Association between the Potential Influence of a Lifestyle Intervention in Older Individuals with Excess Weight and Metabolic Syndrome on Untreated Household Cohabitants and Their Family Support: The PREDIMED-Plus Study
Abstract
1. Introduction
2. Material and Methods
2.1. Study Design
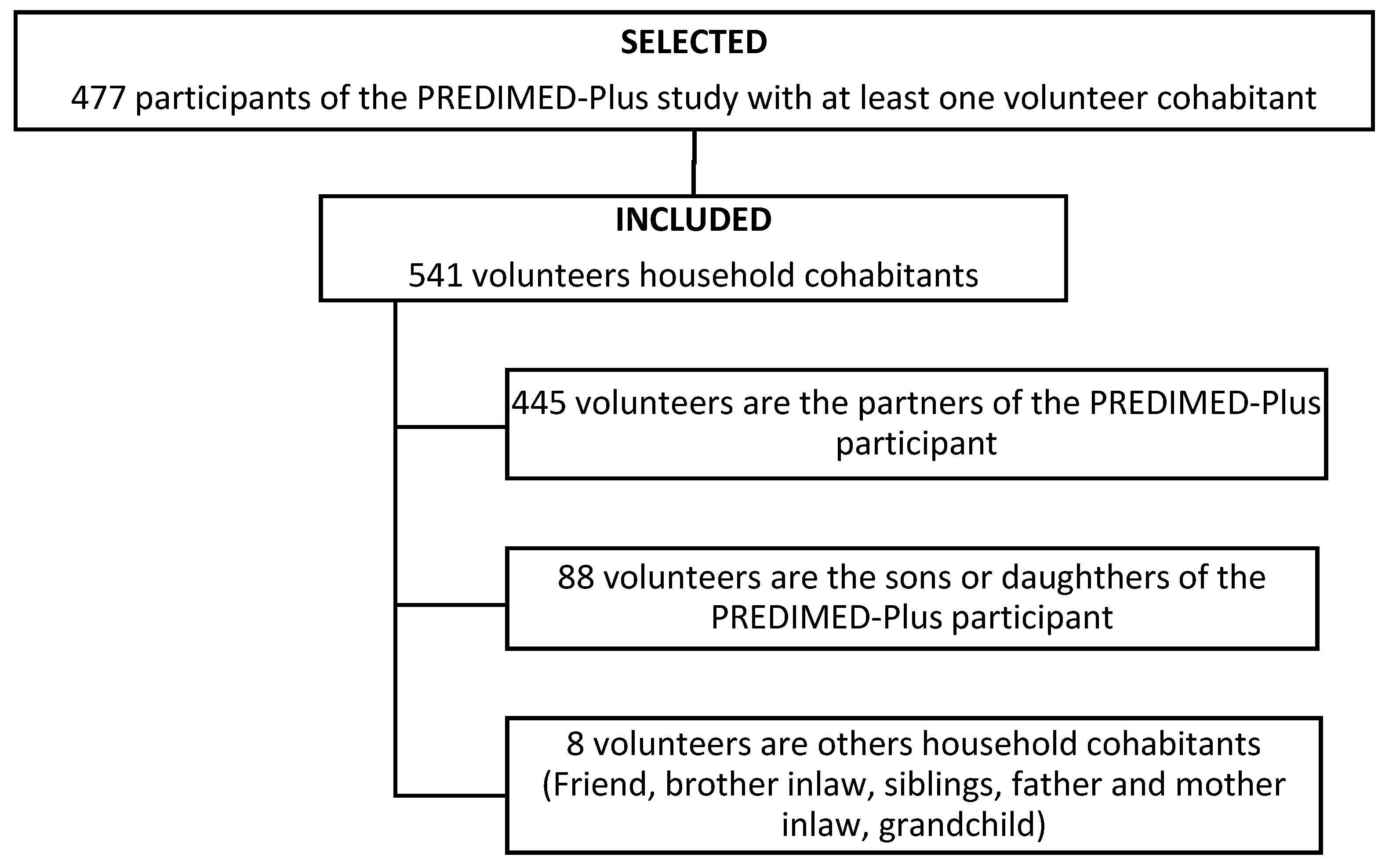
2.2. Participants, Recruitment, and Randomization
2.3. Sociodemographic and Anthropometric Variables
2.4. Adherence to the Mediterranean Diet
2.5. Physical Activity
2.6. Social Characteristics of the Household Cohabitants
2.6.1. Family Function
2.6.2. Social Support
2.7. PREDIMED-Plus Lifestyle Intervention
2.8. Statistical Analysis
3. Results
3.1. Associations among the PREDIMED-Plus Participants’ Sons and Daughters
3.2. Associations among the PREDIMED-Plus Participants’ Partners
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| BMI | body mass index |
| IR | interquartile range |
| erMedDiet | energy-restricted Mediterranean diet |
| MedDiet | Mediterranean diet |
| MET | metabolic equivalent |
| PREDIMED | prevención con dieta Mediterránea |
| SD | standard deviation |
References
- Ng, M.; Fleming, T.; Robinson, M.; Thomson, B.; Graetz, N.; Margono, C.; Mullany, E.C.; Biryukov, S.; Abbafati, C.; Abera, S.F.; et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014, 384, 766–781. [Google Scholar] [CrossRef]
- Woodard, G.A.; Encarnacion, B.; Peraza, J.; Hernandez-Boussard, T.; Morton, J. Halo effect for bariatric surgery: Collateral weight loss in patients’ family members. Arch. Surg. 2011, 146, 1185–1190. [Google Scholar] [CrossRef] [PubMed]
- Lent, M.R.; Bailey-Davis, L.; Irving, B.A.; Wood, G.C.; Cook, A.M.; Hirsch, A.G.; Still, C.D.; Benotti, P.N.; Franceschelli-Hosterman, J. Bariatric surgery patients and their families: Health, physical activity, and social support. Obes. Surg. 2016, 26, 2981–2988. [Google Scholar] [CrossRef] [PubMed]
- Madan, A.K.; Turman, K.A.; Tichansky, D.S. Weight changes in spouses of gastric bypass patients. Obes. Surg. 2005, 15, 191–194. [Google Scholar] [CrossRef] [PubMed]
- Pearson, D.; Scott, J.D.; Beffa, L.; Rhyne, R.; Shull, T. Is there a “halo effect” for bariatric surgery? Am. Surg. 2018, 84, e328–e329. [Google Scholar] [CrossRef] [PubMed]
- Berglind, D.; Willmer, M.; Tynelius, P.; Ghaderi, A.; Näslund, E.; Rasmussen, F. Women undergoing Roux-en-Y Gastric Bypass surgery: Family resemblance in pre- to postsurgery physical activity and sedentary behavior in children and spouses. Surg. Obes. Relat. Dis. 2015, 11, 690–696. [Google Scholar] [CrossRef]
