Eating Behavior (Duration, Content, and Timing) Among Workers Living under Different Levels of Urbanization
Abstract
1. Introduction
2. Methods
2.1. Population
2.2. Ethical Aspects
2.3. Data Collection
2.4. Statistical Analysis
3. Results
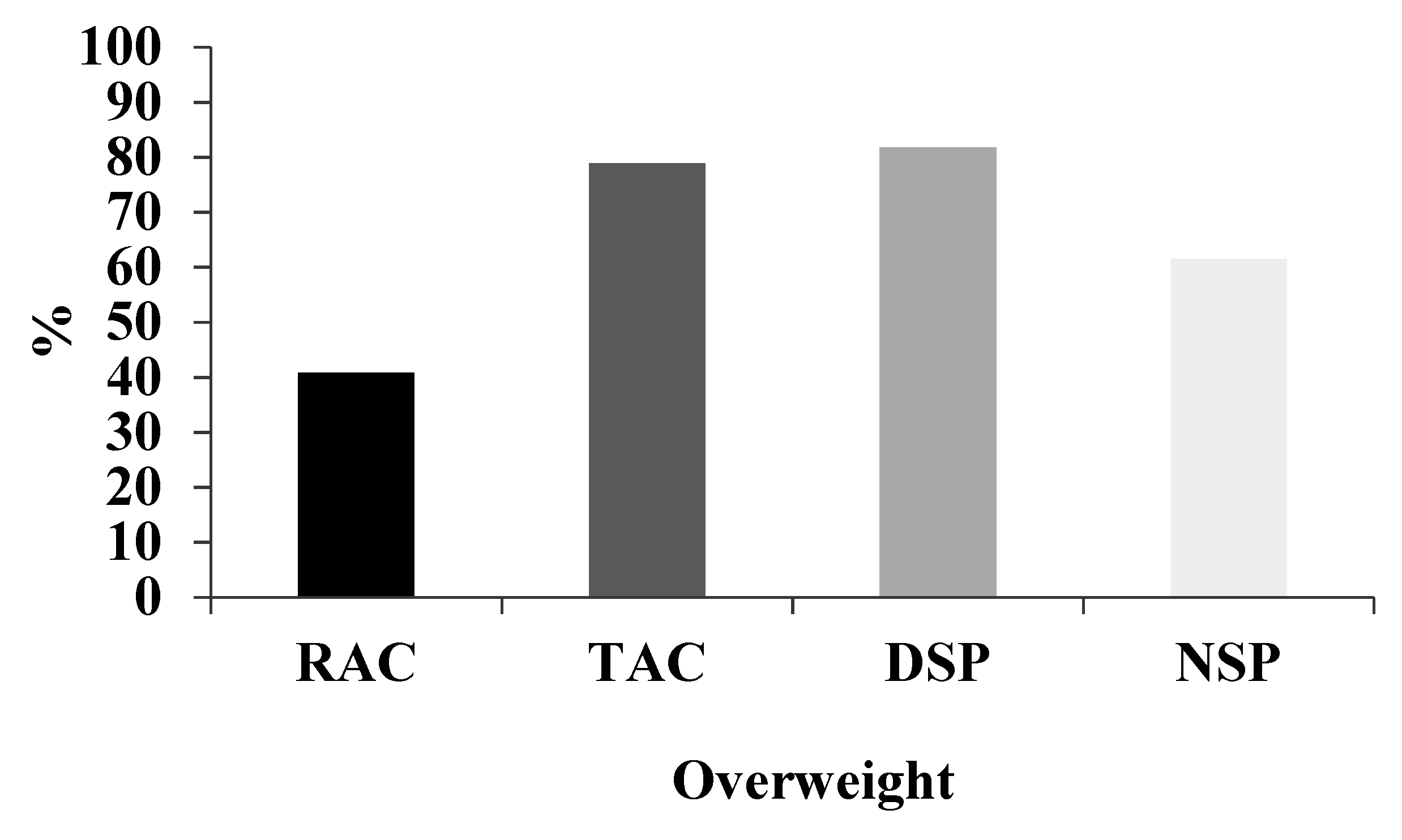
3.1. Sociodemographic and Anthropometric Characteristics
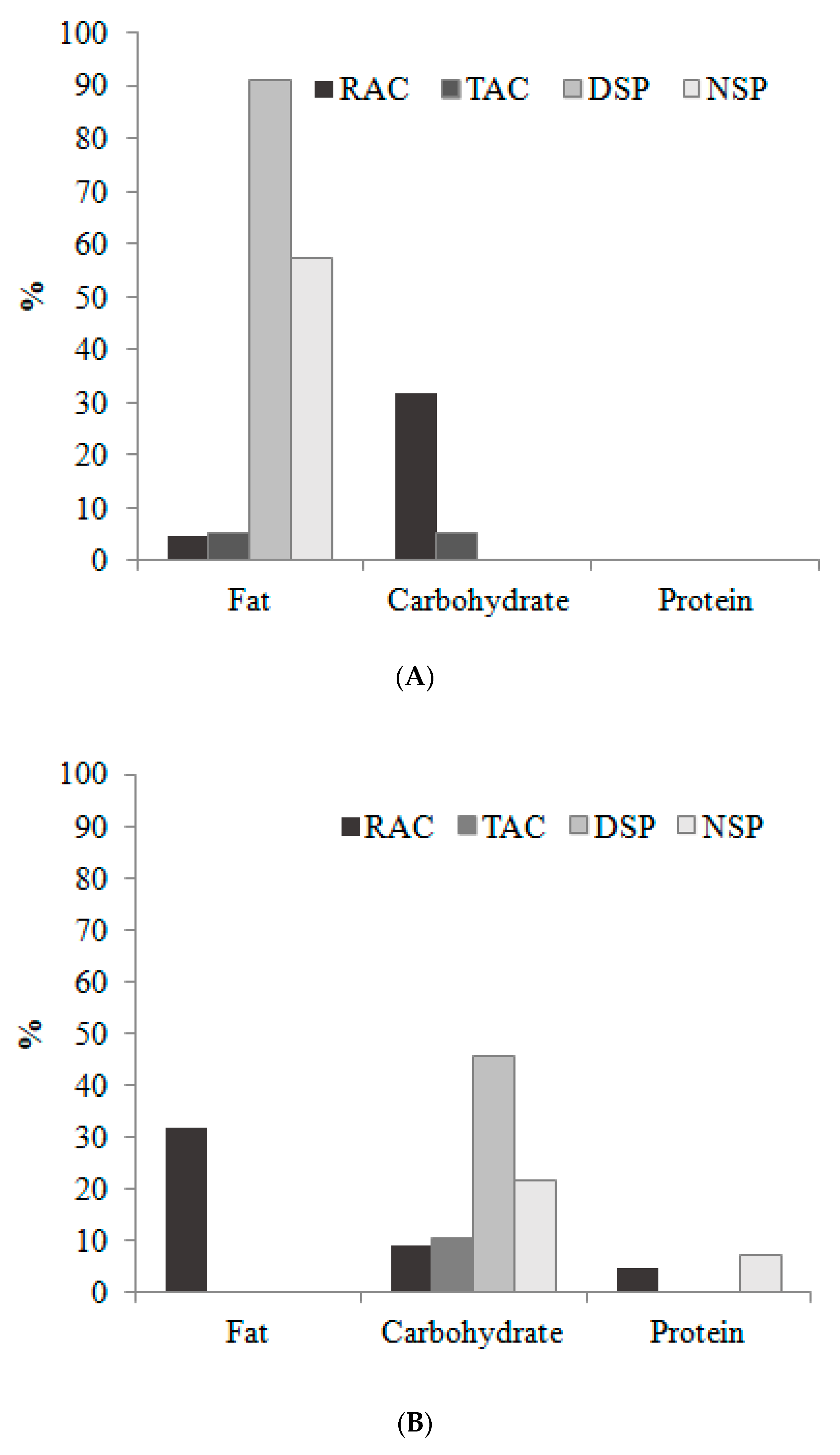
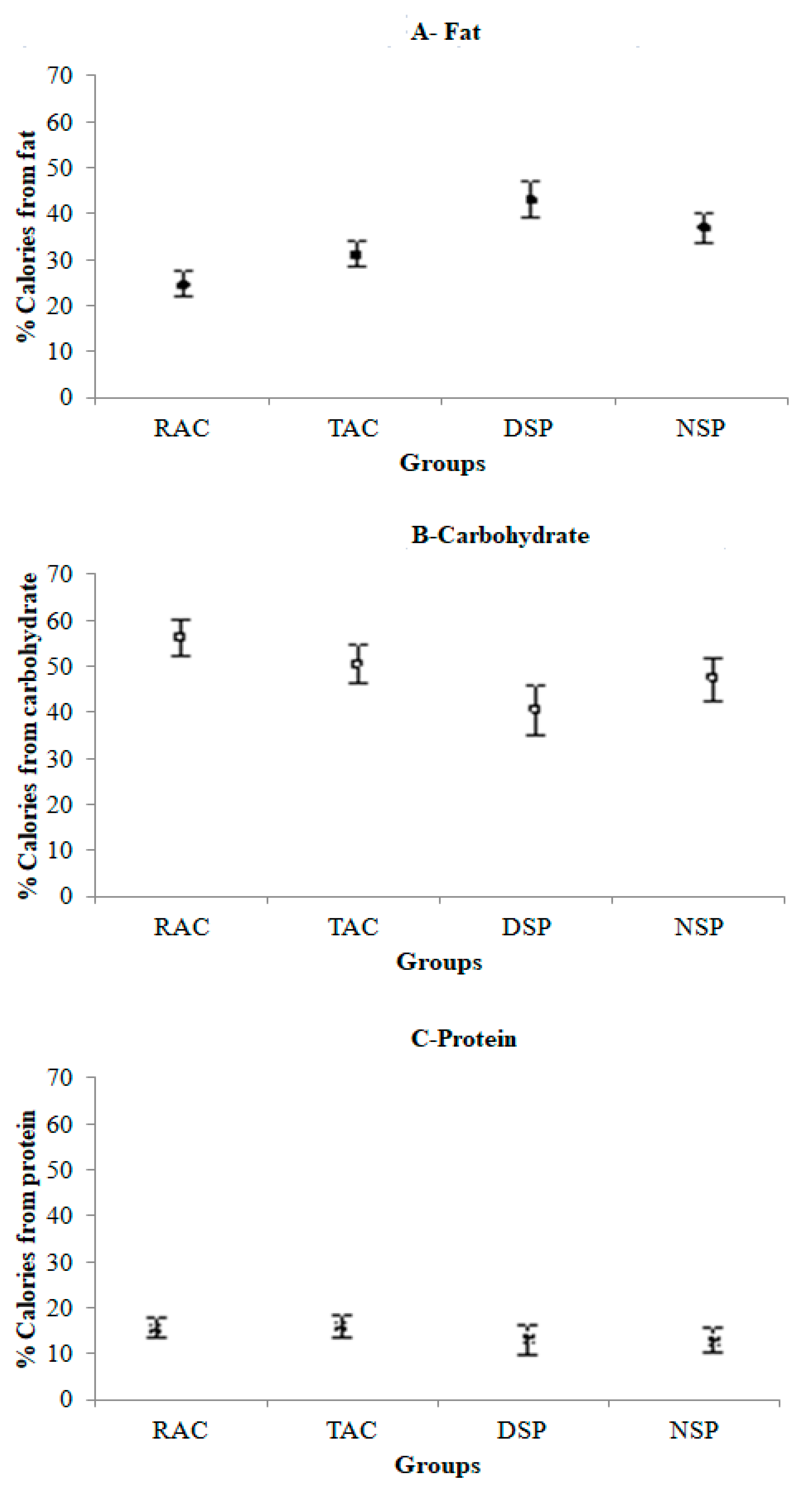
3.2. Energy and Macronutrient Consumption
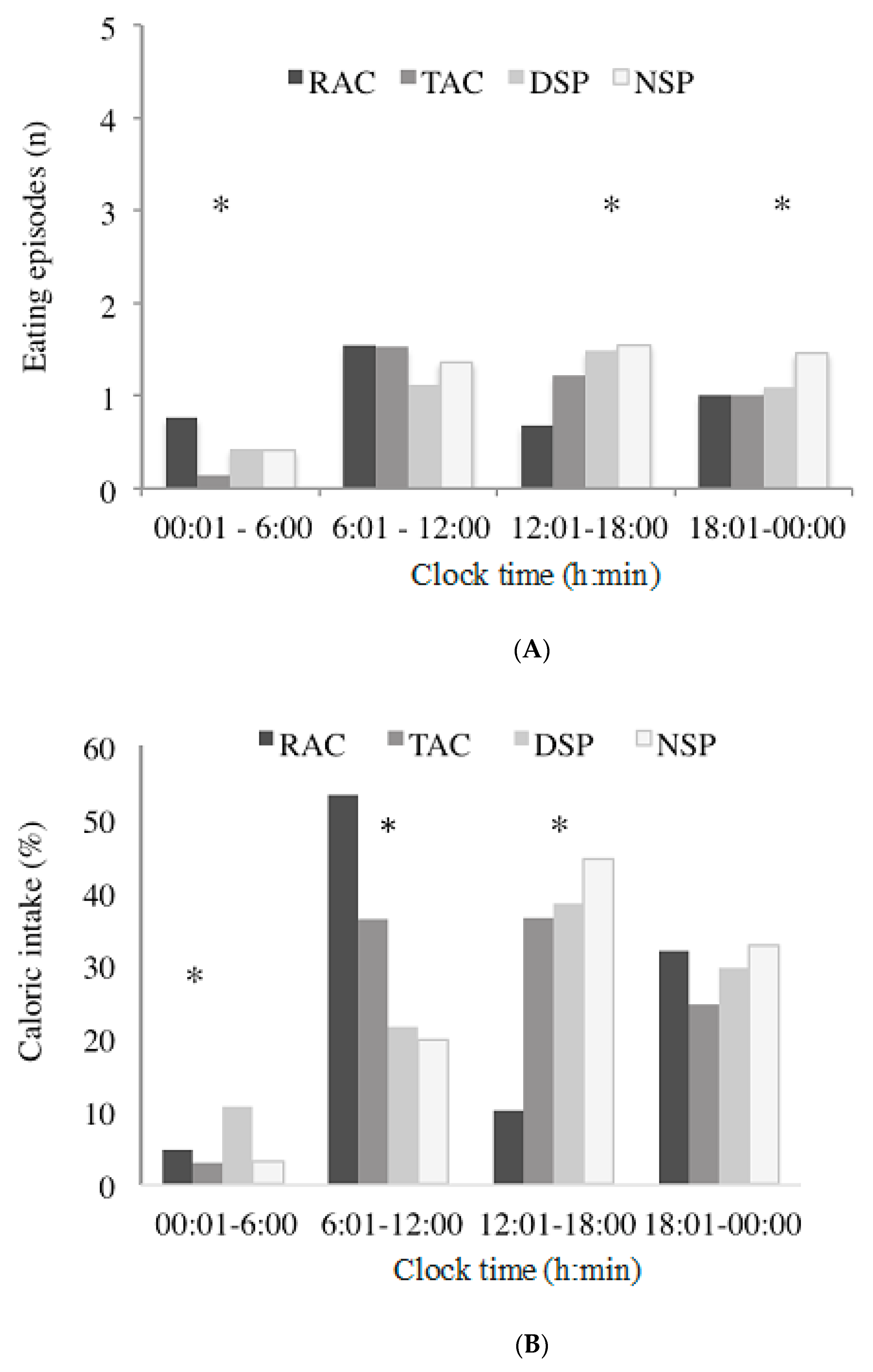
3.3. Eating Duration and Timing
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Green, A.; Cohen-Zion, M.; Haim, A.; Dagan, Y. Evening light exposure to computer screens disrupts human sleep, biological rhythms, and attention abilities. Chronobiol. Int. 2017, 34, 855–865. [Google Scholar] [CrossRef]
- Wright, K.P., Jr.; McHill, A.W.; Birks, B.R.; Griffin, B.R.; Rusterholz, T.; Chinoy, E.D. Entrainment of the human circadian clock to the natural light-dark cycle. Curr. Biol. 2013, 23, 1554–1558. [Google Scholar] [CrossRef]
- Beale, A.D.; Pedrazzoli, M.; Gonçalves, B.S.B.; Beijamini, F.; Duarte, N.E.; Egan, K.J.; Knutson, K.L.; von Schantz, M.; Roden, L.C. Comparison between an African town and a neighbouring village shows delayed, but not decreased, sleep during the early stages of urbanisation. Sci. Rep. 2017, 7, 5697. [Google Scholar] [CrossRef] [PubMed]
