Food Insecurity and Major Diet-Related Morbidities in Migrating Children: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
3. Results
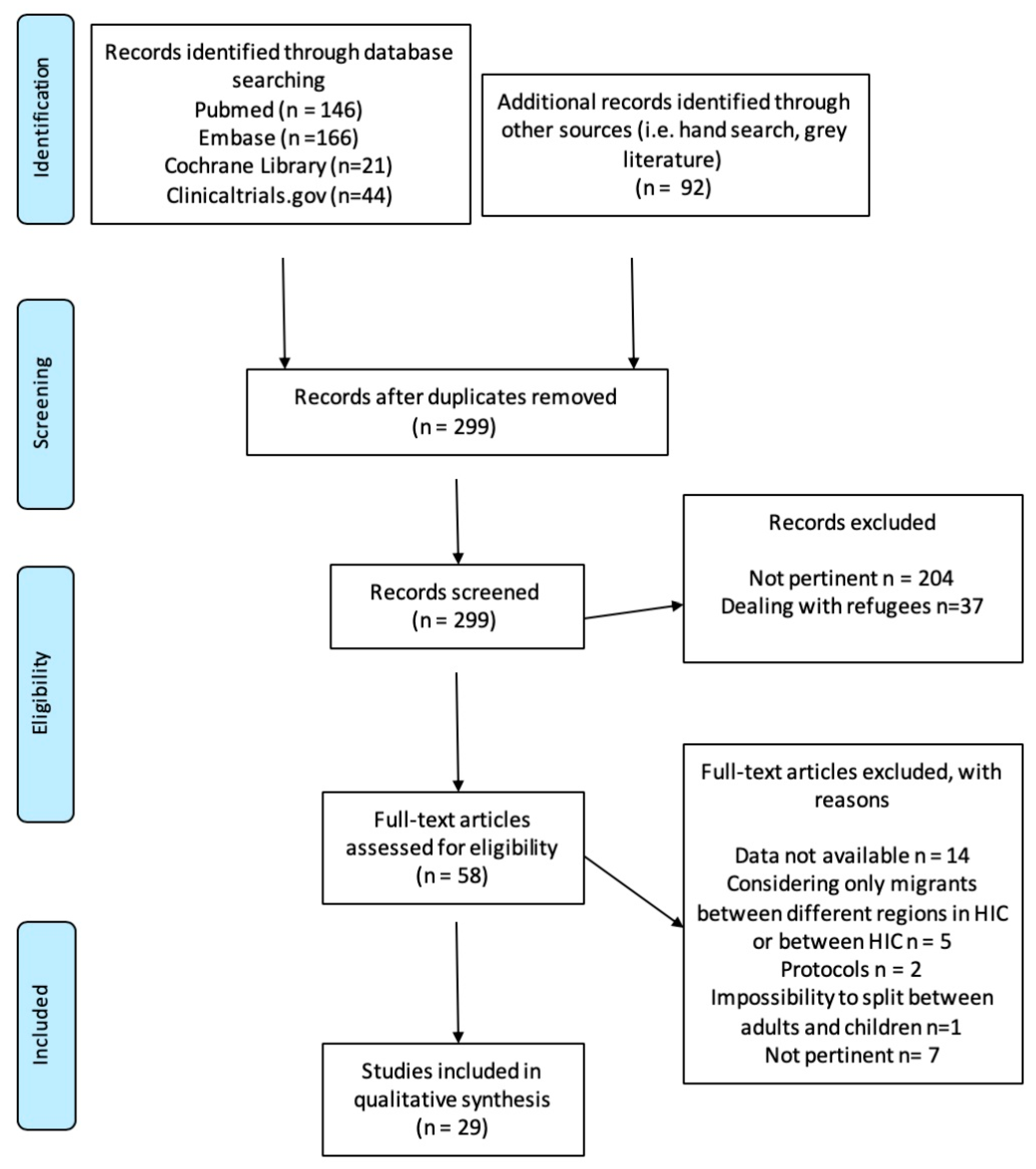
3.1. Search Yields, Risk of Bias, and Quality of Reporting
3.2. Evidence Synthesis
3.2.1. Overweight, Obesity, and Associated Complications
3.2.2. Stunting
3.2.3. Early Childhood Caries
3.2.4. Micronutrient Deficiency
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- United Nations, Deparment of Economic and Social Affairs, Population Division (2019). World Population Prospects 2019. Available online: https://www.un.org/en/development/desa/population/index.asp (accessed on 26 December 2019).
- Foresight. Migration and Global Environmental Change; Final project report; The Government Office for Science: London, UK, 2011; pp. 43–45.
- Holben, D.H. Position of the American Dietetic Association: Food insecurity and hunger in the United States. J. Am. Diet. Assoc. 2006, 106, 446–458. [Google Scholar] [CrossRef]
- Cook, J.T.; Frank, D.A.; Levenson, S.M.; Neault, N.B.; Heeren, T.C.; Black, M.M.; Berkowitz, C.; Casey, P.H.; Meyers, A.F.; Cutts, D.B.; et al. Child food insecurity increases risks posed by household food insecurity to young children’s health. J. Nutr. 2006, 136, 1073–1076. [Google Scholar] [CrossRef]
- Rose-Jacobs, R.; Black, M.M.; Casey, P.H.; Cook, J.T.; Cutts, D.B.; Chilton, M.; Heeren, T.; Levenson, S.M.; Meyers, A.F.; Frank, D.A. Household food insecurity: Associations with at-risk infant and toddler development. Pediatrics 2008, 121, 65–72. [Google Scholar] [CrossRef]
- Cook, J.T.; Frank, D.A.; Berkowitz, C.; Black, M.M.; Casey, P.H.; Cutts, D.B.; Meyers, A.F.; Zaldivar, N.; Skalicky, A.; Levenson, S.M.; et al. Food insecurity is associated with adverse health outcomes among human infants and toddlers. J. Nutr. 2004, 134, 1432–1438. [Google Scholar] [CrossRef]
- Whitaker, R.C.; Phillips, S.M.; Orzol, S.M. Food insecurity and the risks of depression and anxiety in mothers and behavior problems in their preschool-aged children. Pediatrics 2006, 118, e859–868. [Google Scholar] [CrossRef]
- Jyoti, D.F.; Frongillo, E.A.; Jones, S.J. Food insecurity affects school children’s academic performance, weight gain, and social skills. J. Nutr. 2005, 135, 2831–2839. [Google Scholar] [CrossRef]
- Nord, M.; Andrews, M.S.; Carlson, S. Household food security in the United States, 2008; Dept. of Agriculture, Economic Research Service: Washington, DC, USA, 2008.
