Self-Reported Eating Speed and Incidence of Gestational Diabetes Mellitus: the Japan Environment and Children’s Study
Abstract
1. Introduction
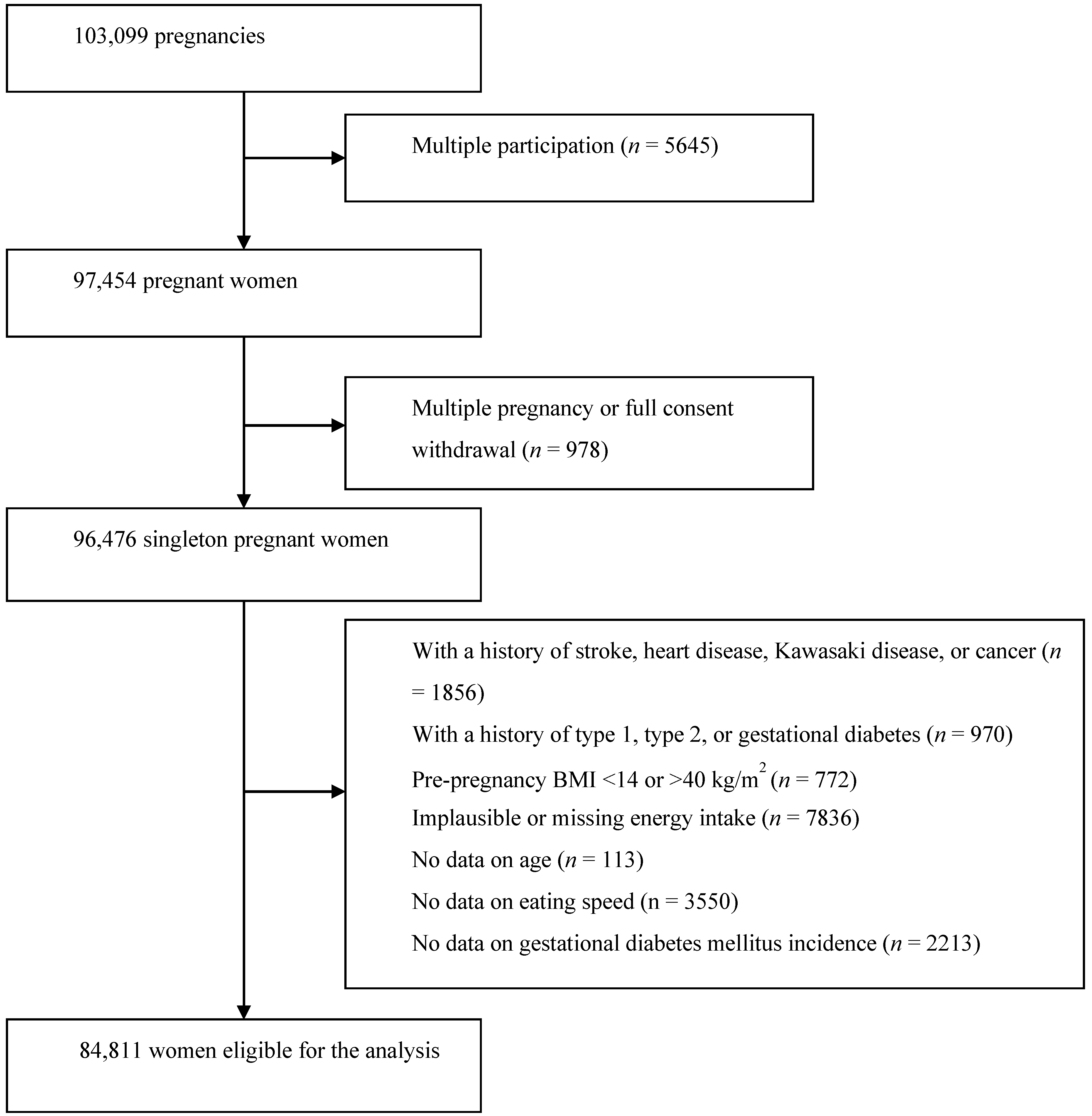
2. Research Design and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Ohkuma, T.; Hirakawa, Y.; Nakamura, U.; Kiyohara, Y.; Kitazono, T.; Ninomiya, T. Association between eating rate and obesity: A systematic review and meta-analysis. Int. J. Obes. 2015, 39, 1589–1596. [Google Scholar] [CrossRef] [PubMed]
- Robinson, E.; Almiron-Roig, E.; Rutters, F.; de Graaf, C.; Forde, C.G.; Tudur Smith, C.; Nolan, S.J.; Jebb, S.A. A systematic review and meta-analysis examining the effect of eating rate on energy intake and hunger. Am. J. Clin. Nutr. 2014, 100, 123–151. [Google Scholar] [CrossRef] [PubMed]
- Nagahama, S.; Kurotani, K.; Pham, N.M.; Nanri, A.; Kuwahara, K.; Dan, M.; Nishiwaki, Y.; Mizoue, T. Self-reported eating rate and metabolic syndrome in Japanese people: Cross-sectional study. BMJ Open 2014, 4, e005241. [Google Scholar] [CrossRef] [PubMed]
- Shin, A.; Lim, S.Y.; Sung, J.; Shin, H.R.; Kim, J. Dietary intake, eating habits, and metabolic syndrome in Korean men. J. Am. Diet. Assoc. 2009, 109, 633–640. [Google Scholar] [CrossRef] [PubMed]
- Zhu, B.; Haruyama, Y.; Muto, T.; Yamazaki, T. Association between eating speed and metabolic syndrome in a three-year population-based cohort study. J. Epidemiol. 2015, 25, 332–336. [Google Scholar] [CrossRef]
- Sakurai, M.; Nakamura, K.; Miura, K.; Takamura, T.; Yoshita, K.; Nagasawa, S.Y. Self-reported speed of eating and 7-year risk of type 2 diabetes mellitus in middle-aged Japanese men. Metab. Clin. Exp. 2012, 61, 1566–1571. [Google Scholar] [CrossRef]
- American Diabetes Association: Gestational diabetes mellitus. Diabetes Care 2003, 26 (Suppl. 1), S103–S105. [CrossRef]
- Reece, E.A.; Leguizamon, G.; Wiznitzer, A. Gestational diabetes: The need for a common ground. Lancet 2009, 373, 1789–1797. [Google Scholar] [CrossRef]
- Morikawa, M.; Yamada, T.; Yamada, T.; Akaishi, R.; Nishida, R.; Cho, K. Change in the number of patients after the adoption of IADPSG criteria for hyperglycemia during pregnancy in Japanese women. Diabetes Res. Clin. Pract. 2010, 90, 339–342. [Google Scholar] [CrossRef]
