hermans, R.C.J.; Smit, K.; van den Broek, N.; Evenhuis, I.J.; Veldhuis, L. Adolescents’ Food Purchasing Patterns in The School Food Environment: Examining the Role of Perceived Relationship Support and Maternal Monitoring. Nutrients 2020, 12, 733. [Google Scholar] [CrossRef]
- Mensink, F.; Schwinghammer, S.A.; Smeets, A. The Healthy School Canteen programme: A promising intervention to make the school food environment healthier. J. Environ. Public Health 2012, 2012, 415746. [Google Scholar] [CrossRef] [PubMed]
- Milder, I.E.; Mikolajczak, J.; van den Berg, S.W.; van de Veen-van Hofwegen, M.; Bemelmans, W.J. Food supply and actions to improve dietary behaviour of students—A comparison between secondary schools participating or not participating in the ‘Healthy School Canteen Program’. Public Health Nutr. 2014, 18, 198–207. [Google Scholar] [CrossRef][Green Version]
- Van Rijn, M.J. Kamerbrief Over De Gezondheidseisen Van Schoolkantine [Letter to the Parlement about Health Regulations in School Canteens]. Available online: https://www.rijksoverheid.nl/documenten (accessed on 3 February 2017).
- Geurts, M.; Brants, H.; Milder, I. De Voedingsomgeving op Scholen: De Stand Van Zaken in Het Voortgezet Onderwijs En Middelbaar Beroepsonderwijs Anno 2015. [the Food Environment at Schools: The State of Art in Secondary (Vocational) Education Anno 2015]. Available online: http://www.rivm.nl/Documenten_en_publicaties/Wetenschappelijk/Rapporten/2016/mei/De_voedingsomgeving_op_scholen_De_stand_van_zaken_in_het_voortgezet_onderwijs_en_middelbaar_beroepsonderwijs_anno_2015 (accessed on 7 December 2018).
- iResearch, Inventarisatie Van Veranderingen in Schoolkantines Na Bezoek En Advies Van De Schoolkantine Brigade [Inventarisation of Changes in School Canteens after a Visit and Advise of the School Canteen Brigade, 2014]. Available online: https://static1.squarespace.com/static/5883d149e3df28fd7860bf14/t/590c4a96f7e0ab1d6d76a068/1493977754205/Inventarisatie+van+veranderingen+in+schoolkantine+%282014%29.pdf (accessed on 10 August 2020).
- Veldhuis, L.; Mensink, F.; Wolvers, D. Guidelines for Healthier Canteens, Fact Sheet; Netherlands Nutrition Centre: The Hague, The Netherlands, 2017; Available online: https://www.voedingscentrum.nl/Assets/Uploads/voedingscentrum/Documents/Professionals/Pers/Factsheets/English/Fact%20sheet%20Guidelines%20for%20Healthier%20Canteens.pdf (accessed on 10 June 2020).
- Brink, E.; van Rossum, C.; Postma-Smeets, A.; Stafleu, A.; Wolvers, D.; van Dooren, C.; Toxopeus, I.; Buurma-Rethans, E.; Geurts, M.; Ocké, M. Development of healthy and sustainable food-based dietary guidelines for the Netherlands. Public Health Nutr. 2019, 22, 2419–2435. [Google Scholar] [CrossRef] [PubMed]
- Evenhuis, I.J.; Vyth, E.L.; van Nassau, F.; Veldhuis, L.; Westerman, M.J.; Seidell, J.C.; Renders, C.M. What do secondary schools need to create healthier canteens? The development of an implementation plan. Under review. 2020. [Google Scholar]
- Evenhuis, I.J.; Veldhuis, L.; Jacobs, S.M.; Renders, C.M.; Seidell, J.C.; Schuit-Van Raamsdonk, H. Brengt de Kantinescan Aanbod En Uitstraling Goed in Kaart? [Is the Canteen Scan Able to Map the Availability and Accessibility Properly?]. Available online: https://gezondeschoolkantine.voedingscentrum.nl/Assets/Uploads/de-gezonde-kantine/Documents/Factsheet%20kantinescan.pdf (accessed on 23 November 2019).
