Zinc Burden Evokes Copper Deficiency in the Hypoalbuminemic Hemodialysis Patients
Abstract
1. Introduction
2. Patients and Methods
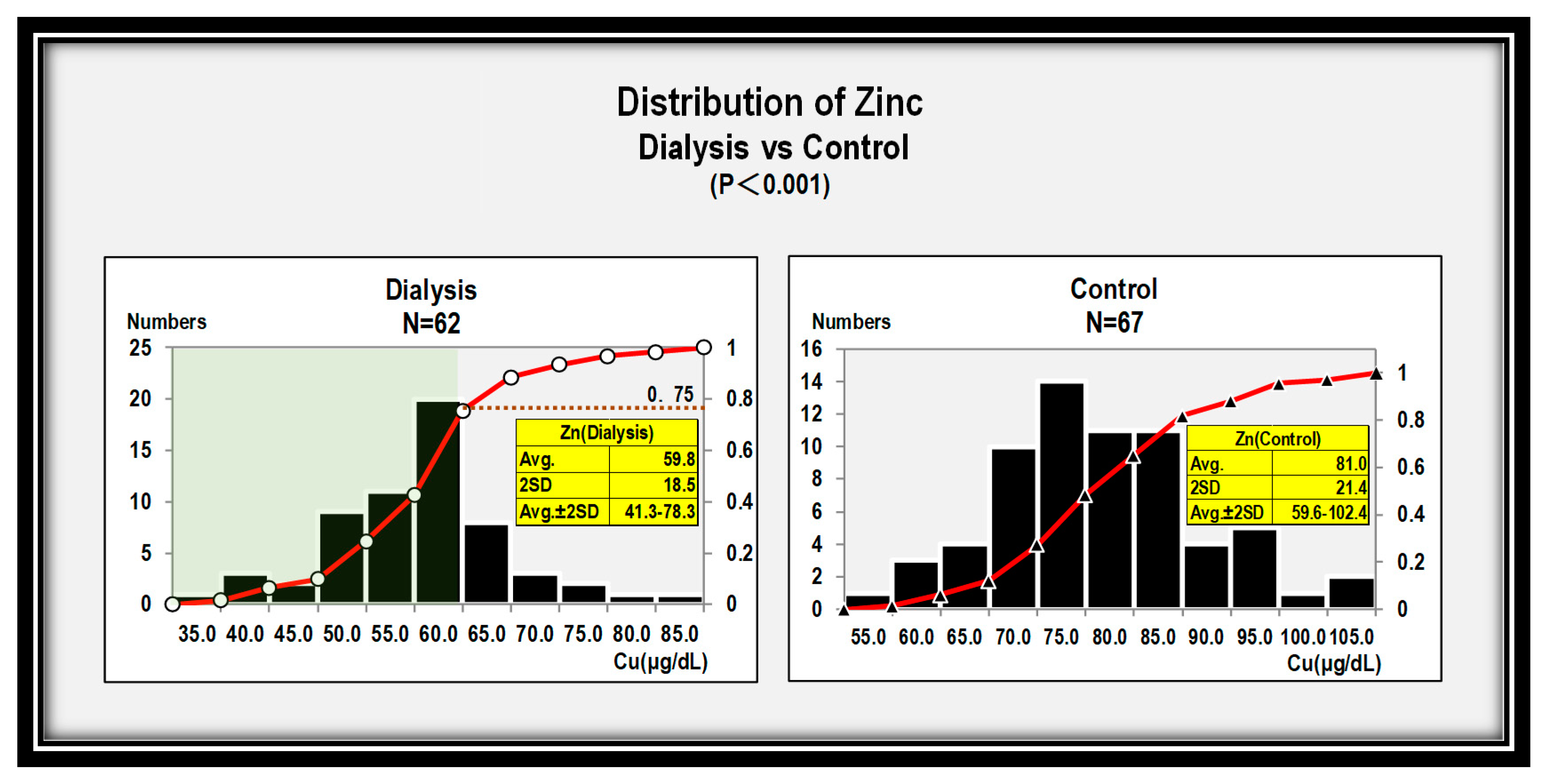
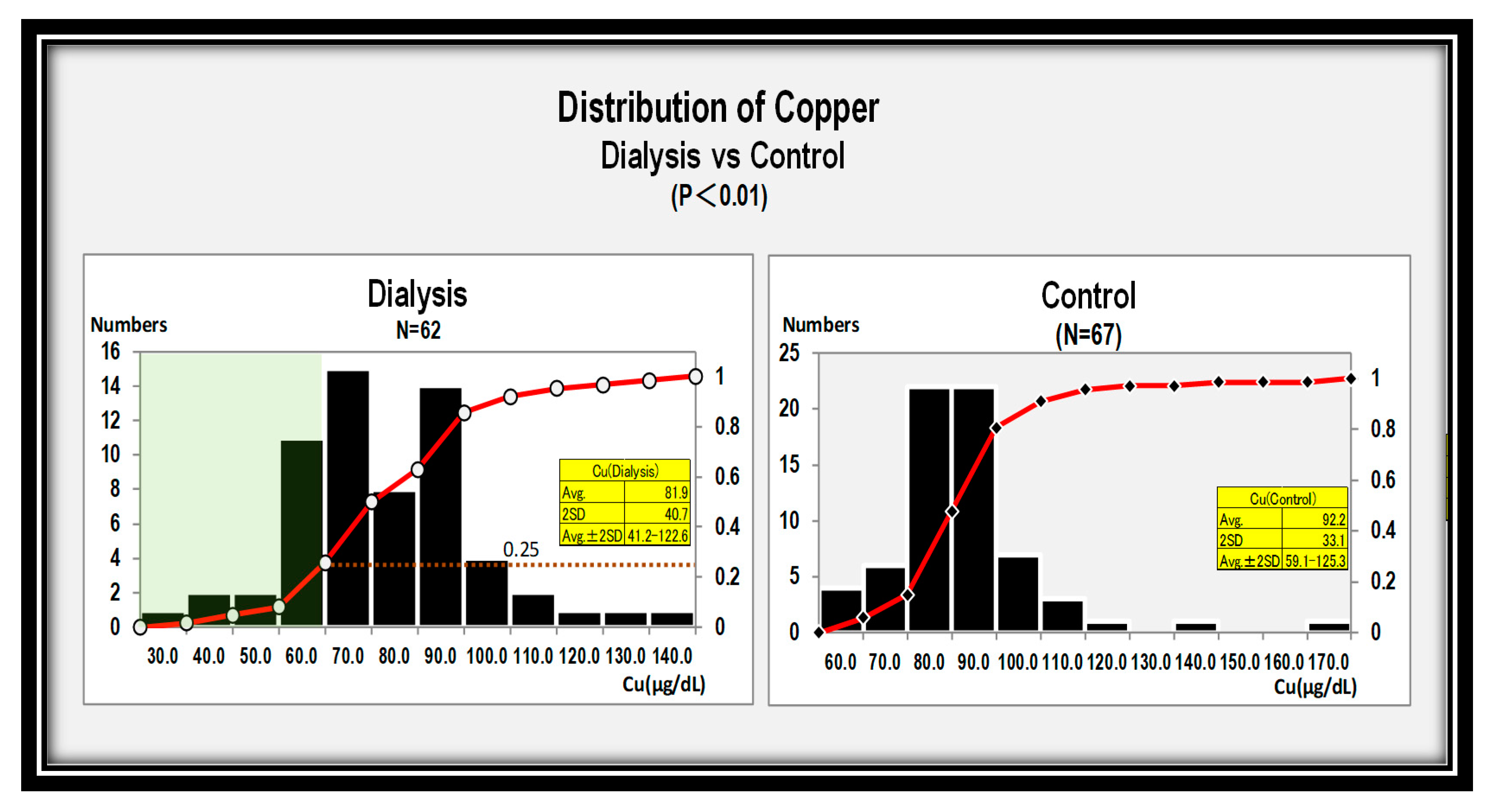
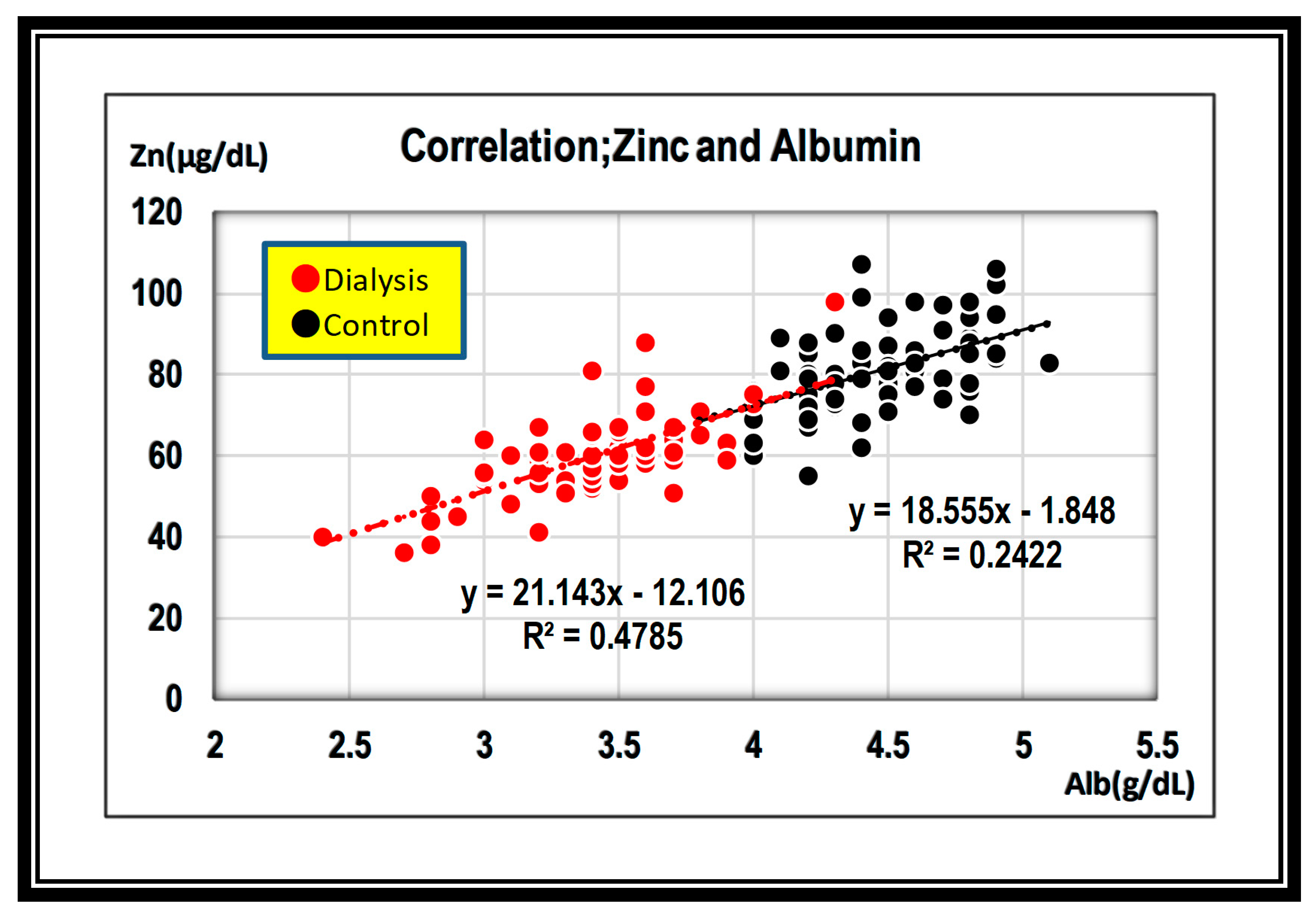
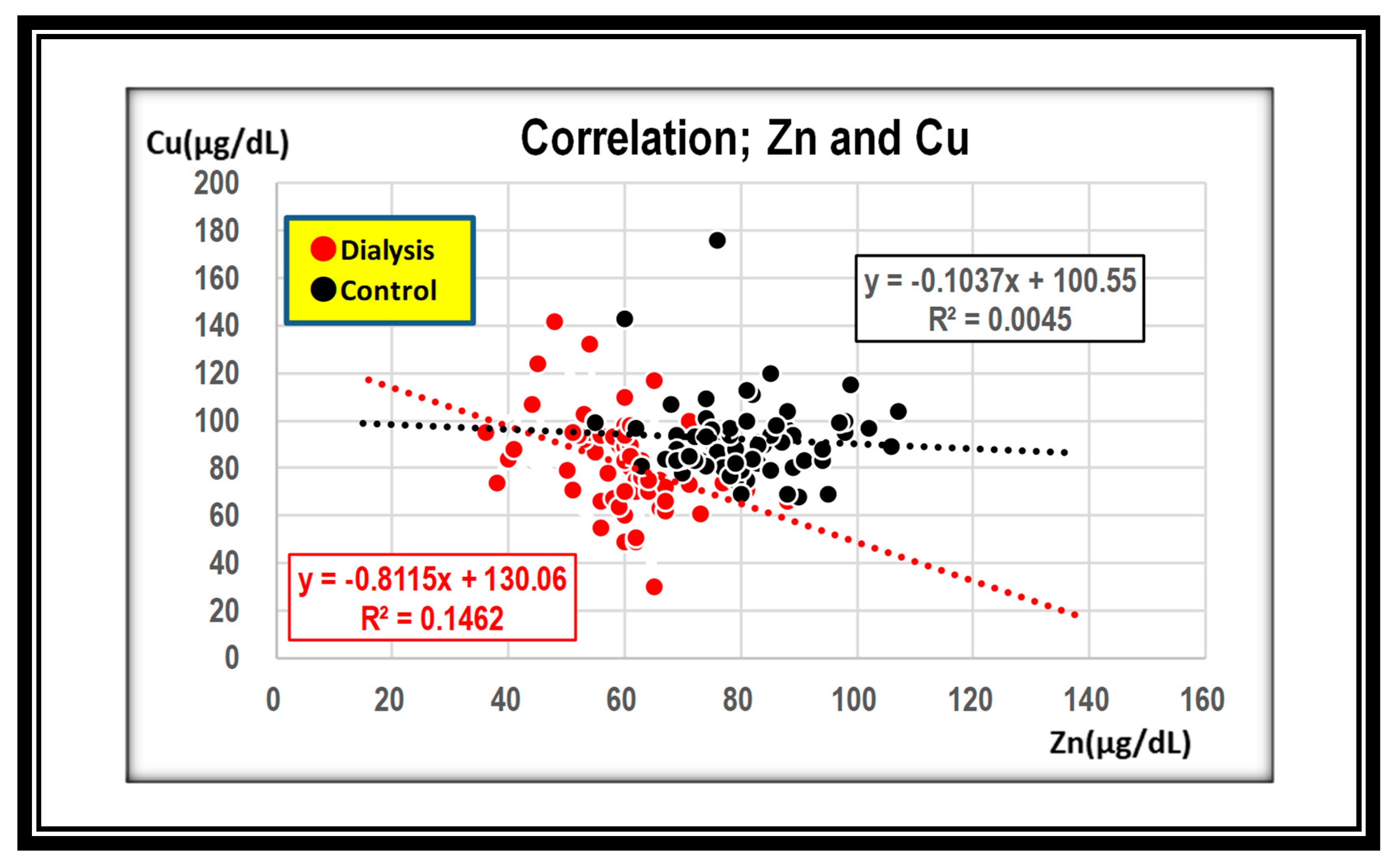
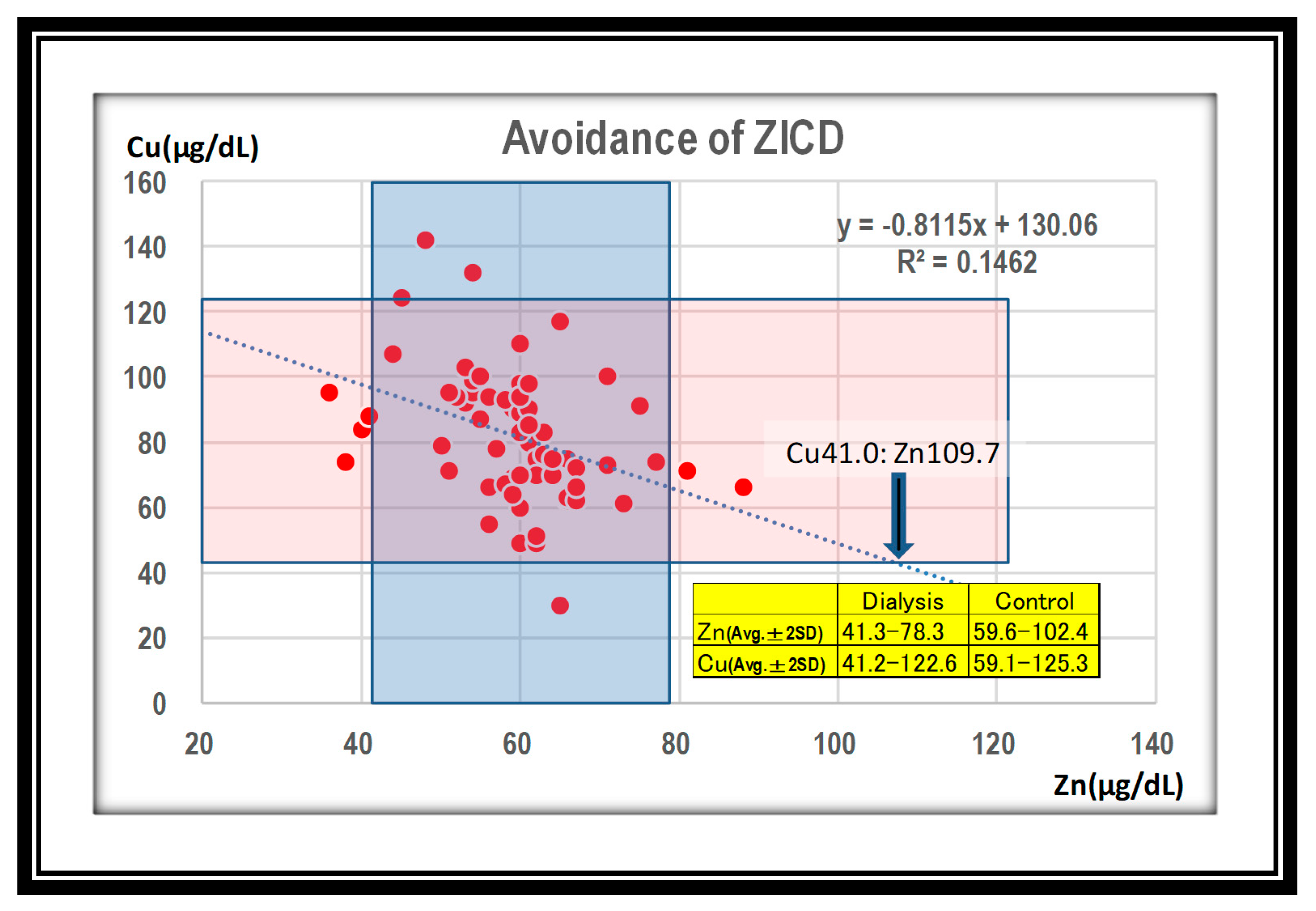
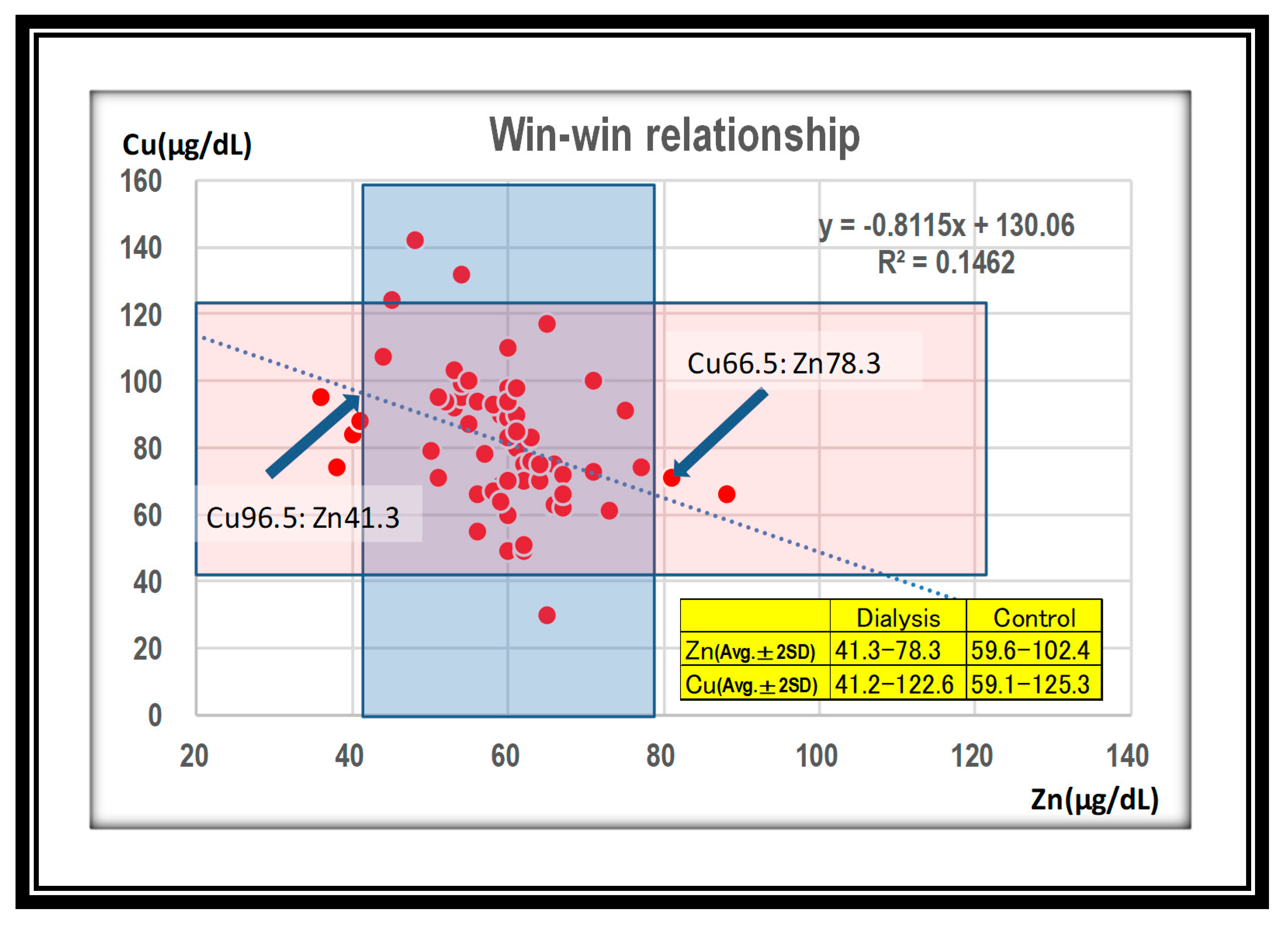
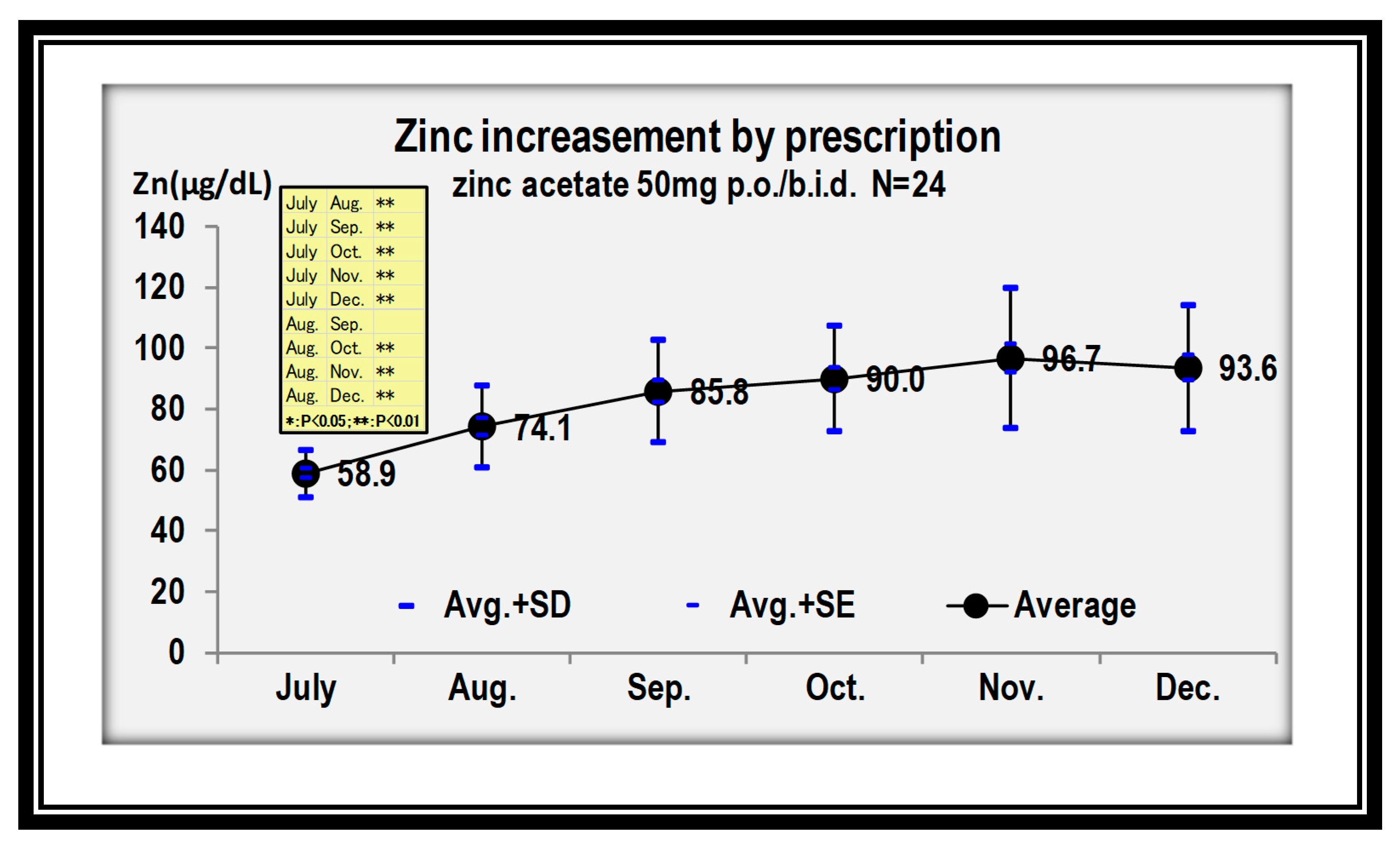
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Prasad, A.S.; Brewer, G.J.; Schoomaker, E.B.; Rabbani, P. Hypocupremia Induced by Zinc Therapy in Adults. JAMA 1978, 240, 2166. [Google Scholar] [CrossRef]
- Lu, J.; Stewart, A.J.; Sadler, P.J.; Pinheiro, T.J.; Blindauer, C.A. Albumin as a zinc carrier: Properties of its high-affinity zinc-binding site. Biochem. Soc. Trans. 2008, 36, 1317–1321. [Google Scholar] [CrossRef]
- Miyata, S.; Okuno, T.; Shimamura, Y.; Miyake, T. Absorption and excertion of zinc in the aged. Nippon. Ronen Igakkai Zasshi. Jpn. J. Geriatr. 1987, 24, 272–277. [Google Scholar] [CrossRef] [PubMed]
