Comparison of Footsteps Using Connected Bracelets with the Timed Up-and-Go Test and the 6-Minutes Walking Test in a Prospective Colorectal Surgery Cohort
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Gustafsson, U.O.; Scott, M.J.; Schwenk, W.; Demartines, N.; Roulin, D.; Francis, N.; McNaught, C.E.; Macfie, J.; Liberman, A.S.; Soop, M.; et al. Guidelines for perioperative care in elective colonic surgery: Enhanced Recovery After Surgery (ERAS(®)) Society recommendations. World J. Surg. 2013, 37, 259–284. [Google Scholar] [CrossRef] [PubMed]
- Wind, J.; Polle, S.W.; Fung Kon Jin, P.H.P.; Dejong, C.H.C.; Von Meyenfeldt, M.F.; Ubbink, D.T.; Gouma, D.J.; Bemelman, W.A. Systematic review of enhanced recovery programmes in colonic surgery. Br. J. Surg. 2006, 93, 800–809. [Google Scholar] [CrossRef] [PubMed]
- Stabenau, H.F.; Becher, R.D.; Gahbauer, E.A.; Leo-Summers, L.; Allore, H.G.; Gill, T.M. Functional Trajectories Before and After Major Surgery in Older Adults. Ann. Surg. 2018, 268, 911–917. [Google Scholar] [CrossRef] [PubMed]
- Gillis, C.; Li, C.; Lee, L.; Awasthi, R.; Augustin, B.; Gamsa, A.; Liberman, A.S.; Stein, B.; Charlebois, P.; Feldman, L.S.; et al. Prehabilitation versus rehabilitation: A randomized control trial in patients undergoing colorectal resection for cancer. Anesthesiology 2014, 121, 937–947. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Carli, F.; Lee, L.; Charlebois, P.; Stein, B.; Liberman, A.S.; Kaneva, P.; Augustin, B.; Wongyingsinn, M.; Gamsa, A.; et al. Impact of a trimodal prehabilitation program on functional recovery after colorectal cancer surgery: A pilot study. Surg. Endosc. 2013, 27, 1072–1082. [Google Scholar] [CrossRef] [PubMed]
- Piraux, E.; Caty, G.; Reychler, G. Effects of preoperative combined aerobic and resistance exercise training in cancer patients undergoing tumour resection surgery: A systematic review of randomised trials. Surg. Oncol. 2018, 27, 584–594. [Google Scholar] [CrossRef] [PubMed]
- ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: Guidelines for the six-minute walk test. Am. J. Respir. Crit. Care Med. 2002, 166, 111–117. [Google Scholar] [CrossRef] [PubMed]
- Bellet, R.N.; Adams, L.; Morris, N.R. The 6-minute walk test in outpatient cardiac rehabilitation: Validity, reliability and responsiveness—A systematic review. Physiotherapy 2012, 98, 277–286. [Google Scholar] [CrossRef] [PubMed]
- Podsiadlo, D.; Richardson, S. The timed ‘Up & Go’: A test of basic functional mobility for frail elderly persons. J. Am. Geriatr. Soc. 1991, 39, 142–148. [Google Scholar]
- Romain, B.; Hubner, M. Postoperative Footsteps and Outcomes—A Pilot Study. General Medicine: Open Access. 2016. Available online: http://www.esciencecentral.org/journals/postoperative-footsteps-and-outcomes--a-pilot-study-2327-5146-1000239.php?aid=72525 (accessed on 13 September 2019).