- De La Iglesia, H.O.; Fernández-Duque, E.; Golombek, D.A.; Lanza, N.; Duffy, J.F.; Czeisler, C.A.; Valeggia, C.R. Access to electric light is associated with shorter sleep duration in a traditionally hunter-gatherer community. J. Biol. Rhythms. 2015, 30, 342–350. [Google Scholar] [CrossRef] [PubMed]
- Moreno, C.R.C.; Vasconcelos, S.; Marqueze, E.C.; Lowden, A.; Middleton, B.; Fischer, F.M.; Louzada, F.M.; Skene, D.J. Sleep patterns in Amazon rubber tappers with and without electric light at home. Sci. Rep. 2015, 5, 14074. [Google Scholar] [CrossRef] [PubMed]
- Pilz, L.K.; Levandovski. R.; Oliveira, M.A.B.; Hidalgo, M.P.; Roenneberg, T. Sleep and light exposure across different levels of urbanization in Brazilian communities. Sci. Rep. 2018, 8, 11389. [Google Scholar] [CrossRef] [PubMed]
- Mota, M.C.; Silva, C.M.; Balieiro, L.C.T.; Fahmy, W.M.; Crispim, C.A. Social jetlag and metabolic control in non-communicable chronic diseases: A study addressing different obesity statuses. Sci. Rep. 2017, 25, 6358. [Google Scholar] [CrossRef]
- Sharma, A.; Laurenti, M.C.; Dalla Man, C.; Varghese, R.T.; Cobelli, C.; Rizza, R.A.; Matveyenko, A.; Vella, A. Glucose metabolism during rotational shift-work in healthcare workers. Diabetologia 2017, 60, 1483–1490. [Google Scholar] [CrossRef]
