5-cis-, Trans- and Total Lycopene Plasma Concentrations Inversely Relate to Atherosclerotic Plaque Burden in Newly Diagnosed Type 2 Diabetes Subjects
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Clinical and Laboratory Determinations
2.3. Sonographic Assessment of Carotid Atherosclerotic Plaques
2.4. Dietary Intake
2.5. Clinical and Laboratory Determinations
3. Results
3.1. Participants’ Characteristics
3.2. Dietary Intake
3.3. Association between Lycopene Isomers and Lipoprotein Particles
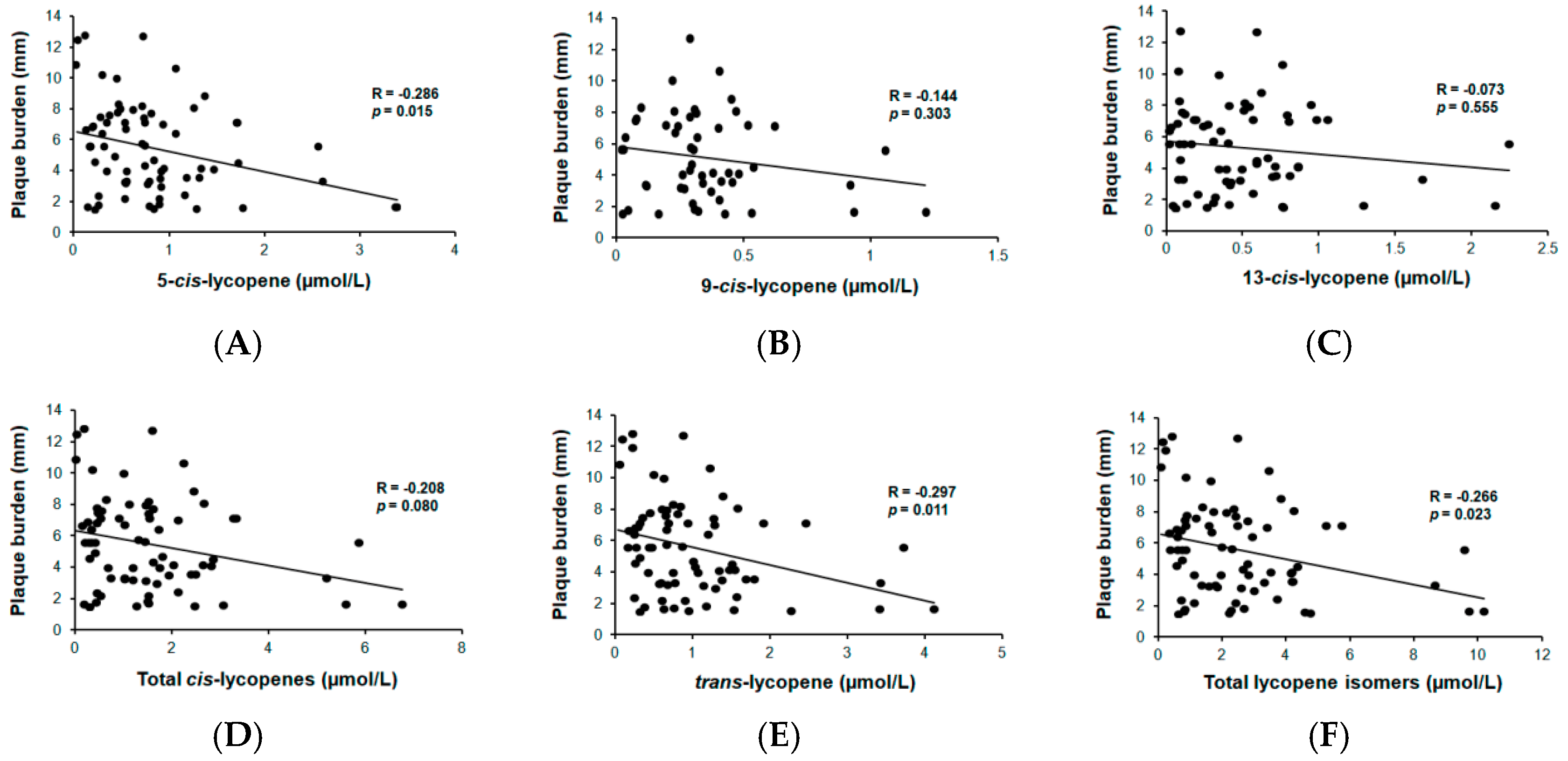
3.4. Association between Lycopene Isomers and Atherosclerotic Burden
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Williams, R.; Colagiuri, S.; Chan, J.; Gregg, E.W.; Ke, C.; Lim, L.L.; Yang, X. IDF Diabetes Atlas, 9th ed.; International Diabetes Federation: Brussels, Belgium, 2019; ISBN 978-2-930229-87-4. [Google Scholar]
- Piepoli, M.F.; Abreu, A.; Albus, C.; Ambrosetti, M.; Brotons, C.; Catapano, A.L.; Corra, U.; Cosyns, B.; Deaton, C.; Graham, I.; et al. Update on cardiovascular prevention in clinical practice: A position paper of the European Association of Preventive Cardiology of the European Society of Cardiology. Eur. J. Prev. Cardiol. 2020, 27, 181–205. [Google Scholar] [CrossRef] [PubMed]
- Kaneto, H.; Katakami, N.; Matsuhisa, M.; Matsuoka, T. Role of reactive oxygen species in the progression of type 2 diabetes and atherosclerosis. Mediat. Inflamm. 2010, 2010, 453892. [Google Scholar] [CrossRef] [PubMed]
- Jomova, K.; Valko, M. Health protective effects of carotenoids and their interactions with other biological antioxidants. Eur. J. Med. Chem. 2013, 70, 102–110. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Qiu, R.; Cao, Y.; Ouyang, W.-F.; Li, H.-B.; Ling, W.-H.; Chen, Y.-M. Higher dietary and serum carotenoid levels are associated with lower carotid intima-media thickness in middle-aged and elderly people. Br. J. Nutr. 2018, 119, 590–598. [Google Scholar] [CrossRef] [PubMed]
- McQuillan, B.M.; Hung, J.; Beilby, J.P.; Nidorf, M.; Thompson, P.L. Antioxidant vitamins and the risk of carotid atherosclerosis. The Perth Carotid Ultrasound Disease Assessment study (CUDAS). J. Am. Coll. Cardiol. 2001, 38, 1788–1794. [Google Scholar] [CrossRef]
- Zou, Z.; Xu, X.; Huang, Y.; Xiao, X.; Ma, L.; Sun, T.; Dong, P.; Wang, X.; Lin, X. High serum level of lutein may be protective against early atherosclerosis: The Beijing atherosclerosis study. Atherosclerosis 2011, 219, 789–793. [Google Scholar] [CrossRef] [PubMed]
- Dwyer, J.H.; Paul-Labrador, M.J.; Fan, J.; Shircore, A.M.; Bairey Merz, C.N.; Dwyer, K.M. Progression of Carotid Intima-Media Thickness and Plasma Antioxidants: The Los Angeles Atherosclerosis Study. Arterioscler. Thromb. Vasc. Biol. 2004, 24, 313–319. [Google Scholar] [CrossRef]