- Gustafsson, U.O.; Scott, M.J.; Schwenk, W.; Demartines, N.; Roulin, D.; Francis, N.; McNaught, C.E.; Macfie, J.; Liberman, A.S.; Soop, M.; et al. Guidelines for perioperative care in elective rectal/pelvic surgery: Enhanced Recovery After Surgery (ERAS(®)) Society recommendations. World J. Surg. 2013, 37, 285–305. [Google Scholar] [CrossRef]
- Enright, P.L.; Sherrill, D.L. Reference equations for the six-minute walk in healthy adults. Am. J. Respir. Crit. Care Med. 1998, 158, 1384–1387. [Google Scholar] [CrossRef]
- Robinson, T.N.; Wu, D.S.; Sauaia, A.; Dunn, C.L.; Stevens-Lapsley, J.E.; Moss, M.; Stiegmann, G.V.; Gajdos, C.; Cleveland, J.C., Jr.; Inouye, S.K. Slower walking speed forecasts increased postoperative morbidity and 1-year mortality across surgical specialties. Ann. Surg. 2013, 258, 582. [Google Scholar] [CrossRef]
- Cheema, F.N.; Abraham, N.S.; Berger, D.H.; Albo, D.; Taffet, G.E.; Naik, A.D. Novel approaches to perioperative assessment and intervention may improve long-term outcomes after colorectal cancer resection in older adults. Ann. Surg. 2011, 253, 867–874. [Google Scholar] [CrossRef] [PubMed]
- Silver, J.K.; Baima, J. Cancer prehabilitation: An opportunity to decrease treatment-related morbidity, increase cancer treatment options, and improve physical and psychological health outcomes. Am. J. Phys. Med. Rehabil. 2013, 92, 715–727. [Google Scholar] [CrossRef] [PubMed]