- Kc, K.; Shakya, S.; Zhang, H. Gestational diabetes mellitus and macrosomia: A literature review. Ann. Nutr. Metab. 2015, 66 (Suppl. 2), 14–20. [Google Scholar] [CrossRef]
- He, X.J.; Qin, F.Y.; Hu, C.L.; Zhu, M.; Tian, C.Q.; Li, L. Is gestational diabetes mellitus an independent risk factor for macrosomia: A meta-analysis? Arch. Gynecol. Obstet. 2015, 291, 729–735. [Google Scholar] [CrossRef] [PubMed]
- Bellamy, L.; Casas, J.P.; Hingorani, A.D.; Williams, D. Type 2 diabetes mellitus after gestational diabetes: A systematic review and meta-analysis. Lancet 2009, 373, 1773–1779. [Google Scholar] [CrossRef]
- Li, J.; Song, C.; Li, C.; Liu, P.; Sun, Z.; Yang, X. Increased risk of cardiovascular disease in women with prior gestational diabetes: A systematic review and meta-analysis. Diabetes Res. Clin. Pract. 2018, 140, 324–338. [Google Scholar] [CrossRef] [PubMed]
- Boerschmann, H.; Pfluger, M.; Henneberger, L.; Ziegler, A.G.; Hummel, S. Prevalence and predictors of overweight and insulin resistance in offspring of mothers with gestational diabetes mellitus. Diabetes Care 2010, 33, 1845–1849. [Google Scholar] [CrossRef]
- Maftei, O.; Whitrow, M.J.; Davies, M.J.; Giles, L.C.; Owens, J.A.; Moore, V.M. Maternal body size prior to pregnancy, gestational diabetes and weight gain: Associations with insulin resistance in children at 9-10 years. Diabetic Med. J. Br. Diabetic Assoc. 2015, 32, 174–180. [Google Scholar] [CrossRef]
- Shepherd, E.; Gomersall, J.C.; Tieu, J.; Han, S.; Crowther, C.A.; Middleton, P. Combined diet and exercise interventions for preventing gestational diabetes mellitus. Cochrane Database Syst. Rev. 2017, 11, Cd010443. [Google Scholar] [CrossRef]
- Zhang, C.; Rawal, S.; Chong, Y.S. Risk factors for gestational diabetes: Is prevention possible? Diabetologia 2016, 59, 1385–1390. [Google Scholar] [CrossRef]
- Kawamoto, T.; Nitta, H.; Murata, K.; Toda, E.; Tsukamoto, N.; Hasegawa, M. Rationale and study design of the Japan environment and children’s study (JECS). BMC Public Health 2014, 14, 25. [Google Scholar] [CrossRef]
- Michikawa, T.; Nitta, H.; Nakayama, S.F.; Yamazaki, S.; Isobe, T.; Tamura, K.; Suda, E.; Ono, M.; Yonemoto, J.; Iwai-Shimada, M.; et al. Baseline Profile of Participants in the Japan Environment and Children’s Study (JECS). J. Epidemiol. 2018, 28, 99–104. [Google Scholar] [CrossRef]
