Intestinal TG3- and TG2-Specific Plasma Cell Responses in Dermatitis Herpetiformis Patients Undergoing a Gluten Challenge
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Serology
2.3. Skin and Small Bowel Biopsies
2.4. Detection of TG3- and TG2-Specific Plasma Cells
2.5. Statistics
3. Results
3.1. General response to the gluten challenge in DH patients
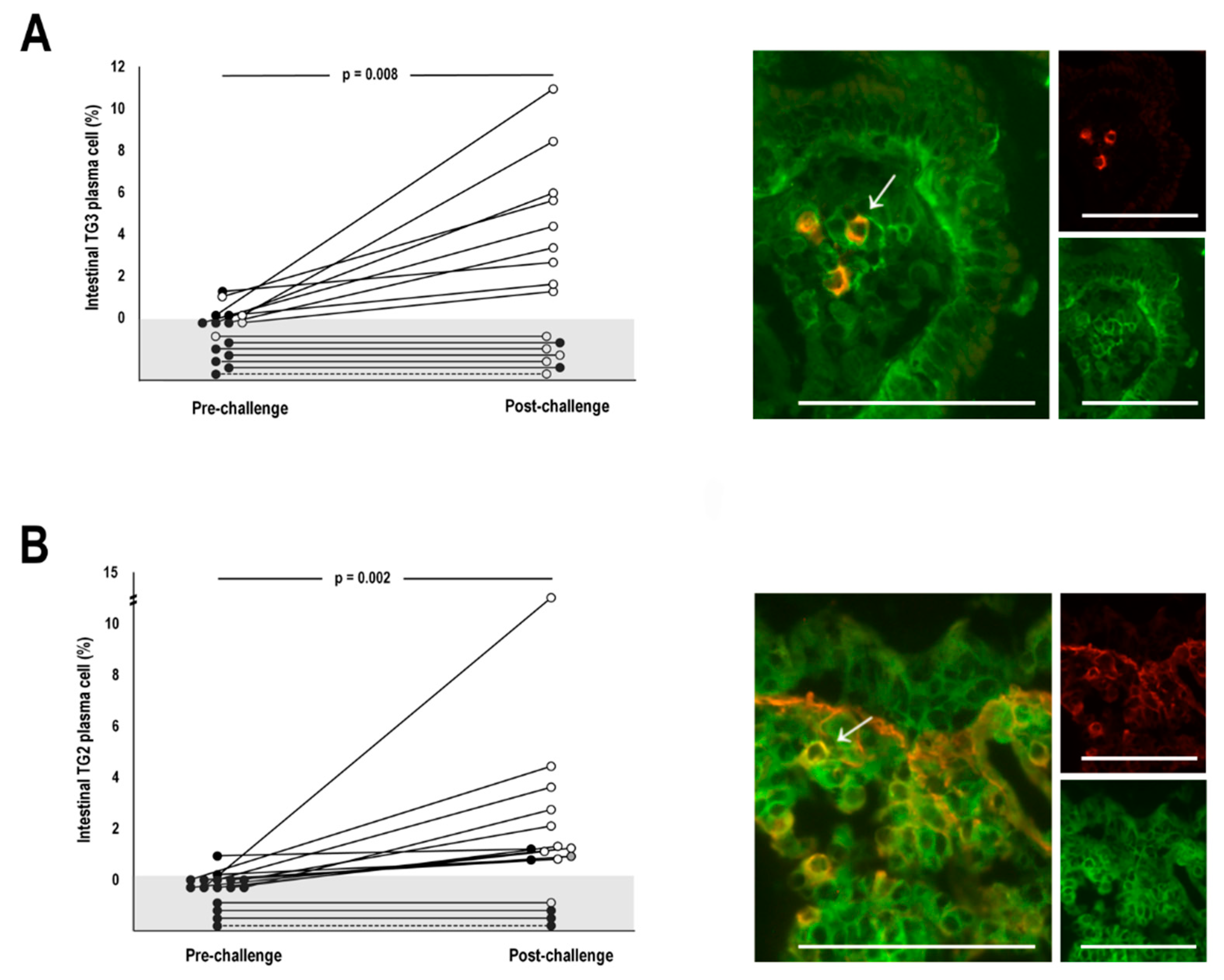
3.2. TG3-specific plasma cell responses
3.3. TG2-specific plasma cell responses
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Sardy, M.; Karpati, S.; Merkl, B.; Paulsson, M.; Smyth, N. Epidermal transglutaminase (TGase 3) is the autoantigen of dermatitis herpetiformis. J. Exp. Med. 2002, 195, 747–757. [Google Scholar] [CrossRef] [PubMed]
- Hull, C.M.; Liddle, M.; Hansen, N.; Meyer, L.J.; Schmidt, L.; Taylor, T.; Jaskowski, T.D.; Hill, H.R.; Zone, J.J. Elevation of IgA anti-epidermal transglutaminase antibodies in dermatitis herpetiformis. Br. J. Dermatol. 2008, 159, 120–124. [Google Scholar] [CrossRef] [PubMed]
- Salmi, T.T.; Kurppa, K.; Hervonen, K.; Laurila, K.; Collin, P.; Huhtala, H.; Saavalainen, P.; Sievänen, H.; Reunala, T.; Kaukinen, K. Serum transglutaminase 3 antibodies correlate with age at celiac disease diagnosis. Dig. Liver Dis. 2016, 48, 632–637. [Google Scholar] [CrossRef] [PubMed]
- Marietta, E.V.; Camilleri, M.J.; Castro, L.A.; Krause, P.K.; Pittelkow, M.R.; Murray, J.A. Transglutaminase autoantibodies in dermatitis herpetiformis and celiac sprue. J. Investig Dermatol. 2008, 128, 332–335. [Google Scholar] [CrossRef]
- Bardella, M.T.; Fredella, C.; Trovato, C.; Ermacora, E.; Cavalli, R.; Saladino, V.; Prampolini, L. Long-term remission in patients with dermatitis herpetiformis on a normal diet. Br. J. Dermatol. 2003, 149, 968–971. [Google Scholar] [CrossRef]
- Hietikko, M.; Hervonen, K.; Salmi, T.; Ilus, T.; Zone, J.J.; Kaukinen, K.; Reunala, T.; Lindfors, K.; Lindfors, K. Disappearance of epidermal transglutaminase and IgA deposits from the papillary dermis of dermatitis herpetiformis patients after a long-term gluten-free diet. Br. J. Dermatol. 2018, 178, 198–201. [Google Scholar] [CrossRef]