- McLennan, E.; Oliphant, R.; Moug, S.J. Limited preoperative physical capacity continues to be associated with poor postoperative outcomes within a colorectal ERAS programme. Ann. R. Coll. Surg. Engl. 2019, 101, 261–267. [Google Scholar] [CrossRef] [PubMed]
- Hughes, M.J.; Hackney, R.J.; Lamb, P.J.; Wigmore, S.J.; Christopher Deans, D.A.; Skipworth, R.J.E. Prehabilitation Before Major Abdominal Surgery: A Systematic Review and Meta-analysis. World J. Surg. 2019, 43, 1661–1668. [Google Scholar] [CrossRef] [PubMed]
- Carli, F.; Charlebois, P.; Stein, B.; Feldman, L.; Zavorsky, G.; Kim, D.J.; Scott, S.; Mayo, N.E. Randomized clinical trial of prehabilitation in colorectal surgery. Br. J. Surg. 2010, 97, 1187–1197. [Google Scholar] [CrossRef] [PubMed]
- Teo, J.Y.K.; Turner, R.; Self, M. Effect of exercise prehabilitation on functional status of patients undergoing bowel resection: A systematic review. ANZ J. Surg. 2020. [Google Scholar] [CrossRef] [PubMed]
- Carli, F.; Bousquet-Dion, G.; Awasthi, R.; Elsherbini, N.; Liberman, S.; Boutros, M.; Stein, B.; Charlebois, P.; Ghitulescu, G.; Morin, N.; et al. Effect of Multimodal Prehabilitation vs Postoperative Rehabilitation on 30-Day Postoperative Complications for Frail Patients Undergoing Resection of Colorectal Cancer: A Randomized Clinical Trial. JAMA Surg. 2020. [Google Scholar] [CrossRef] [PubMed]
