Does Eating Addiction Favor a More Varied Diet or Contribute to Obesity?—The Case of Polish Adults
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Sample Collection
2.2. Food Intake Variety
- Inadequate FIV (<20 food products weekly)
- Sufficient FIV (20–29 food products weekly)
- Good FIV (30–39 food products weekly)
- Very good FIV (≥40 food products weekly)
2.3. Eating Addiction
2.4. Physical Activity and Other Lifestyle Factors
2.5. Sociodemographic Characteristics
2.6. Statistical Analysis
3. Results
3.1. Characteristics of the Study Sample
3.2. Food Intake Variety and Other Lifestyle Factors
3.3. Eating Addiction
3.4. Relationship between Food Intake Variety and Eating Addiction
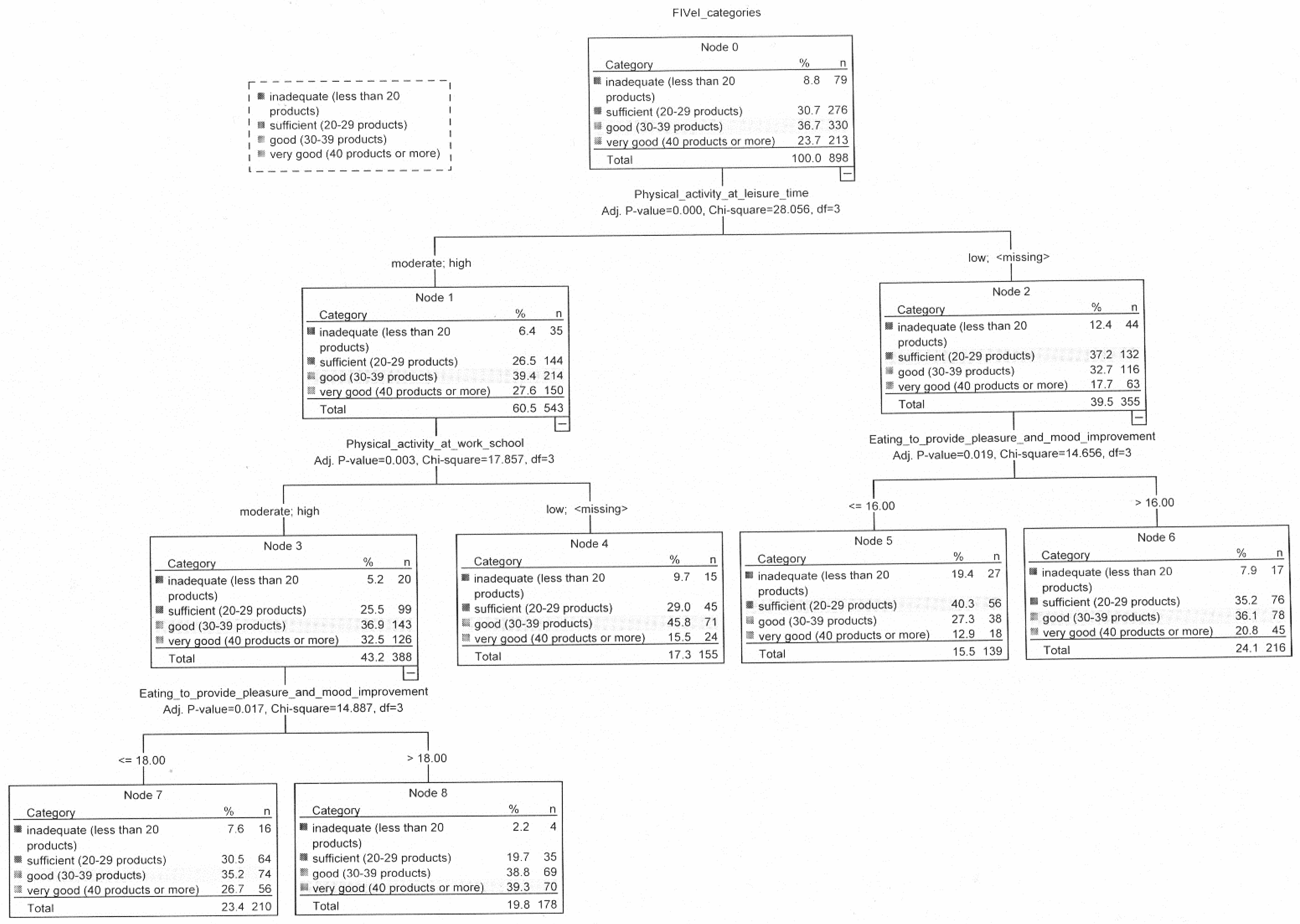
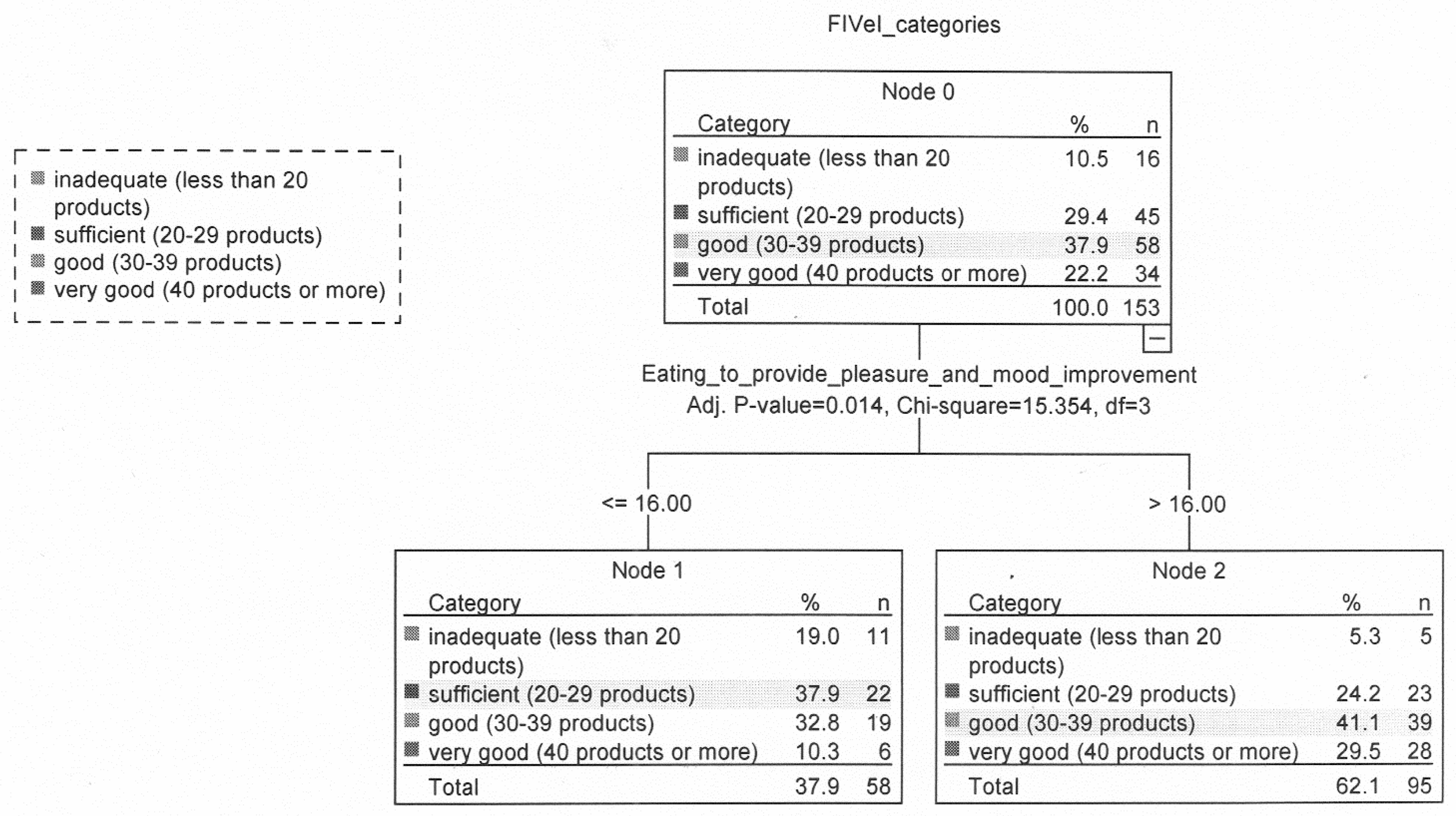
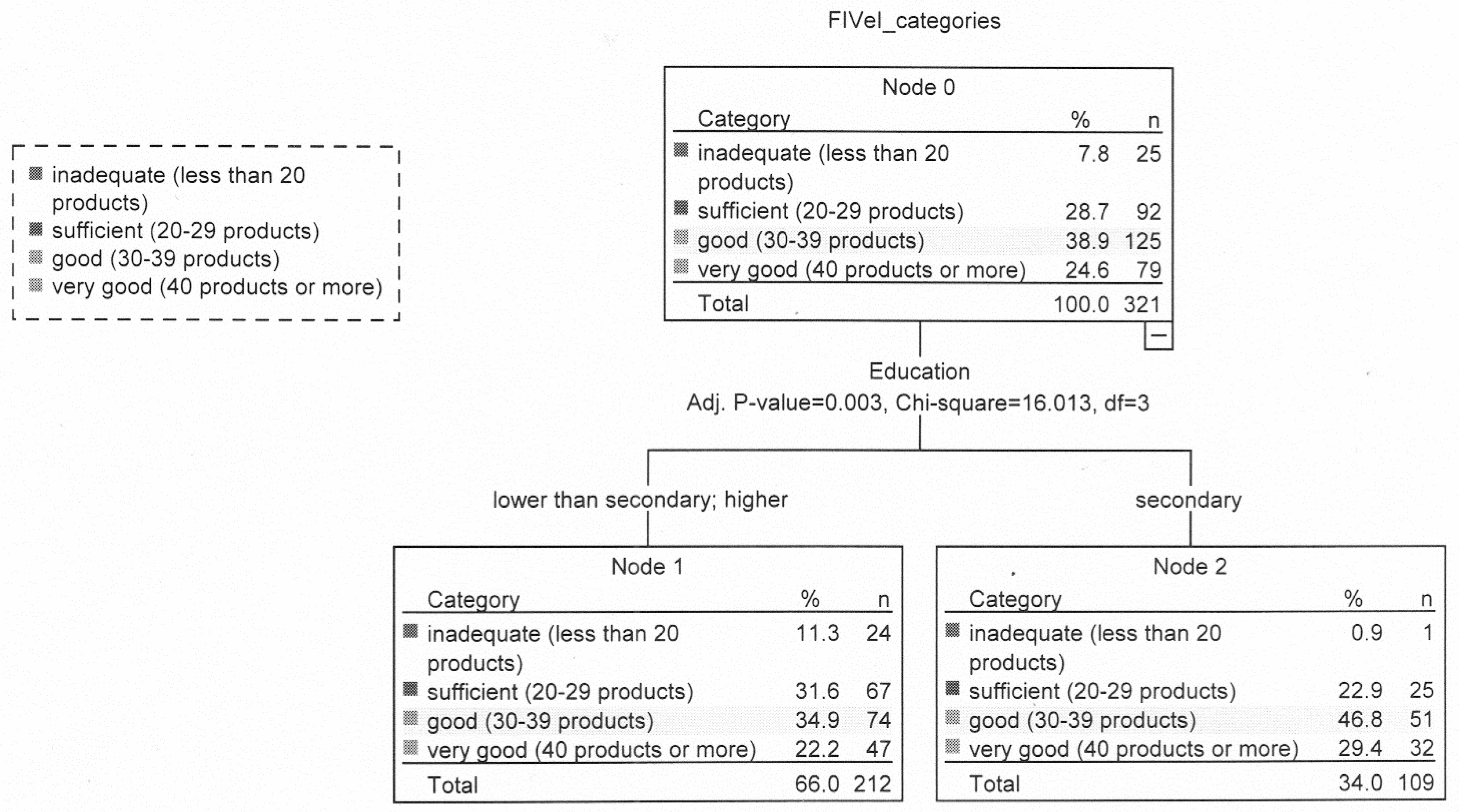
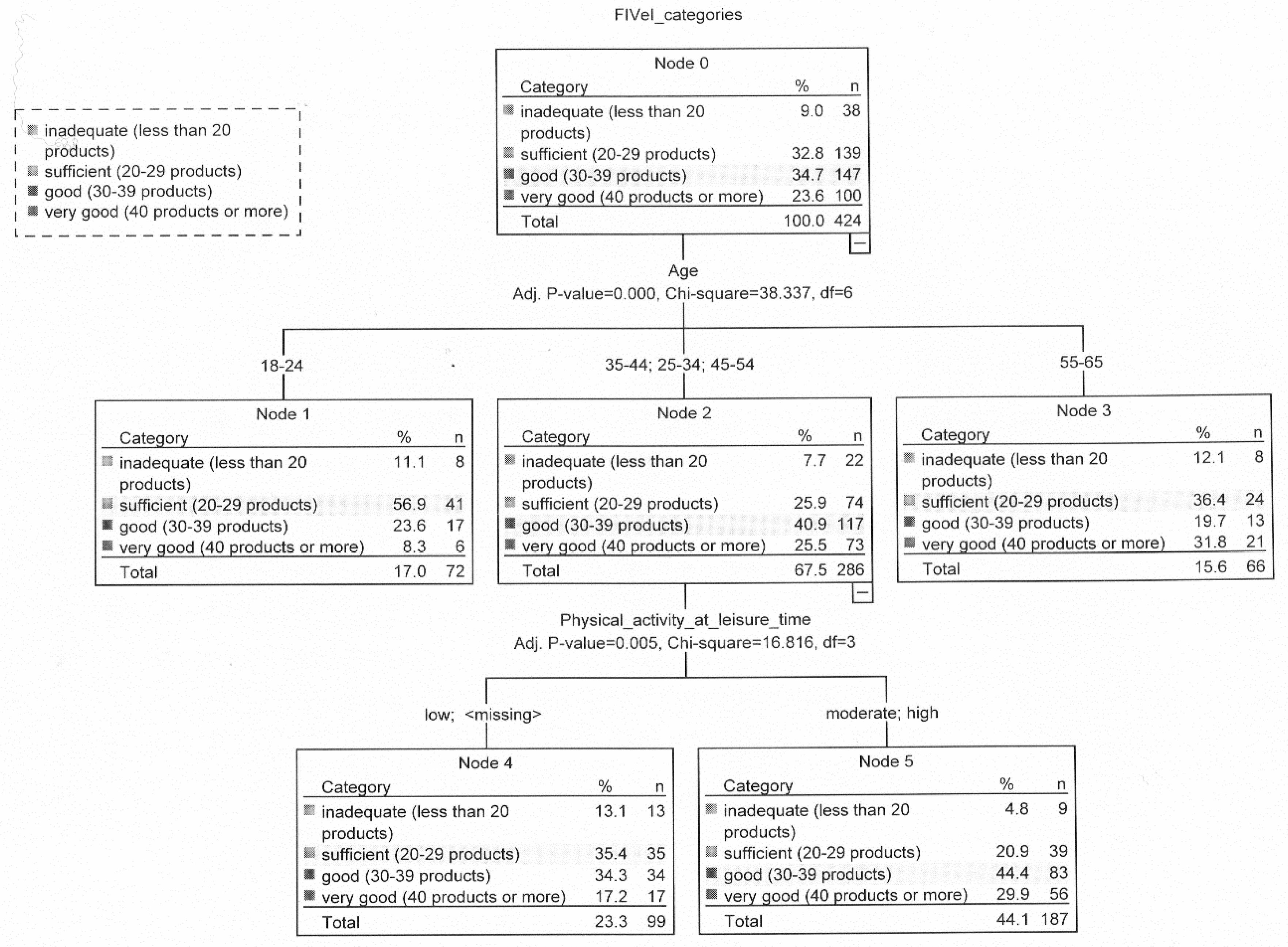
3.5. Relationship between Food Intake Variety and Lifestyle and Sociodemographic Variables
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Elmadfa, I.; Meyer, A. Developing Suitable Methods of Nutritional Status Assessment: A Continuous Challenge. Adv. Nutr. 2014, 5, 5905–5985. [Google Scholar] [CrossRef] [PubMed]
- Schulze, M.; Martínez-González, M.; Fung, T.; Lichtenstein, A.; Forouhi, N. Food based dietary patterns and chronic disease prevention. BMJ 2018, 361, k2396. [Google Scholar] [CrossRef] [PubMed]
- Blair, S.N.; Hand, G.A.; Hill, J.O. Energy balance: A crucial issue for exercise and sports medicine. Br. J. Sports Med. 2015, 49, 970–971. [Google Scholar] [CrossRef] [PubMed]
- Hobbs, M.; Pearson, N.; Foster, P.J.; Biddle, S.J. Sedentary behaviour and diet across the lifespan: An updated systematic review. Br. J. Sports Med. 2014, 49, 1179–1188. [Google Scholar] [CrossRef]
- Compernolle, S.; De Cocker, K.; Teixeira, P.J.; Oppert, J.-M.; Roda, C.; Mackenbach, J.D.; Lakerveld, J.; McKee, M.; Glonti, K.; Rutter, H.; et al. The associations between domain-specific sedentary behaviours and dietary habits in European adults: A cross-sectional analysis of the SPOTLIGHT survey. BMC Public Health 2016, 16, 1057. [Google Scholar] [CrossRef]
- Schultchen, D.; Reichenberger, J.; Mittl, T.; Weh, T.R.M.; Smyth, J.M.; Blechert, J.; Pollatos, O. Bidirectional relationship of stress and affect with physical activity and healthy eating. Br. J. Health Psychol. 2019, 24, 315–333. [Google Scholar] [CrossRef]
- Devonport, T.J.; Nicholls, W.; Fullerton, C. A systematic review of the association between emotions and eating behaviour in normal and overweight adult populations. J. Health Psychol. 2019, 24, 3–24. [Google Scholar] [CrossRef]
- Dohle, S.; Hartmann, C.; Keller, C. Physical activity as a moderator of the association between emotional eating and BMI: Evidence from the Swiss Food Panel. Psychol. Health 2014, 29, 1062–1080. [Google Scholar] [CrossRef]
- Gearhardt, A.N.; Corbin, W.R.; Brownell, K.D. Food addiction: An examination of the diagnostic criteria for dependence. J. Addict. Med. 2009, 3, 1–7. [Google Scholar] [CrossRef]
