Dietary Fructose Intake and Hippocampal Structure and Connectivity during Childhood
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Clinical Characteristics and Demographics
2.3. Dietary Measures
2.4. Magnetic Resonance Imaging (MRI) Acquisition
2.5. MRI Data Processing
2.6. Statistical Analysis
3. Results
3.1. Participant Characteristics
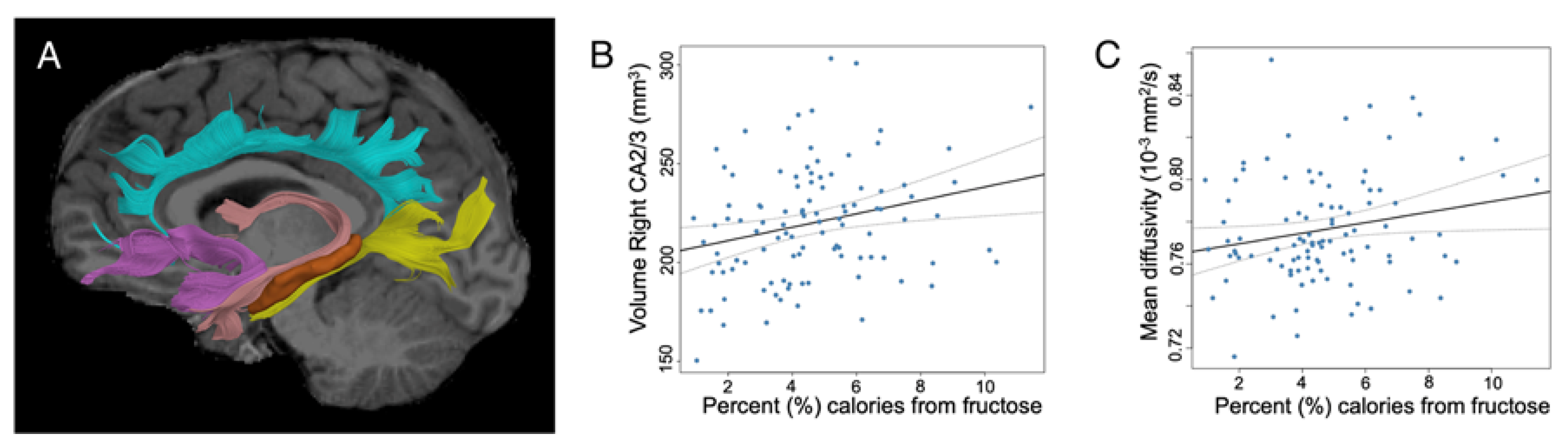
3.2. Influence of Diet on Hippocampal Volumes
3.3. Influence of Diet on Hippocampal Connectivity
3.4. Post-hocs for Diffusion Imaging Measures
4. Discussion
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Bray, G.A.; Nielsen, S.J.; Popkin, B.M. Consumption of high-fructose corn syrup in beverages may play a role in the epidemic of obesity. Am. J. Clin. Nutr. 2004, 79, 537–543. [Google Scholar] [CrossRef]
- Basciano, H.; Federico, L.; Adeli, K. Fructose, insulin resistance, and metabolic dyslipidemia. Nutr. Metab. 2005, 2, 5. [Google Scholar] [CrossRef]
- Tappy, L.; Le, K.A. Metabolic Effects of Fructose and the Worldwide Increase in Obesity. Physiol. Rev. 2010, 90, 23–46. [Google Scholar] [CrossRef]
- Johnson, R.J.; Segal, M.S.; Sautin, Y.; Nakagawa, T.; Feig, D.I.; Kang, D.-H.; Gersch, M.S.; Benner, S.; Sánchez-Lozada, L.G. Potential role of sugar (fructose) in the epidemic of hypertension, obesity and the metabolic syndrome, diabetes, kidney disease, and cardiovascular disease. Am. J. Clin. Nutr. 2007, 86, 899–906. [Google Scholar]
- Lindqvist, A.; Baelemans, A.; Erlanson-Albertsson, C. Effects of sucrose, glucose and fructose on peripheral and central appetite signals. Regul. Pept. 2008, 150, 26–32. [Google Scholar] [CrossRef]
- Page, K.A.; Chan, O.; Arora, J.; Belfort-DeAguiar, R.; Dzuira, J.; Roehmholdt, B.; Cline, G.W.; Naik, S.; Sinha, R.; Constable, R.T.; et al. Effects of Fructose vs Glucose on Regional Cerebral Blood Flow in Brain Regions Involved with Appetite and Reward Pathways. JAMA 2013, 309, 63. [Google Scholar] [CrossRef]
- Luo, S.; Monterosso, J.R.; Sarpelleh, K.; Page, K.A. Differential effects of fructose versus glucose on brain and appetitive responses to food cues and decisions for food rewards. Proc. Natl. Acad. Sci. USA 2015, 112, 6509–6514. [Google Scholar] [CrossRef]
- Teff, K.L.; Elliott, S.S.; Tschöp, M.; Kieffer, T.J.; Rader, D.; Heiman, M.; Townsend, R.R.; Keim, N.L.; D’Alessio, D.; Havel, P.J. Dietary Fructose Reduces Circulating Insulin and Leptin, Attenuates Postprandial Suppression of Ghrelin, and Increases Triglycerides in Women. J. Clin. Endocrinol. Metab. 2004, 89, 2963–2972. [Google Scholar] [CrossRef]
- Cha, S.H.; Wolfgang, M.; Tokutake, Y.; Chohnan, S.; Lane, M.D. Differential effects of central fructose and glucose on hypothalamic malonyl—CoA and food intake. Proc. Natl. Acad. Sci. USA 2008, 105, 16871–16875. [Google Scholar] [CrossRef]
- Erlanson-Albertsson, C.; Lindqvist, A. Fructose affects enzymes involved in the synthesis and degradation of hypothalamic endocannabinoids. Regul. Pept. 2010, 161, 87–91. [Google Scholar] [CrossRef]
- Lowette, K.; Roosen, L.; Tack, J.; Vanden Berghe, P. Effects of high-fructose diets on central appetite signaling and cognitive function. Front. Nutr. 2015, 2, 5. [Google Scholar] [CrossRef]
- Lakhan, S.E.; Kirchgessner, A. The emerging role of dietary fructose in obesity and cognitive decline. Nutr. J. 2013, 12, 114. [Google Scholar] [CrossRef]
