Comparison of Structured Nutrition Therapy for Ramadan with Standard Care in Type 2 Diabetes Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
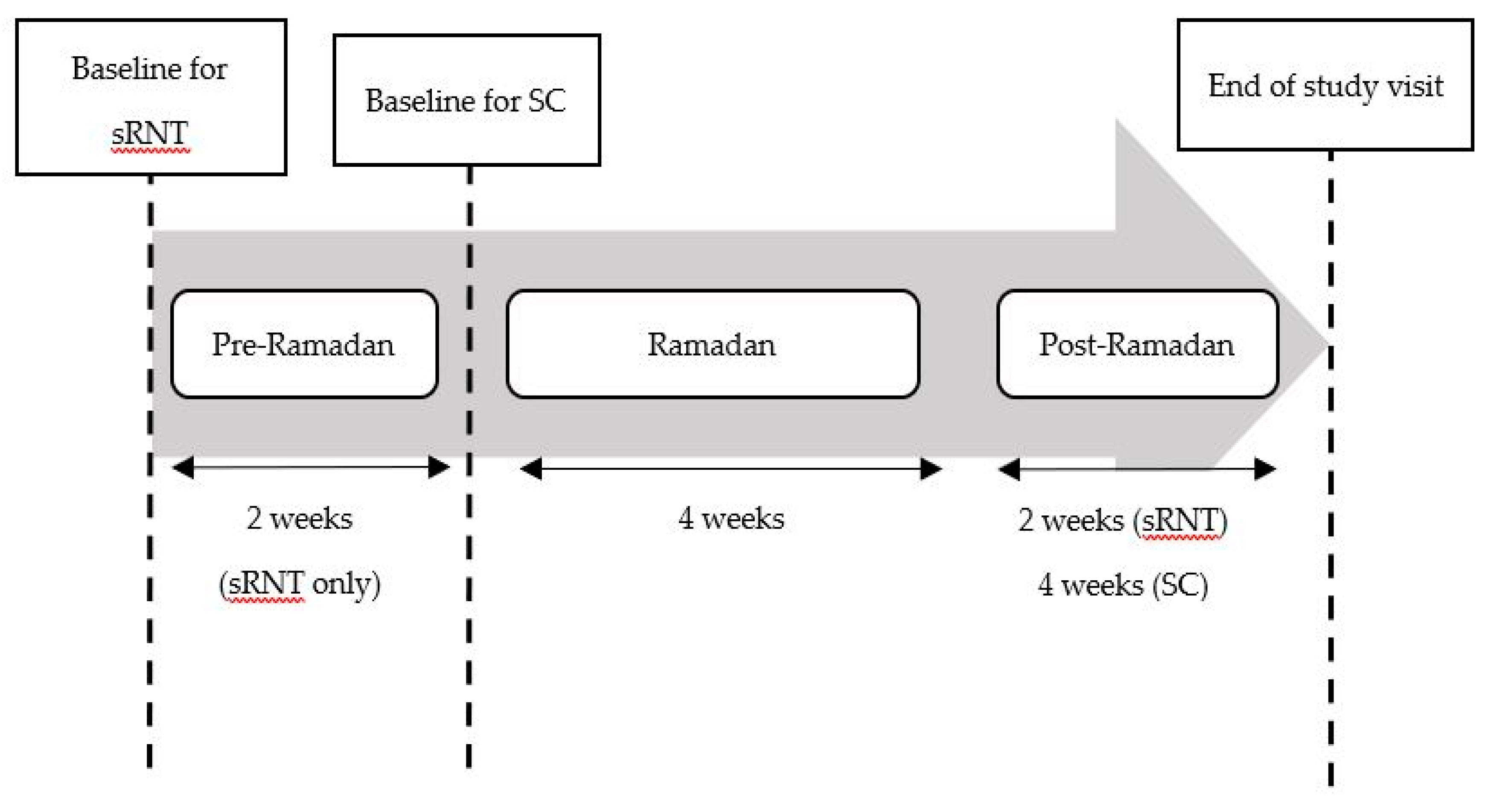
2.2. Study Design
2.3. Study Procedures
2.3.1. Structured Ramadan Nutrition Therapy Group
2.3.2. Standard Care Group
2.4. Outcome Measurements
2.5. Sample Size
2.6. Statistical Analyses
3. Results
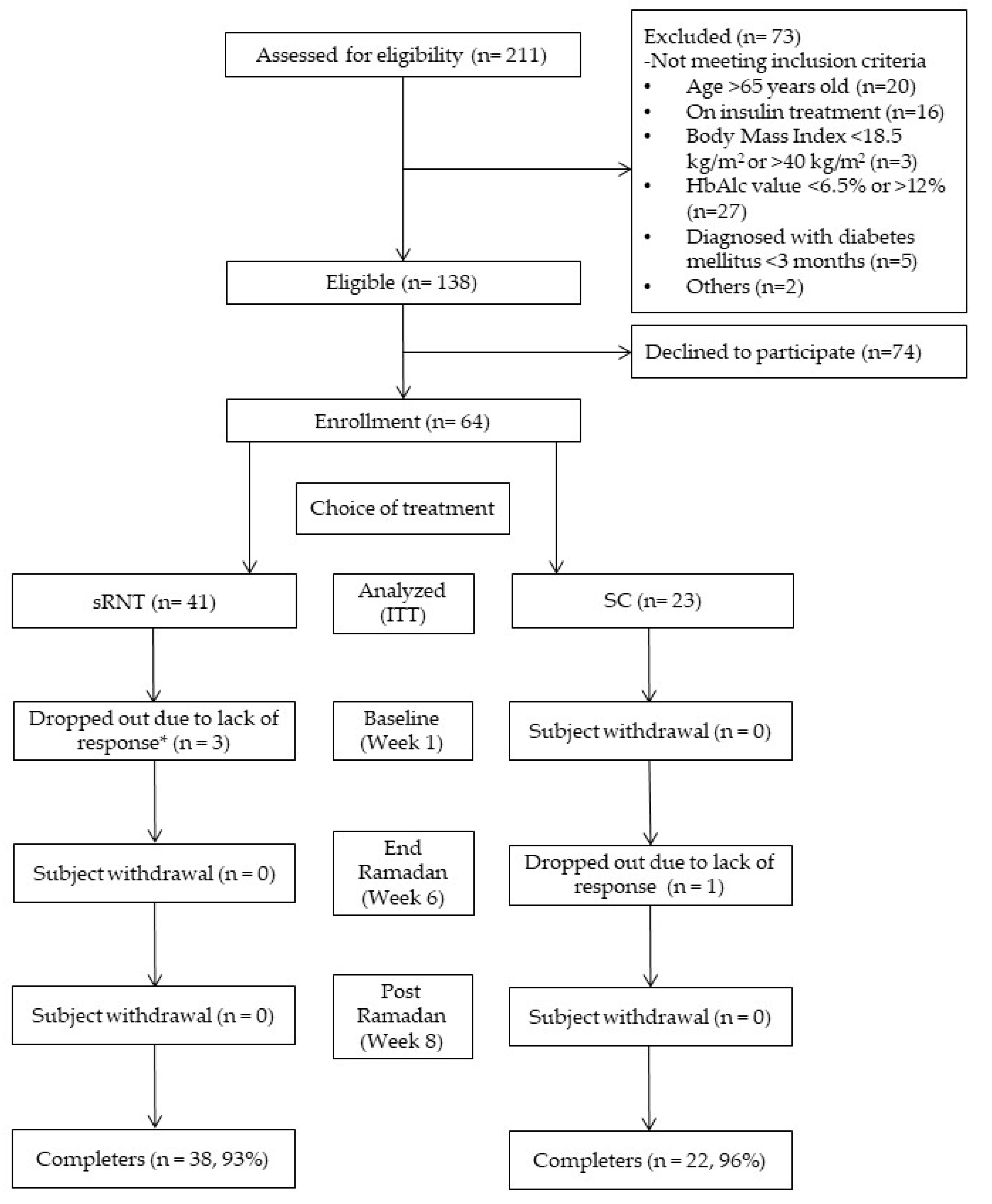
3.1. Recruitment and Baseline Characteristics
3.2. Clinical Outcomes
3.3. Dietary Intake and Quality of Life (QoL)
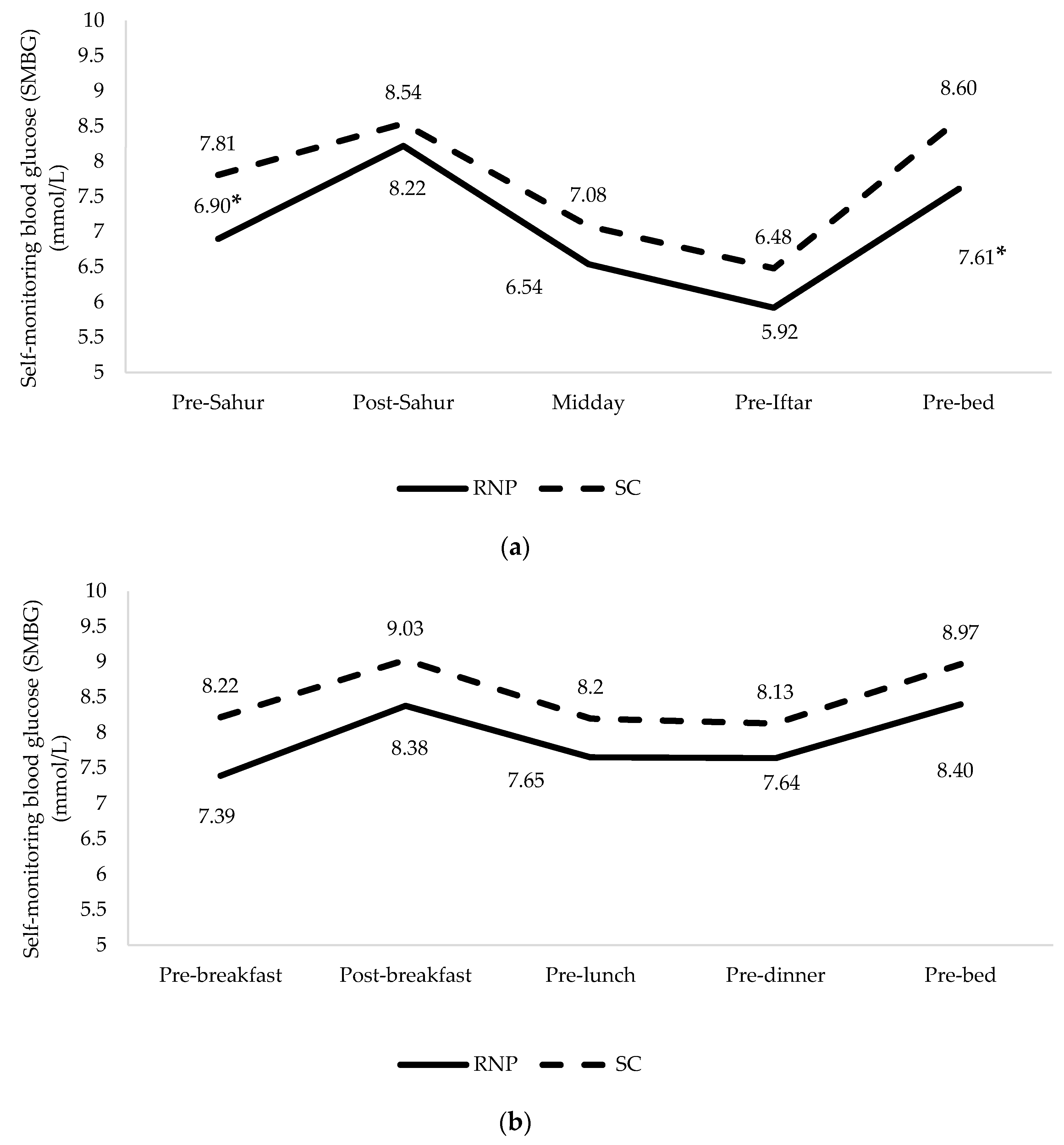
3.4. Self-monitoring Blood Glucose Profiles
3.5. Continuous Glucose Monitoring Profiles
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Hassanein, M.M.; Al-Arouj, M.; Hamdy, O.; Bebakar, W.M.W.; Jabbar, A.; Al-Madani, A.; Hanif, W.; Lessan, N.; Basit, A.; Tayeb, K.; et al. Diabetes and Ramadan: Practical guidelines. Diabetes Res. Clin. Pract. 2017, 126, 303–316. [Google Scholar] [CrossRef]
- Al-Arouj, M.; Assaad-Khalil, S.; Buse, J.B.; Fahdil, I.; Fahmy, M.; Hafez, S.; Hassanein, M.; Ibrahim, M.; Kendall, D.; Kishawi, S.; et al. Recommendations for Management of Diabetes During Ramadan. Diabetes Care 2010, 33, 1895–1902. [Google Scholar] [CrossRef]
- Jabbar, A.; Hassanein, M.M.; Beshyah, S.A.; Boye, K.S.; Yu, M.; Babineaux, S.M. CREED study: Hypoglycaemia during Ramadan in individuals with Type 2 diabetes mellitus from three continents. Diabetes Res. Clin. Pract. 2017, 132, 19–26. [Google Scholar] [CrossRef]