- Spaeth, A.M.; Dinges, D.F.; Goel, N. Effects of experimental sleep restriction on weight gain, caloric intake, and meal timing in healthy adults. Sleep 2013, 36, 981–990. [Google Scholar] [CrossRef]
- Kecklund, G.; Axelsson, J. Health consequences of shift work and insufficient sleep. BMJ 2016, 355, i5210. [Google Scholar] [CrossRef]
- Hoevenaar-Blom, M.P.; Spijkerman, A.M.; Kromhout, D.; Van Den Berg, J.F.; Verschuren, W.M. Sleep duration and sleep quality in relation to 12 years cardiovascular disease incidence: The Morgen study. Sleep 2011, 34, 1487–1492. [Google Scholar] [CrossRef] [PubMed]
- Barger, L.K.; Rajaratnam, S.M.W.; Cannon, C.P.; Lukas, M.A.; Im, K.; Goodrich, E.L.; Czeisler, C.A.; O’Donoghue, M.L. Short sleep duration, obstructive sleep apnea, shiftwork, and the risk of adverse cardiovascular events in patients after an acute coronary syndrome. J. Am. Heart Assoc. 2017, 6, e006959. [Google Scholar] [CrossRef] [PubMed]
- Bass, J.; Takahashi, J.S. Circadian integration of metabolism and energetics. Science 2010, 330, 1349–1354. [Google Scholar] [CrossRef]
- Gifkins, J.; Johnston, A.; Loudoun, R. The impact of shift work on eating patterns and self-care strategies utilised by experienced and inexperienced nurses. Chronobiol. Int. 2018, 35, 811–820. [Google Scholar] [CrossRef] [PubMed]