- Hsu, T.M.; Kanoski, S.E. Blood-brain barrier disruption: Mechanistic links between Western diet consumption and dementia. Front. Aging Neurosci. 2014, 6, 88. [Google Scholar] [CrossRef]
- Davidson, T.L.; Chan, K.; Jarrard, L.E.; Kanoski, S.E.; Clegg, D.J.; Benoit, S.C. Contributions of the Hippocampus and Medial Prefrontal Cortex to Energy and Body Weight Regulation. Hippocampus 2009, 19, 235–252. [Google Scholar] [CrossRef]
- Hannapel, R.C.; Henderson, Y.H.; Nalloor, R.; Vazdarjanova, A.; Parent, M.B. Ventral hippocampal neurons inhibit postprandial energy intake. Hippocampus 2017, 27, 274–284. [Google Scholar] [CrossRef]
- Agrawal, R.; Gomez-Pinilla, F. “Metabolic syndrome” in the brain: Deficiency in omega-3 fatty acid exacerbates dysfunctions in insulin receptor signalling and cognition. J. Physiol. 2012, 590, 2485–2499. [Google Scholar] [CrossRef]
- Wu, H.-W.; Ren, L.-F.; Zhou, X.; Han, D.-W. A high-fructose diet induces hippocampal insulin resistance and exacerbates memory deficits in male Sprague-Dawley rats. Nutr. Neurosci. 2015, 18, 323–328. [Google Scholar] [CrossRef]
- Hsu, T.M.; Konanur, V.R.; Taing, L.; Usui, R.; Kayser, B.D.; Goran, M.I.; Kanoski, S.E. Effects of sucrose and high fructose corn syrup consumption on spatial memory function and hippocampal neuroinflammation in adolescent rats. Hippocampus 2015, 25, 227–239. [Google Scholar] [CrossRef]
- Djordjevic, A.; Bursać, B.; Veličković, N.; Vasiljević, A.; Matić, G. The impact of different fructose loads on insulin sensitivity, inflammation, and PSA-NCAM-mediated plasticity in the hippocampus of fructose-fed male rats. Nutr. Neurosci. 2015, 18, 66–75. [Google Scholar] [CrossRef]
- Van der Borght, K.; Köhnke, R.; Göransson, N.; Deierborg, T.; Brundin, P.; Erlanson-Albertsson, C.; Lindqvist, A. Reduced neurogenesis in the rat hippocampus following high fructose consumption. Regul. Pept. 2011, 167, 26–30. [Google Scholar] [CrossRef]
- Ross, A.P.; Bartness, T.J.; Mielke, J.G.; Parent, M.B. A high fructose diet impairs spatial memory in male rats. Neurobiol. Learn. Mem. 2009, 92, 410–416. [Google Scholar] [CrossRef]
- Hebben, N.; Corkin, S.; Eichenbaum, H.; Shedlack, K. Diminished ability to interpret and report internal states after bilateral medial temporal resection: Case, H.M. Behav. Neurosci. 1985, 99, 1031–1039. [Google Scholar] [CrossRef]
- Rozin, P.; Dow, S.; Moscovitch, M.; Rajaram, S. What Causes Humans to Begin and End a Meal? A Role for Memory for What Has Been Eaten, as Evidenced by a Study of Multiple Meal Eating in Amnesic Patients. Psychol. Sci. 1998, 9, 392–396. [Google Scholar] [CrossRef]
- Maller, J.J.; Welton, T.; Middione, M.; Callaghan, F.M.; Rosenfeld, J.V.; Grieve, S.M. Revealing the Hippocampal Connectome through Super-Resolution 1150-Direction Diffusion MRI. Sci. Rep. 2019, 9, 2418. [Google Scholar] [CrossRef] [PubMed]
- Chudasama, Y.; Doobay, V.M.; Liu, Y. Hippocampal-Prefrontal Cortical Circuit Mediates Inhibitory Response Control in the Rat. J. Neurosci. 2012, 32, 10915–10924. [Google Scholar] [CrossRef] [PubMed]
- Hsu, T.M.; Noble, E.E.; Liu, C.M.; Cortella, A.M.; Konanur, V.R.; Suarez, A.N.; Reiner, D.J.; Hahn, J.D.; Hayes, M.R.; Kanoski, S.E. A hippocampus to prefrontal cortex neural pathway inhibits food motivation through glucagon-like peptide-1 signaling. Mol. Psychiatry 2018, 23, 1555–1565. [Google Scholar] [CrossRef] [PubMed]