- Gorin, A.A.; Wing, R.R.; Fava, J.L.; Jakicic, J.M.; Jeffery, R.; West, D.S.; Brelje, K.; Dilillo, V.G.; Bright, R.; Pera, V.; et al. Weight loss treatment influences untreated spouses and the home environment: Evidence of a ripple effect. Int. J. Obes. 2008, 32, 1678–1684. [Google Scholar] [CrossRef]
- Golan, R.; Schwarzfuchs, D.; Stampfer, M.J.; Shai, I. Halo effect of a weight-loss trial on spouses: The DIRECT-Spouse study. Public Health Nutr. 2010, 13, 544–549. [Google Scholar] [CrossRef]
- Rossini, R.; Moscatiello, S.; Tarrini, G.; Di Domizio, S.; Soverini, V.; Romano, A.; Mazzotti, A.; Dalle Grave, R.; Marchesini, G. Effects of cognitive-behavioral treatment for weight loss in family members. J. Am. Diet. Assoc. 2011, 111, 1712–1719. [Google Scholar] [CrossRef] [PubMed]
- Macario, E.; Sorensen, G. Spousal similarities in fruit and vegetable consumption. Am. J. Health Promot. 1998, 12, 369–377. [Google Scholar] [CrossRef]
- Vauthier, J.M.; Lluch, A.; Lecomte, E.; Artur, Y.; Herbeth, B. Family resemblance in energy and macronutrient intakes: The Stanislas Family Study. Int. J. Epidemiol. 1996, 25, 1030–1037. [Google Scholar] [CrossRef]
- Aggarwal, B.; Liao, M.; Allegrante, J.P.; Mosca, L. Low social support level is associated with non-adherence to diet at 1 year in the family intervention trial for heart health (FIT heart). J. Nutr. Educ. Behav. 2010, 42, 380–388. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez Martín, A.; Novalbos Ruiz, J.P.; Martinez Nieto, J.M.; Escobar Jiménez, L.; Castro de Haro, A.L. Characteristics of eating disorders in a university hospital-based Spanish population. Eur. J. Clin. Nutr. 2005, 59, 459–462. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Rodríguez Martín, A.; Novalbos Ruiz, J.P.; Martínez Nieto, J.M.; Escobar Jiménez, L.; Castro de Haro, A.L. Epidemiological study of the influence of family and socioeconomic status in disorders of eating behaviour. Eur. J. Clin. Nutr. 2004, 58, 846–852. [Google Scholar] [CrossRef] [PubMed]
- Martínez-González, M.A.; Buil-Cosiales, P.; Corella, D.; Bulló, M.; Fitó, M.; Vioque, J.; Romaguera, D.; Martínez, J.A.; Wärnberg, J.; López-Miranda, J.; et al. Cohort Profile: Design and methods of the PREDIMED-Plus randomized trial. Int. J. Epidemiol. 2018, 48. [Google Scholar] [CrossRef]
- Salas-Salvadó, J.; Díaz-López, A.; Ruiz-Canela, M.; Basora, J.; Fitó, M.; Corella, D.; Serra-Majem, L.; Wärnberg, J.; Romaguera, D.; Estruch, R.; et al. Effect of a lifestyle intervention program with energy-restricted mediterranean diet and exercise on weight loss and cardiovascular risk factors: One-year results of the PREDIMED-plus trial. Diabetes Care 2019, 42, 777–788. [Google Scholar] [CrossRef]
