Gastroprotective and Healing Effects of Polygonum cuspidatum Root on Experimentally Induced Gastric Ulcers in Rats
Abstract
:1. Introduction
2. Materials and Methods
2.1. Plant Materials and Sample Preparation
2.2. High-Performance Liquid Chromatography (HPLC) Analysis
2.3. Animals
2.4. HCl/EtOH-Induced Acute Gastric Lesions
2.5. Indomethacin-Induced Acute Gastric Lesions
2.6. Acetic Acid-Induced Chronic Gastric Lesions
2.7. Gastric Secretion in Pylorus-Ligated Rats
2.8. Measurement of Superoxide Dismutase (SOD), Glutathione (GSH) Level, and Catalase (CAT) Activity
2.9. Determination of PGE2
2.10. Statistical Analysis
3. Results
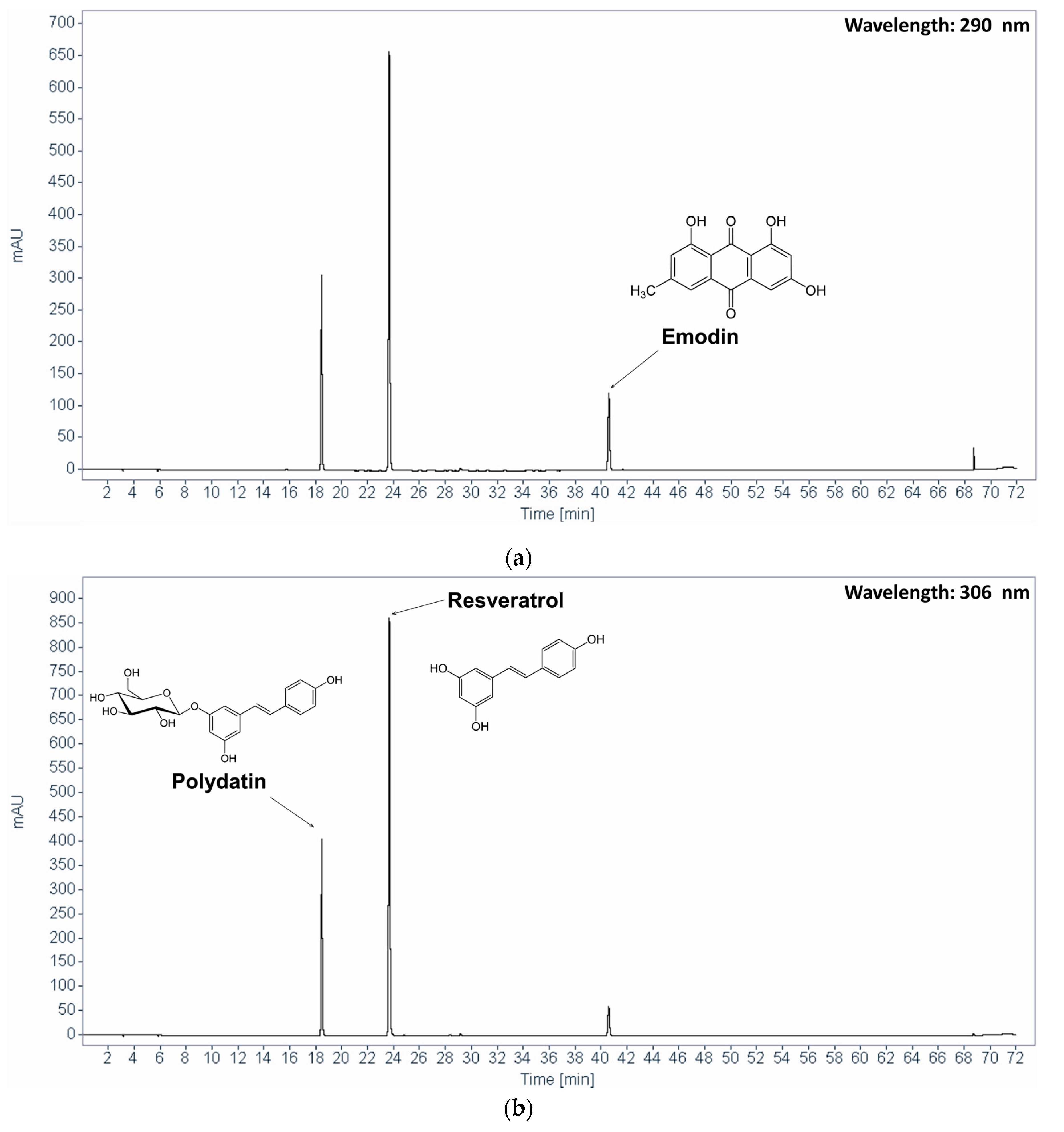
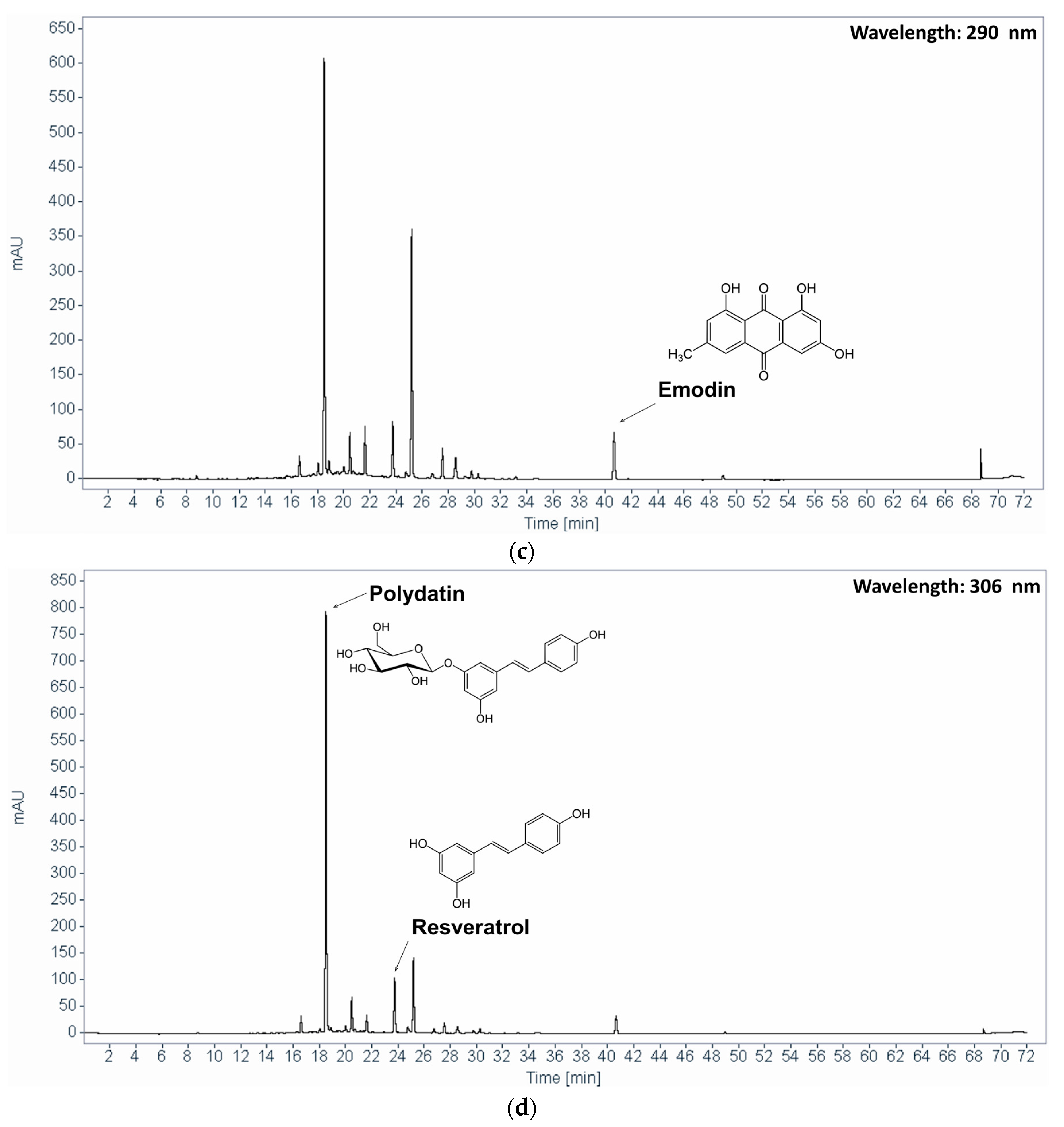
3.1. HPLC Analysis of PCE
3.2. Effect of PCE on HCl/EtOH-Induced Acute Gastric Lesions
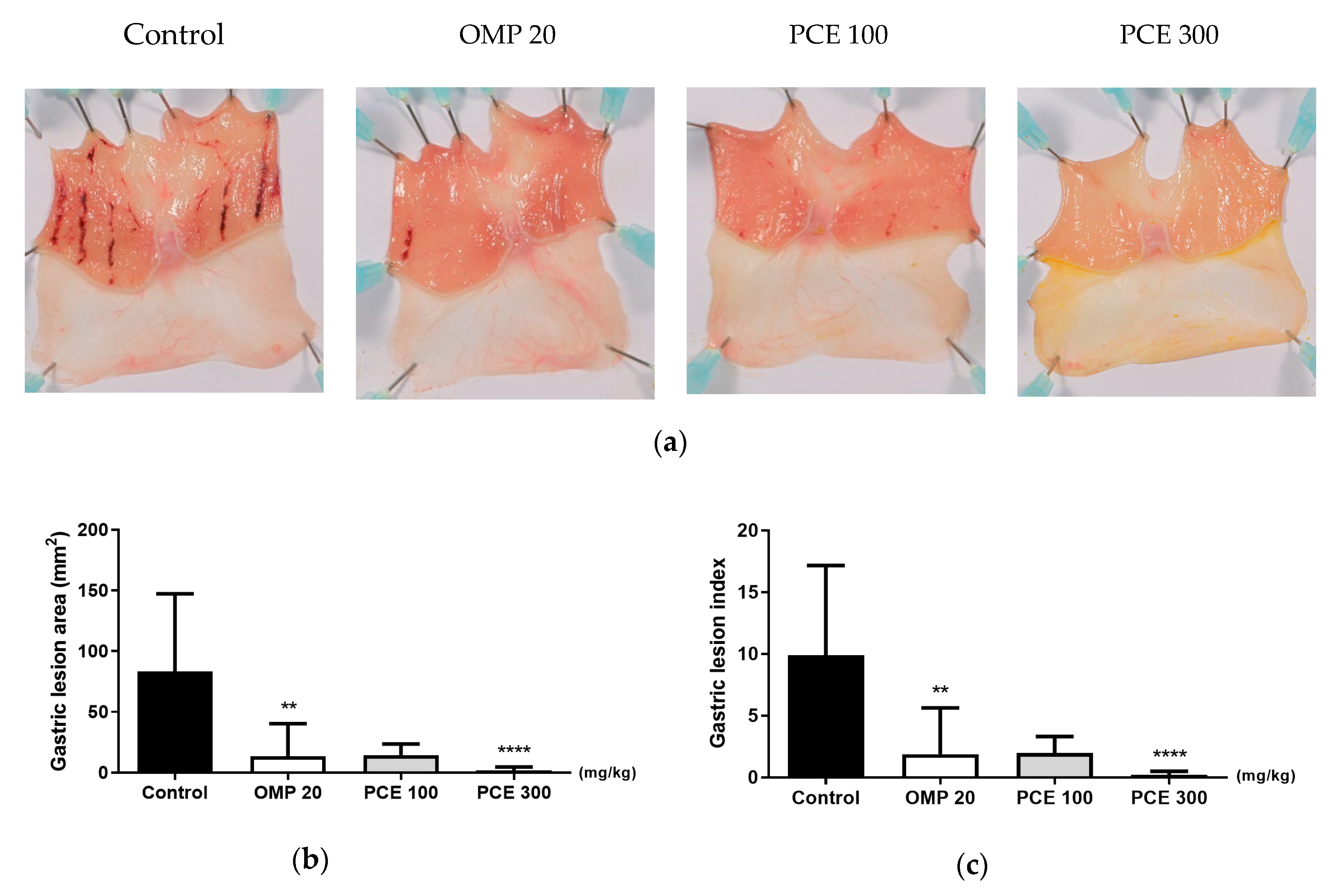
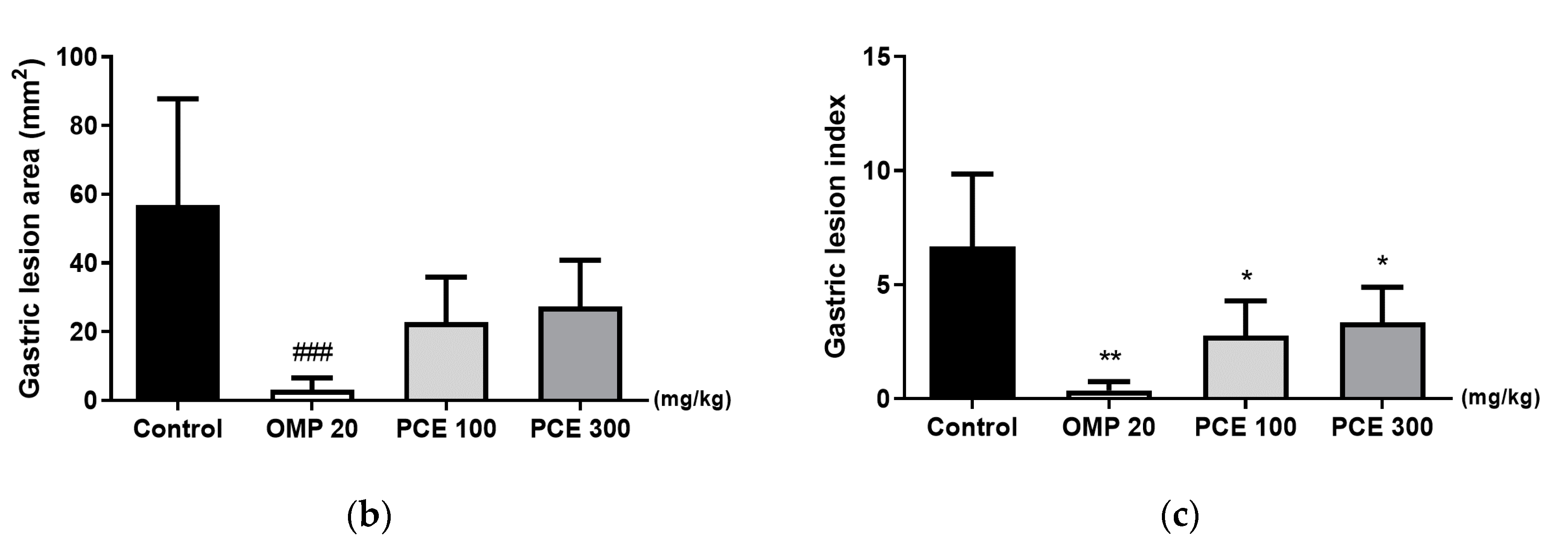
3.3. Effect of PCE on Indomethacin-Induced Acute Gastric Lesions
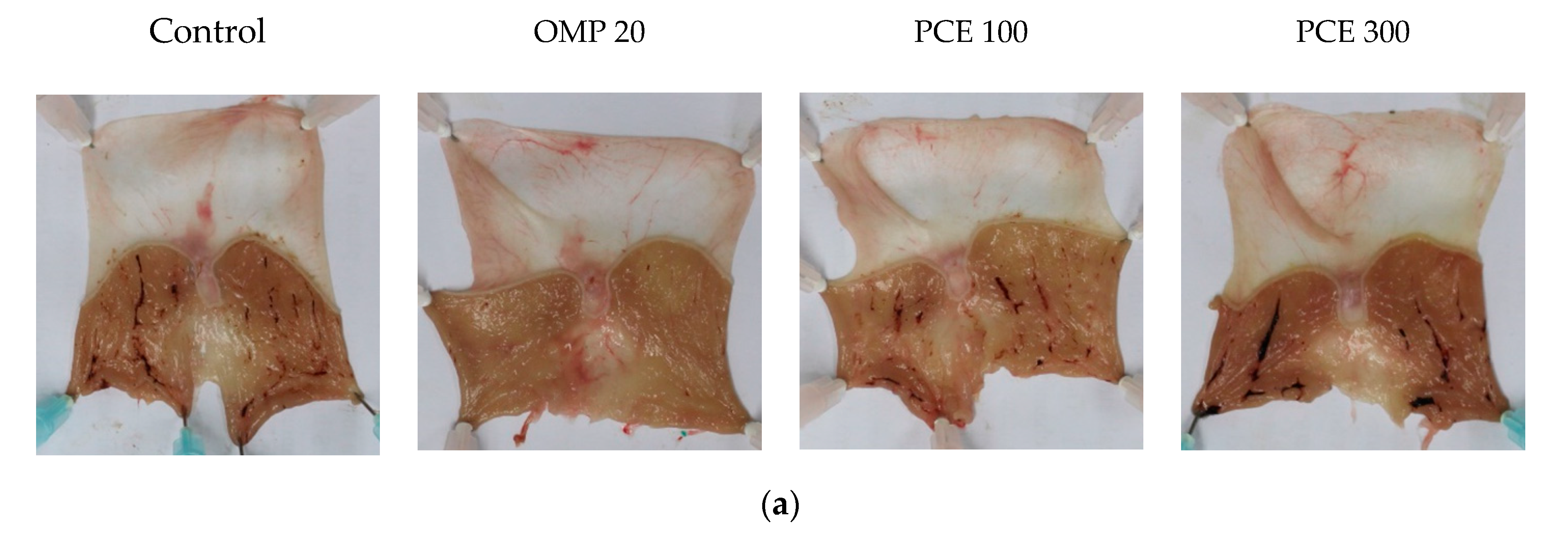
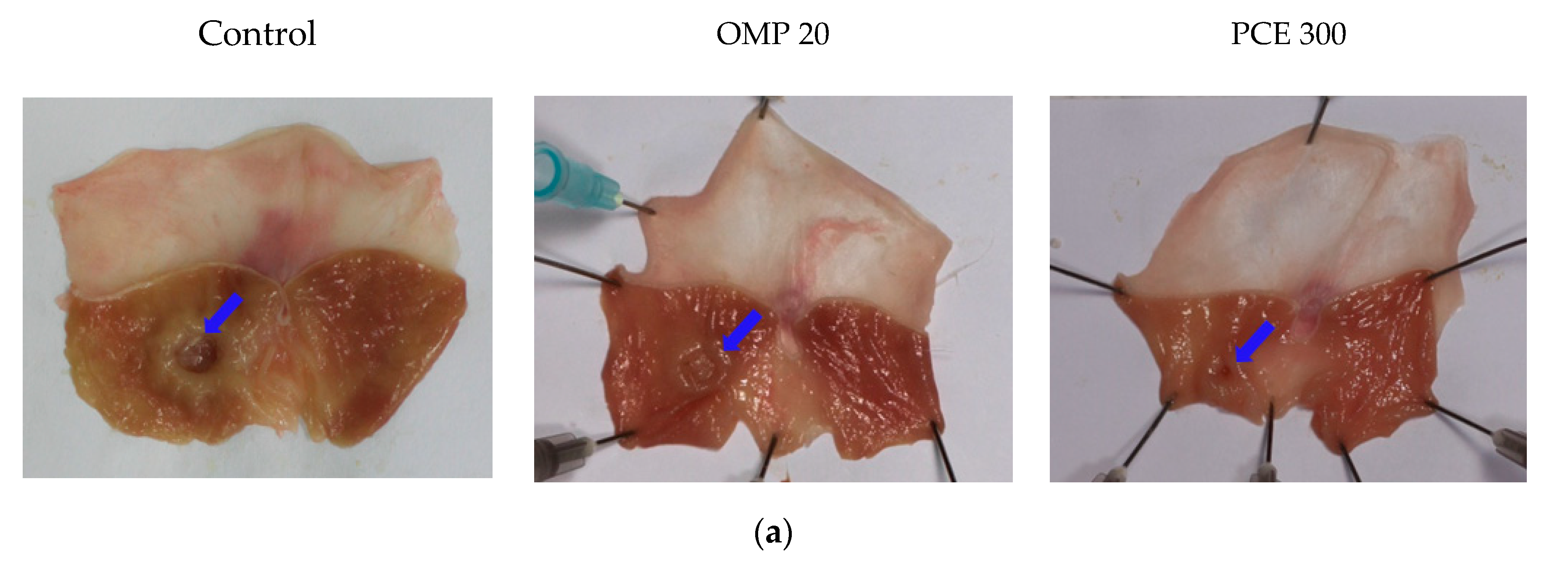
3.4. Healing Effect of PCE on Acetic Acid-Induced Chronic Gastric Ulcer
3.5. Effect of PCE on Gastric Secretion
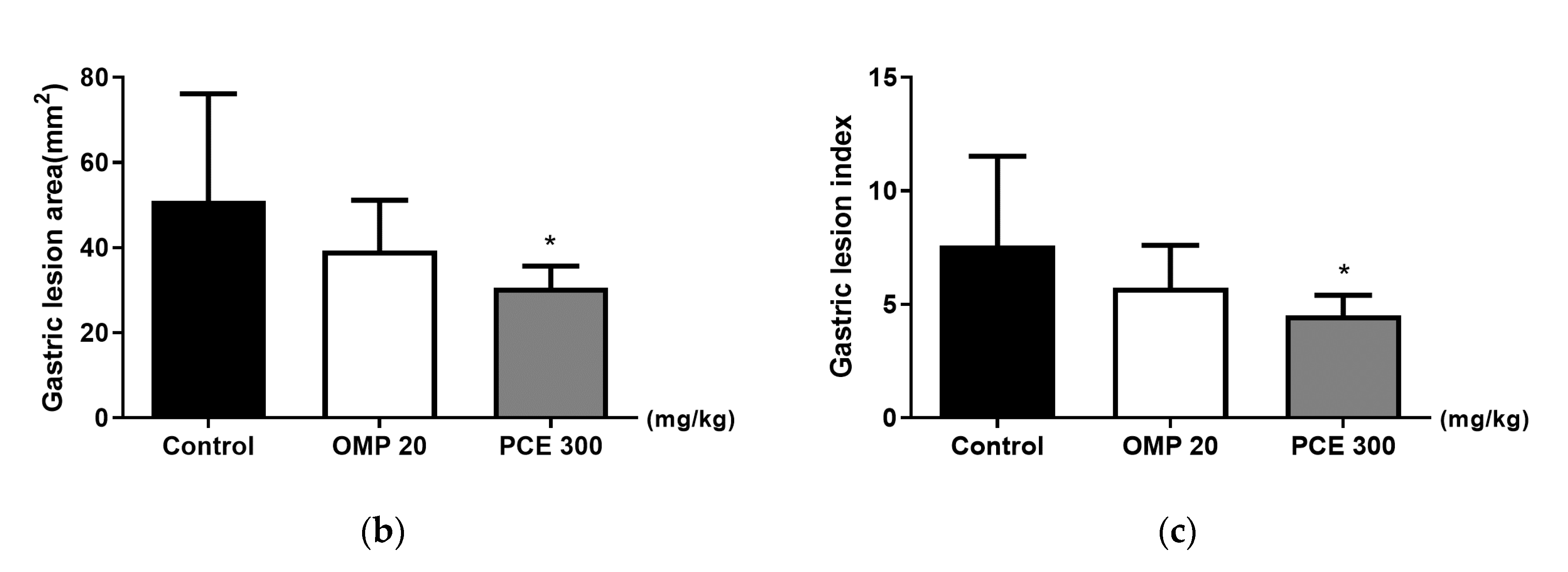
3.6. Effects of PCE on the Levels of SOD, GSH, and CAT in the Stomach Tissue of the HCl/EtOH-Treated Rats
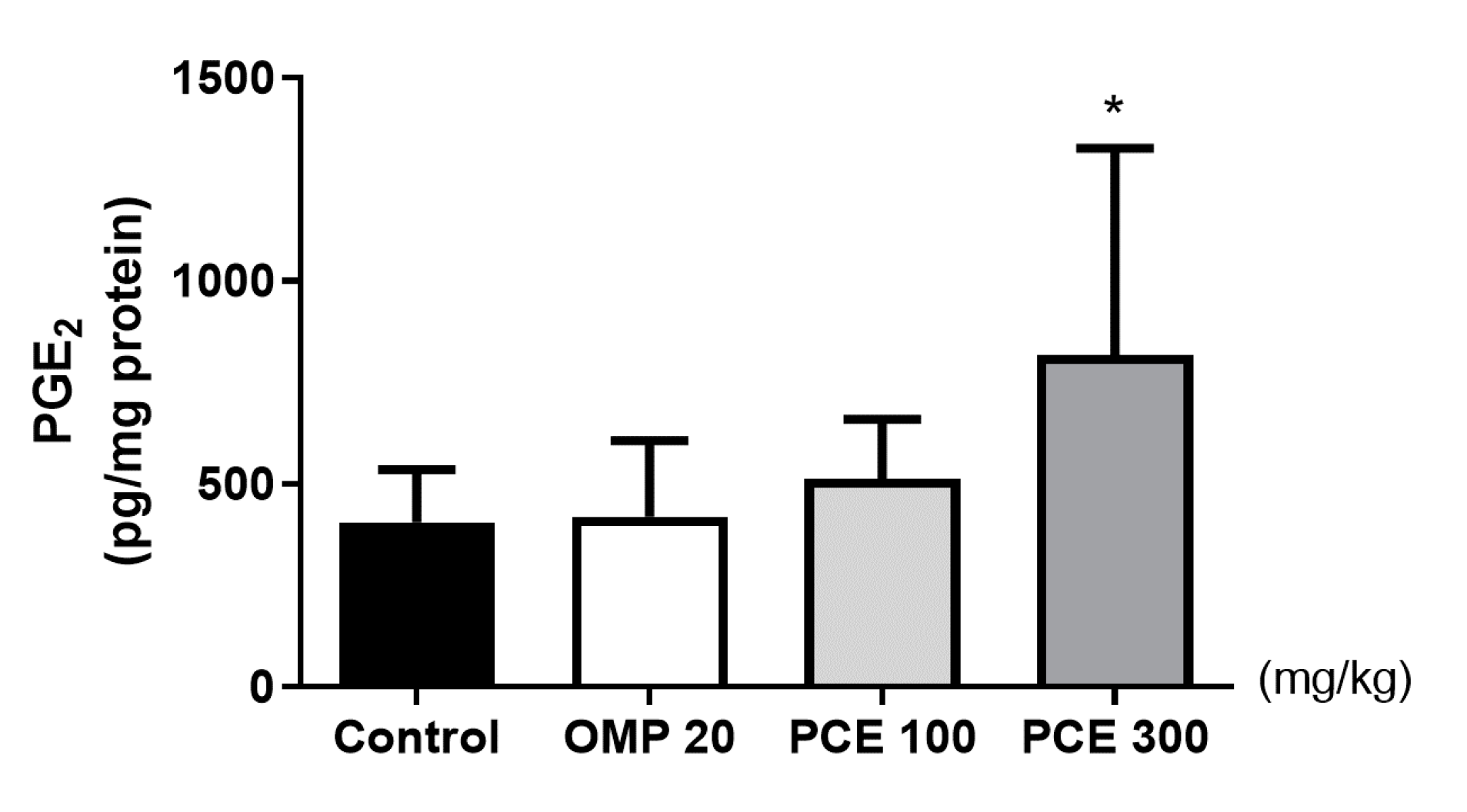
3.7. Effects of PCE on the PGE2 Level of Stomach Tissue
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Teschke, R.; Wolff, A.; Frenzel, C.; Eickhoff, A.; Schulze, J. Herbal traditional Chinese medicine and its evidence base in gastrointestinal disorders. World J. Gastroenterol. 2015, 21, 4466. [Google Scholar] [CrossRef] [PubMed]
- Megala, J.; Geetha, A. Antiulcerogenic activity of hydroalcoholic fruit extract of Pithecellobium dulce in different experimental ulcer models in rats. J. Ethnopharmacol. 2012, 142, 415–421. [Google Scholar] [CrossRef] [PubMed]