- Condon, C.J.; Freeman, R.M. Zinc Metabolism in Renal Failure. Ann. Intern. Med. 1970, 73, 531. [Google Scholar] [CrossRef] [PubMed]
- Abdulla, M. How adequate is plasma zinc as an indicator of zinc status? Prog. Clin. Biol. Res. 1983, 129, 171–183. [Google Scholar] [PubMed]
- Gomi, T.; Yuhara, M.; Nakayama, D.; Kasatani, T.; Ikeda, T.; Saito, M. Zinc metabolism in chronic hemodialysis patients. J. Jpn. Soc. Dial. Ther. 1984, 17, 39–46. [Google Scholar] [CrossRef]
- Duncan, A.; Yacoubian, C.; Watson, N.; Morrison, I. The risk of copper deficiency in patients prescribed zinc supplements. J. Clin. Pathol. 2015, 68, 723–725. [Google Scholar] [CrossRef]
- Duncan, A.; Talwar, D.; Morrison, I. The predictive value of low plasma copper and high plasma zinc in detecting zinc-induced copper deficiency. Ann. Clin. Biochem. Int. J. Lab. Med. 2016, 53, 575–579. [Google Scholar] [CrossRef]
- Hayton, B.A.; Broome, H.E.; Lilenbaum, R.C. Copper deficiency-induced anemia and neutropenia secondary to intestinal malabsorption. Am. J. Hematol. 1995, 48, 45–47. [Google Scholar] [CrossRef]
- Schleper, B.; Stuerenburg, H.J. Copper deficiency-associated myelopathy in a 45-year-old woman. J. Neurol. 2001, 248, 705–706. [Google Scholar] [CrossRef]
- Kumar, N.; Ahlskog, J.E.; Klein, C.J.; Port, J.D. Imaging features of copper deficiency myelopathy: A study of 25 cases. Neuroradiology 2005, 48, 78–83. [Google Scholar] [CrossRef] [PubMed]
- Everett, C.M.; Matharu, M.; Gawler, J. Neuropathy progressing to myeloneuropathy 20 years after partial gastrectomy. Neurology 2006, 66, 1451. [Google Scholar] [CrossRef] [PubMed]
- Halfdanarson, T.R.; Kumar, N.; Phyliky, R.L.; Hogan, W.J.; Li, C.-Y. Hematological manifestations of copper deficiency: A retrospective review. Eur. J. Haematol. 2008, 80, 523–531. [Google Scholar] [CrossRef] [PubMed]
- Jaiser, S.; Winston, G.P. Copper deficiency myelopathy. J. Neurol. 2010, 257, 869–881. [Google Scholar] [CrossRef]