- Sweeney, P.; Yang, Y. An excitatory ventral hippocampus to lateral septum circuit that suppresses feeding. Nat. Commun. 2015, 6, 10188. [Google Scholar] [CrossRef] [PubMed]
- Russo, C.; Russo, A.; Pellitteri, R.; Stanzani, S. Hippocampal Ghrelin-positive neurons directly project to arcuate hypothalamic and medial amygdaloid nuclei. Could they modulate food-intake? Neurosci. Lett. 2017, 653, 126–131. [Google Scholar] [CrossRef] [PubMed]
- Geha, P.; Cecchi, G.; Constable, R.T.; Abdallah, C.; Small, D.M. Reorganization of brain connectivity in obesity. Hum. Brain Mapp. 2017, 38, 1403–1420. [Google Scholar] [CrossRef]
- Alexander, A.L.; Lee, J.E.; Lazar, M.; Field, A.S. Diffusion Tensor Imaging of the Brain. Neurotherapeutics 2007, 4, 316–329. [Google Scholar] [CrossRef]
- Koebnick, C.; Langer-Gould, A.M.; Gould, M.K.; Chao, C.R.; Iyer, R.L.; Smith, N.; Chen, W.; Jacobsen, S.J. Sociodemographic Characteristics of Members of a Large, Integrated Health Care System: Comparison with US Census Bureau Data. Perm. J. 2012, 16, 37–41. [Google Scholar] [CrossRef] [PubMed]
- Defining Childhood Obesity|Overweight & Obesity|CDC. Available online: https://www.cdc.gov/obesity/childhood/defining.html (accessed on 1 November 2019).
- Marshall, W.A.; Tanner, J.M. Variations in pattern of pubertal changes in girls. Arch. Dis. Child. 1969, 44, 291–303. [Google Scholar] [CrossRef] [PubMed]
- Marshall, W.A.; Tanner, J.M. Variations in the pattern of pubertal changes in boys. Arch. Dis. Child. 1970, 45, 13–23. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen, A.R.; Wohlfahrt-Veje, C.; Tefre de Renzy-Martin, K.; Hagen, C.P.; Tinggaard, J.; Mouritsen, A.; Mieritz, M.G.; Main, K.M. Validity of self-assessment of pubertal maturation. Pediatrics 2015, 135, 86–93. [Google Scholar] [CrossRef]
- Johnson, R.K.; Driscoll, P.; Goran, M.I. Comparison of Multiple-Pass 24-Hour Recall Estimates of Energy Intake with Total Energy Expenditure Determined by the Doubly Labeled Water Method in Young Children. J. Am. Diet. Assoc. 1996, 96, 1140–1144. [Google Scholar] [CrossRef]
- Schakel, S.F.; Buzzard, I.M.; Gebhardt, S.E. Procedures for Estimating Nutrient Values for Food Composition Databases. J. Food Compos. Anal. 1997, 10, 102–114. [Google Scholar] [CrossRef]
- Iglesias, J.E.; Augustinack, J.C.; Nguyen, K.; Player, C.M.; Player, A.; Wright, M.; Roy, N.; Frosch, M.P.; McKee, A.C.; Wald, L.L.; et al. A computational atlas of the hippocampal formation using ex vivo, ultra-high resolution MRI: Application to adaptive segmentation of in vivo MRI. NeuroImage 2015, 115, 117–137. [Google Scholar] [CrossRef]
- Backhausen, L.L.; Herting, M.M.; Buse, J.; Roessner, V.; Smolka, M.N.; Vetter, N.C. Quality Control of Structural MRI Images Applied Using FreeSurfer—A Hands-On Workflow to Rate Motion Artifacts. Front. Neurosci. 2016, 10, 558. [Google Scholar] [CrossRef]
- Calvo-Ochoa, E.; Hernández-Ortega, K.; Ferrera, P.; Morimoto, S.; Arias, C. Short-term high-fat-and-fructose feeding produces insulin signaling alterations accompanied by neurite and synaptic reduction and astroglial activation in the rat hippocampus. J. Cereb. Blood Flow Metab. 2014, 34, 1001–1008. [Google Scholar] [CrossRef]
- Molteni, R.; Barnard, R.J.; Ying, Z.; Roberts, C.K.; Gómez-Pinilla, F. A high-fat, refined sugar diet reduces hippocampal brain-derived neurotrophic factor, neuronal plasticity, and learning. Neuroscience 2002, 112, 803–814. [Google Scholar] [CrossRef]