- Gururatsakul, M.; Holloway, R.H.; Talley, N.J.; Holtmann, G.J. Association between clinical manifestations of complicated and uncomplicated peptic ulcer and visceral sensory dysfunction. J. Gastroenterol. Hepatol. 2010, 25, 1162–1169. [Google Scholar] [CrossRef] [PubMed]
- Barkun, A.; Leontiadis, G. Systematic review of the symptom burden, quality of life impairment and costs associated with peptic ulcer disease. Am. J. Med. 2010, 123, 358–366.e2. [Google Scholar] [CrossRef]
- Kurata, J.; Haile, B. Epidemiology of peptic ulcer disease. Clin. Gastroenterol. 1984, 13, 289–307. [Google Scholar]
- Kim, S.G.; Kim, J.G.; Shin, S.K.; Kim, H.S.; Seol, S.Y. Guidelines of diagnosis for peptic ulcer disease. Korean J. Gastroenterol. 2009, 54, 279–284. [Google Scholar] [CrossRef] [Green Version]
- Khushtar, M.; Siddiqui, H.H.; Dixit, R.K.; Khan, M.S.; Iqbal, D.; Rahman, M.A. Amelioration of gastric ulcers using a hydro-alcoholic extract of Triphala in indomethacin-induced Wistar rats. Eur. J. Integr. Med. 2016, 8, 546–551. [Google Scholar] [CrossRef]
- Adinortey, M.B.; Ansah, C.; Galyuon, I.; Nyarko, A. In vivo models used for evaluation of potential antigastroduodenal ulcer agents. Ulcers 2013, 2013, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Okabe, S.; Pfeiffer, C.J. Chronicity of acetic acid ulcer in the rat stomach. Am. J. Dig. Dis. 1972, 17, 619–629. [Google Scholar] [CrossRef]
- Penston, J.G. A decade of experience with long-term continuous treatment of peptic ulcers with H2-receptor antagonists. Aliment. Pharmacol. Ther. 1993, 7, 27–33. [Google Scholar] [CrossRef]