- Capps, R. Hardship among Children of Immigrants: Finding from the National Survey of America’s Families; The Urban Institute: Washington, DC, USA, 2001; pp. 1–8. [Google Scholar]
- Hernandez, D.J.; College, H.; Napierala, J.S. Children in Immigrant Families: Essential to America’s Future. The Foundation for Child Development: New York, NY, USA, 2012; Available online: https://www.fcd-us.org/children-in-immigrant-families-essential-to-americas-future/ (accessed on 26 December 2019).
- Pettoello-Mantovani, M.; Ehrich, J.; Sacco, M.; Ferrara, P.; Giardino, I.; Pop, T.L. Food in security and children’s rights to adequate nutrition in Europe. J. Pediatr. 2018, 198, 329–330. [Google Scholar] [CrossRef]
- Audrey, L.; Pereira, L.; Handa, S.; Holmqvist, G. Prevalence and correlates of food insecurity among children across the globe. Available online: https://www.unicef-irc.org/publications/pdf/IWP_2017_09.pdf (accessed on 22 January 2020).
- Verga, M.E.; Widmeier-Pasche, V.; Beck-Popovic, M.; Pauchard, J.Y.; Gehri, M. Iron deficiency in infancy: Is an immigrant more at risk? Swiss Med. Wkly. 2014, 144, w14065. [Google Scholar] [CrossRef]
- Thacher, T.D.; Pludowki, P.; Shaw, N.J.; Mughal, M.Z.; Munns, C.F.; Högler, W. Nutritional rickets in immigrant and refugee children. Public Health Rev. 2016, 37, 3. [Google Scholar] [CrossRef]
- Carter, R.C.; Jacobson, J.L.; Burden, M.J.; Armony-Sivan, R.; Dodge, N.C.; Angelilli, M.L.; Lozoff, B.; Jacobson, S.W. Iron deficiency anemia and cognitive function in infancy. Pediatrics 2010, 126, e427–434. [Google Scholar] [CrossRef]
- Renzaho, A.M.; Swinburn, B.; Burns, C. Maintenance of traditional cultural orientation is associated with lower rates of obesity and sedentary behaviours among African migrant children to developed countries. Int. J. Obes. 2008, 32, 594–600. [Google Scholar] [CrossRef] [PubMed]
- Roberts, M.W. Dental health of children: Where we are today and remaining challenges. J. Clin. Pediatr. Dent. 2008, 32, 231–234. [Google Scholar] [CrossRef] [PubMed]
- Patrick, D.L.; Lee, R.S.; Nucci, M.; Grembowski, D.; Jolles, C.Z.; Milgrom, P. Reducing oral health disparities: A focus on social and cultural determinants. BMC Oral Health 2006, 6, 1–17. [Google Scholar] [CrossRef]
- American Academy of Pediatric Dentistry. Reference manual 2004–2005. Pediatr. Dent. 2004, 26, 1–203. [Google Scholar]
- Ripa, L.W. Nursing caries: A comprehensive review. Pediatr. Dent. 1988, 10, 262–282. [Google Scholar]
- Lane, G.; Farag, M.; White, J.; Nisbet, C.; Vatanparast, H. Chronic health disparities among refugee and immigrant children in Canada. Appl. Physiol. Nutr. Metab. 2018, 43, 1043–1058. [Google Scholar] [CrossRef]
- Beiser, M.; Hou, F.; Hyman, I.; Tousignant, M. Poverty, family process, and the mental health of immigrant children in Canada. Am. J. Publ. Health. 2002, 92, 220–227. [Google Scholar] [CrossRef]
- Beiser, M. Longitudinal research to promote effective refugee resettlement. Transcult. Psychiatry 2006, 43, 56–71. [Google Scholar] [CrossRef]
- Rousseau, C.; Drapeau, A. Are refugee children an at-risk group? A longitudinal study of Cambodian adolescents. J. Refugee Stud. 2003, 16, 67–81. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Effective Public Health Practice Project. Quality assessment tool for quantitative studies. Available online: https://merst.ca/wp-content/uploads/2018/02/quality-assessment-tool_2010.pdf (accessed on 19 December 2019).
- World Health Organization. Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection. Definition of key terms. Available online: https://www.who.int/hiv/pub/guidelines/arv2013/intro/keyterms/en/ (accessed on 19 December 2019).
- OMICS International. Nutritional status research articles. Available online: https://www.omicsonline.org/nutrition-disorder-and-therapy/nutritional-status-research-articles.php (accessed on 19 December 2019).
- Miller, M.A.; Zachary, J.F. Chapter 1 Mechanisms and Morphology of Cellular Injury, Adaptation, and Death. In Pathologic Basis of Veterinary Disease, 6th ed.; Zachary, J.F., Ed.; Mosby Elsevier: St. Louis, MI, USA, 2017; pp. 2–43.e19. [Google Scholar]
- Food and Agriculture Organization of the United Nations. Food Security Information for Action Practical Guides. An Introduction to the Basic Concepts of Food Security. FAO 2008. Available online: http://www.fao.org/3/al936e/al936e00.pdf (accessed on 19 December 2019).
- Winkleby, M.A.; Jatulis, D.E.; Frank, E.; Fortmann, S.P. Socioeconomic status and health: How education, income, and occupation contribute to risk factors for cardiovascular disease. Am. J. Public Health 1992, 82, 816–820. [Google Scholar] [CrossRef]
- International Organization for Migration. Key migration terms. Available online: https://www.iom.int/key-migration-terms (accessed on 23 December 2019).
