Longitudinal Changes in Food Addiction Symptoms and Body Weight among Adults in a Behavioral Weight-Loss Program
Abstract
:1. Introduction
2. Materials and Methods
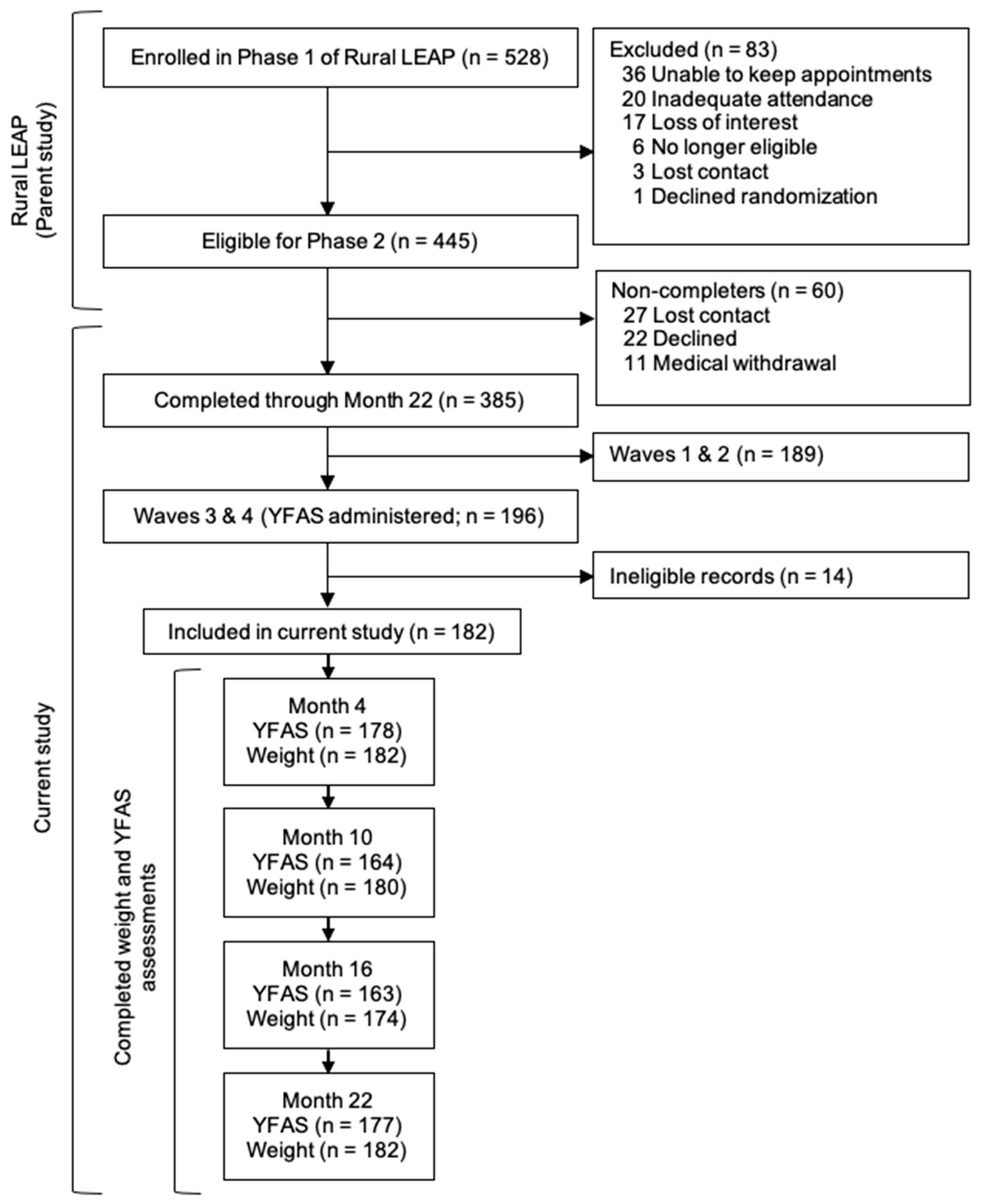
2.1. Participants
2.2. Main Variables
2.2.1. Problem foods
2.2.2. Food Addiction Symptoms
2.2.3. Body Weight
2.3. Recruitment and Initial Assessment
2.4. Intervention
2.5. Statistical Analyses
3. Results
3.1. Demographics
3.2. Phase 1 Problem Food Consumption
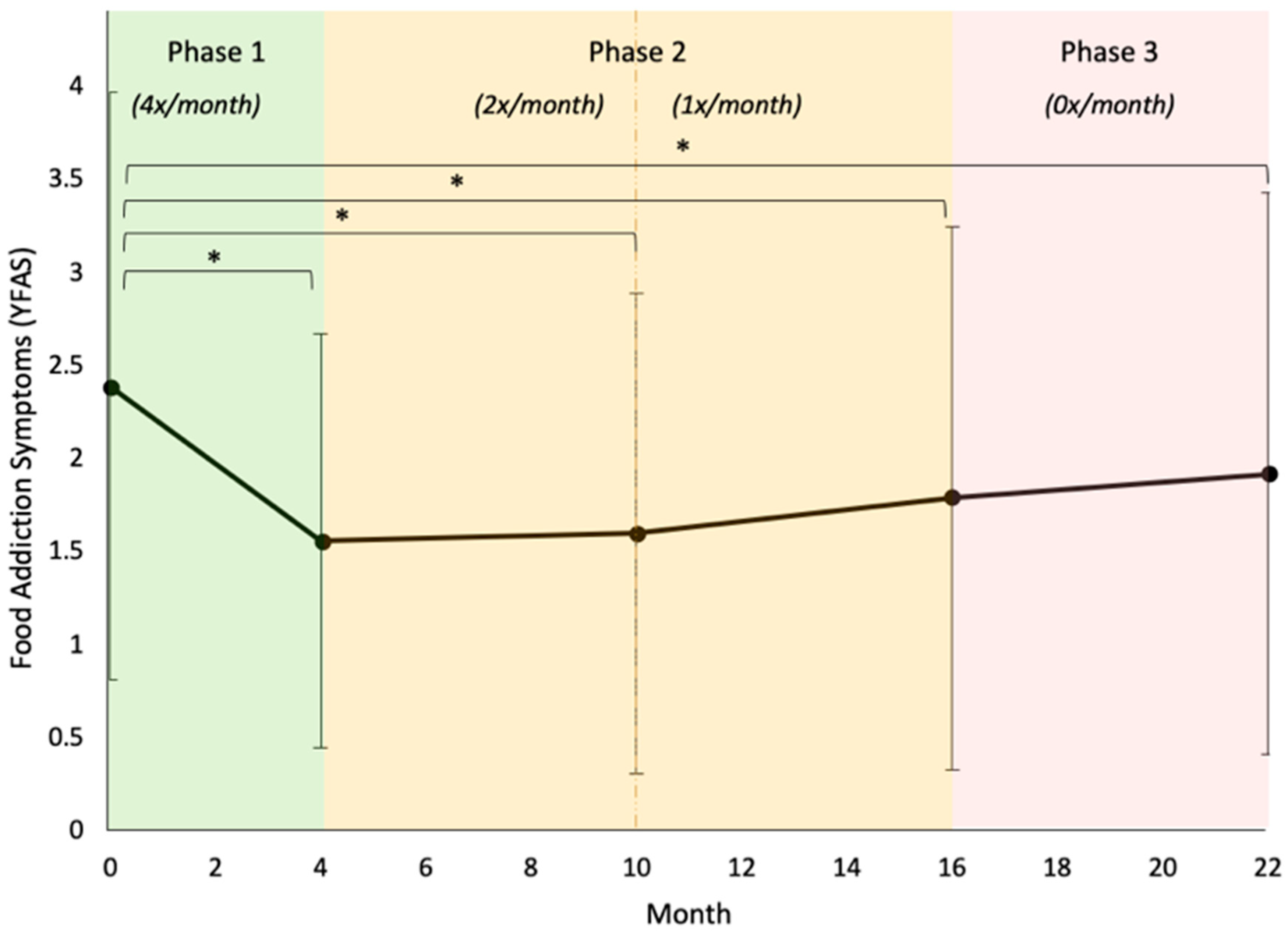
3.3. Aim 1: Long-Term Changes in Food Addiction Symptoms
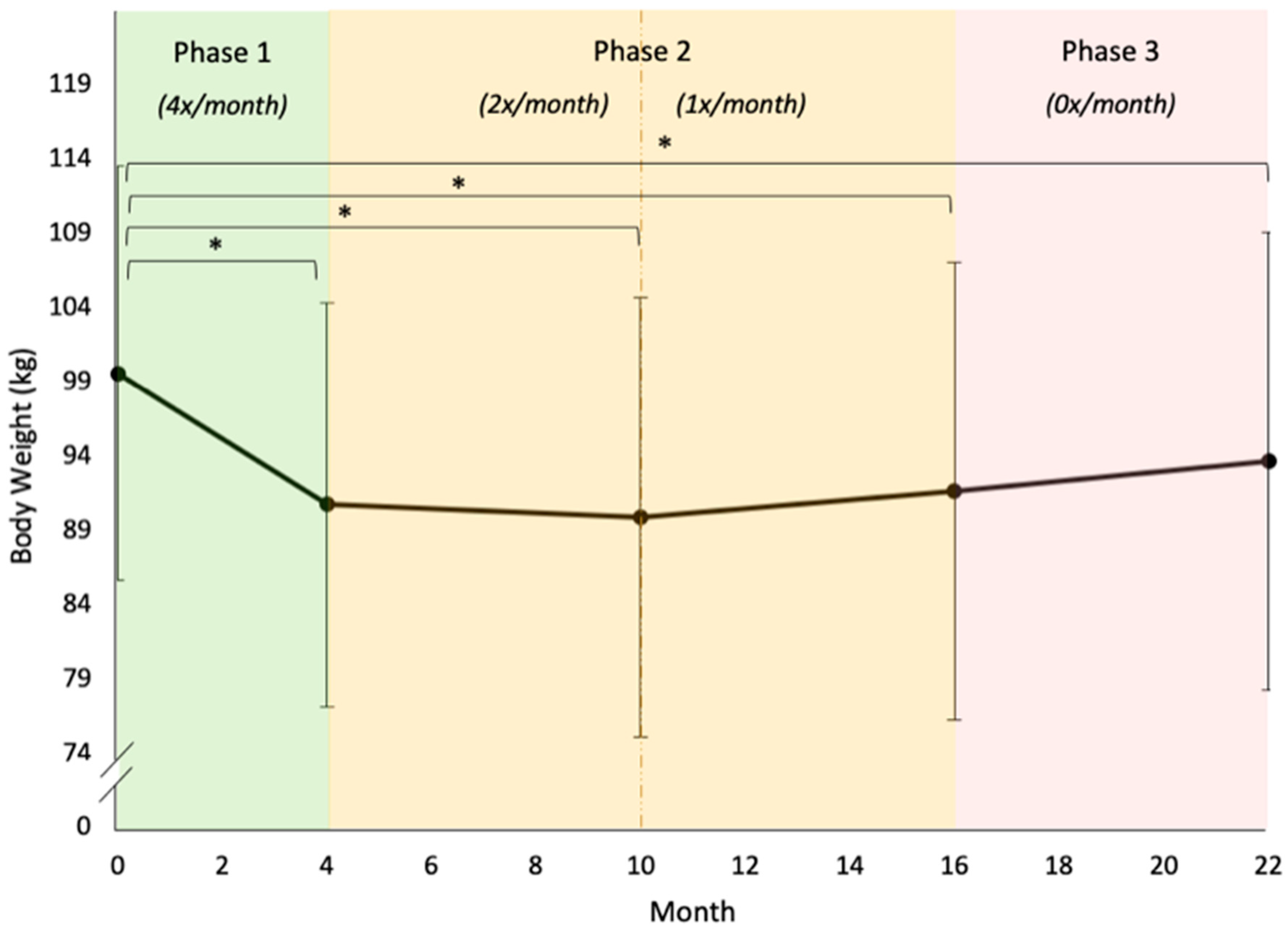
3.4. Aim 2: Long-Term Changes in Body Weight
3.5. ANOVAs and Bonferroni Post-Hocs: Food Addiction Symptoms and Body Weight
3.5.1. Food Addiction
3.5.2. Body Weight
4. Discussion
4.1. Food Addiction and Problem Foods
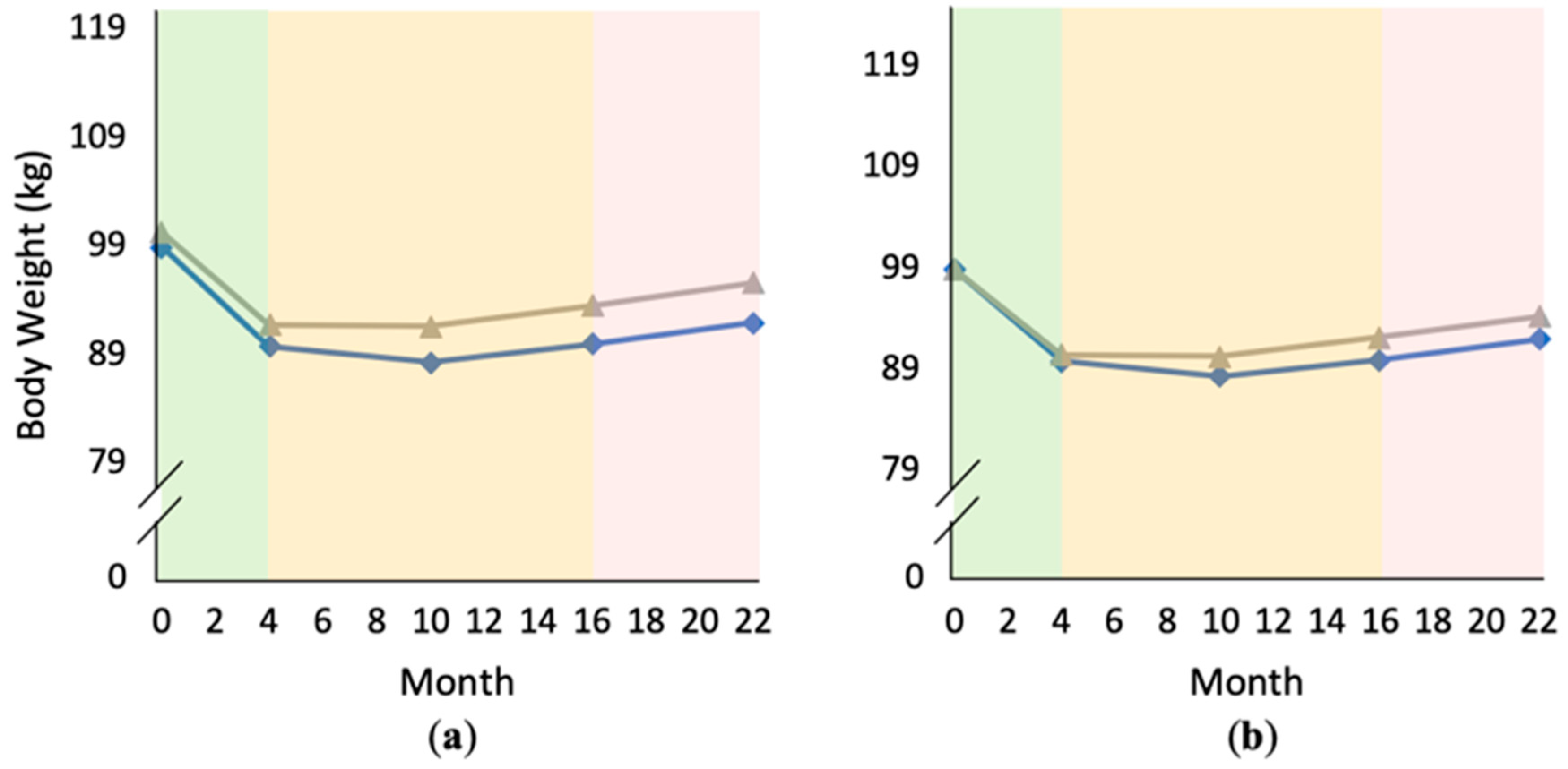
4.2. Food Addiction and Weight
4.3. Problem Foods and Weight
4.4. Implications and Future Directions
4.5. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Avena, N.M.; Rada, P.; Hoebel, B.G. Evidence for sugar addiction: Behavioral and neurochemical effects of intermittent, excessive sugar intake. Neurosci. Biobehav. Rev. 2008, 32, 20–39. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carter, A.; Hendrikse, J.; Lee, N.; Yücel, M.; Verdejo-Garcia, A.; Andrews, Z.B.; Hall, W. The neurobiology of “food addiction” and its implications for obesity treatment and policy. Annu. Rev. Nutr. 2016, 36, 105–128. [Google Scholar] [CrossRef] [PubMed]
- Gordon, E.L.; Ariel-Donges, A.H.; Bauman, V.; Merlo, L.J. What Is the Evidence for “Food Addiction?” A Systematic Review. Nutrients 2018, 10, 477. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gordon, E.L.; Lent, M.R.; Merlo, L.J. The Effect of Food Composition and Behavior on Neurobiological Response to Food: A Review of Recent Research. Curr. Nutr. Rep. 2020, 9, 75–82. [Google Scholar] [CrossRef] [PubMed]