- Schulz, K.F.; Altman, D.G.; Moher, D. CONSORT 2010 Statement: Updated guidelines for reporting parallel group randomised trials. BMC Med. 2010, 8, 18. [Google Scholar] [CrossRef] [PubMed]
- Grol, R.; Wensing, M.; Eccles, M.; Davis, D. Improving Patient Care: The Implementation of Change in Health Care; Wiley: Hoboken, NJ, USA, 2013. [Google Scholar]
- Evenhuis, I.J.; Wezenbeek, N.L.W.J.; Vyth, E.L.; Veldhuis, L.; Poelman, M.P.; Wolvers, D.; Seidell, J.C.; Renders, C.M. Development of the ‘Canteen Scan’: An online tool to monitor implementation of healthy canteen guidelines. BMC Public Health 2018, 18, 1109. [Google Scholar] [CrossRef]
- Kremers, S.P.; de Bruijn, G.J.; Visscher, T.L.; van Mechelen, W.; de Vries, N.K.; Brug, J. Environmental influences on energy balance-related behaviors: A dual-process view. Int. J. Behav. Nutr. Phys. Act. 2006, 3, 9. [Google Scholar] [CrossRef]
- Janssen, E.H.; Singh, A.S.; van Nassau, F.; Brug, J.; van Mechelen, W.; Chinapaw, M.J. Test-retest reliability and construct validity of the DOiT (Dutch Obesity Intervention in Teenagers) questionnaire: Measuring energy balance-related behaviours in Dutch adolescents. Public Health Nutr. 2014, 17, 277–286. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.S.; Vik, F.N.; Chinapaw, M.J.; Uijtdewilligen, L.; Verloigne, M.; Fernandez-Alvira, J.M.; Stomfai, S.; Manios, Y.; Martens, M.; Brug, J. Test-retest reliability and construct validity of the ENERGY-child questionnaire on energy balance-related behaviours and their potential determinants: The ENERGY-project. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 136. [Google Scholar] [CrossRef] [PubMed]
- Van Assema, P.; Brug, J.; Ronda, G.; Steenhuis, I. The relative validity of a short Dutch questionnaire as a means to categorize adults and adolescents to total and saturated fat intake. J. Hum. Nutr. Diet 2001, 14, 377–390. [Google Scholar] [CrossRef] [PubMed]
- Bogers, R.P.; Van Assema, P.; Kester, A.D.; Westerterp, K.R.; Dagnelie, P.C. Reproducibility, validity, and responsiveness to change of a short questionnaire for measuring fruit and vegetable intake. Am. J. Epidemiol. 2004, 159, 900–909. [Google Scholar] [CrossRef] [PubMed]
- Martens, M.K.; van Assema, P.; Brug, J. Why do adolescents eat what they eat? Personal and social environmental predictors of fruit, snack and breakfast consumption among 121-4-year-old Dutch students. Public Health Nutr. 2005, 8, 1258–1265. [Google Scholar] [CrossRef]
- Drennan, J. Cognitive interviewing: Verbal data in the design and pretesting of questionnaires. J. Adv. Nurs. 2003, 42, 57–63. [Google Scholar] [CrossRef]
- Tavakol, M.; Dennick, R. Making sense of Cronbach’s alpha. Int. J. Med. Educ. 2011, 2, 53–55. [Google Scholar] [CrossRef] [PubMed]