- Bravis, V.; Hui, E.; Salih, S.; Mehar, S.; Hassanein, M.; Devendra, D. Ramadan Education and Awareness in Diabetes (READ) programme for Muslims with Type 2 diabetes who fast during Ramadan. Diabet. Med. 2010, 27, 327–331. [Google Scholar] [CrossRef]
- Yarahmadi, S.; Larijani, B.; Bastanhagh, M.H.; Pajouhi, M.; Jalili, R.B.; Zahedi, F.; Zendehdel, K.; Akrami, S.M. Metabolic and clinical effects of Ramadan fasting in patients with type II diabetes. JCPSP 2003, 13, 329–332. [Google Scholar]
- International Diabetes Federation and the DAR International Alliance. Diabetes and Ramadan: Practical Guidelines; International Diabetes Federation: Brussels, Belgium, 2016. [Google Scholar]
- Chee, W.; Singh, H.K.G.; Hamdy, O.; Mechanick, J.I.; Lee, V.K.M.; Barua, A.; Ali, S.Z.M.; Hussein, Z. Structured lifestyle intervention based on a trans-cultural diabetes-specific nutrition algorithm (tDNA) in individuals with type 2 diabetes: A randomized controlled trial. BMJ Open Diabetes Res. Care 2017, 5, e000384. [Google Scholar] [CrossRef] [PubMed]
- The Look AHEAD Study: A Description of the Lifestyle Intervention and the Evidence Supporting It*. Obes. 2006, 14, 737–752. [CrossRef] [PubMed]