- Ifland, J.R.; Preuss, H.G.; Marcus, M.T.; Rourke, K.M.; Taylor, W.C.; Burau, K.; Jacobs, W.S.; Kadish, W.; Manso, G. Refined food addiction: A classic substance use disorder. Med. Hypotheses 2009, 72, 518–526. [Google Scholar] [CrossRef]
- Meule, A.; Gearhardt, A.N. Food addiction in the light of DSM-5. Nutrients 2014, 6, 3653–3671. [Google Scholar] [CrossRef] [PubMed]
- Olsen, C.M. Natural rewards, neuroplasticity, and non-drug addictions. Neuropharmacology 2011, 61, 1109–1122. [Google Scholar] [CrossRef] [Green Version]
- Pursey, K.M.; Stanwell, P.; Gearhardt, A.N.; Collins, C.E.; Burrows, T.L. The prevalence of food addiction as assessed by the Yale Food Addiction Scale: A systematic review. Nutrients 2014, 6, 4552–4590. [Google Scholar] [CrossRef] [Green Version]
- Pursey, K.M.; Davis, C.; Burrows, T.L. Nutritional Aspects of Food Addiction. Curr. Addict. Rep. 2017, 4, 142–150. [Google Scholar] [CrossRef]
- Ruffle, J.K. Molecular neurobiology of addiction: What’s all the (Δ) FosB about? Am. J. Drug Alcohol Abus. 2014, 40, 428–437. [Google Scholar] [CrossRef]
- Schulte, E.M.; Avena, N.M.; Gearhardt, A.N. Which foods may be addictive? The roles of processing, fat content, and glycemic load. PLoS ONE 2015, 10, e0117959. [Google Scholar] [CrossRef] [PubMed]
- Gearhardt, A.N.; Yokum, S.; Orr, P.T.; Stice, E.; Corbin, W.R.; Brownell, K.D. Neural correlates of food addiction. Arch. Gen. Psychiatry 2011, 68, 808–816. [Google Scholar] [CrossRef] [PubMed]