- Boeing, T.; da Silva, L.M.; Somensi, L.B.; Cury, B.J.; Costa, A.P.M.; Petreanu, M.; Niero, R.; de Andrade, S.F. Antiulcer mechanisms of Vernonia condensata Baker: A medicinal plant used in the treatment of gastritis and gastric ulcer. J. Ethnopharmacol. 2016, 184, 196–207. [Google Scholar] [CrossRef] [PubMed]
- Chey, W.D.; Leontiadis, G.I.; Howden, C.W.; Moss, S.F. ACG Clinical guideline: Treatment of Helicobacter pylori infection. Am. J. Gastroenterol. 2017, 112, 212–239. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.H.; Lee, D.J.; Kim, K.M.; Park, S.B.; Kim, B.T.; Joo, N.S.; Cho, D.Y.; Kim, K.N.; Seo, S.W.; Park, S.E.; et al. Diagnosis and management of peptic ulcer disease. Korean J. Fam. Pract. 2013, 3, 395–405. [Google Scholar]
- Peng, W.; Qin, R.; Li, X.; Zhou, H. Botany, phytochemistry, pharmacology, and potential application of Polygonum cuspidatum Sieb.et Zucc.: A review. J. Ethnopharmacol. 2013, 148, 729–745. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Chen, M.X.; Kongstad, K.T.; Jäger, A.K.; Staerk, D. Potential of Polygonum cuspidatum root as an antidiabetic food: Dual high-resolution α-glucosidase and PTP1B inhibition profiling combined with HPLC-HRMS and NMR for identification of antidiabetic constituents. J. Agric. Food Chem. 2017, 65, 4421–4427. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.; Kim, H.; Ko, H. Endothelium dependent vasorelaxant effect of aqueous extract of Polygoni cuspidatae radix on arterial contraction in rabbit. Korean J. Orient. Physiol. Pathol. 2008, 22, 131–136. [Google Scholar]
- Sohn, E.; Kim, J.; Kim, C.S.; Lee, Y.M.; Kim, J.S. Extract of Polygonum cuspidatum attenuates diabetic retinopathy by inhibiting the high-mobility group box-1 (HMGB1) signaling pathway in streptozotocin-induced diabetic rats. Nutrients 2016, 8, 140. [Google Scholar] [CrossRef]