- Besharov, D.J.; Lopez, M.H. Adjusting to a World in Motion: Trends in Global Migration and Migration Policy, 1st ed.; Oxford University Press: New York, NY, USA, 2016; ISBN 978-019-021-139-4. [Google Scholar]
- Rosas, L.G.; Guendelman, S.; Harley, K.; Fernald, L.C.; Neufeld, L.; Mejia, F.; Eskenazi, B. Factors associated with overweight and obesity among children of Mexican descent: Results of a binational study. J. Immigr. Minor. Health 2011, 13, 169–180. [Google Scholar] [CrossRef]
- Kaiser, L.L.; Aguilera, A.L.; Horowitz, M.; Lamp, C.; Johns, M.; Gomez-Camacho, R.; Ontai, L.; de la Torre, A. Correlates of food patterns in young Latino children at high risk of obesity. Public Health Nutr. 2015, 18, 3042–3050. [Google Scholar] [CrossRef][Green Version]
- Kobel, S.; Lämmle, C.; Wartha, O.; Kesztyüs, D.; Wirt, T.; Steinacker, J.M. Effects of a randomised controlled school-based health promotion intervention on obesity related behavioural outcomes of children with migration background. J. Immigr. Minor. Health 2017, 19, 254–262. [Google Scholar] [CrossRef]
- Kobel, S.; Wirt, T.; Schreiber, A.; Kesztyüs, D.; Kettner, S.; Erkelenz, N.; Wartha, O.; Steinacker, J.M. Intervention effects of a school-based health promotion programme on obesity related behavioural outcomes. J. Obes. 2014, 2014, 1–8. [Google Scholar] [CrossRef]
- Early, G.J.; Cheffer, N.D. Motivational interviewing and home visits to improve health behaviors and reduce childhood obesity: A pilot study. Hisp. Health Care Int. 2019, 17, 103–110. [Google Scholar] [CrossRef]
- Geremia, R.; Cimadon, H.M.; de Souza, W.B.; Pellanda, L.C. Childhood overweight and obesity in a region of Italian immigration in Southern Brazil: A cross-sectional study. Ital. J. Pediatr. 2015, 41, 28. [Google Scholar] [CrossRef]
- Distel, L.M.L.; Egbert, A.H.; Bohnert, A.M.; Santiago, C.D. chronic stress and food insecurity: examining key environmental family factors related to body mass index among low-income mexican-origin youth. Fam. Community Health 2019, 42, 213–220. [Google Scholar] [CrossRef]
- Buscemi, J.; Beech, B.M.; Relyea, G. Predictors of obesity in Latino children: Acculturation as a moderator of the relationship between food insecurity and body mass index percentile. J. Immigr. Minor. Health 2011, 13, 149–154. [Google Scholar] [CrossRef]
- Kilanowski, J.F. Patterns and correlates of nutrition among migrant farm-worker children. West. J. Nurs. Res. 2012, 34, 396–416. [Google Scholar] [CrossRef]
- Ebenegger, V.; Marques-Vidal, P.M.; Nydegger, A.; Laimbacher, J.; Niederer, I.; Bürgi, F.; Giusti, V.; Bodenmann, P.; Kriemler, S.; Puder, J.J. Independent contribution of parental migrant status and educational level to adiposity and eating habits in preschool children. Eur. J. Clin. Nutr. 2011, 65, 210–218. [Google Scholar] [CrossRef]
- Huang, X.; Chen, W.; Lin, Y.; Zhang, Q.; Ling, L. Association between acculturation and body weight status among migrant children in Guangzhou, China: A cross-sectional study. BMJ Open 2018, 8, e018768. [Google Scholar] [CrossRef]
- Tsujimoto, T.; Kajio, H.; Sugiyama, T. Obesity, diabetes, and length of time in the United States: Analysis of National Health and Nutrition Examination Survey 1999 to 2012. Medicine (Baltimore) 2016, 95, e4578. [Google Scholar] [CrossRef]
- Iguacel, I.; Fernández-Alvira, J.M.; Ahrens, W.; Bammann, K.; Gwozdz, W.; Lissner, L.; Michels, N.; Reisch, L.; Russo, P.; Szommer, A.; et al. Prospective associations between social vulnerabilities and children’s weight status. Results from the IDEFICS study. Int. J. Obes. (Lond) 2018, 42, 1691–1703. [Google Scholar] [CrossRef]
- Labree, W.; van de Mheen, D.; Rutten, F.; Rodenburg, G.; Koopmans, G.; Foets, M. Differences in Overweight and Obesity among Children from Migrant and Native Origin: The Role of Physical Activity, Dietary Intake, and Sleep Duration. PLoS ONE 2015, 10, e0123672. [Google Scholar] [CrossRef]
- Besharat Pour, M.; Bergström, A.; Bottai, M.; Kull, I.; Wickman, M.; Håkansson, N.; Wolk, A.; Moradi, T. Effect of parental migration background on childhood nutrition, physical activity, and body mass index. J. Obes. 2014, 406529. [Google Scholar] [CrossRef]
- Chomitz, V.R.; Brown, A.; Lee, V.; Must, A.; Chui, K.K.H. Healthy Living Behaviors AmongChinese-American Preschool-Aged Children: Results of a Parent Survey. J. Immigr. Minor. Health 2018, 20, 926–935. [Google Scholar] [CrossRef]
- Alasagheirin, M.H.; Clark, M.K. Skeletal growth, body composition, and metabolic risk among North Sudanese immigrant children. Public Health Nurs. 2018, 35, 91–99. [Google Scholar] [CrossRef]
- Tovar, A.; Hennessy, E.; Pirie, A.; Must, A.; Gute, D.M.; Hyatt, R.R.; Kamins, C.L.; Hughes, S.O.; Boulos, R.; Sliwa, S.; et al. Feeding styles and child weight status among recent immigrant mother-child dyads. Int. J. Behav. Nutr. Phys. Act. 2012, 9, 62. [Google Scholar] [CrossRef]
- Cheah, C.S.; Van Hook, J. Chinese and Korean immigrants’ early life deprivation: An important factor for child feeding practices and children’s body weight in the United States. Soc. Sci. Med. 2012, 74, 744–752. [Google Scholar] [CrossRef][Green Version]
- Cook, W.K.; Tseng, W.; Tam, C.; John, I.; Lui, C. Ethnic-group socioeconomic status as an indicator of community-level disadvantage: A study of overweight/obesity in Asian American adolescents. Soc. Sci. Med. 2017, 184, 15–22. [Google Scholar] [CrossRef]
- Zulfiqar, T.; Strazdins, L.; Dinh, H.; Banwell, C.; D’Este, C. Drivers of Overweight/Obesity in 4-11 Year Old Children of Australians and Immigrants; Evidence from Growing Up in Australia. J. Immigr. Minor. Health 2019, 21, 737–750. [Google Scholar] [CrossRef]