- Mottalib, A.; Abrahamson, M.J.; Pober, D.M.; Polak, R.; Eldib, A.; Tomah, S.; Ashrafzadeh, S.; Hamdy, O. Effect of diabetes-specific nutrition formulas on satiety and hunger hormones in patients with type 2 diabetes. Nutr. Diabetes 2019, 9, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Hassanein, M.M.; Abdelgadir, E.; Bashier, A.; Rashid, F.; Al Saeed, M.; Khalifa, A.; Eltayb, F.; Abuelkheir, S.; Abdellatif, M.; Sayyah, F.; et al. The role of optimum diabetes care in form of Ramadan focused diabetes education, flash glucose monitoring system and pre-Ramadan dose adjustments in the safety of Ramadan fasting in high risk patients with diabetes. Diabetes Res. Clin. Pract. 2019, 150, 288–295. [Google Scholar] [CrossRef] [PubMed]
- Alawadi, F.; Rashid, F.; Bashier, A.; Abdelgadir, E.; Al Saeed, M.; Abuelkheir, S.; Khalifa, A.; Al Sayyah, F.; Bachet, F.; Elsayed, M.; et al. The use of Free Style Libre Continues Glucose Monitoring (FSL-CGM) to monitor the impact of Ramadan fasting on glycemic changes and kidney function in high-risk patients with diabetes and chronic kidney disease stage 3 under optimal diabetes care. Diabetes Res. Clin. Pract. 2019, 151, 305–312. [Google Scholar] [CrossRef] [PubMed]
- Bashier, A.; Khalifa, A.; Al Awadi, F.F.; Alsayyah, F.; Al Saeed, M.; Rashid, F.; Abdelgadir, E.; Bachet, F.; Abuelkheir, S.; Elsayed, M.; et al. Impact of optimum diabetes care on the safety of fasting in Ramadan in adult patients with type 2 diabetes mellitus on insulin therapy. Diabetes Res. Clin. Pract. 2019, 150, 301–307. [Google Scholar] [CrossRef] [PubMed]