- Gearhardt, A.N.; Corbin, W.R.; Brownell, K.D. Preliminary validation of the Yale Food Addiction Scale. Appetite 2009, 52, 430–436. [Google Scholar] [CrossRef]
- Gearhardt, A.N.; Corbin, W.R.; Brownell, K.D. Development of the Yale Food Addiction Scale Version 2.0. Psychol Addict. Behav. 2016, 30, 113–121. [Google Scholar] [CrossRef] [PubMed]
- Ayaz, A.; Nergiz-Unal, R.; Dedebayraktar, D.; AkyoL, A.; Pekcan, A.G.; Besler, H.T.; Buyuktuncer, Z. How does food addiction influence dietary intake profile? PLoS ONE 2018, 13, e0195541. [Google Scholar] [CrossRef] [PubMed]
- Pursey, K.; Collins, C.; Stanwell, P.; Burrows, T. Foods and dietary profiles associated with ‘food addiction’ in young adults. Addict. Behav. Rep. 2015, 2, 41–48. [Google Scholar] [CrossRef] [PubMed]
- Pedram, P.; Sun, G. Hormonal and dietary characteristics in obese human subjects with and without food addiction. Nutrients 2014, 7, 223–238. [Google Scholar] [CrossRef]
- Burrows, T.; Hides, L.; Brown, R.; Dayas, C.V.; Kay-Lambkin, F. Differences in Dietary Preferences, Personality and Mental Health in Australian Adults with and without Food Addiction. Nutrients 2017, 9, 285. [Google Scholar] [CrossRef]
- Küçükerdönmez, Ö.; Urhan, M.; Altın, M.; Hacıraifoğlu, Ö.; Yıldız, B. Assessment of the relationship between food addiction and nutritional status in schizophrenic patients. Nutr. Neurosci. 2019, 22, 392–400. [Google Scholar] [CrossRef]
- Linardon, J. The relationship between dietary restraint and binge eating: Examining eating-related self-efficacy as a moderator. Appetite 2018, 127, 126–129. [Google Scholar] [CrossRef]
- Denny, K.N.; Loth, K.; Eisenberg, M.E.; Neumark-Sztainer, D. Intuitive eating in young adults. Who is doing it, and how is it related to disordered eating behaviors? Appetite 2013, 60, 13–19. [Google Scholar] [CrossRef]
- Paans, N.; Gibson-Smith, D.; Bot, M.; van Strien, T.; Brouwer, I.; Visser, M.; Penninx, B. Depression and eating styles are independently associated with dietary intake. Appetite 2019, 134, 103–110. [Google Scholar] [CrossRef]
- Camilleri, G.; Méjean, C.; Kesse-Guyot, E.; Andreeva, V.; Bellisle, F.; Hercberg, S.; Péneau, S. The Associations between Emotional Eating and Consumption of Energy-Dense Snack Foods Are Modified by Sex and Depressive Symptomatology. J. Nutr. 2014, 144, 1264–1273. [Google Scholar] [CrossRef]
- Konttinen, H.; Männistö, S.; Sarlio-Lähteenkorva, S.; Silventoinen, K.; Haukkala, A. Emotional eating, depressive symptoms and self-reported food consumption. A population-based study. Appetite 2010, 54, 473–479. [Google Scholar] [CrossRef] [PubMed]
- van Strien, T.; Cebolla, A.; Etchemendy, E.; Gutiérrez-Maldonado, J.; Ferrer-García, M.; Botella, C.; Baños, R. Emotional eating and food intake after sadness and joy. Appetite 2013, 66, 20–25. [Google Scholar] [CrossRef] [PubMed]
- Cleobury, L.; Tapper, K. Reasons for eating ‘unhealthy’ snacks in overweight and obese males and females. J. Hum. Nutr. Diet. 2013, 27, 333–341. [Google Scholar] [CrossRef] [PubMed]