- Gletsu, N.; Broderius, M.; Frediani, J.; Zhao, V.M.; Griffith, D.P.; Davis, S.S.; Sweeney, J.F.; Lin, E.; Prohaska, J.R.; Ziegler, T.R. Incidence and prevalence of copper deficiency following roux-en-y gastric bypass surgery. Int. J. Obes. 2011, 36, 328–335. [Google Scholar] [CrossRef]
- Willis, M.S.; Monaghan, S.A.; Miller, M.L.; McKenna, R.W.; Perkins, W.D.; Levinson, B.S.; Bhushan, V.; Kroft, S.H. Zinc-induced copper defiency: A report of three cases initially recognized on bone marrow examination. Am. J. Clin. Pathol. 2005, 123, 125–131. [Google Scholar] [CrossRef]
- Halfdanarson, T.R.; Kumar, N.; Hogan, W.J.; Murray, J.A. Copper Deficiency in Celiac Disease. J. Clin. Gastroenterol. 2009, 43, 162–164. [Google Scholar] [CrossRef]
- Stec, J.; Podracká, Ľ.; Pavkovčeková, O.; Kollár, J.; Pavkovčeková, O. Zinc and Copper Metabolism in Nephrotic Syndrome. Nephron 1990, 56, 186–187. [Google Scholar] [CrossRef]