- Rose, C.; Armbruster, F.P.; Ruppert, J.; Igl, B.; Zillikens, D.; Shimanovich, I. Autoantibodies against epidermal transglutaminase are a sensitive diagnostic marker in patients with dermatitis herpetiformis on a normal or gluten-free diet. J. Am. Acad. Dermatol. 2009, 61, 39–43. [Google Scholar] [CrossRef]
- Reunala, T.; Salmi, T.T.; Hervonen, K.; Laurila, K.; Kautiainen, H.; Collin, P.; Kaukinen, K. IgA antiepidermal transglutaminase antibodies in dermatitis herpetiformis: A significant but not complete response to a gluten-free diet treatment. Br. J. Dermatol. 2015, 17, 1139–1141. [Google Scholar] [CrossRef]
- Mansikka, E.; Hervonen, K.; Kaukinen, K.; Ilus, T.; Oksanen, P.; Lindfors, K.; Laurila, K.; Hietikko, M.; Taavela, J.; Jernman, J.; et al. Gluten challenge induces skin and small bowel relapse in long-term gluten-free diet-treated dermatitis herpetiformis. J. Investig. Dermatol. 2019, 139, 2108–2114. [Google Scholar] [CrossRef]
- Hall, M.A.; Lanchbury, J.S.; Bolsover, W.J.; Welsh, K.I.; Ciclitira, P.J. HLA association with dermatitis herpetiformis is accounted for by a cis or transassociated DQ heterodimer. Gut 1991, 32, 487–490. [Google Scholar] [CrossRef][Green Version]
- Gawkrodger, D.J.; Blackwell, J.N.; Gilmour, H.M.; Rifkind, E.A.; Heading, R.C.; Barnetson, R.S. Dermatitis herpetiformis: Diagnosis, diet and demography. Gut 1984, 25, 151–157. [Google Scholar] [CrossRef]
- Reunala, T.; Kosnai, I.; Karpati, S.; Kuitunen, P.; Török, E.; Savilahti, E. Dermatitis herpetiformis: Jejunal findings and skin response to gluten free diet. Arch. Dis. Child. 1984, 59, 517–522. [Google Scholar] [CrossRef]
- Savilahti, E.; Reunala, T.; Mäki, M. Increase of lymphocytes bearing the gamma/delta T cell receptor in the jejunum of patients with dermatitis herpetiformis. Gut 1992, 33, 206–211. [Google Scholar] [CrossRef] [PubMed]
- Järvinen, T.T.; Kaukinen, K.; Laurila, K.; Kyrönpalo, S.; Rasmussen, M.; Mäki, M.; Korhonen, H.; Reunala, T.; Collin, P. Intraepithelial lymphocytes in celiac disease. Am. J. Gastroenterol. 2003, 98, 1332–1337. [Google Scholar] [CrossRef] [PubMed]
- Dieterich, W.; Ehnis, T.; Bauer, M.; Donner, P.; Volta, U.; Riecken, E.O.; Schuppan, D. Identification of tissue transglutaminase as the autoantigen of celiac disease. Nat. Med. 1997, 3, 797–801. [Google Scholar] [CrossRef] [PubMed]