- Iriart, C.; Handal, A.J.; Boursaw, B.; Rodrigues, G. Chronic malnutrition among overweight Hispanic children: Understanding health disparities. J. Immigr. Minor. Health 2011, 13, 1069–1075. [Google Scholar] [CrossRef]
- Choudhary, N.; Parthasarathy, D. Is migration status a determinant of urban nutrition insecurity? Empirical evidence from Mumbai city, India. J. Biosoc. Sci. 2009, 41, 583–605. [Google Scholar] [CrossRef]
- Lee, S.K.; Nam, S.Y.; Hoffman, D. Changes in nutritional status among displaced North Korean children living in South Korea. Ann. Hum. Biol. 2015, 42, 581–584. [Google Scholar] [CrossRef]
- Werneck, R.I.; Lawrence, H.P.; Kulkarni, G.V.; Locker, D. Early childhood caries and access to dental care among children of Portuguese-speaking immigrants in the city of Toronto. J. Can. Dent. Assoc. 2008, 74, 805. [Google Scholar]
- Vatanparast, H.; Nisbet, C.; Gushulak, B. Vitamin D insufficiency and bone mineral status in a population of newcomer children in Canada. Nutrients 2013, 5, 1561–1572. [Google Scholar] [CrossRef]
- Sacri, A.S.; Hercberg, S.; Gouya, L.; Levy, C.; Bocquet, A.; Blondel, B.; Vincelet, C.; Hebel, P.; Vinatier, I.; de Montalembert, M.; et al. Very low prevalence of iron deficiency among young French children: A national cross-sectional hospital-based survey. Matern. Child. Nutr. 2018, 14, e12460. [Google Scholar] [CrossRef]
- Saunders, N.R.; Parkin, P.C.; Birken, C.S.; Maguire, J.L.; Borkhoff, C.M.; TARGet Kids! Collaboration. Iron status of young children from immigrant families. Arch. Dis. Child. 2016, 101, 1130–1136. [Google Scholar] [CrossRef]
- Kim, Y.N.; Lora, K.R.; Giraud, D.W.; Driskell, J.A. Nonsupplemented children of Latino immigrants have low vitamin E intakes and plasma concentrations and normal vitamin C, selenium, and carotenoid intakes and plasma concentrations. J. Am. Diet. Assoc. 2006, 106, 385–391. [Google Scholar] [CrossRef]
- Datar, A.; Sturm, R.; Magnabosco, J.L. Childhood overweight and academic performance: National study of kindergartners and first-graders. Obes. Res. 2004, 12, 58–68. [Google Scholar] [CrossRef]
- Strauss, R.S.; Pollack, H.A. Social marginalization of overweight children. Arch. Pediatr. Adolesc. Med. 2003, 157, 746–752. [Google Scholar] [CrossRef]
- Swallen, K.C.; Reither, E.N.; Haas, S.A.; Meier, A.M. Overweight, obesity, and health-related quality of life among adolescents: The national longitudinal study of adolescent health. Pediatrics 2005, 115, 340–347. [Google Scholar] [CrossRef]
- Del Rio-Navarro, B.; Velazquez-Monroy, O.; Sanchez-Castillo, C.; Lara-Esqueda, A.; Berber, A.; Fanghanel, G.; Violante, R.; Tapia-Conyer, R.; James, W.P.; Encuesta Nacional de Salud 2000 Working Group; et al. The high prevalence of overweight and obesity in Mexican children. Obes. Res. 2004, 12, 215–223. [Google Scholar] [CrossRef]
- Reilly, J.; Kelly, J. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: Systematic review. Int. J. Obes. (Lond) 2011, 35, 891–898. [Google Scholar] [CrossRef]
- Caprio, S.; Daniels, S.R.; Drewnowski, A.; Kaufman, F.R.; Palinkas, L.A.; Rosenbloom, A.L.; Schwimmer, J.B. Influence of race, ethnicity, and culture on childhood obesity: Implications for prevention and treatment: A consensus statement of Shaping America’s Health and the Obesity Society. Diabetes Care 2008, 31, 2211–2221. [Google Scholar] [CrossRef]
- Elinder, L.S.; Heinemans, N.; Zeebari, Z.; Patterson, E. Longitudinal changes in health behaviours and body weight among Swedish school children–associations with age, gender and parental education–the SCIP school cohort. BMC Public Health 2014, 14, 640. [Google Scholar] [CrossRef]
- Lasserre, A.M.; Chiolero, A.; Cachat, F.; Paccaud, F.; Bovet, P. Overweight in Swiss children and associations with children’s and parents’ characteristics. Obesity (Silver Spring) 2007, 15, 2912–2919. [Google Scholar] [CrossRef]
- Sausenthaler, S.; Kompauer, I.; Mielck, A.; Borte, M.; Herbarth, O.; Schaaf, B.; von Berg, A.; Heinrich, J. Impact of parental education and income inequality on children’s food intake. Public Health Nutr. 2007, 10, 24–33. [Google Scholar] [CrossRef]
- Kennedy, S.; Kidd, M.P.; McDonald, J.T.; Biddle, N. The healthy immigrant effect: Patterns and evidence from four countries. J. Int. Migr. Integr. 2015, 16, 317–332. [Google Scholar] [CrossRef]
- Murphy, M.; Robertson, W.; Oyebode, O. Obesity in International Migrant Populations. Curr. Obes. Rep. 2017, 6, 314–323. [Google Scholar] [CrossRef]
- Baker, E.H.; Rendall, M.S.; Weden, M.M. Epidemiological Paradox or Immigrant Vulnerability? Obesity Among Young Children of Immigrants. Demography 2015, 52, 1295–1320. [Google Scholar] [CrossRef]
- Gualdi-Russo, E.; Zaccagni, L.; Manzon, V.S.; Masotti, S.; Rinaldo, N.; Khyatti, M. Obesity and physical activity in children of immigrants. Eur. J. Public Health 2014, 24, 40–46. [Google Scholar] [CrossRef]
- Kuyper, E.M.; Smith, D.; Kaiser, L.L. Does food insecurity influence child feeding practices? J. Hunger. Environ. Nutr. 2009, 4, 147–157. [Google Scholar] [CrossRef]
- Franklin, B.; Jones, A.; Love, D.; Puckett, S.; Macklin, J.; White-Means, S. Exploring mediators of food insecurity and obesity: A review of recent literature. J. Community Health 2012, 37, 253–264. [Google Scholar] [CrossRef]
- Dhurandhar, E.J. The food-insecurity obesity paradox: A resource scarcity hypothesis. Physiol. Behav. 2016, 162, 88–92. [Google Scholar] [CrossRef]