- Evenhuis, I.J.; Vyth, E.L.; Veldhuis, L.; Seidell, J.C.; Renders, C.M. Development and evaluation of the implementation of guidelines for healthier canteens in Dutch Secondary Schools: Study protocol of a Quasi-experimental trial. Front. Public Health 2019, 7, 254. [Google Scholar] [CrossRef] [PubMed]
- Twisk, J.W.R. Applied Multilevel Analysis: A Practical Guide for Medical Researchers; Cambridge University Press: Cambridge, UK, 2006. [Google Scholar]
- Khambalia, A.Z.; Dickinson, S.; Hardy, L.L.; Gill, T.; Baur, L.A. A synthesis of existing systematic reviews and meta-analyses of school-based behavioural interventions for controlling and preventing obesity. Obes. Rev. 2012, 13, 214–233. [Google Scholar] [CrossRef]
- Powell, B.J.; Beidas, R.S.; Lewis, C.C.; Aarons, G.A.; McMillen, J.C.; Proctor, E.K.; Mandell, D.S. Methods to improve the selection and tailoring of implementation strategies. J. Behav. Health Serv. Res. 2015, 44, 117–194. [Google Scholar] [CrossRef]
- Evenhuis, I.J.; Vyth, E.L.; Veldhuis, L.; Jacobs, S.M.; Seidell, J.C.; Renders, C.M. Implementation of guidelines for healthier canteens in Dutch Secondary Schools: A process evaluation. Int. J. Environ. Res. Public Health 2019, 16, 4509. [Google Scholar] [CrossRef]
- Lane, C.; Naylor, P.-J.; Tomlin, D.; Kirk, S.; Hanning, R.; Masse, L.; Olstad, D.L.; Prowse, R.; Caswell, S.; Jarvis, S.; et al. Healthy vending contracts: Do localized policy approaches improve the nutrition environment in publicly funded recreation and sport facilities? Prev. Med. Rep. 2019, 16, 100967. [Google Scholar] [CrossRef]
- Bucher, T.; Collins, C.; Rollo, M.E.; McCaffrey, T.A.; De Vlieger, N.; Van der Bend, D.; Truby, H.; Perez-Cueto, F.J. Nudging consumers towards healthier choices: A systematic review of positional influences on food choice. Br. J. Nutr. 2016, 115, 2252–2263. [Google Scholar] [CrossRef] [PubMed]
- Arno, A.; Thomas, S. The efficacy of nudge theory strategies in influencing adult dietary behaviour: A systematic review and meta-analysis. BMC Public Health 2016, 16, 676. [Google Scholar] [CrossRef] [PubMed]
- Grivois-Shah, R.; Gonzalez, J.R.; Khandekar, S.P.; Howerter, A.L.; O’Connor, P.A.; Edwards, B.A. Impact of healthy vending machine options in a large community health organization. Am. J. Health Promot. 2018, 32, 1425–1430. [Google Scholar] [CrossRef] [PubMed]
- Hollands, G.J.; Carter, P.; Anwer, S.; King, S.E.; Jebb, S.A.; Ogilvie, D.; Shemilt, I.; Higgins, J.P.T.; Marteau, T.M. Altering the availability or proximity of food, alcohol, and tobacco products to change their selection and consumption. Cochrane Database Syst. Rev. 2019, 9, Cd012573. [Google Scholar]
- von Philipsborn, P.; Stratil, J.M.; Burns, J.; Busert, L.K.; Pfadenhauer, L.M.; Polus, S.; Holzapfel, C.; Hauner, H.; Rehfuess, E. Environmental interventions to reduce the consumption of sugar-sweetened beverages and their effects on health. Cochrane Database Syst. Rev. 2019, 6, Cd012292. [Google Scholar] [CrossRef]