- Schlockow, I. Über ein eigenartiges Rückenmarksleiden der Zinkhüttenarbeiter. Dtsch. Med. Wöchensch. 1875, 1, 208–210, 221–222. (In German) [Google Scholar]
- Lanska, D.J.; Remler, B. Myelopathy among zinc-smelter workers in Upper Silesia during the late 19th century. Neurology 2014, 82, 1175–1179. [Google Scholar] [CrossRef]
- Sugiura, T.; Goto, K.; Ito, K.; Ueta, A.; Fujimoto, S.; Togari, H. Chronic zinc toxicity in an infant who received zinc therapy for atopic dermatitis. Acta Paediatr. 2005, 94, 1333–1335. [Google Scholar] [CrossRef] [PubMed]
- Yaldizli, Ö.; Johansson, U.; Gizewski, E.R.; Maschke, M. Copper deficiency myelopathy induced by repetitive parenteral zinc supplementation during chronic hemohemodialysis. J. Neurol. 2006, 253, 1507–1509. [Google Scholar] [CrossRef] [PubMed]
- Nations, S.P.; Boyer, P.J.; Love, L.A.; Burritt, M.F.; Butz, J.A.; Wolfe, G.I.; Hynan, L.; Reisch, J.; Trivedi, J.R. Denture cream: An unusual source of excess zinc, leading to hypocupremia and neurologic disease. Neurology 2008, 71, 639–643. [Google Scholar] [CrossRef] [PubMed]