- Sarlio-Lahteenkorva, S.; Lahelma, E. Food insecurity is associated with past and present economic disadvantage and body mass index. J. Nutr. 2001, 131, 2880–2884. [Google Scholar] [CrossRef]
- Kossmann, J.; Nestel, P.M.; Herrera, M.G.; El Amin, A.; Fawzi, W.W. Undernutrition in relation to childhood infections: A prospective study in the Sudan. Eur. J. Clin. Nutr. 2000, 54, 463–472. [Google Scholar] [CrossRef]
- de Onis, M.; Branca, F. Childhood stunting: A global perspective. Matern. Child. Nutr. 2016, 12, 12–26. [Google Scholar] [CrossRef]
- Schroth, R.J.; Harrison, R.L.; Moffatt, M.E. Oral health of indigenous children and the influence of early childhood caries on childhood health and well-being. Pediatr. Clin. N. Am. 2009, 56, 1481–1499. [Google Scholar] [CrossRef]
- Clarke, M.; Locker, D.; Berall, G.; Pencharz, P.; Kenny, D.J.; Judd, P. Malnourishment in a population of young children with severe early childhood caries. Pediatr. Dent. 2006, 28, 254–259. [Google Scholar]
- Bobetsis, Y.A.; Barros, S.P.; Offenbacher, S. Exploring the relationship between periodontal disease and pregnancy complications. J. Am. Dent. Assoc. 2006, 137, 7S–13S. [Google Scholar] [CrossRef]
- Birch, S.; Anderson, R. Financing and delivering oral health care: What can we learn from other countries? J. Can. Dent. Assoc. 2005, 71, 243a–243d. [Google Scholar]
- Bhatti, T.; Rana, Z.; Grootendorst, P. Dental insurance, income and the use of dental care in Canada. J. Can. Dent. Assoc. 2007, 73, 57. [Google Scholar]
- Charoenngam, N.; Shirvani, A.; Holick, M.F. Vitamin D for skeletal and non-skeletal health: What we should know. J. Clin. Orthop. Trauma 2019, 10, 1082–1093. [Google Scholar] [CrossRef]
- Holick, M.F. Resurrection of vitamin D deficiency and rickets. J. Clin. Investig. 2006, 116, 2062–2072. [Google Scholar] [CrossRef]
- Yentür Doni, N.; Yıdız Zeyrek, F.; Simşek, Z.; Zeyrek, D. The effects of intestinal parasites on anemia of children. Turkiye Parazitol Derg 2014, 38, 85–90. [Google Scholar] [CrossRef]
- Fontanelli Sulekova, L.; Ceccarelli, G.; Pombi, M.; Esvan, R.; Lopalco, M.; Vita, S.; Mattiucci, S.; Gabrielli, S.; Sanitary Bureau of the Asylum Seekers Center of Castelnuovo di Porto. Occurrence of intestinal parasites among asylum seekers in Italy: A cross-sectional study. Travel Med. Infect. Dis. 2019, 27, 46–52. [Google Scholar] [CrossRef]
- Vallée, L. Iron and neurodevelopment. Arch. Pediatr. 2017, 24, 5S18–5S22. [Google Scholar] [CrossRef]
- Kim, J.; Wessling-Resnick, M. Iron and mechanisms of emotional behavior. J. Nutr. Biochem. 2014, 25, 1101–1107. [Google Scholar] [CrossRef]
- de Silva, A.; Atukorala, S.; Weerasinghe, I.; Ahluwalia, N. Iron supplementation improves iron status and reduces morbidity in children with or without upper respiratory tract infections: A randomized controlled study in Colombo, Sri Lanka. Am. J. Clin. Nutr. 2003, 77, 234–241. [Google Scholar] [CrossRef]
- Lozoff, B.; Klein, N.K.; Nelson, E.C.; McClish, D.K.; Manuel, M.; Chacon, M.E. Behavior of infants with iron-deficiency anemia. Child. Dev. 1998, 69, 24–36. [Google Scholar] [CrossRef]
- Burden, M.J.; Westerlund, A.J.; Armony-Sivan, R.; Nelson, C.A.; Jacobson, S.W.; Lozoff, B.; Angelilli, M.L.; Jacobson, J.L. An event-related potential study of attention and recognition memory in infants with iron-deficiency anemia. Pediatrics 2007, 120, e336–e345. [Google Scholar] [CrossRef]
- Carrilho Galvao, F.; Da Costa Gileno, M.; Olivi Malta, J.; Vicentini, V.; Da Costa Gileno, M.; Anibal, F. Anemia in patients with intestinal parasitic infection. Rev. Ibero-Latinoam Parasitol. 2011, 70, 206–211. [Google Scholar]
- D’Innocenzo, S.; Biagi, C.; Lanari, M. Obesity and the Mediterranean Diet: A Review of Evidence of the Role and Sustainability of the Mediterranean Diet. Nutrients 2019, 11, 1306. [Google Scholar] [CrossRef]
- Berkowitz, S.A.; Hulberg, A.C.; Hong, C.; Stowell, B.J.; Tirozzi, K.J.; Traore, C.Y.; Atlas, S.J. Addressing basic resource needs to improve primary care quality. BMJ Qual. Saf. 2016, 25, 164–172. [Google Scholar] [CrossRef]
- Barrett, M.; Combs, V.; Su, J.G.; Henderson, K.; Tuffli, M.; AIR Louisville Collaborative. AIR Louisville: Addressing asthma with technology, crowdsourcing, cross-sector collaboration, and policy. Health Aff. (Millwood) 2018, 37, 525–534. [Google Scholar] [CrossRef]
- Schickedanz, A.; Hamity, C.; Rogers, A.; Sharp, A.L.; Jackson, A. Clinician experiences and attitudes regarding screening for social determinants of health in a large integrated health system. Med. Care 2019, 57, S197–S201. [Google Scholar] [CrossRef]
- Vest, J.R.; Menachemi, N.; Grannis, S.J.; Ferrell, J.L.; Kasthurirathne, S.N.; Zhang, Y.; Tong, Y.; Halverson, P.K. Impact of risk stratification on referrals and uptake of wraparound services that address social determinants. Am. J. Prev. Med. 2019, 56, e125–e133. [Google Scholar] [CrossRef]
- Buitron de la Vega, P.; Losi, S.; Sprague Martinez, L.; Bovell-Ammon, A.; Garg, A.; James, T.; Ewen, A.M.; Stack, M.; DeCarvalho, H.; Sandel, M.; et al. Implementing an EHR-based screening and referral system to address social determinants of health in primary care. Med. Care 2019, 57, S133–S139. [Google Scholar] [CrossRef]
- Tong, S.T.; Liaw, W.R.; Kashiri, P.L.; Pecsok, J.; Rozman, J.; Bazemore, A.W.; Krist, A.H. Clinician experiences with screening for social needs in primary care. J. Am. Board Fam. Med. 2018, 31, 351–363. [Google Scholar] [CrossRef]
- The American Board of Family Medicine. PRIME Registry. Available online: https://primeregistry.org/ (accessed on 19 December 2019).