- Lluch, A.; Herbeth, B.; Méjean, L.; Siest, G. Dietary intakes, eating style and overweight in the Stanislas Family Study. Int. J. Obes. 2000, 24, 1493–1499. [Google Scholar] [CrossRef] [PubMed]
- Klesges, R.C.; Isbell, T.R.; Klesges, L.M. Relationship between dietary restraint, energy intake, physical activity, and body weight: A prospective analysis. J. Abnorm. Psychol. 1992, 101, 668–674. [Google Scholar] [CrossRef]
- van Strien, T.; Konttinen, H.; Ouwens, M.; van de Laar, F.; Winkens, L. Mediation of emotional and external eating between dieting and food intake or BMI gain in women. Appetite 2020, 145, 104493. [Google Scholar] [CrossRef]
- Houben, K.; Jansen, A. When food becomes an obsession: Overweight is related to food-related obsessive-compulsive behavior. J. Health Psychol. 2019, 24, 1145–1152. [Google Scholar] [CrossRef]
- Vadiveloo, M.; Dixon, L.B.; Parekh, N. Associations between dietary variety and measures of body adiposity: A systematic review of epidemiological studies. Br. J. Nutr. 2013, 109, 1557–1572. [Google Scholar] [CrossRef]
- Hruby, A.; Hu, F.B. The Epidemiology of Obesity: A Big Picture. Pharmacoeconomics 2015, 33, 673–689. [Google Scholar] [CrossRef]
- Bezerra, I.N.; Sichieri, R. Household food diversity and nutritional status among adults in Brazil. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 22. [Google Scholar] [CrossRef]
- Zhang, Q.; Chen, X.; Liu, Z.; Varma, D.S.; Wan, R.; Zhao, S. Diet diversity and nutritional status among adults in southwest China. PLoS ONE 2017, 12, e0172406. [Google Scholar] [CrossRef] [PubMed]
- Keim, N.L.; Forester, S.M.; Lyly, M.; Aaron, G.J.; Townsend, M.S. Vegetable variety is a key to improved diet quality in low-income women in California. J. Acad. Nutr. Diet. 2014, 114, 430–435. [Google Scholar] [CrossRef] [PubMed]
- Azadbakht, L.; Esmaillzadeh, A. Dietary diversity score is related to obesity and abdominal adiposity among Iranian female youth. Public Health Nutr. 2011, 14, 62–69. [Google Scholar] [CrossRef] [PubMed]
- Murphy, S.P.; Foote, J.A.; Wilkens, L.R.; Basiotis, P.P.; Carlson, A.; White, K.K.; Yonemori, K.M. Simple measures of dietary variety are associated with improved dietary quality. J. Am. Diet. Assoc. 2006, 106, 425–429. [Google Scholar] [CrossRef]
- Bernstein, M.A.; Tucker, K.L.; Ryan, N.D.; O’Neill, E.F.; Clements, K.M.; Nelson, M.E.; Evans, W.J.; Fiatarone Singh, M.A. Higher dietary variety is associated with better nutritional status in frail elderly people. J. Am. Diet. Assoc. 2002, 102, 1096–1104. [Google Scholar] [CrossRef]
- Niedzwiedzka, E.; Wadolowska, L. Accuracy Analysis of the Food Intake Variety Questionnaire (FIVeQ). Reproducibility Assessment among Older People. Pakistan J. Nutr. 2008, 7, 426–435. [Google Scholar] [CrossRef][Green Version]
- Ogińska-Bulik, N. Osobowość Typu D: Teoria i Badania; Type D Personality; Theory and Research; Wyd.WSHE: Łódź, Poland, 2009. [Google Scholar]
- Beliefs and Eating Habits Questionnaire. Behavioral Conditions of Nutrition Team, Committee of Human Nutrition Science. Polish Academy of Science. Warsaw 2014. Available online: http://www.knozc.pan.pl/ (accessed on 15 October 2018).