- Abdelgadir, E.; Rashid, F.; Bashier, A.; Al Saeed, M.; Khalifa, A.; Al Awadi, F.F.; Hassanein, M. Use of flash glucose monitoring system in assessing safety of the SGLT2 inhibitors during Ramadan fasting in high risk insulin treated patients with type 2 diabetes. Diabetes Metab. Syndr. Clin. Res. Rev. 2019, 13, 2927–2932. [Google Scholar] [CrossRef] [PubMed]
- El Toony, L.F.; Hamad, D.A.; Omar, O.M. Outcome of focused pre-Ramadan education on metabolic and glycaemic parameters in patients with type 2 diabetes mellitus. Diabetes Metab. Syndr. Clin. Res. Rev. 2018, 12, 761–767. [Google Scholar] [CrossRef] [PubMed]
- The Zimbabwe Hand Jive: A Simple Method of Portion Control. Available online: https://www.umassmed.edu/dcoe/diabetes-education/nutrition/zimbabwe-hand-jive/ (accessed on 2 December 2019).
- Imai, S.; Matsuda, M.; Hasegawa, G.; Fukui, M.; Obayashi, H.; Ozasa, N.; Kajiyama, S. A simple meal plan of ‘eating vegetables before carbohydrate’ was more effective for achieving glycemic control than an exchange-based meal plan in Japanese patients with type 2 diabetes. Asia Pac. J. Clin. Nutr. 2011, 20, 161. [Google Scholar] [PubMed]
- Malaysian Dietitians’ Association. Medical Nutrition Therapy Guidelines for Type 2 Diabetes Mellitus, 2nd ed.; Malaysian Dietitians’ Association and Ministry of Health: Putrajaya, Malaysia, 2013. [Google Scholar]
- Ministry of Health Malaysia. Campaign Quarter Quarter Half, Malaysian Healthy Plate; Nutrition Division, Ministry of Health: Putrajaya, Malaysia, 2017.