- Hedera, P.; Peltier, A.; Fink, J.K.; Wilcock, S.; London, Z.; Brewer, G.J. Myelopolyneuropathy and pancytopenia due to copper deficiency and high zinc levels of unknown origin II. The denture cream is a primary source of excessive zinc. NeuroToxicology 2009, 30, 996–999. [Google Scholar] [CrossRef]
- Prodan, C.I.; Holland, N.; Wisdom, P.; Burstein, S.; Bottomley, S. CNS demyelination associated with copper deficiency and hyperzincemia. Neurology 2002, 59, 1453–1456. [Google Scholar] [CrossRef]
- Hedera, P.; Fink, J.K.; Bockenstedt, P.L.; Brewer, G.J. Myelopolyneuropathy and Pancytopenia Due to Copper Deficiency and High Zinc Levels of Unknown Origin. Arch. Neurol. 2003, 60, 1303–1306. [Google Scholar] [CrossRef]
- Kumar, N.; Elliott, M.A.; Hoyer, J.D.; Harper, C.M., Jr.; Ahlskog, J.E.; Phyliky, R.L. “Myelodysplastic syndrome,” myeloneuropathy, and copper deficiency. Mayo. Clin. Proc. 2005, 80, 943–946. [Google Scholar] [CrossRef]