- Story, M.; Kaphingst, K.M.; Robinson-O’Brien, R.; Glanz, K. Creating healthy food and eating environments: Policy and environmental approaches. Annu. Rev. Public Health 2008, 29, 253–272. [Google Scholar] [CrossRef]
- Townsend, N.; Foster, C. Developing and applying a socio-ecological model to the promotion of healthy eating in the school. Public Health Nutr. 2013, 16, 1101–1108. [Google Scholar] [CrossRef]
- Larson, N.; Story, M. A review of environmental influences on food choices. Ann. Behav. Med. 2009, 38 (Suppl. S1), S56–S73. [Google Scholar] [CrossRef]
- Hermans, R.C.J.; de Bruin, H.; Larsen, J.K.; Mensink, F.; Hoek, A.C. Adolescents’ Responses to a school-based prevention program promoting healthy eating at school. Front. Public Health 2017, 5, 309. [Google Scholar] [CrossRef]
- Draper, C.E.; Grobler, L.; Micklesfield, L.K.; Norris, S.A. Impact of social norms and social support on diet, physical activity and sedentary behaviour of adolescents: A scoping review. Child Care Health Dev. 2015, 41, 654–667. [Google Scholar] [CrossRef]
- Meiklejohn, S.; Ryan, L.; Palermo, C. A systematic review of the impact of multi-strategy nutrition education programs on health and nutrition of adolescents. J. Nutr. Educ. Behav. 2016, 48, 631–646.e1. [Google Scholar] [CrossRef]
- Craigie, A.M.; Lake, A.A.; Kelly, S.A.; Adamson, A.J.; Mathers, J.C. Tracking of obesity-related behaviours from childhood to adulthood: A systematic review. Maturitas 2011, 70, 266–284. [Google Scholar] [CrossRef] [PubMed]
- Higgs, S. Social norms and their influence on eating behaviours. Appetite 2015, 86, 38–44. [Google Scholar] [CrossRef] [PubMed]
- Yoong, S.L.; Nathan, N.; Wolfenden, L.; Wiggers, J.; Reilly, K.; Oldmeadow, C.; Wyse, R.; Sutherland, R.; Delaney, T.; Butler, P.; et al. CAFÉ: A multicomponent audit and feedback intervention to improve implementation of healthy food policy in primary school canteens: A randomised controlled trial. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 126. [Google Scholar] [CrossRef] [PubMed]
- Tugault-Lafleur, C.N.; Black, J.L.; Barr, S.I. A systematic review of methods to assess children’s diets in the school context. Adv. Nutr. 2017, 8, 63–79. [Google Scholar] [CrossRef]
- Mason, T.B.; Do, B.; Wang, S.; Dunton, G.F. Ecological momentary assessment of eating and dietary intake behaviors in children and adolescents: A systematic review of the literature. Appetite 2020, 144, 104465. [Google Scholar] [CrossRef]
- van Nassau, F.; Singh, A.S.; van Mechelen, W.; Brug, J.; Chinapaw, M.J. Implementation evaluation of school-based obesity prevention programmes in youth; how, what and why? Public Health Nutr. 2015, 18, 1531–1534. [Google Scholar] [CrossRef]
- Saunders, R.P.; Evans, M.H.; Joshi, P. Developing a process-evaluation plan for assessing health promotion program implementation: A how-to guide. Health Promot. Pract. 2005, 6, 134–147. [Google Scholar] [CrossRef]