- Willett, W. Nutritional Epidemiology, 3rd ed.; Oxford University Press: New York, NY, USA, 2013. [Google Scholar]
- Mafauzy, M.; Mohammed, W.B.; Anum, M.Y.; Zulkifli, A.; Ruhani, A.H. A study of the fasting diabetic patients during the month of Ramadan. Med. J. Malays. 1990, 45, 14–17. [Google Scholar]
- Goldberg, G.R.; Black, A.E.; Jebb, S.A.; Cole, T.J.; Murgatroyd, P.R.; Coward, W.A.; Prentice, A.M. Critical evaluation of energy intake data using fundamental principles of energy physiology: 1. Derivation of cut-off limits to identify under-recording. Eur. J. Clin. Nutr. 1991, 45, 569–581. [Google Scholar]
- Bujang, M.A.; Ismail, M.; Hatta, N.K.; Othman, S.H.; Baharum, N.; Lazim, S.S. Validation of the Malay version of Diabetes Quality of Life (DQOL) questionnaire for adult population with type 2 diabetes mellitus. Malays. J. Med. Sci. 2017, 24, 86–96. [Google Scholar] [CrossRef]
- Battelino, T.; Danne, T.; Bergenstal, R.M.; Amiel, S.A.; Beck, R.; Biester, T.; Bosi, E.; Buckingham, B.A.; Cefalu, W.T.; Close, K.L.; et al. Clinical Targets for Continuous Glucose Monitoring Data Interpretation: Recommendations from the International Consensus on Time in Range. Diabetes Care 2019, 42, 1593–1603. [Google Scholar] [CrossRef]
- Lee, J.Y.; Wong, C.P.; Tan, C.S.S.; Nasir, N.H.; Lee, S.W.H. Telemonitoring in fasting individuals with Type 2 Diabetes Mellitus during Ramadan: A prospective, randomised controlled study. Sci. Rep. 2017, 7, 10119. [Google Scholar] [CrossRef]
- Billingham, S.A.; Whitehead, A.L.; Julious, S.A. An audit of sample sizes for pilot and feasibility trials being undertaken in the United Kingdom registered in the United Kingdom Clinical Research Network database. BMC Med. Res. Methodol. 2013, 13, 104. [Google Scholar] [CrossRef]
- Montori, V.M.; Guyatt, G.H. Intention-to-treat principle. CMAJ 2001, 165, 1339–1341. [Google Scholar] [PubMed]
- Vasan, S.K.; Karol, R.; Mahendri, N.V.; Arulappan, N.; Jacob, J.J.; Thomas, N. A prospective assessment of dietary patterns in Muslim subjects with type 2 diabetes who undertake fasting during Ramadan. Indian J. Endocrinol. Metab. 2012, 16, 552–557. [Google Scholar] [PubMed]
- Sil, A.; Kumar, P.; Kumar, R.; Das, N.K. Selection of control, randomization, blinding, and allocation concealment. Indian Dermatol. Online J. 2019, 10, 601–605. [Google Scholar] [PubMed]
- Atwine, F.; Hultsjö, S.; Albin, B.; Hjelm, K. Health-care seeking behaviour and the use of traditional medicine among persons with type 2 diabetes in south-western Uganda: A study of focus group interviews. Pan Afr. Med. J. 2015, 20, 1–13. [Google Scholar] [CrossRef]
- Finch, G.M.; Day, J.E.; Welch, D.A.; Rogers, P.J. Appetite changes under free-living conditions during Ramadan fasting. Appetite 1998, 31, 159–170. [Google Scholar] [CrossRef]
- Gulati, S.; Misra, A.; Nanda, K.; Pandey, R.M.; Garg, V.; Ganguly, S.; Cheung, L. Efficacy and tolerance of a diabetes specific formula in patients with type 2 diabetes mellitus: An open label, randomized, crossover study. Diabetes Metab. Syndr. Clin. Res. Rev. 2015, 9, 252–257. [Google Scholar] [CrossRef]
- Mottalib, A.; Mohd-Yusof, B.-N.; Shehabeldin, M.; Pober, D.M.; Mitri, J.; Hamdy, O. Impact of diabetes-specific nutritional formulas versus oatmeal on postprandial glucose, insulin, GLP-1 and postprandial lipidemia. Nutrients 2016, 8, 443. [Google Scholar] [CrossRef]