- Schro, H.; Corella, D.; Salas-salvado, J.; Lamuela-ravento, R.; Ros, E.; Salaverrı, I.; Vinyoles, E.; Go, E. A short screener is valid for assessing Mediterranean diet adherence among older. J. Nutr. 2011, 141, 1140–1145. [Google Scholar] [CrossRef]
- Elosua, R.; Marrugat, J.; Molina, L.; Pons, S.; Pujol, E. Validation of the Minnesota leisure time physical activity questionnaire in Spanish men. The MARATHOM investigators. Am. J. Epidemiol. 1994, 139, 1197–1209. [Google Scholar] [CrossRef]
- Elosua, R.; Garcia, M.; Aguilar, A.; Molina, L.; Covas, M.I.; Marrugat, J. Validation of the Minnesota leisure time physical activity questionnaire in Spanish women. Investigators of the MARATDON Group. Med. Sci. Sports Exerc. 2000, 32, 1431–1437. [Google Scholar] [CrossRef]
- Bellón Saameño, J.; Delgado Sánchez, A.; Luna del Castillo, J.D.D.; Lardelli Claret, P. Validez y fiabilidad del cuestionario de función familiar Apgar-familiar. Aten. Primaria 1996, 18, 273–342. [Google Scholar]
- Smilkstein, G.; Ashworth, C.; Montano, D. Validity and reliability of the family APGAR as a test of family function. J. Fam. Pract. 1982, 15, 303–311. [Google Scholar] [PubMed]
- Broadhead, W.E.; Gehlbach, S.H.; De Gruy, F.V.; Kaplan, B.H. The Duke-UNC functional social support questionnaire: Measurement of social support in family medicine patients. Med. Care 1988, 26, 709–723. [Google Scholar] [CrossRef] [PubMed]
- Bellón Saameño, J.; Delgado Sánchez, A.; Luna del Castillo, J.D.D.; Lardelli Claret, P. Validez y fiabilidad del cuestionario de apoyo social funcional Duke-UNC-11. Aten. Primaria 1996, 18, 153–163. [Google Scholar] [PubMed]
- White, E.; Hurlich, M.; Thompson, R.; Woods, M.; Henderson, M.; Urban, N.; Kristal, A. Dietary changes among husbands of participants in a low-fat dietary intervention. Am. J. Prev. Med. 1991, 7, 319–325. [Google Scholar] [CrossRef]
- Shattuck, A.; White, E.; Kristal, A. How women’s adopted low-fat diets affect their husbands. Am. J. Public Health 1992, 82, 1244–1250. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Zimmerman, R.S.; Gerace, T.A.; Smith, J.C.; Benezra, J. The effects of a worksite health promotion program on the wives of fire fighters. Soc. Sci. Med. 1988, 26, 537–543. [Google Scholar] [CrossRef]
- Wen, L.K.; Shepherd, M.D.; Parchman, M.L. Family support, diet, and exercise among older Mexican Americans with type 2 diabetes. Diabetes Educ. 2004, 30, 980–993. [Google Scholar] [CrossRef] [PubMed]