- Ding, X.P.; Zhang, C.L.; Qi, J.; Sun, L.Q.; Qin, M.J.; Yu, B.Y. The Spectrum-Effect integrated fingerprint of Polygonum cuspidatum based on HPLC-diode array detection-flow injection-chemiluminescence. Chin. J. Nat. Med. 2013, 11, 546–552. [Google Scholar] [CrossRef]
- Park, B.; Lee, I.S.; Hyun, S.W.; Jo, K.; Lee, T.G.; Kim, J.S.; Kim, C.S. The protective effect of polygonum cuspidatum (PCE) aqueous extract in a dry eye model. Nutrients 2018, 10, 1550. [Google Scholar] [CrossRef] [Green Version]
- Park, B.; Jo, K.; Lee, T.G.; Hyun, S.W.; Kim, J.S.; Kim, C.S. Polydatin inhibits NLRP3 inflammasome in dry eye disease by attenuating oxidative stress and inhibiting the NF-κB pathway. Nutrients 2019, 11, 2792. [Google Scholar] [CrossRef] [Green Version]
- Hussein, S.A.; Karousa, M.M.; Amin, A.; Awadalla, M.A. Evaluation of gastroprotective effect and anti-inflammatory role of resveratrol against gastric mucosal alterations in experimental model of gastritis in rats. Int. J. Pharma Sci. 2016, 6, 1559–1570. [Google Scholar]
- Solmaz, A.; Şener, G.; Çetinel, Ş.; Yüksel, M.; Yeğen, C.; Yeğen, B.Ç. Protective and therapeutic effects of resveratrol on acetic acid-induced gastric ulcer. Free Radic. Res. 2009, 43, 594–603. [Google Scholar] [CrossRef] [PubMed]
- Mishra, V. Potent gastroprotective effect chrysophanol and emodin from Rehum Emodi via H+ K+ atpase inhibition and increasing the PGE2 Level in rats. Nat. Prod. Indian J. 2016, 12, 1–12. [Google Scholar]
- Mizui, T.; Doteuchi, M. Effect of polyamines on acidified ethanol-induced gastric lesions in rats. Jpn. J. Pharmacol. 1983, 33, 939–945. [Google Scholar] [CrossRef]
- Okabe, S.; Amagase, K. An overview of acetic acid ulcer models—The history and state of the art of peptic ulcer research. Biol. Pharm. Bull. 2005, 28, 1321–1341. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shay, H.; Gruenstein, M. A simple and safe method for the gastric instillation of fluids in the rat. J. Lab. Clin. Med. 1946, 31, 1384–1386. [Google Scholar]