- Ibrahim, M.; Al Magd, M.A.; Annabi, F.A.; Assaad-Khalil, S.; Ba-Essa, E.M.; Fahdil, I.; Karadeniz, S.; Meriden, T.; Misha’L, A.A.; Pozzilli, P.; et al. Recommendations for management of diabetes during Ramadan: Update 2015. BMJ Open Diabetes Res. Care 2015, 3, e000108. [Google Scholar] [CrossRef]
- Green, A.J.; Fox, K.M.; Grandy, S. Self-reported hypoglycemia and impact on quality of life and depression among adults with type 2 diabetes mellitus. Diabetes Res. Clin. Pract. 2012, 96, 313–318. [Google Scholar] [CrossRef]
- Tahara, Y.; Shima, K. The response of GHb to stepwise plasma glucose change over time in diabetic patients. Diabetes Care 1993, 16, 1313–1314. [Google Scholar] [CrossRef]
- Tahara, Y.; Shima, K. Kinetics of HbA1c, glycated albumin, and fructosamine and analysis of their weight functions against preceding plasma glucose level. Diabetes Care 1995, 18, 440–447. [Google Scholar] [CrossRef] [PubMed]
- Hirst, J.A.; Stevens, R.J.; Farmer, A.J. Changes in HbA1c level over a 12-week follow-up in patients with type 2 diabetes following a medication change. PLoS ONE 2014, 9, 1–7. [Google Scholar] [CrossRef] [PubMed]
| Structured Ramadan Nutrition Therapy (sRNT) | Standard Care (SC) |
|---|---|
Received structured Ramadan Nutrition Plan consisting of;
| Continued usual treatment consisting of; |
| sRNT (n = 41) | SC (n = 23) | p-Value | |||
|---|---|---|---|---|---|
| n (%) | Mean ± SD | n (%) | Mean ± SD | ||
| Age (years) | 48 ± 9 | 48 ± 10 | 0.909 | ||
| Male, n (%) | 17 (41.5) | 14 (60.9) | 0.193 | ||
| Duration of diabetes (years) | 6 ± 4 | 4 ± 3 | 0.069 | ||
| Number of co-morbidities | 0.9 ± 0.8 | 0.8 ± 0.8 | 0.799 | ||
| Number of oral diabetes medications | 1.4 ± 0.6 | 1.4 ± 0.7 | 0.600 | ||
| Type of oral diabetes medications | |||||
| Alpa-glucosidase inhibitors | 2 (5.0) | 1 (4.3) | |||
| DPP4 inhibitors | 6 (15.0) | 2 (8.7) | |||
| Metformin | 12 (30.0) | 12 (52.2) | |||
| Sitagliptin plus metformin | 17 (42.5) | 7 (30.4) | |||
| Sulphonylurea | 19 (47.5) | 9 (39.1) | |||
| Previous Ramadan experiences | |||||
| Previous dietician encounter | 19 (46.3) | 12 (52.2) | 0.795 | ||
| Previous Ramadan advice | 7 (17.1) | 4 (17.4) | - | ||
| Hypoglycemia frequency | 4 (9.8) | 1 (4.3) | 0.312 | ||
| Glucose-related outcomes | |||||
| Fasting blood glucose (mmol/L) | 7.82 ± 2.39 | 7.18 ± 2.26 | 0.304 | ||
| HbA1c (%) | 8.1 ± 1.7 | 7.8 ± 1.2 | 0.451 | ||
| Anthropometry | |||||
| Weight (kg) | 78.9 ± 18.2 | 76.2 ± 14.2 | 0.534 | ||
| Body Mass Index (kg/m2) | 30.9 ± 5.8 | 29.1 ± 4.6 | 0.201 | ||
| Waist circumference (cm) | 99.6 ± 12.7 | 94.9 ± 10.5 | 0.134 | ||
| Blood pressure | |||||
| Systolic (mm Hg) | 126 ± 16 | 130 ± 20 | 0.330 | ||
| Diastolic (mm Hg) | 86 ± 9 | 86 ± 11 | 0.970 | ||
| Lipid profiles | |||||
| Total cholesterol (mmol/L) | 4.91 ± 1.18 | 5.09 ± 1.60 | 0.599 | ||
| Triglycerides (mmol/L) | 1.73 ± 1.03 | 1.63 ± 0.90 | 0.694 | ||
| HDL-cholesterol (mmol/L) | 1.44 ± 0.31 | 1.36 ± 0.24 | 0.302 | ||
| LDL- cholesterol (mmol/L) | 2.66 ± 0.94 | 3.00 ± 1.41 | 0.302 | ||
| Energy intake and physical activity | |||||
| Energy intake (kcal/day) | 1472 ± 250 | 1429 ± 374 | 0.624 | ||
| Total physical activity level (MET/minutes/weeks) | 2564.83 ± 2424.44 | 2917.78 ± 2587.97 | 0.587 | ||
| Sitting (MET/minutes/weeks) | 2043.83 ± 909.64 | 2197.30 ± 798.24 | 0.502 | ||
| Quality of life | |||||
| RV-DQOL13 Total score | 29.12 ± 7.72 | 26.83 ± 5.86 | 0.220 | ||