- Walton, K.; Haycraft, E.; Jewell, K.; Breen, A.; Simpson, J.R.; Haines, J.; Walton, K.; Haycraft, E.; Jewell, K.; Breen, A.; et al. The family mealtime observation study (FaMOS): Exploring the role of family functioning in the association between mothers’ and fathers’ food parenting practices and children’s nutrition risk. Nutrients 2019, 11, 630. [Google Scholar] [CrossRef]
- Higgs, S.; Thomas, J. Social influences on eating. Curr. Opin. Behav. Sci. 2016, 9, 1–6. [Google Scholar] [CrossRef]
- Higgs, S. Social norms and their influence on eating behaviours. Appetite 2015, 86, 38–44. [Google Scholar] [CrossRef]
- Gottlieb, B.H.; Bergen, A.E. Social support concepts and measures. J. Psychosom. Res. 2010, 69, 511–520. [Google Scholar] [CrossRef] [PubMed]
| Son or Daughter n = 88 | Partner n = 445 | p-Value | |
|---|---|---|---|
| Sociodemographic characteristics | |||
| Age (years) | 31.5 [25.0; 41.0] | 66.0 [60.0; 70.0] | <0.001 |
| Sex * | |||
| Women | 31.8 (28) | 66.3 (295) | <0.001 |
| Men | 68.2 (60) | 33.7 (150) | |
| Education level * | |||
| University | 20.5 (18) | 17.4 (74) | 0.080 |
| High school | 21.6 (19) | 13.4 (57) | |
| Secondary school | 25.0 (22) | 23.0 (98) | |
| Elementary school | 33.0 (29) | 46.2 (197) | |
| Anthropometric measures | |||
| Weight (kg) | 78.6 (14.8) | 74.1 (13.8) | 0.030 |
| Height (cm) | 172 (9.05) | 163 (7.95) | <0.001 |
| BMI (kg/m2) | 26.2 (5.0) | 27.8 (4.5) | 0.022 |
| Chronic disease prevalence * | |||
| Hypertension | 29.9 (26) | 40.4 (175) | 0.085 |
| Dyslipidemia | 25.0 (22) | 41.1 (177) | 0.007 |
| Type 2 diabetes mellitus | 9.0 (8) | 15.9 (69) | 0.140 |
| Lifestyle | |||
| Adherence to the MedDiet (score) | 7.00 [5.00; 8.00] | 9.00 [8.00; 10.0] | <0.001 |
| Physical activity (METs/min/week) | 1954 [988; 3402] | 1866 [871; 3432] | 0.727 |
| Eating together (times per week) | 8.00 [6.00; 14.0] | 16.0 [13.0; 21.0] | <0.001 |
| Social characteristics of the household PREDIMED-Plus cohabitants | |||
| Family function (score) | 9.00 [8.00; 10.0] | 10.0 [9.00; 10.0] | <0.001 |
| Family APGAR items | |||
| Adaptability * | 0.875 | ||
| Hardly ever | 0.0 (0) | 1.0 (3) | |
| Some of the time | 12.5 (5) | 15.5 (44) | |
| Almost always | 87.5 (35) | 83.4 (236) | |
| Partnership * | 0.001 | ||
| Hardly ever | 0.0 (0) | 2.4 (7) | |
| Some of the time | 37.5 (15) | 12.7 (36) | |
| Almost always | 62.5 (25) | 84.8 (240) | |
| Growth * | <0.001 | ||
| Hardly ever | 5.0 (2) | 1.4 (4) | |
| Some of the time | 35.0 (14) | 11.0 (31) | |