- Al-Amin, M.; Zinchenko, A.; Geyer, T. Hippocampal subfield volume changes in subtypes of attention deficit hyperactivity disorder. Brain Res. 2018, 1685, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Tamnes, C.K.; Walhovd, K.B.; Engvig, A.; Grydeland, H.; Krogsrud, S.K.; Østby, Y.; Holland, D.; Dale, A.M.; Fjell, A.M. Regional Hippocampal Volumes and Development Predict Learning and Memory. Dev. Neurosci. 2014, 36, 161–174. [Google Scholar] [CrossRef] [PubMed]
- Jenkinson, M.; Beckmann, C.F.; Behrens, T.E.J.; Woolrich, M.W.; Smith, S.M. FSL. Neuroimage 2012, 62, 782–790. [Google Scholar] [CrossRef] [PubMed]
- Cabeen, R.P.; Laidlaw, D.H.; Toga, A.W. Quantitative Imaging Toolkit: Software for Interactive 3D Visualization, Processing, and Analysis of Neuroimaging Datasets. In Proceedings of the Annual Meeting of the International Society for Magnetic Resonance in Medicine (ISMRM), Paris, France, 2018. [Google Scholar]
- Arsigny, V.; Fillard, P.; Pennec, X.; Ayache, N. Log-Euclidean metrics for fast and simple calculus on diffusion tensors. Magn. Reson. Med. 2006, 56, 411–421. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Yushkevich, P.A.; Alexander, D.C.; Gee, J.C. Deformable registration of diffusion tensor MR images with explicit orientation optimization. Med. Image Anal. 2006, 10, 764–785. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Peng, H.; Dawe, R.J.; Arfanakis, K. Enhanced ICBM Diffusion Tensor Template of the Human Brain. Neuroimage 2011, 54, 974–984. [Google Scholar] [CrossRef]
- Cabeen, R.P.; Bastin, M.E.; Laidlaw, D.H. Kernel Regression Estimation of Fiber Orientation Mixtures in Diffusion MRI. Neuroimage 2016, 127, 158–172. [Google Scholar] [CrossRef]
- Wakana, S.; Caprihan, A.; Panzenboeck, M.M.; Fallon, J.H.; Perry, M.; Gollub, R.L.; Hua, K.; Zhang, J.; Jiang, H.; Dubey, P.; et al. Reproducibility of quantitative tractography methods applied to cerebral white matter. Neuroimage 2007, 36, 630–644. [Google Scholar] [CrossRef]
- Catani, M.; Thiebaut de Schotten, M. A diffusion tensor imaging tractography atlas for virtual in vivo dissections. Cortex 2008, 44, 1105–1132. [Google Scholar] [CrossRef]
- Neil, J.; Miller, J.; Mukherjee, P.; Hüppi, P.S. Diffusion tensor imaging of normal and injured developing human brain—A technical review. NMR Biomed. 2002, 15, 543–552. [Google Scholar] [CrossRef]
- Snook, L.; Paulson, L.-A.; Roy, D.; Phillips, L.; Beaulieu, C. Diffusion tensor imaging of neurodevelopment in children and young adults. NeuroImage 2005, 26, 1164–1173. [Google Scholar] [CrossRef] [PubMed]
- Mukherjee, P.; McKinstry, R.C. Diffusion tensor imaging and tractography of human brain development. Neuroimaging Clin. N. Am. 2006, 16, 19–43. [Google Scholar] [CrossRef] [PubMed]
- Bonekamp, D.; Nagae, L.M.; Degaonkar, M.; Matson, M.; Abdalla, W.M.; Barker, P.B.; Mori, S.; Horská, A. Diffusion tensor imaging in children and adolescents: Reproducibility, hemispheric, and age-related differences. Neuroimage 2007, 34, 733–742. [Google Scholar] [CrossRef] [PubMed]
- Drewnowski, A.; Rehm, C.D. Energy intakes of US children and adults by food purchase location and by specific food source. Nutr. J. 2013, 12, 59. [Google Scholar] [CrossRef] [PubMed]
- CDC Know Your Limit for Added Sugars. Available online: https://www.cdc.gov/nutrition/data-statistics/know-your-limit-for-added-sugars.html (accessed on 19 December 2019).