| Variables | n | Baseline | End-Ramadan Visit | Post-Ramadan Visit | Within-Group p-value | Changes at End-Ramadan from Baseline ∆ | Changes at Post Ramadan from Baseline ∆ | Interaction p-Value |
|---|---|---|---|---|---|---|---|---|
| Fasting blood glucose (mmol/L) | 0.020 | |||||||
| sRNT | 41 | 7.82 ± 2.39 | 6.35 ± 1.64 | 6.93 ± 1.91 | <0.001 | −1.47 ± 0.30 * | −0.90 ± 0.32 * | |
| SC | 23 | 7.18 ± 2.26 | 6.94 ± 1.61 | 7.34 ± 1.44 | 0.491 | −0.25 ± 0.40 | 0.15 ± 0.30 | |
| HbA1c (%) | 0.174 | |||||||
| sRNT | 41 | 8.1 ± 1.7 | Not measured | 7.4 ± 1.3 | <0.001 | Not measured | −0.72 ± 0.16 | |
| SC | 23 | 7.8 ± 1.2 | 7.4 ± 1.2 | 0.155 | −0.35 ± 0.24 | |||
| Weight (kg) | 0.845 | |||||||
| sRNT | 41 | 78.9 ± 18.2 | 76.9 ± 18.0 | 77.3 ± 18.2 | <0.001 | −2.05 ± 0.24 | −1.60 ± 0.28 | |
| SC | 23 | 76.2 ± 14.2 | 74.3 ± 13.9 | 74.6 ± 13.8 | <0.001 | −1.87 ± 0.32 | −1.57 ± 0.31 | |
| Body Mass Index (kg/m2) | 0.772 | |||||||
| sRNT | 41 | 30.9 ± 5.8 | 30.1 ± 5.8 | 30.3 ± 5.8 | <0.001 | −0.80 ± 0.10 | −0.64 ± 0.11 | |
| SC | 23 | 29.1 ± 4.6 | 28.4 ± 4.5 | 28.5 ± 4.4 | <0.001 | −0.71 ± 0.12 | −0.60 ± 0.11 | |
| Waist circumference (cm) | 0.604 | |||||||
| sRNT | 41 | 99.6 ± 12.7 | 98.3 ± 13.2 | 96.2 ± 13.1 | <0.001 | −1.33 ± 0.63 | −3.40 ± 0.65 | |
| SC | 23 | 94.9 ± 10.5 | 94.6 ± 11.4 | 92.4 ± 11.0 | 0.018 | −0.30 ± 0.94 | −2.47 ± 0.84 | |
| Systolic blood pressure (mmHg) | 0.886 | |||||||
| sRNT | 41 | 126 ± 16 | 121 ± 14 | 124 ± 10 | 0.140 | −4.56 ± 2.43 | −2.05 ± 2.32 | |
| SC | 23 | 130 ± 20 | 126 ± 15 | 127 ± 18 | 0.229 | −4.35 ± 2.79 | −3.48 ± 2.70 | |
| Diastolic blood pressure (mmHg) | 0.885 | |||||||
| sRNT | 41 | 86 ± 9 | 82 ± 10 | 84 ± 10 | 0.031 | −3.49 ± 1.20 | −1.02 ± 1.31 | |
| SC | 23 | 86 ± 11 | 82 ± 9 | 84 ± 10 | 0.097 | −3.70 ± 1.46 | −2.04 ± 1.89 | |
| Total cholesterol (mmol/L) | 0.641 | |||||||
| sRNT | 41 | 4.91 ± 1.18 | 4.35 ± 0.96 | 4.81 ± 0.94 | <0.001 | −0.55 ± 0.14 | −0.10 ± 0.15 | |
| SC | 23 | 5.09 ± 1.60 | 4.64 ± 1.31 | 4.89 ± 1.35 | 0.135 | −0.46 ± 0.25 | −0.20 ± 0.24 | |
| Triglycerides (mmol/L) | 0.034 | |||||||
| sRNT | 41 | 1.73 ± 1.03 | 1.32 ± 0.57 | 1.52 ± 0.81 | <0.001 | −0.40 ± 0.10 | −0.21 ± 0.08 * | |
| SC | 23 | 1.63 ± 0.90 | 1.59 ±1.24 | 1.83 ± 1.28 | 0.296 | −0.04 ± 0.18 | 0.20 ± 0.17 | |
| HDL-cholesterol (mmol/L) | 0.092 | |||||||
| sRNT | 41 | 1.44 ± 0.31 | 1.34 ± 0.25 | 1.60 ± 0.31 | <0.001 | −0.10 ± 0.02 | 0.16 ± 0.03 | |
| SC | 23 | 1.36 ± 0.24 | 1.32 ± 0.23 | 1.46 ± 0.32 | 0.013 | −0.05 ± 0.04 | 0.10 ± 0.06 | |
| LDL-cholesterol (mmol/L) | 0.481 | |||||||
| sRNT | 40 | 2.66 ± 0.94† | 2.44 ± 0.96 | 2.57 ± 0.89 | 0.093 | −0.24 ± 0.12 | −0.11 ± 0.11 | |
| SC | 23 | 3.00 ± 1.41 | 2.54 ± 0.97 | 2.53 ± 0.96 | 0.174 | −0.33 ± 0.23 | −0.34 ± 0.22 | |
| Dietary intake | ||||||||
| Energy intake (kcal/day) | 0.347 | |||||||
| sRNT | 41 | 1472 ± 250 | 1226 ± 229 | 1354 ± 317 | <0.001 | −246 ± 45 | −118 ± 50 | |
| SC | 23 | 1429 ± 374 | 1234 ± 280 | 1449 ± 375 | 0.038 | −195 ± 90 | 20 ± 103 | |
| Carbohydrate (%) | 0.015 | |||||||
| sRNT | 41 | 55 ± 5 | 53 ± 6 | 51 ± 6 | 0.003 | −2.4 ± 1.1 * | −3.9 ± 1.2 * | |
| SC | 23 | 51 ± 8 | 53 ± 7 | 53 ± 10 | 0.460 | 2.4 ± 2.0 | 2.2 ± 2.3 | |
| Protein (%) | 0.026 | |||||||
| sRNT | 41 | 15 ± 3 | 18 ± 3 | 16 ± 4 | 0.003 | 2.2 ± 0.6 * | 0.9 ± 0.7 | |
| SC | 23 | 16 ± 3 | 16 ± 3 | 16 ± 3 | 0.569 | −0.5 ± 0.8 | −0.8 ± 0.8 | |
| Total fat (%) | 0.163 | |||||||
| sRNT | 41 | 30 ± 5 | 29 ± 5 | 32 ± 5 | 0.004 | −0.5 ± 0.9 | 2.5 ± 0.9 | |