| Almost always | 60.0 (24) | 87.6 (248) | |
| Affection * | 0.123 | ||
| Hardly ever | 0.0 (0) | 0.7 (2) | |
| Some of the time | 32.5 (13) | 18.7 (53) | |
| Almost always | 67.5 (27) | 80.6 (228) | |
| Resolve * | 0.449 | ||
| Hardly ever | 0.0 (0) | 0.3 (1) | |
| Some of the time | 0.0 (0) | 3.89 (11) | |
| Almost always | 100.0 (40) | 95.8 (271) | |
| Social support (score) | 48.0 [44.2; 51.0] | 48.0 [41.0; 51.0] | 0.162 |
| Social support sub-scales | |||
| Affective support (score) | 18.0 [16.0; 19.0] | 18.0 [16.0; 20.0] | 0.859 |
| Confidential support (score) | 31.0 [28.0; 33.0] | 29.0 [25.0; 33.0] | 0.031 |
| Adherence to the MedDiet of the PREDIMED-Plus Participant | ||||
|---|---|---|---|---|
| ≤7 n = 48 | 8–10 n = 137 | >10 n = 260 | p-overall | |
| Partner adherence to the MedDiet (score) ‡ | 7.21 (1.79) a | 8.55 (1.78) b | 9.56 (1.84) c | <0.001 |
| Partner physical activity (METs/min/week) | 2355 (2542) | 2522 (2873) | 2724 (2357) | 0.594 |
| Partner adherence to the MedDiet (score) | ||||
| ≤7 n = 101 | 8–10 n = 164 | >10 n = 180 | p-overall | |
| Sociodemographic characteristics | ||||
| Age (years)‡‡ | 64.3 (7.3) a | 65.4 (7.6) b | 66.6 (6.65) c | 0.035 |
| Sex * | ||||
| Women | 65.3 (66) | 64.0 (105) | 68.9 (124) | 0.618 |
| Men | 34.7 (35) | 36.0 (59) | 31.1 (56) | |
| Education level * | ||||
| University | 20.2 (19) | 13.8 (22) | 19.2 (33) | 0.202 |
| High school | 19.1 (18) | 11.9 (19) | 11.6 (20) | |
| Secondary school | 22.3 (21) | 26.9 43) | 19.8 (34) | |
| Elementary school | 38.3 (36) | 47.5 (76) | 49.4 (85) | |
| Chronic disease prevalence * | ||||
| Hypertension | 42.4 (42) | 42.4 (67) | 37.5 (66) | 0.592 |
| Dyslipidemia | 35.7 (35) | 40.4 (63) | 44.6 (79) | 0.346 |
| Type 2 diabetes mellitus | 14.1 (14) | 21.5 (34) | 11.9 (21) | 0.470 |
| Anthropometric measures | ||||
| Weight (kg) | 76.1 (14.4) | 73.5 (13.7) | 73.5 (13.5) | 0.337 |
| Height (cm) | 163 (8.60) | 163 (7.69) | 163 (7.85) | 0.997 |
| BMI (kg/m2) | 28.4 (5.0) | 27.6 (4.7) | 27.5 (3.9) | 0.337 |
| Lifestyle | ||||
| Physical activity (METs/min/week) ‡‡‡ | 1,431 [626; 2240] a | 1,785 [852; 3043] b | 2,437 [1327; 3931] c | <0.001 |
| Eating together (times per week) ‡‡‡‡ | 14.0 [10.0; 21.0] a | 14.0 [12.0; 21.0] b | 21.0 [14.0; 23.5] c | 0.001 |
| Social characteristics of the household PREDIMED-Plus cohabitants | ||||
| Family function (score) | 10.0 [9.00; 10.0] | 10.0 [9.00; 10.0] | 10.0 [9.00; 10.0] | 0.100 |
| Family APGAR items | ||||
| Adaptability * | 0.031 | |||
| Hardly ever | 4.6 (3) | 0.0 (0) | 0.0 (0) | |
| Some of the time | 15.6 (10) | 19.6 (20) | 12.0 (14) | |