- Maruyama, K.; Sato, S.; Ohira, T.; Maeda, K.; Noda, H.; Kubota, Y.; Nishimura, S.; Kitamura, A.; Kiyama, M.; Okada, T.; et al. The joint impact on being overweight of self reported behaviours of eating quickly and eating until full: Cross sectional survey. BMJ 2008, 337, a2002. [Google Scholar]
- Yokoyama, Y.; Takachi, R.; Ishihara, J.; Ishii, Y.; Sasazuki, S.; Sawada, N. Validity of Short and Long Self-Administered Food Frequency Questionnaires in Ranking Dietary Intake in Middle-Aged and Elderly Japanese in the Japan Public Health Center-Based Prospective Study for the Next Generation (JPHC-NEXT) Protocol Area. J. Epidemiol. 2016, 26, 420–432. [Google Scholar] [CrossRef] [PubMed]
- Minakami, H.; Hiramatsu, Y.; Koresawa, M.; Fujii, T.; Hamada, H.; Iitsuka, Y.; Ikeda, T.; Ishikawa, H.; Ishimoto, H.; Itoh, H.; et al. Guidelines for obstetrical practice in Japan: Japan Society of Obstetrics and Gynecology (JSOG) and Japan Association of Obstetricians and Gynecologists (JAOG) 2011 edition. J. Obstet. Gynaecol. Res. 2011, 37, 1174–1197. [Google Scholar] [CrossRef] [PubMed]
- Murphy, K.G.; Bloom, S.R. Gut hormones and the regulation of energy homeostasis. Nature. 2006, 444, 854–859. [Google Scholar] [CrossRef] [PubMed]
- Wren, A.M.; Bloom, S.R. Gut hormones and appetite control. Gastroenterology 2007, 132, 2116–2130. [Google Scholar] [CrossRef]
- Yu, J.H.; Kim, M.S. Molecular mechanisms of appetite regulation. Diabetes Metab. J. 2012, 36, 391–398. [Google Scholar] [CrossRef]
- Kokkinos, A.; le Roux, C.W.; Alexiadou, K.; Tentolouris, N.; Vincent, R.P.; Kyriaki, D. Eating slowly increases the postprandial response of the anorexigenic gut hormones, peptide YY and glucagon-like peptide-1. J. Clin. Endocrinol. Metab. 2010, 95, 333–337. [Google Scholar] [CrossRef]
- Yamane, M.; Ekuni, D.; Mizutani, S.; Kataoka, K.; Sakumoto-Kataoka, M.; Kawabata, Y.; Sakumoto-Kataoka, M.; Kawabata, Y.; Omori, C.; Azuma, T.; et al. Relationships between eating quickly and weight gain in Japanese university students: A longitudinal study. Obesity 2014, 22, 2262–2266. [Google Scholar] [CrossRef]
- Otsuka, R.; Tamakoshi, K.; Yatsuya, H.; Wada, K.; Matsushita, K.; OuYang, P.; Hotta, Y.; Takefuji, S.; Mitsuhashi, H.; Sugiura, K.; et al. Eating fast leads to insulin resistance: Findings in middle-aged Japanese men and women. Prev. Med. 2008, 46, 154–159. [Google Scholar] [CrossRef]