- Lowden, A.; Moreno, C.R.C.; Holmbäck, U.L.F.; Lennernäs, M.; Tucker, P. Eating and shift work-effects on habits, metabolism, and performance. Scand. J. Work Environ. Health 2010, 36, 150–162. [Google Scholar] [CrossRef] [PubMed]
- McHill, A.W.; Phillips, A.J.; Czeisler, C.A.; Keating, L.; Yee, K.; Barger, L.K.; Garaulet, M.; Scheer, F.A.; Klerman, E.B. Later circadian timing of food intake is associated with increased body fat. Am. J. Clin. Nutr. 2017, 106, 1213–1219. [Google Scholar] [CrossRef] [PubMed]
- Jakubowicz, D.; Barnea, M.; Wainstein, J.; Froy, O. High caloric intake at breakfast vs. dinner differentially influences weight loss of overweight and obese women. Obesity 2013, 21, 2504–2512. [Google Scholar] [CrossRef]
- Leung, G.K.W.; Huggins, C.E.; Bonham, M.P. Effect of meal timing on postprandial glucose responses to a low glycemic index meal: A crossover trial in healthy volunteers. Clin. Nutr. 2019, 38, 465–471. [Google Scholar] [CrossRef]
- Sopowski, M.J.; Hampton, S.M.; Ribeiro, D.C.; Morgan, L.; Arendt, J. Postprandial triacylglycerol responses in simulated night and day shift: Gender differences. J. Biol. Rhythm. 2001, 16, 272–276. [Google Scholar] [CrossRef]
- Johnston, J.D. Physiological responses to food intake throughout the day. Nutr. Res. Rev. 2014, 27, 107–118. [Google Scholar] [CrossRef]