| Almost always | 79.7(51) | 80.4 (82) | 88.0 (103) | |
| Partnership * | 0.172 | |||
| Hardly ever | 3.12 (2) | 2.9 (3) | 1.71 (2) | |
| Some of the time | 14.1 (9) | 6.8 (7) | 17.1 (20) | |
| Almost always | 82.8 (53) | 90.2 (92) | 81.2 (95) | |
| Growth * | 0.980 | |||
| Hardly ever | 1.5 (1) | 0.98 (1) | 1.7 (2) | |
| Some of the time | 12.5 (8) | 10.8 (11) | 10.3 (12) | |
| Almost always | 85.9 (55) | 88.2 (90) | 88.0 (103) | |
| Affection * | 0.138 | |||
| Hardly ever | 3.1 (2) | 0.0 (0) | 0.0 (0) | |
| Some of the time | 23.4 (15) | 16.7 (17) | 17.9 (21) | |
| Almost always | 73.4 (47) | 83.3 (85) | 82.1 (96) | |
| Resolve * | 0.673 | |||
| Hardly ever | 1.5 (1) | 0.0 (0) | 0.0 (0) | |
| Some of the time | 3.1 (2) | 3.9 (4) | 4.2 (5) | |
| Almost always | 95.3 (61) | 96.1 (98) | 95.7 (112) | |
| Social support (score) | 44.0 [39.0; 50.0] | 48.0 [42.0; 51.0] | 48.0 [41.0; 52.0] | 0.084 |
| Social support subscales | ||||
| Affective support (score) | 17.0 [15.0; 19.0] | 18.0 [16.0; 20.0] | 18.0 [16.0; 20.0] | 0.064 |
| Confidential support (score) | 27.0 [23.5; 32.0] | 30.0 [25.0; 33.0] | 29.0 [26.0; 33.0] | 0.138 |
| Physical Activity of the PREDIMED-Plus Participant | |||
|---|---|---|---|
| Very Active n = 289 | Active n = 150 | p-value | |
| Partner adherence to the MedDiet (score) | 9.10 (1.97) | 8.80 (1.98) | 0.137 |
| Partner physical activity (Mets/Min/Week) | 2705 (2628) | 2411 (2147) | 0.229 |
| Partner physical activity | |||
| Very Active n = 187 | Active n = 224 | p-value | |
| Sociodemographic characteristics | |||
| Age (years) | 66.6 (6.8) | 65.0 (7.2) | 0.029 |
| Sex * | |||
| Women | 58.8 (110) | 72.3 (162) | 0.006 |
| Men | 41.2 (77) | 27.7 (62) | |
| Education level * | |||
| University | 18.6 (33) | 16.6 (36) | 0.697 |
| High school | 11.3 (20) | 15.2 (33) | |
| Secondary school | 23.7 (42) | 24.0 (52) | |
| Elementary school | 46.3 (82) | 44.2 (96) | |
| Chronic disease prevalence * | |||
| Hypertension | 40.1 (73) | 38.4 (84) | 0.798 |
| Dyslipidemia | 43.9 (79) | 37.9 (83) | 0.267 |
| Type 2 diabetes mellitus | 16.9 (31) | 13.2 (29) | 0.370 |
| Anthropometric measures | |||
| Weight (kg) | 73.1 (13.0) | 74.9 (14,5) | 0.249 |
| Height (cm) | 163 (7.95) | 162 (7.86) | 0.207 |
| BMI (kg/m2) | 27.2 (3.9) | 28.2 (5.0) | 0.050 |
| Lifestyle | |||
| Adherence to the MedDiet (score) | 10.0 [8.00; 11.0] | 9.00 [7.00; 10.0] | <0.001 |
| Eating together (times per week) | 19.0 [14.0; 22.8] | 14.0 [11.0; 21.0] | 0.001 |
| Social characteristics of household PREDIMED-Plus cohabitants | |||