- Tormoehlen, L.M.; Kumar, N. Neurotoxicology: Five new things. Neurol. Clin. Pract. 2012, 2, 301–310. [Google Scholar] [CrossRef]
- Yuzbasiyan-Gurkan, V.; Grider, A.; Nostrant, T.; Cousins, R.J.; Brewer, G.J. Treatment of Wilson’s Disease with Zinc: X. Intestinal Metallothionein Induction. J. Lab. Clin. Med. 1992, 120, 380–386. [Google Scholar]
| Zinc < 60 (μg/dL) N = 27 | Zinc ≧ 60 (μg/dL) N = 38 | ||||
|---|---|---|---|---|---|
| Average | SD | Average | SD | ||
| Age(Y) | 73.9 | 11.9 | 71.0 | 11.6 | |
| Heritage(Y) | 8.5 | 9.3 | 6.0 | 4.2 | |
| T-Cho(mg/dL) | 147.9 | 26.2 | 151.2 | 28.7 | |
| TP(g/dL) | 6.2 | 0.6 | 6.4 | 0.5 | |
| Alb(g/dL) | 3.2 | 0.3 | 3.5 | 0.3 | ※※ |
| CRP(mg/L) | 0.5 | 0.9 | 0.3 | 0.7 | |
| ALP(IU) | 240.7 | 73.4 | 239.6 | 105.9 | |
| WBC(×103) | 5.3 | 1.7 | 5.9 | 2.1 | |
| Hb(g/dL) | 10.4 | 1.0 | 11.1 | 1.1 | |
| MCV(fl) | 93.7 | 6.9 | 94.1 | 5.3 | |
| TSAT(%) | 19.8 | 8.5 | 21.2 | 8.3 | |
| Ferritin(ng/mL) | 71.0 | 55.1 | 77.5 | 67.2 | |
| Cu(μ/dL) | 85.8 | 21.6 | 80.1 | 20.1 | |