- Cole, T.J.; Lobstein, T. Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatr. Obes. 2012, 7, 284–294. [Google Scholar] [CrossRef]
- James, G.; Witten, D.; Hastie, T.; Tibshirani, R. An Introduction to Statistical Learning; Springer: New York, NY, USA, 2015; ISBN 978-1-4614-7137-0. [Google Scholar]
- Gilhooly, C.H.; Das, S.K.; Golden, J.K.; McCrory, M.A.; Dallal, G.E.; Saltzman, E.; Kramer, F.M.; Robert, S.B. Food cravings and energy regulation: The characteristics of craved foods and their relationship with eating behaviors and weight change during 6 months of dietary energy restriction. Int. J. Obes. 2007, 31, 1849–1858. [Google Scholar] [CrossRef]
- Hebebrand, J.; Albayrak, Ö.; Adan, R.; Antel, J.; Dieguez, C.; de Jong, J.; Leng, G.; Menzies, J.; Mercer, J.G.; Murphy, M.; et al. “Eating addiction”, rather than “food addiction”, better captures addictive-like eating behavior. Neurosci. Biobehav. Rev. 2014, 47, 295–306. [Google Scholar] [CrossRef]
- Curtis, C.; Davis, C. A qualitative study of binge eating and obesity from an addiction perspective. Eat. Disord. 2014, 22, 19–32. [Google Scholar] [CrossRef]
- Schulte, E.M.; Avena, N.M.; Gearhardt, A.N. Which foods may Be Addictive? The roles of processing, fat content, and glycemic load. PLoS ONE 2015, 10, e0117959. [Google Scholar] [CrossRef] [PubMed]
- Vanderlinden, J.; Dalle Grave, R.; Vandereycken, W.; Noorduin, C. Which factors do provoke binge-eating? An exploratory study in female students. Eat. Behav. 2001, 2, 79–83. [Google Scholar] [CrossRef]
- Ifland, J.R.; Preuss, H.G.; Marcus, M.T.; Rourke, K.M.; Taylor, W.; Theresa Wright, H. Clearing the confusion around processed food addiction. J. Am. Coll. Nutr. 2015, 34, 240–243. [Google Scholar] [CrossRef] [PubMed]
- White, M.A.; Grilo, C.M. Psychometric properties of the Food Craving Inventory among obese patients with binge eating disorder. Eat. Behav. 2005, 6, 239–245. [Google Scholar] [CrossRef]
- Epel, E.; Lapidus, R.; McEwen, B.; Brownell, K. Stress may add bite to appetite in women: A laboratory study of stress-induced cortisol and eating behavior. Psychoneuroendocrinology 2001, 26, 37–49. [Google Scholar] [CrossRef]
- Zellner, D.A.; Loaiza, S.; Gonzalez, Z.; Pita, J.; Morales, J.; Pecora, D.; Wolf, A. Food selection changes under stress. Physiol. Behav. 2006, 87, 789–793. [Google Scholar] [CrossRef]
- Loprinzi, P.; Smit, E.; Mahoney, S. Physical Activity and Dietary Behavior in US Adults and Their Combined Influence on Health. Mayo Clin. Proc. 2014, 89, 190–198. [Google Scholar] [CrossRef]
- Wadolowska, L.; Kowalkowska, J.; Lonnie, M.; Czarnocinska, J.; Jezewska-Zychowicz, M.; Babicz-Zielinska, E. Associations between physical activity patterns and dietary patterns in a representative sample of Polish girls aged 13–21 years: A cross-sectional study (GEBaHealth Project). BMC Public Health 2016, 16, 698. [Google Scholar] [CrossRef]