| Family function (score) | 10.0 [9.00; 10.0] | 10.0 [9.00; 10.0] | 0.335 |
| Family APGAR items | |||
| Adaptability * | 0.030 | ||
| Hardly ever | 0.0 (0) | 2.1 (3) | |
| Some of the time | 11.5 (15) | 19.4 (27) | |
| Almost always | 88.5 (115) | 78.4 (109) | |
| Partnership * | 1,000 | ||
| Hardly ever | 2.3 (3) | 2.1 (3) | |
| Some of the time | 13.1 (17) | 12.9 (18) | |
| Almost always | 84.6 (110) | 84.9 (118) | |
| Growth * | 0.334 | ||
| Hardly ever | 1.5 (2) | 1.4 (2) | |
| Some of the time | 12.3 (16) | 7.1 (10) | |
| Almost always | 86.2 (112) | 91.4 (127) | |
| Affection * | 0.602 | ||
| Hardly ever | 0.0 (0) | 1.4 (2) | |
| Some of the time | 19.2 (25) | 18.0 (25) | |
| Almost always | 80.8 (105) | 80.6 (112) | |
| Resolve * | 0.751 | ||
| Hardly ever | 0.0 (0) | 0.7 (1) | |
| Some of the time | 3.0 (4) | 4.3 (6) | |
| Almost always | 96.9 (126) | 95.0 (132) | |
| Social support (score) | 49.0 [42.0; 52.0] | 47.0 [40.0; 51.0] | 0.234 |
| Social support subscales | |||
| Affective support (score) | 18.0 [16.0; 20.0] | 18.0 [15.0; 19.0] | 0.101 |
| Confidential support (score) | 29.0 [26.0; 33.0] | 29.0 [25.0; 33.0] | 0.350 |
| Partner Adherence to MedDiet (Score) | β | SE | p-Value |
|---|---|---|---|
| Adherence to the MedDiet of the PREDIMED-Plus participant (score) | 4.3 × 10−1 | 7.4 × 10−1 | <0.001 |
| Physical activity of the PREDIMED-Plus participant (METs/min/week) | −3.7 × 10−5 | 5.7 × 10−5 | 0.514 |
| Age (years) | 3.9 × 10−2 | 2.3 × 10−2 | 0.077 |
| Sex (women) | 3.6 × 10−1 | 3.2 × 10−1 | 0.257 |
| Education level (university vs. high school) | −3.3 × 10−1 | 4.5 × 10−1 | 0.431 |
| Education level (university vs. secondary school) | −3.7 × 10−1 | 3.7 × 10−1 | 0.316 |
| Education level (university vs. elementary school) | −2.8 × 10−1 | 3.6 × 10−1 | 0.437 |
| Hypertension (yes) | −2.0 × 10−3 | 3.1 × 10−1 | 0.994 |
| Dyslipidemia (yes) | 6.1 × 10−1 | 2.7 × 10−1 | 0.026 |
| Type 2 diabetes mellitus (yes) | −2.0 × 10−1 | 3.7 × 10−1 | 0.594 |
| BMI (kg/m2) | −2.9 × 10−2 | 2.9 × 10−2 | 0.322 |
| Family function (score) | 2.3 × 10−1 | 1.1 × 10−1 | 0.046 |
| Social support (score) | 1.2 × 10−2 | 1.9 × 10−1 | 0.508 |
| Follow-up (years) | −2.5 × 10−1 | 3.1 × 10−1 | 0.415 |
| Partner Physical Activity (METs/Min/Week) | β | SE | p-Value |
|---|---|---|---|
| Adherence to the MedDiet of thePREDIMED-Plus participant (score) | −5.1 × 101 | 1.5 × 101 | 0.657 |
| Physical activity of the PREDIMED-Plus participant (METs/min/week) | 1.6 × 10−1 | 8.8 × 10−2 | 0.064 |
| Age (years) | 3.0 × 101 | 3.5 × 101 | 0.398 |