- Gearhardt, A.N.; Corbin, W.R.; Brownell, K.D. Preliminary validation of the Yale food addiction scale. Appetite 2009, 52, 430–436. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schulte, E.M.; Gearhardt, A.N. Associations of Food Addiction in a Sample Recruited to Be Nationally Representative of the United States. Eur. Eat. Disord. Rev. 2017, 26, 112–119. [Google Scholar] [CrossRef] [PubMed]
- Burmeister, J.M.; Hinman, N.; Koball, A.; Hoffmann, D.A.; Carels, R.A. Food addiction in adults seeking weight loss treatment. Implications for psychosocial health and weight loss. Appetite 2013, 60, 103–110. [Google Scholar] [CrossRef]
- Gearhardt, A.N.; White, M.A.; Masheb, R.M.; Morgan, P.T.; Crosby, R.D.; Grilo, C.M. An examination of the food addiction construct in obese patients with binge eating disorder. Int. J. Eat. Disord. 2012, 45, 657–663. [Google Scholar] [CrossRef] [Green Version]
- Masheb, R.M.; Ruser, C.B.; Min, K.M.; Bullock, A.J.; Dorflinger, L.M. Does food addiction contribute to excess weight among clinic patients seeking weight reduction? Examination of the Modified Yale Food Addiction Survey. Compr. Psychiatry 2018, 84, 1–6. [Google Scholar] [CrossRef]
- Long, C.G.; Blundell, J.E.; Finlayson, G. A systematic review of the application and correlates of YFAS-diagnosed ‘food addiction’ in humans: Are eating-related ‘addictions’ a cause for concern or empty concepts? Obes. Facts 2015, 8, 386–401. [Google Scholar] [CrossRef]
- Brunault, P.; Ducluzeau, P.H.; Bourbao-Tournois, C.; Delbachian, I.; Couet, C.; Réveillère, C.; Ballon, N. Food addiction in bariatric surgery candidates: Prevalence and risk factors. Obes. Surg. 2016, 26, 1650–1653. [Google Scholar] [CrossRef]
- Cassin, S.E.; Sijercic, I.; Montemarano, V. Psychosocial Interventions for Food Addiction: A Systematic Review. Curr. Addict. Rep. 2020, 7, 9–19. [Google Scholar] [CrossRef]