- Zach, P.; Mrzílková, J.; Stuchlík, A.; Valeš, K. Delayed Effects of Elevated Corticosterone Level on Volume of Hippocampal Formation in Laboratory Rat. Physiol. Res. 2010, 59, 12. [Google Scholar]
- Teicher, M.H.; Anderson, C.M.; Polcari, A. Childhood maltreatment is associated with reduced volume in the hippocampal subfields CA3, dentate gyrus, and subiculum. Proc. Natl. Acad. Sci. USA 2012, 109, E563–E572. [Google Scholar] [CrossRef]
- Andersson, J.L.; Skare, S.; Ashburner, J. How to correct susceptibility distortions in spin-echo echo-planar images: Application to diffusion tensor imaging. Neuroimage 2003, 20, 870–888. [Google Scholar] [CrossRef]
- Tamnes, C.K.; Bos, M.G.N.; van de Kamp, F.C.; Peters, S.; Crone, E.A. Longitudinal development of hippocampal subregions from childhood to adulthood. Dev. Cogn. Neurosci. 2018, 30, 212–222. [Google Scholar] [CrossRef]
- Canada, K.L.; Ngo, C.T.; Newcombe, N.S.; Geng, F.; Riggins, T. It’s All in the Details: Relations Between Young Children’s Developing Pattern Separation Abilities and Hippocampal Subfield Volumes. Cereb. Cortex 2019, 29, 3427–3433. [Google Scholar] [CrossRef]
- Vuong, B.; Odero, G.; Rozbacher, S.; Stevenson, M.; Kereliuk, S.M.; Pereira, T.J.; Dolinsky, V.W.; Kauppinen, T.M. Exposure to gestational diabetes mellitus induces neuroinflammation, derangement of hippocampal neurons, and cognitive changes in rat offspring. J. Neuroinflamm. 2017, 14, 80. [Google Scholar] [CrossRef]
- Hershey, T.; Perantie, D.C.; Wu, J.; Weaver, P.M.; Black, K.J.; White, N.H. Hippocampal Volumes in Youth with Type 1 Diabetes. Diabetes 2010, 59, 236–241. [Google Scholar] [CrossRef][Green Version]
- Beilharz, J.E.; Maniam, J.; Morris, M.J. Short-term exposure to a diet high in fat and sugar, or liquid sugar, selectively impairs hippocampal-dependent memory, with differential impacts on inflammation. Behav. Brain Res. 2016, 306, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.K.; Ekstrom, A.D.; Ghetti, S. Volume of hippocampal subfields and episodic memory in childhood and adolescence. NeuroImage 2014, 94, 162–171. [Google Scholar] [CrossRef] [PubMed]
- Jabès, A.; Lavenex, P.B.; Amaral, D.G.; Lavenex, P. Postnatal Development of the Hippocampal Formation: A Stereological Study in Macaque Monkeys. J. Comp. Neurol. 2011, 519, 1051–1070. [Google Scholar] [CrossRef] [PubMed]
- Lu, D.; He, L.; Xiang, W.; Ai, W.-M.; Cao, Y.; Wang, X.S.; Pan, A.; Luo, X.-G.; Li, Z.; Yan, X.-X. Somal and Dendritic Development of Human CA3 Pyramidal Neurons from Midgestation to Middle Childhood: A Quantitative Golgi Study. Anat. Rec. 2013, 296 Pt 8, 123–132. [Google Scholar] [CrossRef] [PubMed]
- Golalipour, M.J.; Kafshgiri, S.K.; Ghafari, S. Gestational diabetes induced neuronal loss in CA1 and CA3 subfields of rat hippocampus in early postnatal life. Folia Morphol. 2012, 71, 71–77. [Google Scholar] [PubMed]
- Lotfi, N.; Hami, J.; Hosseini, M.; Haghir, D.; Haghir, H. Diabetes during pregnancy enhanced neuronal death in the hippocampus of rat offspring. Int. J. Dev. Neurosci. 2016, 51, 28–35. [Google Scholar] [CrossRef]