| Overall (n = 50) | ||
|---|---|---|
| Age (years) (mean, SD) | 58.7 (18.2) | |
| BMI (kg/m2) (mean, SD) | 25.4 (4.3) | |
| Gender (M: F) | 34:16 | |
| Alcohol consumption | 33 (66%) | |
| Active smoking | 19 (38%) | |
| Cardiovascular disease | 19 (38%) | |
| Chronic pulmonary disease | 7 (14%) | |
| Diabetes | 6 (12%) | |
| ASA score (I–II: III–IV) | 43:7 | |
| Preoperative physical activity | ||
| None | 16 (32%) | |
| Mild | 28 (56%) | |
| Intensive | 6 (12%) | |
| Malignancy | 27 (54%) | |
| Surgical procedure | ||
| Colon | 38 (76%) | |
| Rectum | 7 (14%) | |
| Other | 5 (10%) | |
| Minimally invasive approach | 44 (88%) | |
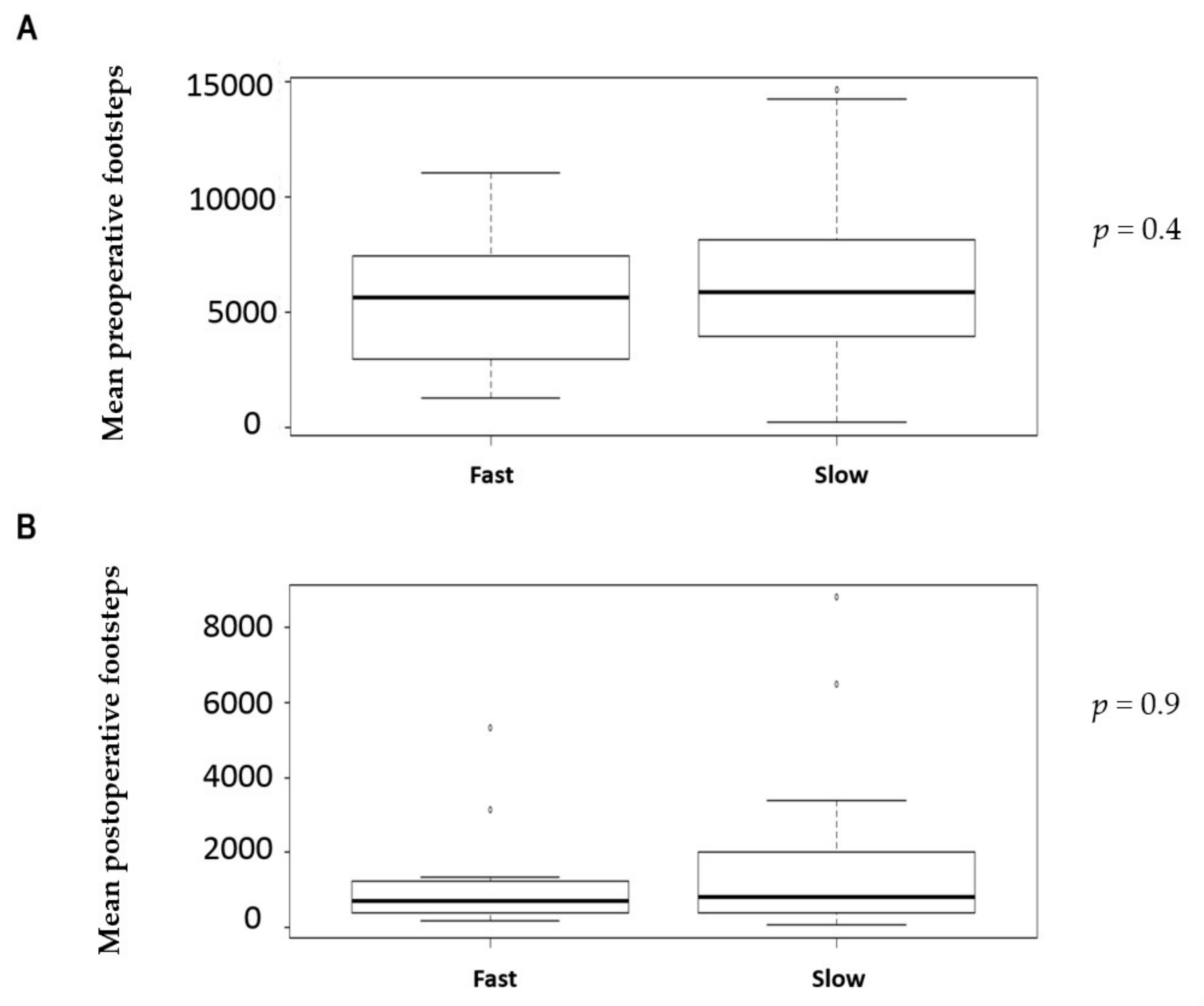
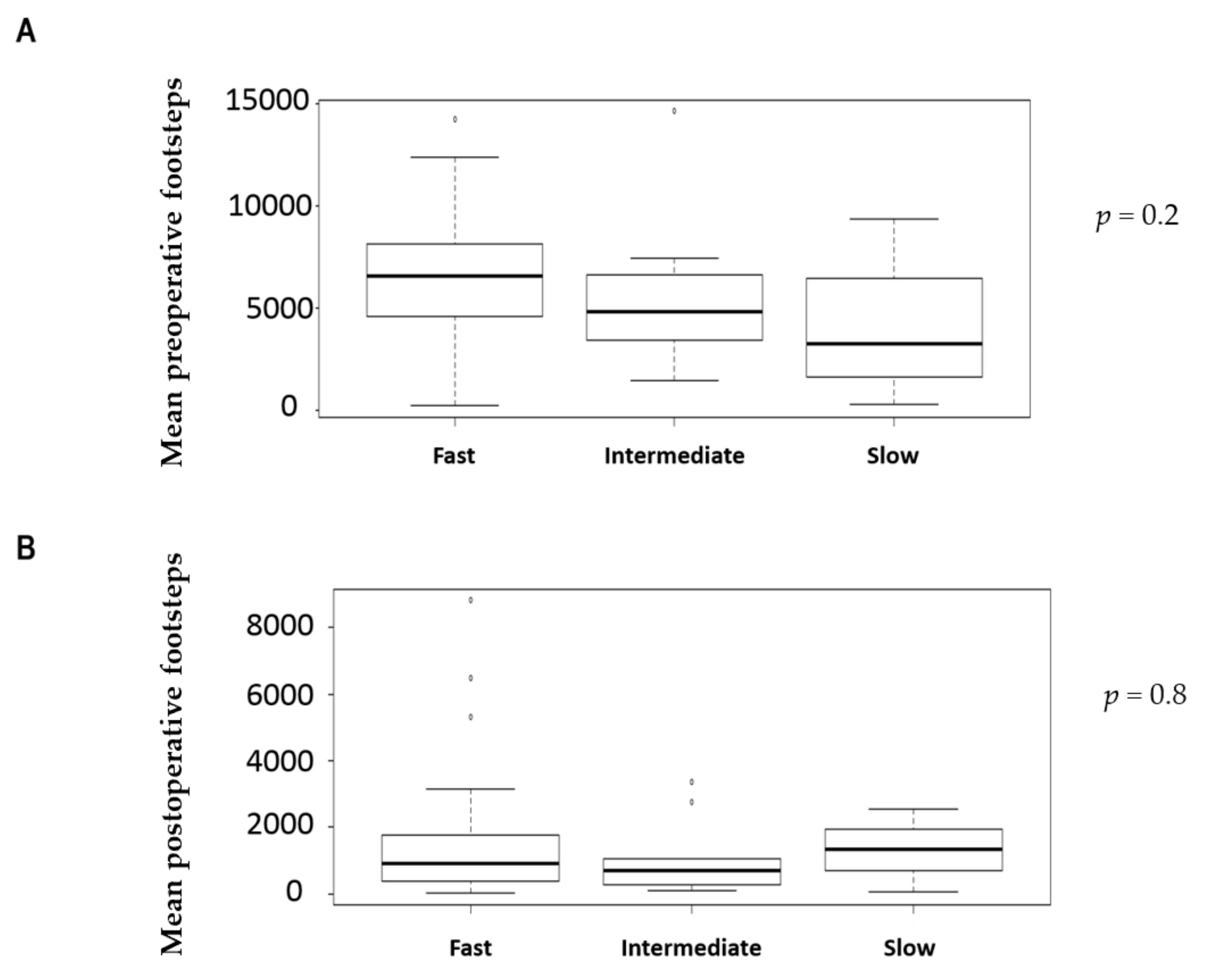
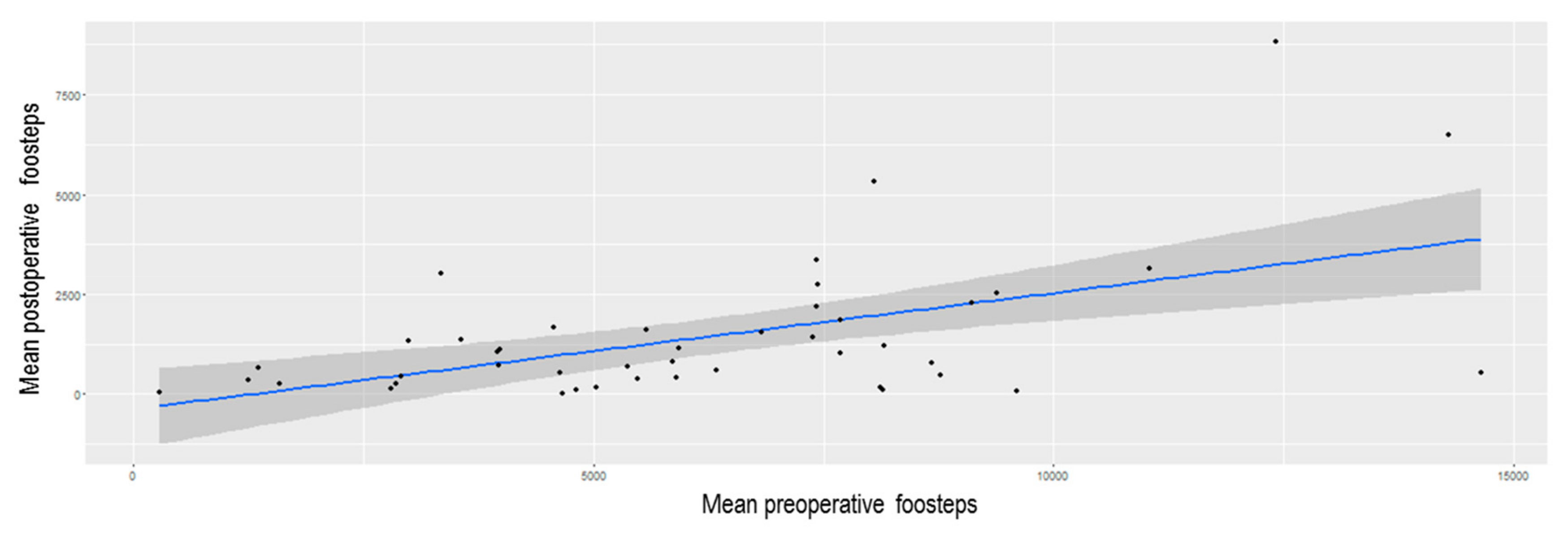
| Mean number of preoperative footsteps | 6163 (SD 4274) | |
| Mean number of postoperative footsteps (from POD0 to POD3) | 1183 (SD 1828) | |
| TUGT | “fast” (≤ 10 sec) | 35 (70%) |
| “intermediate” (11–14 sec) | 11 (22%) | |
| “slow” (≥ 15 sec) | 4 (8%) | |
| 6MWT | Fast | 12 (24%) |