- Rissanen, T.; Voutilainen, S.; Nyyssönen, K.; Salonen, R.; Salonen, J.T. Low plasma lycopene concentration is associated with increased intima-media thickness of the carotid artery wall. Arterioscler. Thromb. Vasc. Biol. 2000, 20, 2677–2681. [Google Scholar] [CrossRef]
- Karppi, J.; Kurl, S.; Ronkainen, K.; Kauhanen, J.; Laukkanen, J.A. Serum carotenoids reduce progression of early atherosclerosis in the carotid artery wall among Eastern Finnish men. PLoS ONE 2013, 8, e64107. [Google Scholar] [CrossRef]
- Rissanen, T.H.; Voutilainen, S.; Nyyssönen, K.; Salonen, R.; Kaplan, G.A.; Salonen, J.T. Serum lycopene concentrations and carotid atherosclerosis: The Kuopio Ischaemic Heart Disease Risk Factor Study. Am. J. Clin. Nutr. 2003, 77, 133–138. [Google Scholar] [CrossRef]
- Polak, J.F.; Szklo, M.; Kronmal, R.A.; Burke, G.L.; Shea, S.; Zavodni, A.E.H.; O’Leary, D.H. The value of carotid artery plaque and intima-media thickness for incident cardiovascular disease: The multi-ethnic study of atherosclerosis. J. Am. Heart Assoc. 2013, 2, e000087. [Google Scholar] [CrossRef] [PubMed]
- Inaba, Y.; Chen, J.A.; Bergmann, S.R. Carotid plaque, compared with carotid intima-media thickness, more accurately predicts coronary artery disease events: A meta-analysis. Atherosclerosis 2012, 220, 128–133. [Google Scholar] [CrossRef] [PubMed]
- Catalan, M.; Herreras, Z.; Pinyol, M.; Sala-Vila, A.; Amor, A.J.; de Groot, E.; Gilabert, R.; Ros, E.; Ortega, E. Prevalence by sex of preclinical carotid atherosclerosis in newly diagnosed type 2 diabetes. Nutr. Metab. Cardiovasc. Dis. 2015, 25, 742–748. [Google Scholar] [CrossRef] [PubMed]
- Mallol, R.; Amigó, N.; Rodríguez, M.A.; Heras, M.; Vinaixa, M.; Plana, N.; Rock, E.; Ribalta, J.; Yanes, O.; Masana, L.; et al. Liposcale: A novel advanced lipoprotein test based on 2D diffusion-ordered 1H NMR spectroscopy. J. Lipid Res. 2015, 56, 737–746. [Google Scholar] [CrossRef]
- Arranz, S.; Martínez-Huélamo, M.; Vallverdu-Queralt, A.; Valderas-Martinez, P.; Illán, M.; Sacanella, E.; Escribano, E.; Estruch, R.; Lamuela-Raventos, R.M. Influence of olive oil on carotenoid absorption from tomato juice and effects on postprandial lipemia. Food Chem. 2015, 168, 203–210. [Google Scholar] [CrossRef]
- Vallverdú-Queralt, A.; Martínez-Huélamo, M.; Arranz-Martinez, S.; Miralles, E.; Lamuela-Raventós, R.M. Differences in the carotenoid content of ketchups and gazpachos through HPLC/ESI(Li(+) )-MS/MS correlated with their antioxidant capacity. J. Sci. Food Agric. 2012, 92, 2043–2049. [Google Scholar] [CrossRef]