- Spiegel, K.; Tasali, E.; Leproult, R.; van Calter, E. Effects of poor and short sleep on glucose metabolism and obesity risk. Na.t Rev. Endocrinol. 2009, 5, 253–261. [Google Scholar] [CrossRef] [PubMed]
- Sherman, H.; Genzer, Y.; Cohen, R.; Chapnik, N.; Madar, Z.; Froy, O. Timed high-fat diet resets circadian metabolism and prevents obesity. FASEB J. 2012, 26, 3493–3502. [Google Scholar] [CrossRef] [PubMed]
- Rothschild, J.; Hoddy, K.K.; Jambazian, P.; Varady, K.A. Time-restricted feeding and risk of metabolic disease: A review of human and animal studies. Nutr. Rev. 2014, 72, 308–318. [Google Scholar] [CrossRef] [PubMed]
- Melkani, G.C.; Panda, S. Time restricted feeding for prevention and treatment of cardiometabolic disorders. J. Physiol. 2017, 595, 3691–3700. [Google Scholar] [CrossRef]
- Njelekela, M.A.; Liu, E.; Mpembeni, R.; Muhihi, A.; Mligiliche, N.; Spiegelman, D.; Finkelstein, J.L.; Fawzi, W.W.; Willett, W.C.; Mtabaji, J. Socio-economic status, urbanization, and cardiometabolic risk factors among middle-aged adults in Tanzania. East. Afr. J. Public Health 2011, 8, 216–223. [Google Scholar]
- IBGE. Xapuri. Available online: https://cidades.ibge.gov.br/brasil/ac/xapuri/panorama (accessed on 3 June 2018).
- WHO (Word Health Organization). Obesity and overweight. Available online: http://www.who.int/mediacentre/factsheets/fs311/en/ (accessed on 3 February 2018).