- Dong, J.Y.; Ikehara, S.; Kimura, T.; Cui, M.; Kawanishi, Y.; Kimura, T. Skipping breakfast before and during early pregnancy and incidence of gestational diabetes mellitus: The Japan Environment and Children’s Study. Am. J. Clin. Nutr. 2020. (Epub ahead of print). [Google Scholar] [CrossRef]
| Slow | Medium | Relatively Fast | Very Fast | p | |
|---|---|---|---|---|---|
| No. of participants | 15,061 | 34,857 | 30,080 | 4813 | |
| Age, years | 29.8 | 30.7 | 31.0 | 31.5 | <0.001 |
| BMI before pregnancy, kg/m2 | 20.6 | 21.0 | 21.5 | 21.8 | <0.001 |
| Gestational weight gain, kg | 10.1 | 10.3 | 10.3 | 10.5 | 0.03 |
| University or higher education, % | 23.2 | 20.8 | 22.4 | 22.4 | <0.001 |
| Family income < 2 million/y, % | 5.3 | 5.1 | 4.6 | 5.2 | <0.001 |
| Housewife, % | 28.2 | 29.0 | 26.3 | 23.0 | <0.001 |
| Married, % | 94.6 | 95.3 | 95.5 | 94.9 | <0.001 |
| Nulliparous, % | 48.3 | 39.2 | 40.6 | 42.4 | <0.001 |
| History of macrosomia baby, % | 0.3 | 0.5 | 0.5 | 0.6 | 0.006 |
| Never smoker, % | 61.1 | 59.7 | 56.9 | 52.4 | <0.001 |
| Never drinker, % | 54.4 | 54.5 | 56.3 | 56.0 | <0.001 |
| Depression, % | 3.7 | 2.7 | 2.8 | 3.9 | <0.001 |
| Polycystic ovarian syndrome, % | 2.4 | 2.0 | 2.4 | 2.2 | 0.005 |
| Physical activity, Met∙h/day | 3.6 | 3.9 | 3.9 | 4.6 | <0.001 |
| Total energy, kcal/day | 1752 | 1750 | 1798 | 1880 | <0.001 |
| White rice, g/day | 272.9 | 281.3 | 292.5 | 305.2 | <0.001 |
| Seafood, g/day | 37.5 | 37.5 | 38.2 | 39.3 | <0.001 |
| Meat, g/day | 68.9 | 69.8 | 74.2 | 81.0 | <0.001 |
| Egg, g/day | 29.6 | 30.4 | 31.9 | 34.5 | <0.001 |
| Coffee, g/day | 101 | 104 | 111 | 118 | <0.001 |
| Green tea, g/day | 165 | 161 | 165 | 182 | <0.001 |
| Milk, g/day | 135 | 127 | 123 | 122 | 0.003 |
| Total dietary fat, g/day | 58.6 | 58.2 | 60.1 | 63.6 | <0.001 |
| Magnesium, mg/day | 233 | 233 | 238 | 246 | <0.001 |
| Total dietary fiber, g/day | 11.0 | 11.0 | 11.2 | 11.5 | <0.001 |
| Chocolate, g/day | 6.2 | 5.6 | 5.8 | 6.4 | <0.001 |
| Isoflavones, mg/day | 30.6 | 31.2 | 31.6 | 32.8 | <0.001 |
| Slow | Medium | Relatively Fast | Very Fast | |
|---|---|---|---|---|
| No of participants | 15,061 | 34,857 | 30,080 | 4813 |