- de Groot, E.; van Leuven, S.I.; Duivenvoorden, R.; Meuwese, M.C.; Akdim, F.; Bots, M.L.; Kastelein, J.J.P. Measurement of carotid intima-media thickness to assess progression and regression of atherosclerosis. Nat. Clin. Pract. Cardiovasc. Med. 2008, 5, 280–288. [Google Scholar] [CrossRef]
- Touboul, P.J.; Hennerici, M.G.; Meairs, S.; Adams, H.; Amarenco, P.; Bornstein, N.; Csiba, L.; Desvarieux, M.; Ebrahim, S.; Hernandez Hernandez, R.; et al. Mannheim carotid intima-media thickness and plaque consensus (2004-2006-2011). Cerebrovasc. Dis. 2012, 34, 290–296. [Google Scholar] [CrossRef]
- Fernández-Ballart, J.D.; Piñol, J.L.; Zazpe, I.; Corella, D.; Carrasco, P.; Toledo, E.; Perez-Bauer, M.; Martínez-González, M.Á.; Salas-Salvadó, J.; Martn-Moreno, J.M. Relative validity of a semi-quantitative food-frequency questionnaire in an elderly Mediterranean population of Spain. Br. J. Nutr. 2010, 103, 1808–1816. [Google Scholar] [CrossRef]
- Badimon, L.; Suades, R.; Crespo, J.; Padro, T.; Chiva-Blanch, G. Diet, microparticles and atherothrombosis. Front. Biosci. Landmark 2018, 23, 432–457. [Google Scholar] [CrossRef]
- Madamanchi, N.R.; Vendrov, A.; Runge, M.S. Oxidative stress and vascular disease. Arterioscler. Thromb. Vasc. Biol. 2005, 25, 29–38. [Google Scholar] [CrossRef] [PubMed]
- Engelhard, Y.N.; Gazer, B.; Paran, E. Natural antioxidants from tomato extract reduce blood pressure in patients with grade-1 hypertension: A double-blind, placebo-controlled pilot study. Am. Heart J. 2006, 151, 100. [Google Scholar] [CrossRef] [PubMed]
- Colmán-Martínez, M.; Martínez-Huélamo, M.; Valderas-Martínez, P.; Arranz-Martínez, S.; Almanza-Aguilera, E.; Corella, D.; Estruch, R.; Lamuela-Raventós, R.M. trans-Lycopene from tomato juice attenuates inflammatory biomarkers in human plasma samples: An intervention trial. Mol. Nutr. Food Res. 2017, 61. [Google Scholar] [CrossRef] [PubMed]
- Ciccone, M.M.; Cortese, F.; Gesualdo, M.; Carbonara, S.; Zito, A.; Ricci, G.; De Pascalis, F.; Scicchitano, P.; Riccioni, G. Dietary intake of carotenoids and their antioxidant and anti-inflammatory effects in cardiovascular care. Mediat. Inflamm. 2013, 2013, 782137. [Google Scholar] [CrossRef]
- Wolak, T.; Paran, E. Can carotenoids attenuate vascular aging? Vascul. Pharmacol. 2013, 59, 63–66. [Google Scholar] [CrossRef]
- Palozza, P.; Simone, R.; Catalano, A.; Parrone, N.; Monego, G.; Ranelletti, F.O. Lycopene regulation of cholesterol synthesis and efflux in human macrophages. J. Nutr. Biochem. 2011, 22, 971–978. [Google Scholar] [CrossRef]