- Alaimo, K.; Oleksyk, S.C.; Drzal, N.B.; Golzynski, D.L.; Lucarelli, J.F.; Wen, Y.; Velie, E.M. Effects of changes in lunch-time competitive foods, nutrition practices, and nutrition policies on low-income middle-school children’s diets. Child. Obes. 2013, 9, 509–523. [Google Scholar] [CrossRef]
| Intervention Schools (N = 10) | Control Schools (N = 10) | |||||
|---|---|---|---|---|---|---|
| Total | Boys | Girls | Total | Boys | Girls | |
| Number of students—n (%) | 645 (46.9) | 302 (46.8) | 343 (53.2) | 731 (53.1) | 318 (43.5) | 413 (56.5) |
| Age (years)—mean (SD) | 13.39 (0.62) | 13.35 (0.55) | 13.42 (0.68) | 13.35 (0.62) | 13.38 (0.66) | 13.33 (0.59) |
| School level n (%) | ||||||
| Vocational education | 284 (44.0) | 125 (41.4) | 159 (46.4) | 310 (42.4) | 147 (46.2) | 163 (39.5) |
| Senior general education | 148 (22.9) | 86 (28.5) | 62 (18.1) | 190 (26.0) | 78 (24.5) | 112 (27.1) |
| Pre-university education | 213 (33.0) | 91 (30.1) | 122 (35.6) | 231 (31.6) | 93 (29.2) | 138 (33.4) |
| Behavioural determinants—Mean (SD) a | ||||||
| Attitude | 2.81 (0.84) | 2.73 (0.84) | 2.88 (0.84) | 2.91 (0.86) | 2.67 (0.88) | 3.09 (0.80) |
| Subjective norm | 2.39 (0.64) | 2.32 (0.64) | 2.44 (0.63) | 2.39 (0.68) | 2.31 (0.71) | 2.46 (0.66) |
| Perceived behavioural control | 3.18 (0.92) | 3.18 (0.95) | 3.18 (0.89) | 3.36 (0.89) | 3.24 (0.93) | 3.46 (0.84) |
| Intention | 2.46 (0.94) | 2.27 (0.97) | 2.64 (0.88) | 2.50 (0.89) | 2.26 (0.87) | 2.68 (0.87) |
| Environmental determinants—n (%) | ||||||
| Breakfast behaviour | ||||||
| Yes, sometimes or always | 610 (94.6) | 294 (97.4) | 316 (92.1) | 705 (96.4) | 311 (97.8) | 394 (95.4) |
| No, never | 35 (5.4) | 8 (2.6) | 27 (7.9) | 26 (3.6) | 7 (2.2) | 19 (4.6) |
| Foods brought from home | ||||||
| Less than four times per week | 53 (8.2) | 23 (7.6) | 30 (8.7) | 79 (10.8) | 39 (12.3) | 40 (9.7) |
| 4 or more times per week | 592 (91.8) | 279 (92.4) | 313 (91.3) | 652 (89.2) | 279 (87.7) | 373 (90.3) |
| Drinks brought from home | ||||||
| Less than four per week | 62 (9.6) | 30 (9.9) | 32 (9.3) | 84 (11.5) | 45 (14.2) | 39 (9.4) |
| 4 or more times per week | 583 (90.4) | 272 (90.1) | 311 (90.7) | 647 (88.5) | 273 (85.8) | 374 (90.6) |
| Amount of money spent on food/drink purchases in school per week | ||||||
| <€1 | 91 (14.1) | 45 (14.9) | 46 (13.4) | 131 (17.9) | 56 (17.6) | 75 (18.2) |
| €1–2 | 354 (54.9) | 154 (51.0) | 200 (58.3) | 442 (60.5) | 180 (56.6) | 262 (63.4) |
| ≥€2 | 200 (31.0) | 103 (34.1) | 97 (28.3) | 158 (21.6) | 82 (25.8) | 76 (18.4) |
| Food or drink purchases in school cafeteria | ||||||
| Less than once per week | 358 (55.5) | 167 (55.3) | 191 (55.7) | 471 (64.4) | 183 (57.5) | 288 (69.7) |
| 1 time per week | 151 (23.4) | 76 (25.2) | 75 (21.9) | 137 (18.7) | 66 (20.8) | 71 (17.2) |
| 2 or more times per week | 136 (21.1) | 59 (19.5) | 77 (22.4) | 123 (16.8) | 69 (21.7) | 54 (13.1) |
| Food or drink purchases in school at vending machine b,c | ||||||