- Swinburn, B.A. Obesity prevention: The role of policies, laws and regulations. Aust. New Zealand Health Policy 2008, 5, 12. [Google Scholar] [CrossRef]
- Gortmaker, S.L.; Swinburn, B.A.; Levy, D.; Carter, R.; Mabry, P.L.; Finegood, D.T.; Moodie, M.L. Changing the future of obesity: Science, policy, and action. Lancet 2011, 378, 838–847. [Google Scholar] [CrossRef]
- Mensah, G.A.; Goodman, R.A.; Zaza, S.; Moulton, A.D.; Kocher, P.L.; Dietz, W.H.; Pechacek, T.F.; Marks, J.S. Law as a tool for preventing chronic diseases: Expanding the range of effective public health strategies. Prev. Chronic. Dis. 2004, 1, A13. [Google Scholar]
- Grimes, K.E. Lessons From ACEs: Pay Now or Pay (More) Later. Acad. Pediatr. 2017, 17, S18–19. [Google Scholar] [CrossRef]
- Stock, R.; Goldberg, B.W. Health reform policy to practice. Oregon’s path to a sustainable health system: A study in innovation, 1st ed.; Academic Press: Oxford, UK, 2017; Chapter 7; pp. 101–119. ISBN 012-809-827-9. [Google Scholar]
- Greaves, F.; Rozenblum, R. Chapter 18: Social and Consumer Informatics. In Key Advances in Clinical Informatics. Transforming Health Care Through Health Information Technology; Aziz Sheikh; Elsevier Science: Amsterdam, The Netherlands, 2017; pp. 257–278. [Google Scholar]
- Rose, G.A. The strategy of preventive medicine; Oxford University Press: Oxford, UK, 1992; p. 12. ISBN 0-19-262125-4. [Google Scholar]
| Author, Year | Migrating from | Immigrating to | Study Design | N, Migrant Characteristics | Age | Outcome Disease | Dietary/Cultural Issues | Main Results | QA |
|---|---|---|---|---|---|---|---|---|---|
| Rosas, 2010 [35] | Mexico | USA (California) | cross-sectional | 603 mother-child pairs Mexico-born and California born-children of Mexican descent | 5 year | overweight/obesity | Maternal obesity was a determinant of childhood obesity in both settings; in Mexico, male gender, high SES and low food security were determinants of childhood obesity. | prevalence of childhood obesity is much higher among children of Mexican descent | 13 |
| Kaiser, 2015 [36] | Mexico | USA (rural communities in California) | cohort | 217 children of Latino descent | 2–8 year | overweight/obesity | Preference of american-style foods after children enter the public school system | 51% of children overweight/obese | 14 |
| Kobel, 2017 [37] | anywhere (mostly Turkey and Russia) | Germany | randomized controlled trial | 525 children with migration background | 7.1 ± 0.7 year | obesity | Lower fruit and vegetable consumption, higher screen media time, lower physical activity | children with migrant background: 11.8% overweight/obese (vs 9% non migrant) – 5.7% obesity if migration background | 14 |
| Early 2019 [39] | Hispanic (85%), Black/African (3%) | USA (California) | quasi-randomized controlled trial | 68 children | 10.8 year | overweight/obesity | inadequate fruit and vegetable consumption, excess of sugar-sweetened beverages | overweight prevalence: 11.8%; obesity prevalence: 54.4% | 12 |
| Geremia, 2015 [40] | Italy | Brazil | cross-sectional | 590 Italian immigrant children | 9–18 year | overweight/obesity | Low frequency of consumption of vegetables, more fat foods. | 1) High prevalence of overweight and obesity in this city; 2) factors such as omission of breakfast, overweight and obesity in the mother, age and male gender were associated with excess weight. | 12 |
| Lane, 2018 [22] | Asia, Middle East, Africa, Latin America, Europe o US. | Canada | cross-sectional | 300 immigrant and refugee children | 3–13 year | health status (stunting, overweight/obesity, hypertension, cholesterol levels, health disparities) | Dietary changes (western diet); many immigrants and refugees vulnerable to health disparities | 1) Refugee children are at risk of stunting while immigrants are more at risk of overweight/obesity, especially if they are older and they are from privileged backgrounds in low-income countries; 2) 29% of newcomer children had borderline or elevated blood pressure and 52% high cholesterol levels | 14 |
| Distel, 2019 [41] | Mexico | USA | cohort | 104 Mexican American children | 8.39 year (6-10) | obesity | Food insecurity and chronic stress | Greater food insecurity associated with higher BMI only when children had high levels of hair cortisol | 16 |
| Buscemi, 2011 [42] | Latino | USA | cross-sectional | 63 Latino children | 2–17 year | obesity | Acculturation as a moderator of the relationship between food insecurity and BMI: higher acculturation and high food security associated with lower BMI | Mean BMI percentile significantly higher for immigrants (85) than non immigrants (70); mean BMI percentile 91 for food secure families and 71 for food insecure (s.s.) | 14 |
| Kilanowski, 2012 [43] | Latino | USA | cross-sectional | 60 parent–child dyads of migrant farmworkers | 2–13 year | overweight/obesity | 55% low or very low household food security; surprisingly, children of migrants better than peers concerning fruit and vegetable consumption | 22% overweight, 26% obese; low or very low levels of food security were seen in 48% of children under-normalweight, 75% overweight, 53% obese | 14 |
| Ebenegger, 2011 [44] | Portugal, Albania/Kosovo, other European countries; Africa, Asia, Latin America, other | Switzerland | cross-sectional | 542 children of migrant (71%) and non-migrant parents | 5.1 ± 0.6 year | overweight/obesity | Children of migrant and low education level parents ate more meals and snacks while watching TV, more fatty foods and less fruit | Children of migrant parents had higher weight, BMI and % body fat compared to non-migrant; parental migrant status and educational level independently contributed to adiposity and eating habits | 14 |
| Huang, 2018 [45] | underdeveloped area in China | developed area in China | cross-sectional | 1154, children-caregiver dyads, internal migrants | 11–17 year | overweight/obesity | Levels of acculturation negatively associated with overweight/obesity; children with urban-to-urban migrant caregivers more likely to be overweight/obese than those with rural-to-urban migrant caregivers | 9,7% overweight/obese (> males, >11-13 yrs rather than 14-17 yrs, >urban-to-urban rather than rural-to-urban) | 15 |