- Saremi, K.; Rad, S.K.; Tayeby, F.; Abdulla, M.A.; Karimian, H.; Majid, N.A. Gastroprotective activity of a novel schiff base derived dibromo substituted compound against ethanol-induced acute gastric lesions in rats. BMC Pharmacol. Toxicol. 2019, 20, 13. [Google Scholar] [CrossRef]
- Marhuenda, E.; Martin, M.J.; Lastra, C.D. Antiulcerogenic activity of aescine in different experimental models. Phytother. Res. 1993, 7, 13–16. [Google Scholar] [CrossRef]
- Takeuchi, K. Pathogenesis of NSAID-induced gastric damage: Importance of cyclooxygenase inhibition and gastric hypermotility. World J. Gastroenterol. 2012, 18, 2147. [Google Scholar] [CrossRef]
- Takagi, K.; Okabe, S.; Saziki, R. A new method for the production of chronic gastric ulcer in rats and the effect of several drugs on its healing. Jpn. J. Pharmacol. 1969, 19, 418–426. [Google Scholar] [CrossRef] [Green Version]
- Banerjee, D.; Maity, B.; Nag, S.K.; Bandyopadhyay, S.K.; Chattopadhyay, S. Healing potential of Picrorhiza kurroa (Scrofulariaceae) rhizomes against indomethacin-induced gastric ulceration: A mechanistic exploration. BMC Complementary Altern. Med. 2008, 8, 3. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Konturek, S.; Konturek, P.; Brzozowski, T. Prostaglandins and ulcer healing. J. Physiol. Pharmacol. 2005, 56, 5. [Google Scholar] [PubMed]
- Baiubon, P.; Kunanusorn, P.; Khonsung, P.; Chiranthanut, N.; Panthong, A.; Rujjanawate, C. Gastroprotective activity of the rhizome ethanol extract of Zingiber simaoense YY Qian in rats. J. Ethnopharmacol. 2016, 194, 571–576. [Google Scholar] [CrossRef] [PubMed]