- Wammes, B.; French, S.; Brug, J. What young Dutch adults say they do to keep from gaining weight: Self-reported prevalence of overeating, compensatory behaviours and specific weight control behaviours. Public Health Nutr. 2007, 10, 790–798. [Google Scholar] [CrossRef]
- Lee, I.; Djoussé, L.; Sesso, H.D.; Wang, L.; Buring, J.E. Physical activity and weight gain prevention. JAMA 2010, 303, 1173–1179. [Google Scholar] [CrossRef]
- Charreire, H.; Kesse-Guyot, E.; Bertrai, S.; Simon, C.; Chaix, B.; Weber, C.; Touvier, M.; Galan, P.; Hercberg, S.; Oppert, J.-M. Associations between dietary patterns, physical activity (leisure-time and occupational) and television viewing in middle-aged French adults. Br. J. Nutr. 2011, 105, 902–910. [Google Scholar] [CrossRef] [PubMed]
- Kesse-Guyot, E.; Bertrais, S.; Peneau, S.; Estaquio, C.; Dauchet, L.; Vergnaud, A.-C.; Czernichow, S.; Galan, P.; Hercberg, S.; Bellisle, F. Dietary patterns and their sociodemographic and behavioural correlates in French middle-aged adults from the SU.VI.MAX cohort. Eur. J. Clin. Nutr. 2009, 63, 521–528. [Google Scholar] [CrossRef] [PubMed]
- Li, J.T.E.; Pursey, K.M.; Duncan, M.J.; Burrows, T. Addictive Eating and Its Relation to Physical Activity and Sleep Behavior. Nutrients 2018, 10, 1428. [Google Scholar] [CrossRef]
- Luo, S.; O’Connor, S.G.; Belcher, B.R.; Page, K.A. Effects of Physical Activity and Sedentary Behavior on Brain Response to High-Calorie Food Cues in Young Adults. Obesity 2018, 26, 540–546. [Google Scholar] [CrossRef] [PubMed]
- Shook, R.; Hand, G.; Drenowatz, C.; Hebert, J.R.; Paluch, A.E.; Blundell, J.E.; Hill, J.O.; Katzmarzyk, P.T.; Church, T.S.; Blair, S.N. Low levels of physical activity are associated with dysregulation of energy intake and fat mass gain over 1 year. Am. J. Clin. Nutr. 2015, 102, 1332–1338. [Google Scholar] [CrossRef] [PubMed]
- Yannakoulia, M.; Mamalaki, E.; Anastasiou, C.; Mourtzi, N.; Lambrinoudaki, I.; Scarmeas, N. Eating habits and behaviors of older people: Where are we now and where should we go? Maturitas 2018, 114, 14–21. [Google Scholar] [CrossRef]
- Tsujim, T.; Yamamoto, K.; Yamasaki, K.; Hayashi, F.; Momoki, C.; Yasui, Y.; Ohfuji, S.; Fukushima, W.; Habu, D. Lower dietary variety is a relevant factor for malnutrition in older Japanese home-care recipients: A cross-sectional study. BMC Geriatr. 2019, 19, 197. [Google Scholar] [CrossRef]
- Drewnowski, A.; Henderson, S.A.; Driscoll, A.; Rolls, B.J. The Dietary Variety Score: Assessing diet quality in healthy young and older adults. J. Am. Diet. Assoc. 1997, 97, 266–271. [Google Scholar] [CrossRef]
- Morozink Boylan, J.; Cundiff, J.M.; Jakubowski, K.P.; Pardini, D.A.; Matthews, K.A. Pathways Linking Childhood SES and Adult Health Behaviors and Psychological Resources in Black and White Men. Ann. Behav. Med. 2018, 52, 1023–1035. [Google Scholar] [CrossRef]
- Adler, N.E.; Stewart, J. Health disparities across the lifespan: Meaning, methods, and mechanisms. Ann. NY Acad. Sci. 2010, 1186, 5–23. [Google Scholar] [CrossRef]