- Fisberg, R.M.; Slater, B.; Marchioni, D.M.L.; Martini, L.A. Inquéritos Alimentares. Métodos e Bases Científicos, 1st ed.; Manole: Barueri, SP, Brasil, 2005; pp. 150–155. ISBN 9788520416389. [Google Scholar]
- Pinheiro, A.B.V.; Lacerda, E.M.A.; Gomes, M.C.S.; Costa, V.M. Tabela para Avaliação de Consumo Alimentar em Medidas Caseiras, 4th ed.; Atheneu: São Paulo, SP, Brasil, 2000; ISBN 9788573796780. [Google Scholar]
- Fisberg, R.M.; Marchioni, D.M.L. Manual de avaliação do consumo alimentar em estudos populacionais: A experiência do inquérito de saúde em São Paulo, 1st ed.; Faculdade de Saúde Pública da USP: São Paulo, SP, Brasil, 2014; ISBN 978-85-88848-10-8. [Google Scholar]
- NDSR Software. NCC—Nutrition Coordinating System. Available online: http://license.umn.edu/technologies/ndsr87072_nutrition-data-system-for-research-nutritional-analysis-software (accessed on 21 July 2018).
- Universidade Estadual de Campinas—UNICAMP. Tabela Brasileira de Composição de Alimentos—TACO, 4th ed.; UNICAMP/NEPA: Campinas, SP, Brasil, 2011. [Google Scholar]
- Gill, S.; Panda, S. A smartphone app reveals erratic diurnal eating patterns in humans that can be modulated for health benefits. Cell Metab. 2015, 22, 789–798. [Google Scholar] [CrossRef]
- Pasqua, I.C.; Moreno, C.R.C. The nutritional status and eating habits of shift workers: A chronobiological approach. Chronobiol. Int. 2004, 21, 949–959. [Google Scholar] [CrossRef]
- Castro, J.M. The time of day of food intake influences overall intake in humans. J. Nutr. 2004, 134, 104–111. [Google Scholar] [CrossRef]
- Nascer e pôr do sol Xapuri, Brasil. Available online: https://www.sunrise-and-sunset.com/pt (accessed on 20 June 2018).
- Institute of Medicine. Dietary Reference Intakes Estimated Average Requirements for Groups; National Academy Press: Washington, DC, USA, 2014. Available online: https://www.nal.usda.gov/sites/default/files/fnic_uploads/DRIEssentialGuideNutReq.pdf (accessed on 1 June 2018).
- Yoshida, J.; Eguchi, E.; Nagaoka, K.; Ito, T.; Ogino, K. Association of night eating habits with metabolic syndrome and its components: A longitudinal study. BMC Public Health 2018, 18, 1366. [Google Scholar] [CrossRef]
- Collado, M.C.; Engen, P.A.; Bandín, C.; Cabrera-Rubio, R.; Voigt, R.M.; Green, S.J.; Naqib, A.; Keshavarzian, A.; Scheer, F.A.J.L.; Garaulet, M. Timing of food intake impacts daily rhythms of human salivary microbiota a randomized, crossover study. FASEB J. 2018, 32, 2060–2072. [Google Scholar] [CrossRef]
- Voigt, R.M.; Forsyth, C.B.; Green, S.J.; Mutlu, E.; Engen, P.; Vitaterna, M.H.; Turek, F.W.; Keshavarzian, A. Circadian disorganization alters intestinal microbiota. PLoS ONE 2014, 9, e97500. [Google Scholar] [CrossRef] [PubMed]
- Ma, Y.; Bertone, E.R.; Stanek, E.J.; Reed, G.W.; Hebert, J.R.; Cohen, N.L.; Merriam, P.A.; Ockene, I.S. Association between eating patterns and obesity in a free-living US adult population. Am. J. Epidemiol. 2003, 158, 85–92. [Google Scholar] [CrossRef] [PubMed]
- Colles, S.L.; Dixon, J.B.; O’Brien, P.E. Night eating syndrome and nocturnal snacking: Association with obesity, binge eating and psychological distress. Int. J. Obes. 2007, 31, 1722–1730. [Google Scholar] [CrossRef] [PubMed]
- Arble, D.M.; Bass, J.; Laposky, A.D.; Vitaterna, M.H.; Turek, F.W. Circadian timing of food intake contributes to weight gain. Obesity 2009, 17, 2100–2102. [Google Scholar] [CrossRef]
- Guerrero-Vargas, N.N.; Espitia-Bautista, E.; Buijis, R.M.; Escobar, C. Shift-work: Is time of eating determining metabolic health? Evidence from animal models. Proc. Nutr. Soc. 2018, 77, 199–215. [Google Scholar] [CrossRef]
- Wehrens, S.M.T.; Christou, S.; Isherwood, C.; Middleton, B.; Gibbs, M.A.; Archer, S.N.; Skene, D.J.; Johnston, J.D. Meal timing regulates the human circadian system. Curr. Biol. 2017, 27, 1768–1775. [Google Scholar] [CrossRef]