- Müller, L.; Goupy, P.; Fröhlich, K.; Dangles, O.; Caris-Veyrat, C.; Böhm, V. Comparative study on antioxidant activity of lycopene (Z)-isomers in different assays. J. Agric. Food Chem. 2011, 59, 4504–4511. [Google Scholar] [CrossRef]
- Rinaldi de Alvarenga, J.F.; Tran, C.; Hurtado-Barroso, S.; Martinez-Huélamo, M.; Illan, M.; Lamuela-Raventos, R.M. Home cooking and ingredient synergism improve lycopene isomer production in Sofrito. Food Res. Int. 2017, 99, 851–861. [Google Scholar] [CrossRef]
- Valderas-Martinez, P.; Chiva-Blanch, G.; Casas, R.; Arranz, S.; Martínez-Huélamo, M.; Urpi-Sarda, M.; Torrado, X.; Corella, D.; Lamuela-Raventós, R.M.; Estruch, R. Tomato Sauce Enriched with Olive Oil Exerts Greater Effects on Cardiovascular Disease Risk Factors than Raw Tomato and Tomato Sauce: A Randomized Trial. Nutrients 2016, 8, 170. [Google Scholar] [CrossRef]
- Vallverdú-Queralt, A.; Regueiro, J.; de Alvarenga, J.F.R.; Torrado, X.; Lamuela-Raventos, R.M. Carotenoid profile of tomato sauces: Effect of cooking time and content of extra virgin olive oil. Int. J. Mol. Sci. 2015, 16, 9588–9599. [Google Scholar] [CrossRef]
- Hurtado-Barroso, S.; Martínez-Huélamo, M.; Rinaldi de Alvarenga, J.F.; Quifer-Rada, P.; Vallverdú-Queralt, A.; Pérez-Fernández, S.; Lamuela-Raventós, R.M. Acute Effect of a Single Dose of Tomato Sofrito on Plasmatic Inflammatory Biomarkers in Healthy Men. Nutrients 2019, 11, 851. [Google Scholar] [CrossRef] [PubMed]
- Ghavipour, M.; Saedisomeolia, A.; Djalali, M.; Sotoudeh, G.; Eshraghyan, M.R.; Moghadam, A.M.; Wood, L.G. Tomato juice consumption reduces systemic inflammation in overweight and obese females. Br. J. Nutr. 2013, 109, 2031–2035. [Google Scholar] [CrossRef] [PubMed]
- Cuevas-Ramos, D.; Almeda-Valdés, P.; Chávez-Manzanera, E.; Meza-Arana, C.E.; Brito-Córdova, G.; Mehta, R.; Pérez-Méndez, O.; Gómez-Pérez, F.J. Effect of tomato consumption on high-density lipoprotein cholesterol level: A randomized, single-blinded, controlled clinical trial. Diabetes Metab. Syndr. Obes. 2013, 6, 263–273. [Google Scholar] [CrossRef] [PubMed]
- Upritchard, J.E.; Sutherland, W.H.; Mann, J.I. Effect of supplementation with tomato juice, vitamin E, and vitamin C on LDL oxidation and products of inflammatory activity in type 2 diabetes. Diabetes Care 2000, 23, 733–738. [Google Scholar] [CrossRef] [PubMed]
- Shidfar, F.; Froghifar, N.; Vafa, M.; Rajab, A.; Hosseini, S.; Shidfar, S.; Gohari, M. The effects of tomato consumption on serum glucose, apolipoprotein B, apolipoprotein A-I, homocysteine and blood pressure in type 2 diabetic patients. Int. J. Food Sci. Nutr. 2011, 62, 289–294. [Google Scholar] [CrossRef] [PubMed]