- Pechey, R.; Monsivais, P. Socioeconomic inequalities in the healthiness of food choices: Exploring the contributions of food expenditures. Prev. Med. 2016, 88, 203–209. [Google Scholar] [CrossRef] [PubMed]
- Worsley, A.; Blaschea, R.; Ball, K.; Crawford, D. The relationship between education and food consumption in the 1995 Australian National Nutrition Survey. Public Health Nutr. 2004, 7, 649–663. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Eertmans, A.; Baeyens, F.; Van den Bergh, O. Food likes and their relative importance in human eating behavior. Review and preliminary suggestions for health promotion. Health Educ. Res. 2001, 16, 443–456. [Google Scholar] [CrossRef] [PubMed]
- Lumbers, M.; Raats, M. Food choices in later life. In The Psychology of Food Choice; Frontiers in Nutritional Sciences; Shepherd, R., Raats, M., Eds.; CABI Publishing: Wallingford, UK, 2006; Volume 3, pp. 280–310. [Google Scholar]
- Conklin, A.; Forouhi, N.; Suhrcke, M.; Surtees, P.; Wareham, N.; Monsivais, P. Variety More Than Quantity of Fruit And Vegetable Intake Varies By Socioeconomic Status And Financial Hardship. Findings From Older Adults In The EPIC Cohort. Appetite 2014, 83, 248–255. [Google Scholar] [CrossRef]
- Glass, C.; Haas, S.; Reither, E. The Skinny On Success: Body Mass, Gender And Occupational Standing Across The Life Course. Social Forces 2010, 88, 1777–1806. [Google Scholar] [CrossRef]
- Duncan, D.; Wolin, K.; Scharoun-Lee, M.; Ding, E.; Warner, E.; Bennett, G. Does Perception Equal Reality? Weight Misperception in Relation to Weight-Related Attitudes and Behaviors among Overweight and Obese US Adults. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 20. [Google Scholar] [CrossRef]
- Millstein, R.A.; Carlson, S.A.; Fulton, J.E.; Galuska, D.A.; Zhang, J.; Blanck, H.M.; Ainsworth, B.E. Relationships between body size satisfaction and weight control practices among US adults. Medscape J. Med. 2008, 10, 119. [Google Scholar]
- Burton, N.W.; Brown, W.; Dobson, A. Accuracy of body mass index estimated from self-reported height and weight in mid-aged Australian women. Aust. N. Z. J. Public Health 2010, 34, 620–623. [Google Scholar] [CrossRef]
- Visscher, T.L.; Viet, A.L.; Kroesbergen, I.H.; Seidell, J.C. Underreporting of BMI in Adults and Its Effect on Obesity Prevalence Estimations in the Period 1998 to 2001. Obesity 2006, 14, 2054–2063. [Google Scholar] [CrossRef]
- Kurina, L.M.; McClintock, M.K.; Chen, J.-H.; Waite, L.J.; Thisted, R.A.; Lauderdale, D.S. Sleep duration and all-cause mortality: A critical review of measurement and associations. Ann. Epidemiol. 2013, 23, 361–370. [Google Scholar] [CrossRef]
| Statements from the Eating Preoccupation Scale (EPS) | Mean Score ± Standard Deviation * |
|---|---|
| EPS factor: Focusing on eating activities | |
| 2. I think about eating and about my body weight | 3.0 ± 1.2 |
| 6. I believe that my relationship with food is terrible | 2.3 ± 1.1 |
| 8. I feel embarrassed about the amount of food I eat | 2.2 ± 1.1 |
| 9. I plan ahead for situations when I will be able to eat alone | 1.9 ± 1.0 |