| Zn (μg/dL) | 41.3~78.3 |
| Cu (μg/dL) | 66.5~96.5 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nishime, K.; Kondo, M.; Saito, K.; Miyawaki, H.; Nakagawa, T. Zinc Burden Evokes Copper Deficiency in the Hypoalbuminemic Hemodialysis Patients. Nutrients 2020, 12, 577. https://doi.org/10.3390/nu12020577
Nishime K, Kondo M, Saito K, Miyawaki H, Nakagawa T. Zinc Burden Evokes Copper Deficiency in the Hypoalbuminemic Hemodialysis Patients. Nutrients. 2020; 12(2):577. https://doi.org/10.3390/nu12020577
Chicago/Turabian StyleNishime, Keizo, Morihiro Kondo, Kazuhiro Saito, Hisashi Miyawaki, and Takahiko Nakagawa. 2020. "Zinc Burden Evokes Copper Deficiency in the Hypoalbuminemic Hemodialysis Patients" Nutrients 12, no. 2: 577. https://doi.org/10.3390/nu12020577
APA StyleNishime, K., Kondo, M., Saito, K., Miyawaki, H., & Nakagawa, T. (2020). Zinc Burden Evokes Copper Deficiency in the Hypoalbuminemic Hemodialysis Patients. Nutrients, 12(2), 577. https://doi.org/10.3390/nu12020577