- Silbernagel, G.; Pagel, P.; Pfahlert, V.; Genser, B.; Scharnagl, H.; Kleber, M.E.; Delgado, G.; Ohrui, H.; Ritsch, A.; Grammer, T.B.; et al. High-density lipoprotein subclasses, coronary artery disease, and cardiovascular mortality. Clin. Chem. 2017, 63, 1886–1896. [Google Scholar] [CrossRef] [PubMed]
- Cheng, H.M.; Koutsidis, G.; Lodge, J.K.; Ashor, A.; Siervo, M.; Lara, J. Tomato and lycopene supplementation and cardiovascular risk factors: A systematic review and meta-analysis. Atherosclerosis 2017, 257, 100–108. [Google Scholar] [CrossRef]
- Costa-Rodrigues, J.; Pinho, O.; Monteiro, P.R.R. Can lycopene be considered an effective protection against cardiovascular disease? Food Chem. 2018, 245, 1148–1153. [Google Scholar] [CrossRef]
- Karppi, J.; Laukkanen, J.A.; Sivenius, J.; Ronkainen, K.; Kurl, S. Serum lycopene decreases the risk of stroke in men; A population-based follow-up study. Neurology 2012, 79, 1540–1547. [Google Scholar] [CrossRef]
| Variable | Subjects without Atherosclerosis (n = 30) | Atherosclerotic Subjects (n = 75) | p | Reference Interval 1 |
|---|---|---|---|---|
| Females, n (%) | 15 (50) | 33 (44) | 0.577 | - |
| Age, years | 58.7 ± 8.38 | 61.23 ± 6.83 | 0.112 | - |
| BMI (kg/m2) | 31.52 ± 5.49 | 30.75 ± 4.98 | 0.489 | 20–24.9 |
| Waist (cm) | 105.02 ± 11.47 | 104.16 ± 13.34 | 0.765 | <100 (women) <110 (men) |
| Systolic blood pressure (mmHg) | 129.13 ± 17.38 | 132.57 ± 16.46 | 0.343 | <140 |
| Diastolic blood pressure (mmHg) | 83.17 ± 10.74 | 81.93 ± 9.73 | 0.570 | <90 |
| Glucose (mg/dL) | 139.17 ± 16.41 | 140.18 ± 40.59 | 0.857 | 65–110 |
| Insulin (UI/L) | 20.67 ± 16.67 | 18.84 ± 12.15 | 0.538 | 2–15 |
| HOMA-IR | 7.26 ± 6.33 | 6.56 ± 4.45 | 0.529 | <2.15 |
| HbA1C (%) | 6.92 ± 1.43 | 7.41 ± 1.87 | 0.156 | 3.4–5.5 |
| hsCRP (mg/L) | 0.59 ± 0.69 | 0.51 ± 0.53 | 0.488 | <1.07 |
| Triglycerides (mg/dL) | 144.9 ± 94.66 | 151.38 ± 84.29 | 0.733 | 50–150 |
| Total cholesterol (mg/dL) | 198.83 ± 32.47 | 200.5 ± 44.48 | 0.833 | 148–200 |
| HDL (mg/dL) | 50.32 ± 14.84 | 49.09 ± 13.89 | 0.701 | >50 (women) >40 (men) |
| LDL (mg/dL) | 165.98 ± 50.71 | 174.54 ± 56.03 | 0.486 | <130 |
| ApoA1(mg/dL) | 141.46 ± 25.02 | 138.01 ± 21.16 | 0.488 | 102–215 |
| ApoB (mg/dL) | 95.96 ± 23.94 | 104.74 ± 27.85 | 0.145 | 59–155 |
| nonHDL (mg/dL) | 146.83 ± 30.52 | 151.18 ± 41.87 | 0.559 | <100 |
| Hypertension, n (%) | 15 (30) | 41 (55) | 0.665 | |
| Dyslipidemia, n (%) | 11 (37) | 32 (43) | 0.572 | |
| Smokers, n (%) | 4 (13) | 16 (21) | 0.346 | |
| History of premature CVD, n (%) | 2 (7) | 8 (11) | 0.254 | |
| Medication, n (%) | ||||
| GLP-1 agonists | 11 (37) | 41 (55) | 0.096 | |
| Pioglitazone | 11 (37) | 41 (55) | 0.096 | |
| Statin score 2 | 16.02 ± 34.9 | 23.36 ± 46.08 | 0.433 |