- Eastwood, G.L. Is smoking still important in the pathogenesis of peptic ulcer disease? J. Clin. Gastroenterol. 1997, 25, S1–S7. [Google Scholar] [CrossRef] [PubMed]
- Laine, L.; Takeuchi, K.; Tarnawski, A. Gastric mucosal defense and cytoprotection: Bench to bedside. Gastroenterology 2008, 135, 41–60. [Google Scholar] [CrossRef]
- Rezaie, A.; Parker, R.D.; Abdollahi, M. Oxidative stress and pathogenesis of inflammatory bowel disease: An epiphenomenon or the cause? Dig. Dis. Sci. 2007, 52, 2015–2021. [Google Scholar] [CrossRef]
- Wu, X.; Huang, Q.; Xu, N.; Cai, J.; Luo, D.; Zhang, Q.; Su, Z.; Gao, C.; Liu, Y. Antioxidative and anti-inflammatory effects of water extract of Acrostichum aureum Linn. against ethanol-induced gastric ulcer in rats. Evid. Based Complementary Altern. Med. 2018, 2018, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Song, S.H.; Kim, J.E.; Sung, J.E.; Lee, H.A.; Yun, W.B.; Lee, Y.H.; Song, H.; Hwang, D. Anti-ulcer effect of Gallarhois extract with anti-oxidant activity in an ICR model of ethanol/hydrochloride acid-induced gastric injury. J. Tradit. Complementary Med. 2019, 9, 372–382. [Google Scholar] [CrossRef]
- Zhou, D.; Yang, Q.; Tian, T.; Chang, Y.; Li, Y.; Duan, L.R.; Li, H.; Wang, S.W. Gastroprotective effect of gallic acid against ethanol-induced gastric ulcer in rats: Involvement of the Nrf2/HO-1 signaling and anti-apoptosis role. Biomed. Pharmacother. 2020, 126, 110075. [Google Scholar] [CrossRef]
- Szabo, S.; Trier, J.S.; Frankel, P.W. Sulfhydryl compounds may mediate gastric cytoprotection. Science 1981, 214, 200–202. [Google Scholar] [CrossRef]