- Davis, C. A commentary on the associations among ‘food addiction’, binge eating disorder, and obesity: Overlapping conditions with idiosyncratic clinical features. Appetite 2017, 115, 3–8. [Google Scholar] [CrossRef] [PubMed]
- McKenna, R.A.; Rollo, M.E.; Skinner, J.A.; Burrows, T.L. Food Addiction Support: Website Content Analysis. JMIR Cardio 2018, 2, e10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schulte, E.M.; Joyner, M.A.; Potenza, M.N.; Grilo, C.M.; Gearhardt, A.N. Current considerations regarding food addiction. Curr. Psychiatry Rep. 2015, 17, 19. [Google Scholar] [CrossRef] [PubMed]
- Vella, S.L.C.; Pai, N.B. A narrative review of potential treatment strategies for food addiction. Eat. Weight Disord.-Stud. Anorex. Bulim. Obes. 2017, 22, 387–393. [Google Scholar] [CrossRef] [PubMed]
- Foster, G.D.; Makris, A.P.; Bailer, B.A. Behavioral treatment of obesity. Am. J. Clin. Nutr. 2005, 82, 230S–235S. [Google Scholar] [CrossRef] [PubMed]
- Laudet, A.B.; Savage, R.; Mahmood, D. Pathways to long-term recovery: A preliminary investigation. J. Psychoact. Drugs 2002, 34, 305–311. [Google Scholar] [CrossRef]
- Farrow, C.; Tarrant, M.; Khan, S. Using social identity to promote health. In Addiction, Behavioral Change and Social Identity: The Path to Resilience and Recovery; Buckingham, S.A., Best, D., Eds.; Routledge: New York, NY, USA; Abington, UK, 2016. [Google Scholar]
- Sawamoto, R.; Nozaki, T.; Nishihara, T.; Furukawa, T.; Hata, T.; Komaki, G.; Sudo, N. Predictors of successful long-term weight loss maintenance: A two-year follow-up. Biopsychosoc. Med. 2017, 11, 14. [Google Scholar] [CrossRef]
- Chao, A.M.; Wadden, T.A.; Tronieri, J.S.; Pearl, R.L.; Alamuddin, N.; Bakizada, Z.M.; Pinkasavage, E.; Leonard, S.M.; Alfaris, N.; Berkowitz, R.I. Effects of addictive-like eating behaviors on weight loss with behavioral obesity treatment. J. Behav. Med. 2019, 42, 246–255. [Google Scholar] [CrossRef]