| Food Item | 5-cis-Lycopene | 9-cis-Lycopene | 13-cis-Lycopene | trans-Lycopene | Sum of Lycopenes |
|---|---|---|---|---|---|
| Raw tomato, g/day | |||||
| Rho Spearman 1 | 0.189 | 0.190 | 0.154 | 0.184 | 0.209 |
| p1 | 0.073 | 0.072 | 0.145 | 0.082 | 0.046 |
| Gazpacho, g/day | |||||
| Rho Spearman 1 | 0.179 | 0.166 | 0.139 | 0.185 | 0.194 |
| p1 | 0.089 | 0.115 | 0.187 | 0.080 | 0.065 |
| Ketchup/fried tomato sauce, g/day | |||||
| Rho Spearman 1 | 0.227 | 0.210 | 0.188 | 0.215 | 0.206 |
| p1 | 0.032 | 0.049 | 0.078 | 0.041 | 0.053 |
| Total tomato-based foods, g/day | |||||
| Rho Spearman 1 | 0.237 | 0.211 | 0.180 | 0.227 | 0.244 |
| p1 | 0.025 | 0.047 | 0.091 | 0.031 | 0.021 |
| Lycopene Measurement | B (95% CI) | p |
|---|---|---|
| 5-cis-lycopene | −0.99 (−2.01, −0.02) | 0.045 |
| 9-cis-lycopene | −1.26 (−4.56, 2.04) | 0.445 |
| 13-cis-lycopene | −0.54 (−2.09, 1.01) | 0.487 |
| all cis-lycopene | −0.40 (−0.91, 0.11) | 0.122 |
| trans-lycopene | −0.86 (−1.71, −0.01) | 0.047 |
| Total lycopene isomers | −0.31 (−0.64, −0.01) | 0.050 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chiva-Blanch, G.; Jiménez, C.; Pinyol, M.; Herreras, Z.; Catalán, M.; Martínez-Huélamo, M.; Lamuela-Raventos, R.M.; Sala-Vila, A.; Cofán, M.; Gilabert, R.; et al. 5-cis-, Trans- and Total Lycopene Plasma Concentrations Inversely Relate to Atherosclerotic Plaque Burden in Newly Diagnosed Type 2 Diabetes Subjects. Nutrients 2020, 12, 1696. https://doi.org/10.3390/nu12061696
Chiva-Blanch G, Jiménez C, Pinyol M, Herreras Z, Catalán M, Martínez-Huélamo M, Lamuela-Raventos RM, Sala-Vila A, Cofán M, Gilabert R, et al. 5-cis-, Trans- and Total Lycopene Plasma Concentrations Inversely Relate to Atherosclerotic Plaque Burden in Newly Diagnosed Type 2 Diabetes Subjects. Nutrients. 2020; 12(6):1696. https://doi.org/10.3390/nu12061696
Chicago/Turabian StyleChiva-Blanch, Gemma, Claudia Jiménez, Montserrat Pinyol, Zoe Herreras, Marta Catalán, Miriam Martínez-Huélamo, Rosa M Lamuela-Raventos, Aleix Sala-Vila, Montserrat Cofán, Rosa Gilabert, and et al. 2020. "5-cis-, Trans- and Total Lycopene Plasma Concentrations Inversely Relate to Atherosclerotic Plaque Burden in Newly Diagnosed Type 2 Diabetes Subjects" Nutrients 12, no. 6: 1696. https://doi.org/10.3390/nu12061696
APA StyleChiva-Blanch, G., Jiménez, C., Pinyol, M., Herreras, Z., Catalán, M., Martínez-Huélamo, M., Lamuela-Raventos, R. M., Sala-Vila, A., Cofán, M., Gilabert, R., Jiménez, A., & Ortega, E. (2020). 5-cis-, Trans- and Total Lycopene Plasma Concentrations Inversely Relate to Atherosclerotic Plaque Burden in Newly Diagnosed Type 2 Diabetes Subjects. Nutrients, 12(6), 1696. https://doi.org/10.3390/nu12061696