| Sex (women) | −8.1 × 101 | 5.0 × 102 | 0.103 |
| Education level (university vs. high school) | −1.1 × 103 | 7.4 × 102 | 0.120 |
| Education level (university vs. secondary school) | −1.1 × 103 | 5.8 × 102 | 0.070 |
| Education level (university vs. elementary school) | −1.1 × 103 | 5.6 × 102 | 0.043 |
| Hypertension (yes) | 1.5 × 102 | 5.0 × 102 | 0.764 |
| Dyslipidemia (yes) | 8.8 × 102 | 4.2 × 102 | 0.039 |
| Type 2 diabetes mellitus (yes) | −5.2 × 102 | 6.1 × 102 | 0.385 |
| BMI (kg/m2) | −8.1 × 101 | 4.6 × 101 | 0.080 |
| Family function (score) | 6.4 × 101 | 1.8 × 101 | 0.720 |
| Social support (score) | 4.1 × 101 | 2.9 × 101 | 0.169 |
| Follow-up (years) | −4.8 × 102 | 4.9 × 102 | 0.330 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Basora, J.; Villalobos, F.; Pallejà-Millán, M.; Babio, N.; Goday, A.; Castañer, O.; Fitó, M.; Zomeño, M.D.; Pintó, X.; Sacanella, E.; et al. Association between the Potential Influence of a Lifestyle Intervention in Older Individuals with Excess Weight and Metabolic Syndrome on Untreated Household Cohabitants and Their Family Support: The PREDIMED-Plus Study. Nutrients 2020, 12, 1975. https://doi.org/10.3390/nu12071975
Basora J, Villalobos F, Pallejà-Millán M, Babio N, Goday A, Castañer O, Fitó M, Zomeño MD, Pintó X, Sacanella E, et al. Association between the Potential Influence of a Lifestyle Intervention in Older Individuals with Excess Weight and Metabolic Syndrome on Untreated Household Cohabitants and Their Family Support: The PREDIMED-Plus Study. Nutrients. 2020; 12(7):1975. https://doi.org/10.3390/nu12071975
Chicago/Turabian StyleBasora, Josep, Felipe Villalobos, Meritxell Pallejà-Millán, Nancy Babio, Albert Goday, Olga Castañer, Montserrat Fitó, María Dolores Zomeño, Xavier Pintó, Emilio Sacanella, and et al. 2020. "Association between the Potential Influence of a Lifestyle Intervention in Older Individuals with Excess Weight and Metabolic Syndrome on Untreated Household Cohabitants and Their Family Support: The PREDIMED-Plus Study" Nutrients 12, no. 7: 1975. https://doi.org/10.3390/nu12071975
APA StyleBasora, J., Villalobos, F., Pallejà-Millán, M., Babio, N., Goday, A., Castañer, O., Fitó, M., Zomeño, M. D., Pintó, X., Sacanella, E., Paz-Graniel, I., & Salas-Salvadó, J. (2020). Association between the Potential Influence of a Lifestyle Intervention in Older Individuals with Excess Weight and Metabolic Syndrome on Untreated Household Cohabitants and Their Family Support: The PREDIMED-Plus Study. Nutrients, 12(7), 1975. https://doi.org/10.3390/nu12071975