| Less than once per week | 410 (63.6) | 196 (64.9) | 214 (62.4) | 447 (61.1) | 183 (61.2) | 264 (63.9) |
| 1 time per week | 123 (19.1) | 48 (15.9) | 75 (21.9) | 147 (20.1) | 62 (20.7) | 85 (20.6) |
| 2 or more times per week | 112 (17.4) | 58 (19.2) | 54 (15.7) | 101 (13.8) | 54 (18.1) | 47 (11.4) |
| Food purchases outside school | ||||||
| Less than once per week | 401 (62.2) | 175 (57.9) | 226 (65.9) | 480 (65.6) | 170 (53.5) | 310 (75.1) |
| 1 to 3 times per week | 167 (25.9) | 91 (30.1) | 76 (22.2) | 170 (23.3) | 104 (32.7) | 66 (16.0) |
| 4 or more times per week | 77 (11.9) | 36 (11.9) | 41 (12.0) | 81 (11.1) | 44 (13.8) | 37 (9.0) |
| Drink purchases outside school | ||||||
| Less than once per week | 436 (67.6) | 192 (63.6) | 244 (71.1) | 538 (73.6) | 201 (63.2) | 337 (81.6) |
| 1 to 3 times per week | 151 (23.4) | 82 (27.2) | 69 (20.1) | 126 (17.2) | 80 (25.2) | 46 (11.1) |
| 4 or more times per week | 58 (9.0) | 28 (9.3) | 30 (8.7) | 67 (9.2) | 37 (11.6) | 30 (7.3) |
| Intervention Schools (N = 10) | Control Schools (N = 10) | |||||
|---|---|---|---|---|---|---|
| T0 | T1 | Mean Change | T0 | T1 | Mean Change | |
| Healthier products available in the cafeteria ab | 45.80 (27.12) | 77.20 (13.41) | 31.4 | 50.40 (23.00) | 60.10 (15.67) | 9.7 |
| Healthier products available at vending machine abc | 44.70 (19.40) | 49.80 (20.33) | 5.1 | 38.89 (24.30) | 44.22 (22.99) | 5.3 |
| Fulfilled accessibility criteria ad | 44.00 (20.66) | 59.00 (19.69) | 15.0 | 43.00 (20.58) | 50.00 (14.91) | 20.0 |
| Intervention Schools | Control Schools | |||||||
|---|---|---|---|---|---|---|---|---|
| Boys (n = 276) | Girls (n = 308) | Boys (n = 272) | Girls (n = 357) | |||||
| T0 | T1 | T0 | T1 | T0 | T1 | T0 | T1 | |
| Purchase of less healthy products, mean (SD) | 1.50 (3.84) | 0.92 (1.39) | 1.41 (2.11) | 1.39 (4.20) | 1.43 (2.63) | 1.72 (4.97) | 0.91 (1.34) | 1.04 (3.71) |
| Purchase of healthier products, mean (SD) | 0.85 (2.98) | 0.51 (2.23) | 0.80 (1.82) | 1.17 (3.75) | 0.82 (2.83) | 1.17 (4.38) | 0.46 (1.10) | 0.59 (3.78) |
| Bought healthier products of total bought purchases, % | 36.2% | 35.7% | 36.2% | 45.7% | 36.4% | 40.5% | 33.6% | 36.2% |
| Changes in purchases per week over time a | ||||||||
| Healthy score a, % | 50.0% | 53.6% | 51.5% | 46.5% | ||||
| Intervention Schools | Control Schools | |||||||
|---|---|---|---|---|---|---|---|---|
| Boys (n = 270) | Girls (n = 311) | Boys (n = 272) | Girls (n = 364) | |||||
| T0 | T1 | T0 | T1 | T0 | T1 | T0 | T1 | |
| Weekly purchases of less healthy products, mean (SD) | 1.41 (3.03) | 0.88 (2.34) | 1.60 (2.84) | 1.40 (3.31) | 1.51 (2.44) | 1.40 (4.21) | 0.94 (1.78) | 0.83 (1.37) |
| Weekly purchases of healthier products, mean (SD) | 1.11 (3.13) | 0.79 (2.36) | 1.43 (2.40) | 1.48 (3.59) | 1.26 (2.59) | 1.13 (2.85) | 0.97 (1.49) | 0.87 (1.45) |