| SC | 23 | 33 ± 7 | 31 ± 5 | 32 ± 9 | 0.571 | −2.0 ± 1.7 | −1.1 ± 2.2 | |
| Total fiber intake (g/day) | 0.014 | |||||||
| sRNT | 41 | 5 ± 2 | 7 ± 2 | 7 ± 4 | <0.001 | 2.79 ± 0.54 | 2.15 ± 0.60 | |
| SC | 23 | 4 ± 3 | 4 ± 2 | 5 ± 3 | 0.588 | −0.01 ± 0.72 | 0.60 ± 0.87 | |
| Quality of life | ||||||||
| Satisfaction domain score | 0.279 | |||||||
| sRNT | 41 | 15.10 ± 3.59 | 11.24 ± 3.88 | 10.83 ± 5.49 | <0.001 | −3.85 ± 0.75 | −4.27 ± 0.96 | |
| SC | 23 | 15.17 ± 3.97 | 13.26 ± 4.11 | 13.04 ± 4.83 | 0.199 | −1.91 ± 0.76 | −2.13 ± 1.45 | |
| Impact domain score | 0.113 | |||||||
| sRNT | 41 | 7.27 ± 3.75 | 6.56 ± 2.83 | 6.90 ± 2.78 | 0.396 | −0.71 ± 0.57 | −0.37 ± 0.66 | |
| SC | 23 | 5.78 ± 1.62 | 6.74 ± 2.20 | 6.83 ± 2.06 | 0.107 | 0.96 ± 0.52 | 1.04 ± 0.57 | |
| Worry domain score | 0.607 | |||||||
| sRNT | 41 | 6.76 ± 2.68 | 6.41 ± 2.72 | 6.59 ± 2.19 | 0.665 | −0.34 ± 0.40 | −0.17 ± 0.38 | |
| SC | 23 | 5.87 ± 2.07 | 5.96 ± 1.64 | 6.22 ± 2.24 | 0.466 | 0.09 ± 0.21 | 0.35 ± 0.36 | |
| Total score | 0.072 | |||||||
| sRNT | 41 | 29.12 ± 7.72 | 24.22 ± 6.83 | 24.32 ± 8.15 | <0.001 | −4.90 ± 1.25 * | −4.81 ± 1.55 | |
| SC | 23 | 26.83 ± 5.86 | 25.96 ± 6.62 | 26.09 ± 4.84 | 0.749 | −0.87 ± 0.95 | −0.74 ± 1.31 |
| Variables | Adjusted Mean [95% CI] | sRNT Versus SC Adjusted Mean Difference [95% CI] | p-Value | |
|---|---|---|---|---|
| sRNT (n = 14) | SC (n = 7) | |||
| Sensor glucose (mmol/L) | 6.85 [6.05; 7.65] | 8.30 [7.17; 9.43] | −1.45 [−2.84; −0.07] | 0.04 |
| Estimated A1c (%) | 5.93 [5.44; 6.42] | 6.84 [6.14; 7.54] | −0.91 [−1.76; −0.05] | 0.04 |
| Time in range | ||||
|
Above range (>8.3 mmol/L (%)) | 16.61 [7.91; 25.31] | 36.21 [23.87; 48.55] | −19.60 [−34.76; −4.44] | 0.01 |
|
In target range (3.9–8.3 mmol/L (%)) | 82.32 [73.88; 90.76] | 61.79 [49.83; 73.75] | 20.53 [5.86; 35.19] | 0.01 |
|
Below range (<3.9 mmol/L (%)) | 1.45 [0.34; 2.56] | 1.52 [−0.06; 3.10] | −0.07 [−2.02; 1.88] | 0.94 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mohd Yusof, B.-N.; Wan Zukiman, W.Z.H.H.; Abu Zaid, Z.; Omar, N.; Mukhtar, F.; Yahya, N.F.; Mohd Shahar, A.S.; Hasbullah, F.Y.; Liu Xin Yi, R.; Marczewska, A.; et al. Comparison of Structured Nutrition Therapy for Ramadan with Standard Care in Type 2 Diabetes Patients. Nutrients 2020, 12, 813. https://doi.org/10.3390/nu12030813
Mohd Yusof B-N, Wan Zukiman WZHH, Abu Zaid Z, Omar N, Mukhtar F, Yahya NF, Mohd Shahar AS, Hasbullah FY, Liu Xin Yi R, Marczewska A, et al. Comparison of Structured Nutrition Therapy for Ramadan with Standard Care in Type 2 Diabetes Patients. Nutrients. 2020; 12(3):813. https://doi.org/10.3390/nu12030813
Chicago/Turabian StyleMohd Yusof, Barakatun-Nisak, Wan Zul Haikal Hafiz Wan Zukiman, Zalina Abu Zaid, Noraida Omar, Firdaus Mukhtar, Nor Farahain Yahya, Aainaa Syarfa Mohd Shahar, Farah Yasmin Hasbullah, Rachel Liu Xin Yi, Agnieszka Marczewska, and et al. 2020. "Comparison of Structured Nutrition Therapy for Ramadan with Standard Care in Type 2 Diabetes Patients" Nutrients 12, no. 3: 813. https://doi.org/10.3390/nu12030813
APA StyleMohd Yusof, B.-N., Wan Zukiman, W. Z. H. H., Abu Zaid, Z., Omar, N., Mukhtar, F., Yahya, N. F., Mohd Shahar, A. S., Hasbullah, F. Y., Liu Xin Yi, R., Marczewska, A., & Hamdy, O. (2020). Comparison of Structured Nutrition Therapy for Ramadan with Standard Care in Type 2 Diabetes Patients. Nutrients, 12(3), 813. https://doi.org/10.3390/nu12030813