- Perri, M.G.; Shankar, M.N.; Daniels, M.J.; Durning, P.E.; Ross, K.M.; Limacher, M.C.; Janicke, D.M.; Martin, A.D.; Dhara, K.; Bobroff, L.B.; et al. Effect of Telehealth Extended Care for Maintenance of Weight Loss in Rural US Communities: A Randomized Clinical Trial. JAMA Netw. Open 2020, 3, e206764. [Google Scholar] [CrossRef]
- Perri, M.G.; Ariel-Donges, A.H.; Shankar, M.N.; Limacher, M.C.; Daniels, M.J.; Janicke, D.M.; Ross, K.M.; Bobroff, L.B.; Martin, D.; Radcliff, T.A.; et al. Design of the Rural LEAP randomized trial: An evaluation of extended-care programs for weight management delivered via group or individual telephone counseling. Contemp. Clin. Trials 2019, 76, 55–63. [Google Scholar] [CrossRef]
- Burrows, T.; Hides, L.; Brown, R.; Dayas, C.V.; Kay-Lambkin, F. Differences in dietary preferences, personality and mental health in Australian adults with and without food addiction. Nutrients 2017, 9, 285. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lemeshow, A.R.; Rimm, E.B.; Hasin, D.S.; Gearhardt, A.N.; Flint, A.J.; Field, A.E.; Genkinger, J.M. Food and beverage consumption and food addiction among women in the Nurses’ Health Studies. Appetite 2018, 121, 186–197. [Google Scholar] [CrossRef] [PubMed]
- Pursey, K.M.; Collins, C.E.; Stanwell, P.; Burrows, T.L. Foods and dietary profiles associated with ‘food addiction’ in young adults. Addict. Behav. Rep. 2015, 2, 41–48. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- USDA Agricultural Research Service. Available online: https://www.ars.usda.gov/northeast-area/beltsville-md-bhnrc/beltsville-human-nutrition-research-center/food-surveys-research-group/docs/dmr-food-categories/ (accessed on 27 July 2020).