| Bought healthier products of total bought products, % | 44.1% | 47.3% | 47.2% | 51.4% | 45.5% | 44.7% | 50.8% | 51.2% |
| Changes in purchases per week over time a | ||||||||
| Healthy score a, % | 49.3% | 47.3% | 49.3% | 51.6% | ||||
| Model 1 b | Model 2 c | Model 3 d | Model 4 e | ||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | ||
| Purchases cafeteria a | Boys (n = 548) | 0.92 | 0.62; 1.36 | 0.94 | 0.67; 1.32 | 0.96 | 0.68; 1.35 | 0.92 | 0.63; 1.34 |
| Girls (n = 665) | 1.29 | 0.85; 1.96 | 1.29 | 0.83; 1.96 | 1.31 | 0.85; 2.02 | 1.30 | 0.85; 2.00 | |
| Purchases vending machine a | Boys (n = 542) | 1.02 | 0.62; 1.67 | 1.00 | 0.60; 1.67 | 1.03 | 0.62; 1.69 | 1.03 | 0.62; 1.71 |
| Girls (n = 675) | 0.84 | 0.62; 1.14 | 0.81 | 0.59; 1.11 | 0.85 | 0.61; 1.19 | 0.85 | 0.58; 1.23 | |
| Model 1 e | Model 2 f | Model 3 g | Model 4 h | ||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | ||
| Purchases cafeteria ab | Boys (n = 548) | 0.93 | 0.60; 1.44 | 1.02 | 0.69; 1.52 | 1.03 | 0.69; 1.53 | 1.01 | 0.66; 1.55 |
| Girls (n = 665) | 1.13 | 0.70; 1.83 | 1.14 | 0.70; 1.86 | 1.14 | 0.70; 1.88 | 1.13 | 0.69; 1.86 | |
| Purchases vending machine ac | Boys (n = 542) | 1.27 | 0.75; 2.17 | 1.18 | 0.67; 2.05 | 1.18 | 0.68; 2.03 | 1.21 | 0.69; 2.12 |
| Girls (n = 675) | 1.06 | 0.74; 1.50 | 1.14 | 0.77; 1.69 | 1.18 | 0.79; 1.75 | 1.15 | 0.75; 1.78 | |
| Purchases cafeteria and vending machine ad | Boys (n = 620) | 1.17 | 0.84; 1.62 | 1.19 | 0.83; 1.73 | 1.19 | 0.83; 1.70 | 1.14 | 0.79; 1.65 |
| Girls (n = 756) | 0.87 | 0.61; 1.26 | 0.89 | 0.61; 1.28 | 0.90 | 0.62; 1.30 | 0.90 | 0.61; 1.34 | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Evenhuis, I.J.; Jacobs, S.M.; Vyth, E.L.; Veldhuis, L.; de Boer, M.R.; Seidell, J.C.; Renders, C.M. The Effect of Supportive Implementation of Healthier Canteen Guidelines on Changes in Dutch School Canteens and Student Purchase Behaviour. Nutrients 2020, 12, 2419. https://doi.org/10.3390/nu12082419
Evenhuis IJ, Jacobs SM, Vyth EL, Veldhuis L, de Boer MR, Seidell JC, Renders CM. The Effect of Supportive Implementation of Healthier Canteen Guidelines on Changes in Dutch School Canteens and Student Purchase Behaviour. Nutrients. 2020; 12(8):2419. https://doi.org/10.3390/nu12082419
Chicago/Turabian StyleEvenhuis, Irma J., Suzanne M. Jacobs, Ellis L. Vyth, Lydian Veldhuis, Michiel R. de Boer, Jacob C. Seidell, and Carry M. Renders. 2020. "The Effect of Supportive Implementation of Healthier Canteen Guidelines on Changes in Dutch School Canteens and Student Purchase Behaviour" Nutrients 12, no. 8: 2419. https://doi.org/10.3390/nu12082419
APA StyleEvenhuis, I. J., Jacobs, S. M., Vyth, E. L., Veldhuis, L., de Boer, M. R., Seidell, J. C., & Renders, C. M. (2020). The Effect of Supportive Implementation of Healthier Canteen Guidelines on Changes in Dutch School Canteens and Student Purchase Behaviour. Nutrients, 12(8), 2419. https://doi.org/10.3390/nu12082419