| Tsujimoto, 2016 [46] | Mexico, non-hispanic white, non-hispanic black | USA (Boston) | cross-sectional | 28282 foreign-born and US-born children | 2–19 year | overweight/obesity | Obesogenic environment | Prevalences of overweight/obesity lowest in children/adolescents foreign-born and who had been in the US for <1 yr, highest in the US-born (overweight: 23% vs 31.8%, obesity: 8.2% vs16.9%, severe obesity: 2.9% vs 5.4%). Risk of being overweight/obese for US-born vs foreing-born in the US for <1 yr: aOR 2.2 overweight, aOR 3.15 obesity. | 12 |
| Iguacel, 2018 [47] | anywhere | Belgium, Cyprus, Estonia, Germany, Hungary, Italy, Spain, Sweden | cohort | 8624 children of migrant (13,4%) and non-migrant families | 2–9.9 year at baseline 4–11 year after 2 years | overweight/obesity | Partially explained by lifestyle factors (mainly sedentary habits e.g., screen time) | Overweight/obesity at T0: 23.4% migrant origin vs 16.8% native, at T1: 28.5% migrant origin vs 21.5% native (OR 1.3); children with migrant background were more likely to remain o/o after 2 yrs compared to non migrants (OR 1.29) | 15 |
| Labree, 2015 [48] | Turkey, Morocco, other western and not-western countries | Holland (Rotterdam and Eindhoven) | cross-sectional | 1943 immigrant and native parent–child dyads | 8–9 year | overweight/obesity | Low sleep duration, low fruit and high snack intake associated with higher BMIs and prevalence of overweight/obesity; ethnic differences in sleep duration and dietary intake did not have a large impact on ethnic differences in overweight/obesity | children of migrants had ss higher BMI and higher prevalence of ovw/ob, lower prevalence of underweight; higher intake of fruit and vegetables and lower intake of snacks and sweet drinks; lower sleep duration. Less sleep, low fruit intake, and more energy-dense snack consumption correlated with higher BMIs and higher prevalence of overweight and obesity | 13 |
| Besharat Pour, 2014 [49] | anywhere (Africa, Asia, LatinAmerica, Europe excluding Sweden, and Sweden) | Sweden | cohort | 2589 immigrant (22%) and non-immigrant children | 8 year | obesity | Immigrants: higher consumption of fruit/vegetables but also of cakes and sweet | Being overweight and having low physical activity more common among children of immigrant parents (>both immigrant parents) | 13 |
| Chomitz, 2017 [50] | Asian (>Chinese) | USA (Chinatown in Boston) | cross-sectional | 132 Asian American children | 4.9 year (3.5–6) | obesity | Perceived parents’ barriers: 1) worry about safety when child plays outside 2) healthy food too expensive | 32.6% overweight/obese (vs 23.4% overall USA and 9% Asians) - children of less acculturated parents, more likely with lower income or recent immigrants, were 3,5 times more likely to be overweight/obese than those of more acculturated parents - more acculturated more likely to provide fruits daily or more but also more sugary snacks | 14 |
| Alasagheirin, 2018 [51] | Sudan | USA | cross-sectional | 64 immigrant and refugee Sudanese children | 5–18 year | growth, body composition, metabolic risk, physical activity and food security | Food insecurity in 40% of families, sedentary habits reported by many | 32% obese, 46% low lean mass; high cholesterol 23%, high triglycerides 32%, high insulin resistance 15% (correlates with high risk of diabetes and cardiovascular problem); Low bone mass which could contribute to osteoporosis | 13 |
| Tovar, 2012 [52] | Haiti, Latin America, Brazil | USA | randomized controlled trial | 383 mother-child dyads | mothers 20–55 year, children 3–12 year | overweight/obesity | A low demanding/high responsive feeding style is significantly and positively associated with higher child weight. | 72% of mothers and 43% of children overweight/obese. Fifteen percent of mothers reported their feeding style as being high demanding/high responsive; 32% as being high demanding/low responsive; 34% as being low demanding/high responsive and 18% as being low demanding/low responsive. | 18 |
| Cheah, 2012 [53] | China, Korea | USA | cross-sectional | 130 children of first-generation immigrants from China (62%) and Korea (38%) | 3–8 year | obesity | Parents’ food insecurity in their childhood associated with obesity-promoting behaviors and outcomes | 20% overweight/obese; parents with food insecurity in childhood: 1) evaluated their children weighing less than ideal 2) allowed more servings of soda and sweets; early life material deprivation: 1) less concern about children’s diets, 2) less concern child eating too much or becoming overweight | 14 |
| Cook, 2017 [54] | Asia | USA (California) | cohort | 1525 Asian American adolescents | 12–17 year | overweight/obesity | The two lifestyle factors (i.e., physical activity and fast food consumption) were not associated with overweight/obesity | Overweight/obesity rate higher among those with lower (24.7%) than higher (13.4%) family incomes; higher among those in the low-SES (29.0%) than middle/high-level SES ethnic groups (11.6% and 12.8%, respectively). By ethnicity, overweight/obesity lowest among Japanese (4.8%) and highest among Filipino (26.3%) and Southeast Asians (25.5%). Adolescents in high-middle SES were far less likely to be overweight or obese than those in low SES: this was more pronounced for foreign-born adolescents vs US-born. | 14 |
| Zulfiqar, 2018 [55] | HIC and LMIC | Australia | cross-sectional | 4115 children originating from Australia (58%), HIC (30%), LMIC (12%) | 4–11 year | overweight/obesity | Higher intake of both vegetables and sugar-sweetened-beverages, higher inclination toward sedentary activities and lower organized sports participation. | Higher overweight/obesity rates in immigrants from LMIC (LMIC/HIC/Australian %: boys 30/23/22, girls 35/22/24) and higher in second-generation | 15 |