| 10. I am worried about being unable to control the amount of food consumed | 2.3 ± 1.1 |
| 16. I have a low self-esteem because of my uncontrolled eating | 2.1 ± 1.1 |
| EPS factor: Eating to provide pleasure and mood improvement | |
| 1. Eating is a very important part of my life | 3.4 ± 1.1 |
| 11. Eating greatly enhances my mood | 3.2 ± 1.0 |
| 12. Eating is a great pleasure of mine | 3.6 ± 1.0 |
| 13. I make myself “food feasts” for no clear reason | 2.2 ± 1.1 |
| 17. I feel great satisfaction after an abundant meal | 2.8 ± 1.1 |
| 18. I am willing to sacrifice other pleasures for eating | 2.3 ± 1.0 |
| EPS factor: Compulsion to eat and loss of control over food | |
| 3. I eat vast amounts of high-calorie foods in a short period of time | 2. 6 ± 1.0 |
| 4. I snack throughout the day | 2.9± 1.0 |
| 5. I eat even when I am not feeling hunger | 2.4 ± 1.0 |
| 7. I eat more than I had planned | 2.7 ± 1.0 |
| 14. I wake up to eat at night | 1.8 ± 1.0 |
| 15. I clear up my plate even when I am not feeling hungry anymore | 2.9 ± 1.2 |
| Variables | Total (N = 898) | 18.5 kg/m2 ≤ BMI < 25 kg/m2 (N = 424) | 25.0 kg/m2 ≤ BMI < 30 kg/m2 (N = 321) | BMI ≥ 30 kg/m2 (N = 153) | |||||
|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | ||
| Gender * | Female | 433 | 48.2 | 234 | 55.2 | 131 | 40.8 | 68 | 44.4 |
| Male | 465 | 51.8 | 190 | 44.8 | 190 | 59.2 | 85 | 55.6 | |
| Education | Lower than secondary | 348 | 38.8 | 153 | 36.1 | 123 | 38.3 | 72 | 47.1 |
| Secondary | 309 | 34.4 | 153 | 36.1 | 109 | 34.0 | 47 | 30.7 | |
| Higher | 241 | 26.8 | 118 | 27.8 | 89 | 27.7 | 34 | 22.2 | |
| Place of residence | Rural area | 329 | 36.6 | 159 | 37.5 | 113 | 35.2 | 57 | 37.3 |
| City ≤ 100,000 residents | 291 | 32.4 | 140 | 33.0 | 106 | 33.0 | 45 | 29.4 | |
| City > 100,000 residents | 278 | 31.0 | 125 | 29.5 | 102 | 31.8 | 51 | 33.3 | |
| Age * | 18–24 years | 97 | 10.8 | 72 | 17.0 | 18 | 5.6 | 7 | 4.6 |
| 25–34 years | 205 | 22.8 | 117 | 27.6 | 62 | 19.3 | 26 | 17.0 | |
| 35–44 years | 209 | 23.3 | 105 | 24.8 | 67 | 20.9 | 37 | 24.2 | |
| 45–54 years | 168 | 18.7 | 64 | 15.1 | 70 | 21.8 | 34 | 22.2 | |
| 55–65 years | 219 | 24.4 | 66 | 15.5 | 104 | 32.4 | 49 | 32.0 | |
| Age (years) | Mean; standard deviation | 42.0; 13.7 | 38.0 a; 13.3 | 45.6 b; 13.1 | 45.5 b; 12.9 | ||||
| Height (cm) | Mean; standard deviation | 171.4; 9.5 | 170.8 a; 9.1 | 172.4 a; 9.6 | 170.8 a; 9.9 | ||||
| Weight (kg) | Mean; standard deviation | 76.6; 15.8 | 65.7 a; 9.2 | 81.0 b; 10.2 | 97.6 c; 13.8 | ||||
| BMI (kg/m2) | Mean; standard deviation | 26.0; 4.5 | 22.4 a; 1.8 | 27.2 b; 1.4 | 33.4 c; 3.6 | ||||
| Variables | Total Sample (N = 898) | 18.5 kg/m2≤ BMI < 25 kg/m2 (N = 424) | 25.0 kg/m2≤ BMI < 30 kg/m2 (N = 321) | BMI ≥ 30 kg/m2 (N = 153) | |||||
|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | ||
| Food intake variety—FIV | inadequate | 79 | 8.8 | 38 | 9.0 | 25 | 7.8 | 16 | 10.5 |
| sufficient | 276 | 30.7 | 139 | 32.7 | 92 | 28.7 | 45 | 29.4 | |