- Korponay-Szabó, I.R.; Halttunen, T.; Szalai, Z.; Laurila, K.; Kiraly, R.; Kovacs, J.B.; Fésüs, L.; Mäki, M. In vivo targeting of intestinal and extraintestinal transglutaminase 2 by coeliac autoantibodies. Gut 2004, 53, 641–648. [Google Scholar] [CrossRef]
- Dieterich, W.; Schuppan, D.; Laag, E.; Bruckner-Tuderman, L.; Reunala, T.; Kárpáti, S.; Zágoni, T.; Riecken, E.O. Antibodies to tissue transglutaminase as serologic markers in patients with dermatitis herpetiformis. J. Investig. Dermatol. 1999, 113, 133–136. [Google Scholar] [CrossRef]
- Salmi, T.T.; Hervonen, K.; Laurila, K.; Collin, P.; MäKI, M.; Koskinen, O.; Huhtala, H.; Kaukinen, K.; Reunala, T. Small bowel transglutaminase 2-specific IgA deposits in dermatitis herpetiformis. Acta Derm. Venereol. 2014, 94, 393–397. [Google Scholar] [CrossRef]
- Di Niro, R.; Snir, O.; Kaukinen, K.; Yaari, G.; Lundin, K.E.; Gupta, N.T.; Kleinstein, S.H.; Cols, M.; Cerutti, A.; Mäki, M.; et al. Responsive population dynamics and wide seeding into the duodenal lamina propria of transglutaminase-2-specific plasma cells in celiac disease. Mucosal Immunol. 2016, 9, 254–256. [Google Scholar] [CrossRef]
- Di Niro, R.; Mesin, L.; Zheng, N.Y.; Stamnaes, J.; Morrissey, M.; Lee, J.H.; Huang, M.; Iversen, R.; Du Pré, M.F.; Qiao, S.W.; et al. High abundance of plasma cells secreting transglutaminase 2-specific IgA autoantibodies with limited somatic hypermutation in celiac disease intestinal lesions. Nat. Med. 2012, 18, 441–445. [Google Scholar] [CrossRef]
- Hietikko, M.; Koskinen, O.; Kurppa, K.; Laurila, K.; Saavalainen, P.; Salmi, T.; Ilus, T.; Huhtala, H.; Kaukinen, K.; Lindfors, K. Small-intestinal TG2-specific plasma cells at different stages of coeliac disease. BMC Immunol. 2018, 19, 36. [Google Scholar] [CrossRef] [PubMed]
- Hietikko, M.; Hervonen, K.; Ilus, T.; Salmi, T.; Huhtala, H.; Laurila, K.; Rauhavirta, T.; Reunala, T.; Kaukinen, K.; Lindfors, K. Ex vivo culture of duodenal biopsies from patients with Dermatitis herpetiformis indicates that transglutaminase 3 antibody production occurs in the gut. Acta Derm. Venereol. 2018, 98, 366–372. [Google Scholar] [CrossRef] [PubMed]
- Sulkanen, S.; Collin, P.; Laurila, K.; Mäki, M. IgA- and IgG-class antihuman umbilical cord antibody tests in adult coeliac disease. Scand. J. Gastroenterol. 1998, 33, 251–254. [Google Scholar] [CrossRef] [PubMed]