- Schoenfeld, T.J.; McCausland, H.C.; Morris, H.D.; Padmanaban, V.; Cameron, H.A. Stress and Loss of Adult Neurogenesis Differentially Reduce Hippocampal Volume. Biol. Psychiatry 2017, 82, 914–923. [Google Scholar] [CrossRef]
- Kumar, R.S.; Narayanan, S.N.; Kumar, N.; Nayak, S. Exposure to Enriched Environment Restores Altered Passive Avoidance Learning and Ameliorates Hippocampal Injury in Male Albino Wistar Rats Subjected to Chronic Restraint Stress. Int. J. Appl. Basic Med. Res. 2018, 8, 231–236. [Google Scholar]
- Baran, S.E.; Campbell, A.M.; Kleen, J.K.; Foltz, C.H.; Wright, R.L.; Diamond, D.M.; Conrad, C.D. Combination of high fat diet and chronic stress retracts hippocampal dendrites. Neuroreport 2005, 16, 39–43. [Google Scholar] [CrossRef]
- Guo, A.C.; Jewells, V.L.; Provenzale, J.M. Analysis of normal-appearing white matter in multiple sclerosis: Comparison of diffusion tensor MR imaging and magnetization transfer imaging. AJNR Am. J. Neuroradiol. 2001, 22, 1893–1900. [Google Scholar] [PubMed]
- Pierpaoli, C.; Barnett, A.; Pajevic, S.; Chen, R.; Penix, L.R.; Virta, A.; Basser, P. Water diffusion changes in Wallerian degeneration and their dependence on white matter architecture. Neuroimage 2001, 13, 1174–1185. [Google Scholar] [CrossRef] [PubMed]
- Horsfield, M.A.; Jones, D.K. Applications of diffusion-weighted and diffusion tensor MRI to white matter diseases—A review. NMR Biomed. 2002, 15, 570–577. [Google Scholar] [CrossRef] [PubMed]
- Werring, D.J.; Brassat, D.; Droogan, A.G.; Clark, C.A.; Symms, M.R.; Barker, G.J.; MacManus, D.G.; Thompson, A.J.; Miller, D.H. The pathogenesis of lesions and normal-appearing white matter changes in multiple sclerosis: A serial diffusion MRI study. Brain 2000, 123, 1667–1676. [Google Scholar] [CrossRef] [PubMed]
- Wieshmann, U.C.; lark, C.A.C.; Symms, M.R.; Barker, G.J.; Birnie, K.D.; Shorvon, S.D. Water diffusion in the human hippocampus in epilepsy. Magn. Reson. Imaging 1999, 17, 29–36. [Google Scholar] [CrossRef]
- Yoo, S.Y.; Chang, K.-H.; Song, I.C.; Han, M.H.; Kwon, B.J.; Lee, S.H.; Yu, I.K.; Chun, C.-K. Apparent diffusion coefficient value of the hippocampus in patients with hippocampal sclerosis and in healthy volunteers. AJNR Am. J. Neuroradiol. 2002, 23, 809–812. [Google Scholar]
- Schwartz, E.D.; Cooper, E.T.; Fan, Y.; Jawad, A.F.; Chin, C.-L.; Nissanov, J.; Hackney, D.B. MRI diffusion coefficients in spinal cord correlate with axon morphometry. Neuroreport 2005, 16, 73–76. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhang, J.; Oishi, K.; Faria, A.V.; Jiang, H.; Li, X.; Akhter, K.; Rosa-Neto, P.; Pike, G.B.; Evans, A.; et al. Atlas-guided tract reconstruction for automated and comprehensive examination of the white matter anatomy. Neuroimage 2010, 52, 1289–1301. [Google Scholar] [CrossRef]
- Lebel, C.; Walker, L.; Leemans, A.; Phillips, L.; Beaulieu, C. Microstructural maturation of the human brain from childhood to adulthood. NeuroImage 2008, 40, 1044–1055. [Google Scholar] [CrossRef]
- Bava, S.; Thayer, R.; Jacobus, J.; Ward, M.; Jernigan, T.L.; Tapert, S.F. Longitudinal characterization of white matter maturation during adolescence. Brain Res. 2010, 1327, 38–46. [Google Scholar] [CrossRef]