| good | 330 | 36.8 | 147 | 34.7 | 125 | 38.9 | 58 | 37.9 | |
| very good | 213 | 23.7 | 100 | 23.6 | 79 | 24.6 | 34 | 22.2 | |
| Following a diet | yes | 97 | 10.9 | 42 | 10.0 | 37 | 11.6 | 18 | 12.0 |
| Number of cigarettes smoked ** | no smoking | 575 | 64.0 | 266 | 62.7 | 223 | 69.5 | 86 | 56.2 |
| less than 10 cigarettes a day | 174 | 19.4 | 91 | 21.5 | 56 | 17.4 | 27 | 17.6 | |
| 10 or more cigarettes a day | 149 | 16.6 | 67 | 15.8 | 42 | 13.1 | 40 | 26.2 | |
| Physical activity during work/school time | low | 329 | 38.3 | 137 | 34.3 | 123 | 39.4 | 69 | 47.3 |
| moderate | 329 | 38.3 | 158 | 39.5 | 120 | 38.5 | 51 | 34.9 | |
| high | 200 | 23.4 | 105 | 26.2 | 69 | 22.1 | 26 | 17.8 | |
| Physical activity during leisure time *** | low | 344 | 38.8 | 137 | 32.8 | 120 | 37.7 | 87 | 57.6 |
| moderate | 415 | 46.8 | 208 | 49.8 | 153 | 48.1 | 54 | 35.8 | |
| high | 128 | 14.4 | 73 | 17.4 | 45 | 14.2 | 10 | 6.6 | |
| Food intake variety—FIV (number of products) | Mean; standard deviation | 32.6; 10.7 | 32.4 a; 10.6 | 33.0 a; 10.5 | 32.6 a; 11.3 | ||||
| Variables | Total Sample (N = 898) | 18.5 kg/m2 ≤ BMI < 25 kg/m2 (N = 424) | 25.0 kg/m2 ≤ BMI < 30 kg/m2 (N = 321) | BMI ≥ 30 kg/m2 (N = 153) | |||||
|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | ||
| Eating Preoccupation Scale (EPS)—total score *** | low | 237 | 26.4 | 143 | 33.7 | 74 | 23.1 | 20 | 13.1 |
| average | 283 | 31.5 | 121 | 28.6 | 112 | 34.8 | 50 | 32.7 | |
| high | 378 | 42.1 | 160 | 37.7 | 135 | 42.1 | 83 | 54.2 | |
| Eating Preoccupation Scale (EPS)—total score | Mean; standard deviation | 46.4; 11.0 | 45.2 a; 11.6 | 46.7 a,b; 10.6 | 49.1 b; 9.9 | ||||
| EPS factor: Focus on eating activities | Mean; standard deviation | 13.7; 4.8 | 12.9 a; 5.0 | 13.8 b; 4.6 | 15.5 c; 4.1 | ||||
| EPS factor: Eating to provide pleasure and mood improvement | Mean; standard deviation | 17.5; 4.4 | 17.5 a; 4.5 | 17.6 a; 4.2 | 17.5 a; 4.3 | ||||
| EPS factor: Compulsion to eat and loss of control over food | Mean; standard deviation | 15.2; 4.2 | 14.8 a; 4.4 | 15.3 a,b; 4.1 | 16.1 b; 3.9 | ||||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jezewska-Zychowicz, M.; Małachowska, A.; Plichta, M. Does Eating Addiction Favor a More Varied Diet or Contribute to Obesity?—The Case of Polish Adults. Nutrients 2020, 12, 1304. https://doi.org/10.3390/nu12051304
Jezewska-Zychowicz M, Małachowska A, Plichta M. Does Eating Addiction Favor a More Varied Diet or Contribute to Obesity?—The Case of Polish Adults. Nutrients. 2020; 12(5):1304. https://doi.org/10.3390/nu12051304
Chicago/Turabian StyleJezewska-Zychowicz, Marzena, Aleksandra Małachowska, and Marta Plichta. 2020. "Does Eating Addiction Favor a More Varied Diet or Contribute to Obesity?—The Case of Polish Adults" Nutrients 12, no. 5: 1304. https://doi.org/10.3390/nu12051304
APA StyleJezewska-Zychowicz, M., Małachowska, A., & Plichta, M. (2020). Does Eating Addiction Favor a More Varied Diet or Contribute to Obesity?—The Case of Polish Adults. Nutrients, 12(5), 1304. https://doi.org/10.3390/nu12051304