- Taavela, J.; Koskinen, O.; Huhtala, H.; Lähdeaho, M.L.; Popp, A.; Laurila, K.; Collin, P.; Kaukinen, K.; Kurppa, K.; Mäki, M. Validation of morphometric analyses of small-intestinal biopsy readouts in celiac disease. PLoS ONE 2013, 8, e76163. [Google Scholar] [CrossRef]
- Collin, P.; Salmi, T.T.; Hervonen, K.; Kaukinen, K.; Reunala, T. Dermatitis herpetiformis: A cutaneous manifestation of coeliac disease. Ann. Med. 2017, 49, 23–31. [Google Scholar] [CrossRef]
- Høydahl, L.S.; Richter, L.; Frick, R.; Snir, O.; Gunnarsen, K.S.; Landsverk, O.J.; Iversen, R.; Jeliazkov, J.R.; Gray, J.J.; Bergseng, E.; et al. Plasma Cells are the Most Abundant Gluten Peptide MHC-expressing Cells in Inflamed Intestinal Tissues From Patients With Celiac Disease. Gastroenterology 2019, 156, 1428–1439. [Google Scholar] [CrossRef]
- Iversen, R.; Snir, O.; Stensland, M.; Kroll, J.E.; Steinsbø, Ø.; Korponay-Szabo, I.R.; Lundin, K.E.; de Souza, G.A.; Sollid, L.M. Strong Clonal Relatedness between Serum and Gut IgA despite Different Plasma Cell Origins. Cell Rep. 2017, 20, 2357–2367. [Google Scholar] [CrossRef]
- Iversen, R.; Di Niro, R.; Stamnaes, J.; Lundin, K.E.; Wilson, P.C.; Sollid, L.M. Transglutaminase 2-specific autoantibodies in celiac disease target clustered, N-terminal epitopes not displayed on the surface of cells. J. Immunol. 2013, 190, 5981–5991. [Google Scholar] [CrossRef]
- Olbricht, S.M.; Flotte, T.J.; Collins, A.B.; Chapman, C.M.; Harrist, T.J. Dermatitis herpetiformis: Cutaneous deposition of polyclonal IgA1. Arch. Dermatol. 1986, 122, 418–421. [Google Scholar] [CrossRef]
- Barghuthy, F.S.; Kumar, V.; Valeski, E.; Beutner, E.H.; Chorzelski, T.P. Identification of IgA subclasses in skin of dermatitis herpetiformis patients. Int. Arch. Allergy Immunol. 1988, 85, 268–271. [Google Scholar] [CrossRef]
| Dermatitis Herpetiformis n = 16 | Coeliac Disease | Non-Coeliac Controls n = 7 | ||
|---|---|---|---|---|
| Untreated | Treated | |||
| n = 18 | n = 15 | |||
| Females; n (%) | 5 (31) | 11 (61) | 11 (73) | 6 (86) |
| Age, years, median (range) | 58 (37–72) | 50 (18–71) | 48 (19–72) | 47 (24–76) |
| Duration of GFD at diagnosis, years, median (range) | 22 (5–40) | 0 | 1 (1–1) | 0 |
| Pre-Challenge | Post-Challenge | |||