- Rombaldi, A.J.; Silva, M.C.; Neutzling, M.B.; Azevedo, R.A.; Hallal, P.C. Fatores associados ao consumo de dietas ricas em gordura em adultos de uma cidade no sul do Brasil. Rev. Ciênc. Saúde Coletiva 2014, 19, 1513–1521. [Google Scholar] [CrossRef]
- Martins, A.J.; Vasconcelos, S.P.; Skene, D.J.; Lowden, A.; Moreno, C.R.C. Effects of physical activity at work and life-style on sleep in workers from an Amazonian extractivist reserve. Sleep Sci. 2016, 9, 289–294. [Google Scholar] [CrossRef]
- Martins, A.J. Effects of Urbanization on Biological Rhythms and Metabolic Repercussions on the Health of Workers in an Amazonian Community. Ph.D. Thesis, School of Public Health of the USP, São Paulo, Brasil, 2018. [Google Scholar]
- Batista Filho, M.; Souza, A.I.; Miglioli, T.C.; Santos, M.C. Anemia and obesity: A paradox of the nutritional transition in Brazil. Cad. Saúde Públ. 2008, 24, 247–257. [Google Scholar] [CrossRef][Green Version]
- Moreno, C.R.C.; Marqueze, E.C.; Sargent, C.; Wright, K.P., Jr.; Ferguson, S.A.; Tucker, P. Working Time Society consensus statements: Evidence-based effects of shift work on physical and mental health. Ind. Health 2019, 57, 139–157. [Google Scholar] [CrossRef]
- Grundy, A.; Cotterchio, M.; Kirsh, V.A.; Nadalin, V.; Lightfoot, N.; Kreiger, N. Rotating shift work associated with obesity in men from northeastern Ontario. Health Promot. Chronic Dis. Prev. Can. 2017, 37, 238–247. [Google Scholar] [CrossRef] [PubMed]
- Chin, D.L.; Nam, S.; Lee, S.J. Occupational factors associated with obesity and leisure-time physical activity among nurses: A cross sectional study. Int. J. Nurs. Stud. 2016, 57, 60–69. [Google Scholar] [CrossRef] [PubMed]
- Sun, M.; Feng, W.; Wang, F.; Zhang, L.; Wu, Z.; Li, Z.; Zhang, B.; He, Y.; Xie, S.; Li, M.; et al. Night shift work exposure profile and obesity: Baseline results from a Chinese night shift worker cohort. PLoS ONE 2018, 13, e0196989. [Google Scholar] [CrossRef] [PubMed]
- Schiavo-Cardozo, D.; Lima, M.M.; Pareja, J.C.; Geloneze, B. Appetite-regulating hormones from the upper gut: Disrupted control of xenin and ghrelin in night workers. Clin. Endocrinol. 2013, 79, 807–811. [Google Scholar] [CrossRef] [PubMed]
- Hemio, K.; Puttonen, S.; Viitasalo, K.; Härmä, M.; Peltonen, M.; Lindstrom, J. Food and nutrient intake among workers with different shift systems. Occup. Environ. Med. 2015, 72, 513–520. [Google Scholar] [CrossRef] [PubMed]
- Lordan, R.; Tsoupras, A.; Mitra, B.; Zabetakis, I. Dairy fats and cardiovascular disease: Do we really need to be concerned? Foods 2018, 7, 29. [Google Scholar] [CrossRef]
- Instituto Brasileiro de Geografia e Estatística - IBGE. Pesquisa de orçamentos familiares 2008–2009: Análise do consumo alimentar pessoal no Brasil, 1st ed.; Instituto Brasileiro de Geografia e Estatística: Rio de Janeiro, RJ, Brasil, 2011; ISBN 978-85-240-4198-3. [Google Scholar]
- Fonseca, A.B.; Souza, T.S.N.; Frozi, D.S.; Pereira, R.A. Modernidade alimentar e consumo de alimentos: Contribuições sócio-antropológicas para a pesquisa em nutrição. Ciênc. Saúde Coletiva. 2016, 16, 3853–3862. [Google Scholar] [CrossRef]
- Defante, L.R.; Nascimento, L.D.O.; Lima-Filho, D.O. Comportamento de consumo de alimentos de famílias de baixa renda de pequenas cidades brasileiras: O caso de Mato Grosso do Sul. Interações 2015, 16, 265–276. [Google Scholar] [CrossRef][Green Version]
- Jaime, P.C.; Santos, L.M.P. Transição nutricional e a organização do cuidado em alimentação e nutrição na atenção básica em saúde. Divulg Saúde Debate 2014, 51, 72–85. [Google Scholar]