- Zaghlool, S.S.; Abo-Seif, A.A.; Rabeh, M.A.; Abdelmohsen, U.R.; Messiha, B.A. Gastro-protective and anti-oxidant potential of Althaea officinalis and Solanum nigrum on pyloric ligation/indomethacin-induced ulceration in rats. Antioxidants 2019, 8, 512. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Antonisamy, P.; Arasu, M.V.; Dhanasekaran, M.; Choi, K.C.; Aravinthan, A.; Kim, N.S.; Kang, C.W.; Kim, J.H. Protective effects of trigonelline against indomethacin-induced gastric ulcer in rats and potential underlying mechanisms. Food Funct. 2016, 7, 398–408. [Google Scholar] [CrossRef] [PubMed]
- Mei, X.T.; Xu, D.H.; Xu, S.K.; Zheng, Y.P.; Xu, S.B. Zinc (II)–curcumin accelerates the healing of acetic acid-induced chronic gastric ulcers in rats by decreasing oxidative stress and downregulation of matrix metalloproteinase-9. Food Chem. Toxicol. 2013, 60, 448–454. [Google Scholar] [CrossRef]
- Perico, L.L.; Heredia-Vieira, S.C.; Beserra, F.P.; de Cassia Dos Santos, R.; Weiss, M.B.; Resende, F.A.; Dos Santos Ramos, M.A.; Bonifacio, B.V.; Bauab, T.M.; Varanda, E.A.; et al. Does the gastroprotective action of a medicinal plant ensure healing effects? An integrative study of the biological effects of Serjania marginata Casar. (Sapindaceae) in rats. J. Ethnopharmacol. 2015, 172, 312–324. [Google Scholar] [CrossRef] [PubMed]
- Malfertheiner, P.; Chan, F.K.; McColl, K.E. Peptic ulcer disease. The lancet 2009, 374, 1449–1461. [Google Scholar] [CrossRef]
- Uzal, F.A.; Plattner, B.L.; Hostetter, J.M. Alimentary system. In Jubb, Kennedy and Palmer’s Pathology of Domestic Animals, 6th ed.; Maxie, M.G., Ed.; Elsevier: St. Louis, MO, USA, 2016; Volume 2, p. 46. [Google Scholar]
- Jaikumar, S.; Ramaswamy, S.; Asokan, B.R.; Mohan, T.; Gnanavel, M. Anti ulcer activity of methanolic extract of Jatropha curcas (Linn.) on Aspirin-induced gastric lesions in Wistar strain rats. Res. J. Pharm. Biol. Chem. Sci. 2010, 1, 886–897. [Google Scholar]