- Suzuki, Y.; Matsuzawa, H.; Kwee, I.L.; Nakada, T. Absolute eigenvalue diffusion tensor analysis for human brain maturation. NMR Biomed. 2003, 16, 257–260. [Google Scholar] [CrossRef]
- Kumar, R.; Nguyen, H.D.; Macey, P.M.; Woo, M.A.; Harper, R.M. Regional brain axial and radial diffusivity changes during development. J. Neurosci. Res. 2012, 90, 346–355. [Google Scholar] [CrossRef]
- Bockhorst, K.H.; Narayana, P.A.; Liu, R.; Ahobila-Vijjula, P.; Ramu, J.; Kamel, M.; Wosik, J.; Bockhorst, T.; Hahn, K.; Hasan, K.M.; et al. Early postnatal development of rat brain: In vivo diffusion tensor imaging. J. Neurosci. Res. 2008, 86, 1520–1528. [Google Scholar] [CrossRef]
- Zhang, H.; Schneider, T.; Wheeler-Kingshott, C.A.; Alexander, D.C. NODDI: Practical in vivo neurite orientation dispersion and density imaging of the human brain. NeuroImage 2012, 61, 1000–1016. [Google Scholar] [CrossRef]
- Tucker, K.L. Assessment of usual dietary intake in population studies of gene—Diet interaction. Nutr. Metab. Cardiovasc. Dis. 2007, 17, 74–81. [Google Scholar] [CrossRef]
- Moshfegh, A.J.; Rhodes, D.G.; Baer, D.J.; Murayi, T.; Clemens, J.C.; Rumpler, W.V.; Paul, D.R.; Sebastian, R.S.; Kuczynski, K.J.; Ingwersen, L.A.; et al. The US Department of Agriculture Automated Multiple-Pass Method reduces bias in the collection of energy intakes. Am. J. Clin. Nutr. 2008, 88, 324–332. [Google Scholar] [CrossRef]
- Foster, E.; Bradley, J. Methodological considerations and future insights for 24-hour dietary recall assessment in children. Nutr. Res. 2018, 51, 1–11. [Google Scholar] [CrossRef]
- Herrick, K.A.; Rossen, L.; Parsons, R.; Dodd, K. Estimating usual dietary intake from National Health and Nutrition Examination Survey data using the National Cancer Institute method. Natl. Cent. Health Stat. 2018, 178, 1–63. [Google Scholar]
- Vos, M.B.; Kaar, J.L.; Welsh, J.A.; Van Horn, L.V.; Feig, D.I.; Anderson, C.A.M.; Patel, M.J.; Munos, J.C.; Krebs, N.F.; Xanthakos, S.A.; et al. Added Sugars and Cardiovascular Disease Risk in Children. Circulation 2017, 135, e1017–e1034. [Google Scholar] [CrossRef]
| Mean (SD) or N (%) 1 | Range | |
|---|---|---|
| Age, years | 8.55 (1.03) | 7.33–11.34 |
| BMI, kg/m2 | 19.00 (4.12) | 13.62–34.01 |
| BMI percentile | 69.96 (27.33) | 5.28–99.58 |
| BMI z-score | 0.77 (1.08) | −1.78–2.64 |
| BMI category | Healthy-weight: 61 (59%) Overweight: 16 (16%) Obese: 26 (25%) | |
| Sex | Boys: 41 (40%) Girls: 62 (60%) | |
| Tanner Stage of Pubertal Development | Tanner stage 1: 94 (91%) Tanner stage 2: 5 (5%) Tanner stage 3: 3 (3%) Tanner stage 4: 1 (1%) | |
| Energy Intake (kcal) | 1763 (359) | 825–2708 |
| Percent Calories from Added Sugar (%) | 13.91 (6.89) | 2.65–39.90 |
| Percent Calories from Glucose (%) | 4.32 (1.81) | 1.21–8.40 |
| Percent Calories from Fructose (%) | 4.57 (2.19) | 0.93–11.44 |
| Mean (SD) or N (%) 1 | |
|---|---|
| Maternal education 2 | LN: 21 (20%) SC: 29 (28%) CN: 51 (50%) |
| Mother’s race/ethnicity | Hispanic: 59 (57%) Black: 11 (11%) Non-Hispanic White: 20 (19%) Other: 13 (13%) |
| Family income 2 | 0–$30 K: 10 (10%) $30 K–50 K: 29 (29%) $50 K–70 K: 33 (33%) $70 K–90 K: 14 (14%) ≥$90 K: 15 (15%) |
| Predictor Variables | Model 1 ß (sr) | Model 2 ß (sr) | Model 3 ß (sr) | Model 4 ß (sr) | Model 5 ß (sr) |