| Iriart, 2011 [56] | Hispanic | USA | cross-sectional | 3102 Hispanic (38%) and non-Hispanic children | 2–19 year | stunting | Hispanics more likely to be less than full food secure (30.5% vs 11.8%); hispanics with normal weight were more likely to be fully food secure | Hispanics: highest proportion of stunting (6.6%), overweight/obesity (39.3%), stunting among normal weight (7%), stunting among overweight/obese (6%) compared to non-hispanic whites, non-hispanic blacks, other races; tendency for overweight/obesity in hispanic children who face adverse socioeconomic conditions to experience a higher prevalence of stunting | 15 |
| Choudhary, 2009 [57] | 44% rural, 51% urban | Mumbai city | cross-sectional | 481 internal migrant children | <3 year | stunting, underweight, wasting | poverty | Stunting and low mother-BMI >in migrants with high disadvantage for rural migrants; as the years in Mumbai increase, migrants learn to assimilate to the new environment and the disadvantage compared to non-migrants declines | 15 |
| Lee, 2015 [58] | North Korea | South Korea | cohort | 70 immigrant children | 6–15 year | stunting and obesity | Those who lived in South Korea longer were less likely to be currently stunted | At entry 11.4% stunted and only 5.7% after 2 years. The prevalence of obesity was similar to that of SK children. The likelihood of remaining stunted was significantly associated with older age and shorter residency in SK. The was no significant association with food security situation at birth. | 14 |
| Werneck, 2008 [59] | Portugal, Brazil, Angola, Mozambique, Azores | Canada (Toronto) | case-control | 104 immigrant children | ≤48 months | Early childhood caries | Immigrants have difficulty in obtaining dental care primarily; factors that correlated the most with early childhood caries were family without dental insurance, lack of a family dentist, and frequency of snack consumption. | 35% early childhood caries | 15 |
| Vatanparast, 2013 [60] | Asia, Africa, Middle East and Latin America | Canada | cross-sectional | 72 children (33 immigrant and 39 refugee) | 6–11 year | vitamin D deficiency | Calcium intake inadequacy 74% in migrants and 77% in refugees, vitamin D intake inadequacy 81% in migrants and 97% in refugees | Serum vitamin D deficiency/inadequacy in 63% of migrants and 80% of refugees | 12 |
| Sacri, 2017 [61] | anywhere | France | cross-sectional | 657 immigrant (14%) and non-immigrant (86%) children | 3.9 year (<6) | iron deficiency | Male gender, mother being a migrant, underprivileged family status and low maternal education were related to ID | Significantly associated with mother being a migrant: low serum ferritinemia (32.1 mcg/L vs 44.9) and iron deficiency (7% vs 2%); iron deficiency prevalence 2.8% to 3.2% depending on serum ferritin threshold of 10 or 12 µg/L. | 15 |
| Saunders, 2016 [62] | from industrialized and not industrialized countries (especially from Europe) | Canada | cross-sectional | 2614 children (47.6% immigrant) | 12–72 month | iron deficiency | Younger age, male sex, high cow’s milk intake, longer breastfeeding duration associated with lower serum ferritin | No association between family immigrant status and iron status, no need for iron supplementation in immigrants’ children | 15 |
| Kim, 2006 [63] | Latin America | USA (Rural Nebraska) | cohort | 29 Latino immigrant children | 4–8 year | micronutrients deficiency (plasma concentrations of vitamin E, vitamin C, selenium and carotenoids) | 59% reported consuming less than the Estimated Average Requirement for vitamin E; in general, consumption of the Recommended Dietary Allowances for vitamin C and selenium | 69% vitamin E inadequacy; in general, normal levels of vitamin C and selenium. | 13 |
| Author, Year | Study Design | Blinding | Selection Bias | Data Collection | Confounding | Withdrawal and Drop-Outs | Overall Rating |
|---|---|---|---|---|---|---|---|
| Rosas 2010 [35] | 1 | 2 | 3 | 3 | 3 | 1 | 13 |
| Kaiser 2015 [36] | 1 | 2 | 3 | 3 | 3 | 2 | 14 |
| Kobel 2017 [37] | 2 | 2 | 3 | 3 | 2 | 2 | 14 |
| Early 2019 [39] | 1 | 2 | 3 | 3 | 2 | 1 | 12 |
| Geremia 2015 [40] | 1 | 2 | 2 | 3 | 2 | 2 | 12 |
| Lane 2018 [22] | 1 | 2 | 3 | 3 | 3 | 2? | 14 |
| Distel 2019 [41] | 2 | 2 | 3 | 3 | 3 | 3 | 16 |
| Buscemi 2011 [42] | 1 | 2 | 3 | 3 | 3 | 2 | 14 |
| Kilanowski 2012 [43] | 1 | 2 | 3 | 3 | 3 | 2 | 14 |
| Ebenegger 2011 [44] | 1 | 2 | 3 | 3 | 3 | 2 | 14 |
| Huang 2018 [45] | 1 | 2 | 3 | 3 | 3 | 3 | 15 |
| Tsujimoto 2016 [46] | 1 | 2 | 3 | 3 | 2 | 1 | 12 |
| Iguacel 2018 [47] | 1 | 2 | 3 | 3 | 3 | 3 | 15 |
| Labree 2015 [48] | 1 | 2 | 2 | 3 | 2 | 3 | 13 |
| Besharat Pour 2014 [49] | 1 | 2 | 3 | 3 | 2 | 2 | 13 |
| Chomitz 2017 [50] | 1 | 2 | 3 | 3 | 2 | 3 | 14 |
| Alasagheirin 2018 [51] | 1 | 2 | 3 | 3 | 2 | 3 | 13 |
| Tovar 2012 [52] | 3 | 3 | 3 | 3 | 3 | 3 | 18 |
| Cheah 2012 [53] | 1 | 2 | 3 | 3 | 3 | 2 | 14 |
| Cook 2017 [54] | 1 | 2 | 3 | 3 | 3 | 2 | 14 |
| Zulfiqar 2018 [55] | 2 | 2 | 3 | 3 | 2 | 3 | 15 |
| Iriart 2011 [56] | 1 | 2 | 3 | 3 | 3 | 3 | 15 |
| Choudhary 2009 [57] | 2 | 2 | 3 | 3 | 2 | 3 | 15 |
| Lee 2015 [58] | 2 | 2 | 3 | 3 | 2 | 2 | 14 |
| Werneck 2008 [59] | 2 | 3 | 3 | 3 | 3 | 1 | 15 |
| Vatanparast 2013 [60] | 1 | 2 | 3 | 3 | 2 | 1 | 12 |
| Sacri 2017 [61] | 1 | 2 | 3 | 3 | 3 | 3 | 15 |
| Saunders 2016 [62] | 1 | 2 | 3 | 3 | 3 | 3 | 15 |
| Kim 2006 [63] | 1 | 2 | 3 | 3 | 2 | 2 | 13 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dondi, A.; Piccinno, V.; Morigi, F.; Sureshkumar, S.; Gori, D.; Lanari, M. Food Insecurity and Major Diet-Related Morbidities in Migrating Children: A Systematic Review. Nutrients 2020, 12, 379. https://doi.org/10.3390/nu12020379
Dondi A, Piccinno V, Morigi F, Sureshkumar S, Gori D, Lanari M. Food Insecurity and Major Diet-Related Morbidities in Migrating Children: A Systematic Review. Nutrients. 2020; 12(2):379. https://doi.org/10.3390/nu12020379
Chicago/Turabian StyleDondi, Arianna, Valentina Piccinno, Francesca Morigi, Sugitha Sureshkumar, Davide Gori, and Marcello Lanari. 2020. "Food Insecurity and Major Diet-Related Morbidities in Migrating Children: A Systematic Review" Nutrients 12, no. 2: 379. https://doi.org/10.3390/nu12020379
APA StyleDondi, A., Piccinno, V., Morigi, F., Sureshkumar, S., Gori, D., & Lanari, M. (2020). Food Insecurity and Major Diet-Related Morbidities in Migrating Children: A Systematic Review. Nutrients, 12(2), 379. https://doi.org/10.3390/nu12020379