- D’Argenio, G.; Mazzone, G.; Tuccillo, C.; Grandone, I.; Gravina, A.G.; Graziani, G.; Fogliano, V.; Romano, M. Apple polyphenol extracts prevent aspirin-induced damage to the rat gastric mucosa. Br. J. Nutr. 2008, 100, 1228–1236. [Google Scholar] [CrossRef] [Green Version]
- Rodriguez, L.G.; Lagergren, J.; Lindblad, M. Gastric acid suppression and risk of oesophageal and gastric adenocarcinoma: A nested case control study in the UK. Gut 2006, 55, 1538–1544. [Google Scholar] [CrossRef] [Green Version]
| Groups | Gastric Volume (mL) | Gastric pH | Free Acidity (mEq/mL) | Total Acidity (mEq/mL) |
|---|---|---|---|---|
| Control | 5.99 ± 1.64 | 1.68 ± 0.18 | 8.00 ± 2.86 | 13.72 ± 2.31 |
| OMP 20 mg/kg | 4.30 ± 0.99 | 3.07 ± 1.42 * | 2.33 ± 2.66 ## | 9.58 ± 3.98 |
| PCE 100 mg/kg | 4.52 ± 1.85 | 1.87 ± 0.60 | 7.08 ± 3.38 | 13.83 ± 2.40 |
| PCE 300 mg/kg | 6.24 ± 1.50 | 1.59 ± 0.15 | 9.40 ± 1.95 | 14.00 ± 2.32 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, Y.-S.; Nam, Y.; Song, J.; Kim, H. Gastroprotective and Healing Effects of Polygonum cuspidatum Root on Experimentally Induced Gastric Ulcers in Rats. Nutrients 2020, 12, 2241. https://doi.org/10.3390/nu12082241
Kim Y-S, Nam Y, Song J, Kim H. Gastroprotective and Healing Effects of Polygonum cuspidatum Root on Experimentally Induced Gastric Ulcers in Rats. Nutrients. 2020; 12(8):2241. https://doi.org/10.3390/nu12082241
Chicago/Turabian StyleKim, Young-Sik, YunSeol Nam, Jungbin Song, and Hocheol Kim. 2020. "Gastroprotective and Healing Effects of Polygonum cuspidatum Root on Experimentally Induced Gastric Ulcers in Rats" Nutrients 12, no. 8: 2241. https://doi.org/10.3390/nu12082241
APA StyleKim, Y.-S., Nam, Y., Song, J., & Kim, H. (2020). Gastroprotective and Healing Effects of Polygonum cuspidatum Root on Experimentally Induced Gastric Ulcers in Rats. Nutrients, 12(8), 2241. https://doi.org/10.3390/nu12082241