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Preacher, K.J.; Hayes, A.F. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav. Res. MethodsInstrum. Comput. 2004, 36, 717–731. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Preacher, K.J.; Hayes, A.F. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav. Res. Methods 2008, 40, 879–891. [Google Scholar] [CrossRef]
- Petersen, R.; Pan, L.; Blanck, H.M. Racial and ethnic disparities in adult obesity in the United States: CDC’s tracking to inform state and local action. Prev. Chronic Dis. 2019, 16, 1–6. [Google Scholar] [CrossRef] [Green Version]
- Meule, A. A critical examination of the practical implications derived from the food addiction concept. Curr. Obes. Rep. 2019, 8, 11–17. [Google Scholar] [CrossRef] [Green Version]
- Schulte, E.M.; Joyner, M.A.; Schiestl, E.T.; Gearhardt, A.N. Future directions in “food addiction”: Next steps and treatment implications. Curr. Addict. Rep. 2017, 4, 165–171. [Google Scholar] [CrossRef]
- Corwin, R.L. The Face of Uncertainty Eats. Curr. Drug Abus. Rev. 2011, 4, 174–181. [Google Scholar] [CrossRef]
- Corwin, R.L.; Babbs, R.K. Rodent models of binge eating: Are they models of addiction? ILAR J. 2012, 53, 23–34. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fletcher, P.C.; Kenny, P.J. Food addiction: A valid concept? Neuropsychopharmacology 2018, 43, 2506–2513. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Webber, K.H.; Mellin, L.; Mayes, L.; Mitrovic, I.; Saulnier, M. Pilot Investigation of 2 Nondiet Approaches to Improve Weight and Health. Altern. Ther. Health Med. 2018, 24, 16–20. [Google Scholar] [PubMed]
- Sevinçer, G.M.; Konuk, N.; Bozkurt, S.; Coşkun, H. Food addiction and the outcome of bariatric surgery at 1-year: Prospective observational study. Psychiatry Res. 2016, 244, 159–164. [Google Scholar] [CrossRef] [PubMed]
- Lent, M.R.; Eichen, D.M.; Goldbacher, E.; Wadden, T.A.; Foster, G.D. Relationship of food addiction to weight loss and attrition during obesity treatment. Obesity 2014, 22, 52–55. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Murray, S.M.; Tweardy, S.; Geliebter, A.; Avena, N.M. A Longitudinal Preliminary Study of Addiction-Like Responses to Food and Alcohol Consumption Among Individuals Undergoing Weight Loss Surgery. Obes. Surg. 2019, 29, 2700–2703. [Google Scholar] [CrossRef]
- Pepino, M.Y.; Stein, R.I.; Eagon, J.C.; Klein, S. Bariatric surgery-induced weight loss causes remission of food addiction in extreme obesity. Obesity 2014, 22, 1792–1798. [Google Scholar] [CrossRef] [Green Version]
- Wing, R.R.; Hill, J.O. Successful weight loss maintenance. Annu. Rev. Nutr. 2001, 21, 323–341. [Google Scholar] [CrossRef]
- San-Cristobal, R.; Navas-Carretero, S.; Celis-Morales, C.; Brennan, L.; Walsh, M.; Lovegrove, J.A.; Daniel, H.; Saris, W.H.; Traczyk, I.; Manios, Y.; et al. Analysis of dietary pattern impact on weight status for personalised nutrition through on-line advice: The Food4Me Spanish cohort. Nutrients 2015, 7, 9523–9537. [Google Scholar] [CrossRef] [Green Version]
- Hutchesson, M.J.; Collins, C.E.; Morgan, P.J.; Watson, J.F.; Guest, M.; Callister, R. Changes to dietary intake during a 12-week commercial web-based weight loss program: A randomized controlled trial. Eur. J. Clin. Nutr. 2014, 68, 64–70. [Google Scholar] [CrossRef]