|---|---|---|---|---|
| Positive Cases, n (%) | Median (Range) | Positive Cases, n (%) | Median (Range) | |
| Serum TG3 antibodies (AU/mL) | 4 (25) | 4 (0–41) | 14 (88) | 140 (5–190) |
| Dermal TG3-IgA | 1 (16) | 0 (0–1) | 10 (63) | 1 (0–3) |
| Serum TG2 antibodies (U/mL) | 0 (0) | 0 (0–0) | 10 (63) | 101 (0–101) |
| Serum EmA (titre) | 0 (0) | 0 (0–0) | 12 (75) | 1:500 (0–1:4000) |
| Intestinal TG2-IgA deposits | 0 (0) | 0 (0–0) | 10 (63) | 1 (0–3) |
| Vh/CrD | 2.6 (2.1–4.5) | 0.8 (0.1–3.1) | ||
| RS | p-Value | |
|---|---|---|
| TG3-specific plasma cells | ||
| Serum TG3 antibodies | 0.541 | 0.030 |
| Intensity of dermal TG3-IgA | 0.175 | 0.517 |
| Vh/CrD | −0.273 | 0.307 |
| TG2-specific plasma cells | ||
| Serum TG2 antibodies | 0.759 | 0.001 |
| Serum EmA | 0.732 | 0.001 |
| Intensity of intestinal TG2-IgA deposits | 0.691 | 0.003 |
| Vh/CrD | −0.195 | 0.469 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sankari, H.; Hietikko, M.; Kurppa, K.; Kaukinen, K.; Mansikka, E.; Huhtala, H.; Laurila, K.; Reunala, T.; Hervonen, K.; Salmi, T.; et al. Intestinal TG3- and TG2-Specific Plasma Cell Responses in Dermatitis Herpetiformis Patients Undergoing a Gluten Challenge. Nutrients 2020, 12, 467. https://doi.org/10.3390/nu12020467
Sankari H, Hietikko M, Kurppa K, Kaukinen K, Mansikka E, Huhtala H, Laurila K, Reunala T, Hervonen K, Salmi T, et al. Intestinal TG3- and TG2-Specific Plasma Cell Responses in Dermatitis Herpetiformis Patients Undergoing a Gluten Challenge. Nutrients. 2020; 12(2):467. https://doi.org/10.3390/nu12020467
Chicago/Turabian StyleSankari, Hanna, Minna Hietikko, Kalle Kurppa, Katri Kaukinen, Eriika Mansikka, Heini Huhtala, Kaija Laurila, Timo Reunala, Kaisa Hervonen, Teea Salmi, and et al. 2020. "Intestinal TG3- and TG2-Specific Plasma Cell Responses in Dermatitis Herpetiformis Patients Undergoing a Gluten Challenge" Nutrients 12, no. 2: 467. https://doi.org/10.3390/nu12020467
APA StyleSankari, H., Hietikko, M., Kurppa, K., Kaukinen, K., Mansikka, E., Huhtala, H., Laurila, K., Reunala, T., Hervonen, K., Salmi, T., & Lindfors, K. (2020). Intestinal TG3- and TG2-Specific Plasma Cell Responses in Dermatitis Herpetiformis Patients Undergoing a Gluten Challenge. Nutrients, 12(2), 467. https://doi.org/10.3390/nu12020467