- Instituto Brasileiro de Geografia e Estatística (IBGE). Pesquisa de Orçamentos Familiares 2008–2009. Aquisição Alimentar Domiciliar Per Capita Brasil e Grandes Regiões: Comentários dos Resultados, 1st ed.; IBGE: Rio de Janeiro, RJ, Brasil, 2008; ISBN 978-85-240-4168-6. [Google Scholar]
- Roskoden, F.C.; Krüger, J.; Storck, L.J.; Gärtner, S. Physical activity, energy expenditure, nutritional habits, quality of sleep and stress levels in shift-working health care personnel. PLoS ONE 2017, 12, e0169983. [Google Scholar] [CrossRef]
- Heath, G.; Coates, A.; Sargent, C.; Dorrian, J. Sleep duration and chronic fatigue are differently associated with the dietary profile of shift workers. Nutrients 2016, 8, 771. [Google Scholar] [CrossRef] [PubMed]
- Balieiro, L.C.; Rossato, L.T.; Waterhouse, J.; Paim, S.L.; Mota, M.C.; Crispim, C.A. Nutritional status and eating habits of bus drivers during the day and night. Chronobiol. Int. 2014, 31, 1123–1129. [Google Scholar] [CrossRef] [PubMed]
- Barros, G.S.; Meneses, J.N.C.; Silva, J.A. Representações sociais do consumo de carne em Belo Horizonte. Physis Revista de Saúde Coletiva. 2012, 22, 365–383. [Google Scholar] [CrossRef]
- Monteiro, C.; Levy, R.; Claro, R.; De Castro, I.; Cannon, G. Increasing consumption of ultra-processed foods and likely impact on human health: Evidence from Brazil. Public Health Nutr. 2010, 14, 5–13. [Google Scholar] [CrossRef] [PubMed]
- Simões, B.S.; Barreto, S.M.; Molina, M.C.B.; Luft, V.C.; Duncan, B.B.; Schmidt, M.I.; Benseñor, I.J.M.; Cardoso, L.O.; Levy, R.B.; Giatti, L. Consumption of ultra-processed foods and socioeconomic position: A cross-sectional analysis of the Brazilian Longitudinal Study of Adult Health. Cad. Saúde Públ. 2018, 34, e00019717. [Google Scholar]

| Variables | RAC (n = 22) | TAC (n = 19) | DSP (n = 11) | NSP (n = 13) | ||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |
| Marital Status | ||||||||
| Single | 3 | 13.6 | 3 | 15.8 | 2 | 18.2 | 1 | 7.7 |
| Married/living with partner | 19 | 86.4 | 16 | 84.2 | 7 | 58.3 | 11 | 84.6 |
| Divorced/widowed | 0 | 0 | 0 | 0 | 2 | 18.2 | 1 | 7.7 |
| Children < 18 years | ||||||||
| Yes | 17 | 77.3 | 15 | 78.9 | 10 | 90.9 | 11 | 84.6 |
| No | 5 | 22.7 | 4 | 21.1 | 1 | 9.1 | 2 | 15.4 |
| Smoking | ||||||||
| Yes | 8 | 36.4 | 0 | 0 | 1 | 9.1 | 2 | 15.4 |
| No | 14 | 63.6 | 19 | 100 | 10 | 90.9 | 11 | 84.6 |
| Alcohol use | ||||||||
| Yes | 11 | 50 | 7 | 36.8 | 5 | 45.5 | 2 | 15.4 |
| No | 11 | 50 | 12 | 63.2 | 6 | 55 | 11 | 84.6 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tiuganji, N.M.; Nehme, P.; Marqueze, E.C.; Isherwood, C.M.; Martins, A.J.; Vasconcelos, S.; Cipolla-Neto, J.; Lowden, A.; Skene, D.J.; Moreno, C.R.C. Eating Behavior (Duration, Content, and Timing) Among Workers Living under Different Levels of Urbanization. Nutrients 2020, 12, 375. https://doi.org/10.3390/nu12020375
Tiuganji NM, Nehme P, Marqueze EC, Isherwood CM, Martins AJ, Vasconcelos S, Cipolla-Neto J, Lowden A, Skene DJ, Moreno CRC. Eating Behavior (Duration, Content, and Timing) Among Workers Living under Different Levels of Urbanization. Nutrients. 2020; 12(2):375. https://doi.org/10.3390/nu12020375
Chicago/Turabian StyleTiuganji, Natalia M., Patricia Nehme, Elaine C. Marqueze, Cheryl M. Isherwood, Andressa J. Martins, Suleima Vasconcelos, José Cipolla-Neto, Arne Lowden, Debra J. Skene, and Claudia R. C. Moreno. 2020. "Eating Behavior (Duration, Content, and Timing) Among Workers Living under Different Levels of Urbanization" Nutrients 12, no. 2: 375. https://doi.org/10.3390/nu12020375
APA StyleTiuganji, N. M., Nehme, P., Marqueze, E. C., Isherwood, C. M., Martins, A. J., Vasconcelos, S., Cipolla-Neto, J., Lowden, A., Skene, D. J., & Moreno, C. R. C. (2020). Eating Behavior (Duration, Content, and Timing) Among Workers Living under Different Levels of Urbanization. Nutrients, 12(2), 375. https://doi.org/10.3390/nu12020375