- Kong, A.; Beresford, S.A.; Alfano, C.M.; Foster-Schubert, K.E.; Neuhouser, M.L.; Johnson, D.B.; Duggan, C.; Wang, C.Y.; Xiao, L.; Jeffery, R.W.; et al. Self-monitoring and eating-related behaviors are associated with 12-month weight loss in postmenopausal overweight-to-obese women. J. Acad. Nutr. Diet. 2012, 112, 1428–1435. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vidmar, A.P.; Pretlow, R.; Borzutzky, C.; Wee, C.P.; Fox, D.S.; Fink, C.; Mittelman, S.D. An addiction model-based mobile health weight loss intervention in adolescents with obesity. Pediatric Obes. 2019, 14, e12464. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nikiforova, I.; Barnea, R.; Azulai, S.; Susmallian, S. Analysis of the Association between Eating Behaviors and Weight Loss after Laparoscopic Sleeve Gastrectomy. Obes. Facts 2019, 12, 618–631. [Google Scholar] [CrossRef] [PubMed]
- Lennerz, B.; Lennerz, J.K. Food addiction, high-glycemic-index carbohydrates, and obesity. Clin. Chem. 2018, 64, 64–71. [Google Scholar] [CrossRef] [PubMed]
- Cope, E.C.; Gould, E. New evidence linking obesity and food addiction. Biol. Psychiatry 2017, 81, 734–736. [Google Scholar] [CrossRef]
- Burrows, T.; Kay-Lambkin, F.; Pursey, K.; Skinner, J.; Dayas, C. Food addiction and associations with mental health symptoms: A systematic review with meta-analysis. J. Hum. Nutr. Diet. 2018, 31, 544–572. [Google Scholar] [CrossRef]
- Chu, D.T.; Nguyet, N.T.M.; Nga, V.T.; Lien, N.V.T.; Vo, D.D.; Lien, N.; Ngoc, V.T.N.; Le, D.H.; Nga, V.B.; Van Tu, P.; et al. An update on obesity: Mental consequences and psychological interventions. Diabetes Metab. Syndr. Clin. Res. Rev. 2019, 13, 155–160. [Google Scholar] [CrossRef]
- Jorm, A.F.; Korten, A.E.; Christensen, H.; Jacomb, P.A.; Rodgers, B.; Parslow, R.A. Association of obesity with anxiety, depression and emotional well-being: A community survey. Aust. N. Z. J. Public Health 2003, 27, 434–440. [Google Scholar] [CrossRef]
- Kamody, R.C.; Thurston, I.B.; Decker, K.M.; Kaufman, C.C.; Sonneville, K.R.; Richmond, T.K. Relating shape/weight based self-esteem, depression, and anxiety with weight and perceived physical health among young adults. Body Image 2018, 25, 168–176. [Google Scholar] [CrossRef]
- Strine, T.W.; Mokdad, A.H.; Dube, S.R.; Balluz, L.S.; Gonzalez, O.; Berry, J.T.; Manderscheid, R.; Kroenke, K. The association of depression and anxiety with obesity and unhealthy behaviors among community-dwelling US adults. Gen. Hosp. Psychiatry 2008, 30, 127–137. [Google Scholar] [CrossRef]
- Bell, C.G.; Walley, A.J.; Froguel, P. The genetics of human obesity. Nat. Rev. Genet. 2005, 6, 221–234. [Google Scholar] [CrossRef] [PubMed]
- Davis, C.; Loxton, N.J.; Levitan, R.D.; Kaplan, A.S.; Carter, J.C.; Kennedy, J.L. Food addiction’ and its association with a dopaminergic multilocus genetic profile. Physiol. Behav. 2013, 118, 63–69. [Google Scholar] [CrossRef] [PubMed]
- Osadchiy, V.; Labus, J.S.; Gupta, A.; Jacobs, J.; Ashe-McNalley, C.; Hsiao, E.Y.; Mayer, E.A. Correlation of tryptophan metabolites with connectivity of extended central reward network in healthy subjects. PLoS ONE 2018, 13, e0201772. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Santacruz, A.; Marcos, A.; Wärnberg, J.; Martí, A.; Martin-Matillas, M.; Campoy, C.; Moreno, L.A.; Veiga, O.; Redondo-Figuero, C.; Garagorri, J.M.; et al. Interplay between weight loss and gut microbiota composition in overweight adolescents. Obesity 2009, 17, 1906–1915. [Google Scholar] [CrossRef] [Green Version]
- Huseinovic, E.; Winkvist, A.; Bertz, F.; Brekke, H.K. Changes in food choice during a successful weight loss trial in overweight and obese postpartum women. Obesity 2014, 22, 2517–2523. [Google Scholar] [CrossRef]
- Assunção, M.C.F.; Gigante, D.P.; Cardoso, M.A.; Sartorelli, D.S.; Santos, I.S. Randomized, controlled trial promotes physical activity and reduces consumption of sweets and sodium among overweight and obese adults. Nutr. Res. 2010, 30, 541–549. [Google Scholar] [CrossRef]

| Characteristic | M (SD) | n (%) |
|---|---|---|
| Age (years) | 55.4 (9.9) | |
| Weight (kg) | 99.6 (13.9) | |