|---|---|---|---|---|---|
| Percent Calories from Fructose | 3.34 (0.25) ** | 2.56 (0.19) * | 2.80 (0.21) * | 2.70 (0.19) * | 3.33 (0.24) ** |
| Age, years | −1.06 (−0.04) | −1.14 (−0.04) | −1.27 (−0.04) | −1.71 (−0.06) | |
| Sex (1, male; 0, female) | 5.17 (0.07) | 5.44 (0.08) | 6.18 (0.08) | 2.52 (0.03) | |
| Intracranial Volume (mm3) | 1.31 × 10−4 (0.49) *** | 1.30 × 10−4 (0.48) *** | 1.34 × 10−4 (0.47) *** | 1.24 × 10−4 (0.43) *** | |
| BMI z-score | 3.13 (0.11) | 3.05 (0.11) | 5.80 (0.20) * | ||
| Family income (1: <$30 K; 5: >$90 K) | −1.67 (−0.01) | −1.90 (−0.07) | |||
| Mom’s education (CN) | |||||
| LN | 3.24 (0.04) | 2.56 (0.03) | |||
| SC | 2.01 (0.03) | 1.81 (0.03) | |||
| Maternal GDM (1, yes; 0, no) | 4.29 (0.07) | ||||
| Maternal pre-pregnancy BMI, kg/m2 | −1.31 (−0.28) *** | ||||
| R2 | 0.064 | 0.365 | 0.378 | 0.380 | 0.459 |
| ∆R2 | 0.301 | 0.013 | 0.002 | 0.079 | |
| ∆F | 16.78 *** | 2.13 | 0.11 | 6.56 ** |
| Predictor Variables | Model 1 ß (sr) | Model 2 ß (sr) | Model 3 ß (sr) | Model 4 ß (sr) | Model 5 ß (sr) |
|---|---|---|---|---|---|
| Percent Calories from Fructose | 2.51 × 10−6 (0.21) * | 2.66 × 10−6 (0.22) * | 2.79 × 10−6 (0.23) * | 3.51 × 10−6 (0.28) ** | 3.64 × 10−6 (0.29) ** |
| Age, years | −7.52 × 10−6 (−0.28) ** | −7.50 × 10−6 (−0.28) ** | −6.78 × 10−6 (−0.25) ** | −6.95 × 10−6 (−0.26) ** | |
| Sex (1, male; 0, female) | −9.79 × 10−6 (−0.19) | -9.82 × 10−6 (−0.19) | −8.65 × 10−6 (−0.17) | −8.37 × 10−6 (−0.16) | |
| BMI z-score | 1.67 × 10−6 (0.07) | 1.68 × 10−6 (0.07) | 2.40 × 10−6 (0.10) | ||
| Family income (1: <$30 K; 5: >$90 K) | 6.71 × 10−6 (0.29) ** | 6.56 × 10−6 (0.28) ** | |||
| Mom’s education (CN) | |||||
| LN | 3.64 × 10−6 (0.05) | 5.09 × 10−6 (0.07) | |||
| SC | 4.69 × 10−6 (0.08) | 5.67 × 10−6 (0.09) | |||
| Maternal GDM (1, yes; 0, no) | −3.99 × 10−6 (−0.08) | ||||
| Maternal pre-pregnancy BMI, kg/m2 | −3.51 × 10−7 (−0.09) | ||||
| R2 | 0.044 | 0.152 | 0.157 | 0.243 | 0.257 |
| ∆R2 | 0.108 | 0.005 | 0.086 | 0.014 | |
| ∆F | 6.87 ** | 0.57 | 3.42 * | 0.83 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Clark, K.A.; Alves, J.M.; Jones, S.; Yunker, A.G.; Luo, S.; Cabeen, R.P.; Angelo, B.; Xiang, A.H.; Page, K.A. Dietary Fructose Intake and Hippocampal Structure and Connectivity during Childhood. Nutrients 2020, 12, 909. https://doi.org/10.3390/nu12040909
Clark KA, Alves JM, Jones S, Yunker AG, Luo S, Cabeen RP, Angelo B, Xiang AH, Page KA. Dietary Fructose Intake and Hippocampal Structure and Connectivity during Childhood. Nutrients. 2020; 12(4):909. https://doi.org/10.3390/nu12040909
Chicago/Turabian StyleClark, Kristi A., Jasmin M. Alves, Sabrina Jones, Alexandra G. Yunker, Shan Luo, Ryan P. Cabeen, Brendan Angelo, Anny H. Xiang, and Kathleen A. Page. 2020. "Dietary Fructose Intake and Hippocampal Structure and Connectivity during Childhood" Nutrients 12, no. 4: 909. https://doi.org/10.3390/nu12040909
APA StyleClark, K. A., Alves, J. M., Jones, S., Yunker, A. G., Luo, S., Cabeen, R. P., Angelo, B., Xiang, A. H., & Page, K. A. (2020). Dietary Fructose Intake and Hippocampal Structure and Connectivity during Childhood. Nutrients, 12(4), 909. https://doi.org/10.3390/nu12040909