| Slow | 35 (70%) | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Romain, B.; Martin, D.; Fabacher, T.; Pache, B.; Hahnloser, D.; Demartines, N.; Hübner, M. Comparison of Footsteps Using Connected Bracelets with the Timed Up-and-Go Test and the 6-Minutes Walking Test in a Prospective Colorectal Surgery Cohort. Nutrients 2020, 12, 563. https://doi.org/10.3390/nu12020563
Romain B, Martin D, Fabacher T, Pache B, Hahnloser D, Demartines N, Hübner M. Comparison of Footsteps Using Connected Bracelets with the Timed Up-and-Go Test and the 6-Minutes Walking Test in a Prospective Colorectal Surgery Cohort. Nutrients. 2020; 12(2):563. https://doi.org/10.3390/nu12020563
Chicago/Turabian StyleRomain, Benoît, David Martin, Thibaut Fabacher, Basile Pache, Dieter Hahnloser, Nicolas Demartines, and Martin Hübner. 2020. "Comparison of Footsteps Using Connected Bracelets with the Timed Up-and-Go Test and the 6-Minutes Walking Test in a Prospective Colorectal Surgery Cohort" Nutrients 12, no. 2: 563. https://doi.org/10.3390/nu12020563
APA StyleRomain, B., Martin, D., Fabacher, T., Pache, B., Hahnloser, D., Demartines, N., & Hübner, M. (2020). Comparison of Footsteps Using Connected Bracelets with the Timed Up-and-Go Test and the 6-Minutes Walking Test in a Prospective Colorectal Surgery Cohort. Nutrients, 12(2), 563. https://doi.org/10.3390/nu12020563