| No of cases | 298 | 766 | 699 | 139 |
| Model 1 | 1.00 | 1.03 (0.90, 1.18) | 1.07 (0.94, 1.23) | 1.28 (1.05, 1.58) |
| Model 2 | 1.00 | 1.08 (0.94, 1.24) | 1.13 (0.99, 1.30) | 1.35 (1.10, 1.66) |
| Model 3 | 1.00 | 1.08 (0.94, 1.24) | 1.11 (0.97, 1.28) | 1.29 (1.05, 1.59) |
| Model 3 + pre-pregnancy BMI | 1.00 | 1.04 (0.90, 1.19) | 1.01 (0.88, 1.16) | 1.14 (0.93, 1.41) |
| Slow | Medium | Relatively Fast | Very Fast | |
|---|---|---|---|---|
| No. of participants | 10,783 | 26,520 | 23,777 | 3103 |
| No. of cases | 206 | 578 | 541 | 97 |
| Model 1 | 1.00 | 1.07 (0.91, 1.25) | 1.09 (0.93, 1.29) | 1.45 (1.13, 1.85) |
| Model 2 | 1.00 | 1.11 (0.95, 1.31) | 1.16 (0.98, 1.37) | 1.55 (1.21, 1.99) |
| Model 3 | 1.00 | 1.17 (0.95, 1.31) | 1.15 (0.97, 1.35) | 1.50 (1.16, 1.92) |
| Model 3 + pre-pregnancy BMI | 1.00 | 1.07 (0.91, 1.26) | 1.04 (0.88, 1.23) | 1.32 (1.03, 1.70) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dong, J.-Y.; Ikehara, S.; Kimura, T.; Cui, M.; Kawanishi, Y.; Kimura, T.; Ueda, K.; Iso, H.; the Japan Environment and Children’s Study Group. Self-Reported Eating Speed and Incidence of Gestational Diabetes Mellitus: the Japan Environment and Children’s Study. Nutrients 2020, 12, 1296. https://doi.org/10.3390/nu12051296
Dong J-Y, Ikehara S, Kimura T, Cui M, Kawanishi Y, Kimura T, Ueda K, Iso H, the Japan Environment and Children’s Study Group. Self-Reported Eating Speed and Incidence of Gestational Diabetes Mellitus: the Japan Environment and Children’s Study. Nutrients. 2020; 12(5):1296. https://doi.org/10.3390/nu12051296
Chicago/Turabian StyleDong, Jia-Yi, Satoyo Ikehara, Takashi Kimura, Meishan Cui, Yoko Kawanishi, Tadashi Kimura, Kimiko Ueda, Hiroyasu Iso, and the Japan Environment and Children’s Study Group. 2020. "Self-Reported Eating Speed and Incidence of Gestational Diabetes Mellitus: the Japan Environment and Children’s Study" Nutrients 12, no. 5: 1296. https://doi.org/10.3390/nu12051296
APA StyleDong, J.-Y., Ikehara, S., Kimura, T., Cui, M., Kawanishi, Y., Kimura, T., Ueda, K., Iso, H., & the Japan Environment and Children’s Study Group. (2020). Self-Reported Eating Speed and Incidence of Gestational Diabetes Mellitus: the Japan Environment and Children’s Study. Nutrients, 12(5), 1296. https://doi.org/10.3390/nu12051296