| BMI (kg/m2) | 36.6 (3.6) | |
| YFAS symptom score | 2.38 (1.58) | |
| YFAS clinical cutoff | ||
| ≥3 symptoms + distress/impairment | 24 (13.2) | |
| <3 symptoms or no distress/impairment | 158 (86.8) | |
| Gender | ||
| Female | 154 (84.6) | |
| Male | 28 (15.4) | |
| Ethnicity | ||
| Non-Hispanic | 175 (96.2) | |
| Hispanic | 7 (3.8) | |
| Race | ||
| White | 146 (80.2) | |
| Black or African American | 35 (19.2) | |
| Hispanic or Latino | 7 (3.8) | |
| American Indian or Alaskan Native | 6 (3.3) | |
| Asian | 1 (0.5) | |
| Native Hawaiian or Other Pacific Islander | 0 (0.0) | |
| Highest level of education | ||
| <High school | 4 (2.2) | |
| High school or GED | 89 (48.9) | |
| Associate’s degree | 21 (11.5) | |
| Bachelor’s degree | 45 (24.7) | |
| Advanced degree | 23 (12.6) | |
| Annual household income | ||
| <$20,000 | 14 (7.7) | |
| $20,000–$34,999 | 41 (22.5) | |
| $35,000–$49,999 | 31 (17.0) | |
| $50,000–$74,999 | 39 (21.4) | |
| >$75,000 | 45 (24.7) | |
| Unknown | 12 (6.6) |
| Par | Model A | Model B | Model C | Model D | Model E | |
|---|---|---|---|---|---|---|
| Fixed effects | ||||||
| Initial status | ||||||
| Intercept | γ00 | 0.007 (0.058) | −0.216 ** (0.062) | −0.217 *** (0.061) | −0.135 * (0.062) | −0.134 * (0.062) |
| PF Change | γ04 | −0.117 (0.080) | −0.026 (0.084) | −0.026 (0.085) | ||
| PF Baseline | γ03 | 0.088 (0.080) | 0.098 (0.080) | 0.088 (0.080) | ||
| BMI | γ02 | 0.262 *** (0.049) | ||||
| Baseline Age | γ01 | −0.113 * (0.056) | ||||
| Rate of change | ||||||
| Time (linear) | γ10 | −0.082 ** (0.026) | −0.083 ** (0.026) | −0.040 (0.026) | −0.039 (0.026) | |
| X PF Change | γ11 | −0.003 (0.025) | −0.005 (0.025) | |||
| Time (quad) | γ20 | 0.214 *** (0.031) | 0.215 *** (0.031) | 0.135 *** (0.034) | 0.135 *** (0.033) | |
| X PF Change | γ21 | −0.078 * (0.031) | −0.074 * (0.031) | |||
| Random effects | ||||||
| Level 1 | ||||||
| Residual | εij | 0.496 *** (0.027) | 0.385 *** (0.028) | 0.389 *** (0.028) | 0.360 *** (0.026) | 0.352 *** (0.028) |
| BMI | ζ3i | 0.041 (0.042) | ||||
| Level 2 | ||||||
| Intercept | ζ0i | 0.503 *** (0.064) | 0.468 *** (0.063) | 0.437 *** (0.059) | 0.443 *** (0.060) | 0.420 *** (0.059) |
| Time (linear) | ζ1i | 0.034 * (0.013) | 0.034 * (0.013) | 0.034 ** (0.013) | 0.033 ** (0.013) | |
| Time (quad) | ζ2i | 0.042 * (0.017) | 0.036 * (0.016) | 0.041 * (0.016) | 0.036 * (0.016) | |
| Fit Statistics | ||||||
| Deviance | 2165.464 | 2099.093 | 2087.688 | 2046.568 | 2041.203 | |
| AIC | 2171.464 | 2113.093 | 2105.688 | 2070.568 | 2069.203 | |
| BIC | 2185.749 | 2146.424 | 2148.542 | 2127.693 | 2135.849 |
| Par | Model A | Model B | Model C | Model D | Model E | |
|---|---|---|---|---|---|---|
| Fixed effects | ||||||
| Initial status | ||||||
| Intercept | γ00 | 0.003 (0.069) | −0.235 ** (0.070) | −0.228 ** (0.070) | −0.228 ** (0.070) | −0.230 *** (0.052) |
| FA (M) | γ05 | 0.083 (0.091) | 0.105 (0.092) | 0.181 ** (0.069) | ||
| FA (C) | γ06 | 0.101 *** (0.016) | 0.101 *** (0.015) | 0.101 *** (0.016) | ||
| PF Change | γ04 | −0.107 (0.101) | −0.104 (0.101) | −0.063 (0.075) | ||
| PF Baseline | γ03 | 0.005 (0.100) | 0.005 (0.100) | −0.015 (0.075) | ||
| Height | γ01 | 0.610 *** (0.052) | ||||
| White race | γ02 | −0.170 ** (0.052) | ||||
| Rate of change | ||||||
| Time (linear) | γ10 | −0.123 *** (0.015) | −0.121 *** (0.015) | −0.120 *** (0.014) | −0.120 *** (0.014) | |
| X FA (M) | γ12 | 0.051 ** (0.019) | 0.050 ** (0.019) | |||
| X PF Change | γ11 | 0.002 (0.015) | 0.002 (0.015) | |||
| Time (quad) | γ20 | 0.238 *** (0.013) | 0.224 *** (0.013) | 0.224 *** (0.013) | 0.224 *** (0.013) | |
| X FA (M) | γ22 | −0.033 (0.017) | −0.033 * (0.016) | |||
| X PF Change | γ21 | −0.005 (0.014) | −0.005 (0.013) | |||
| Random effects | ||||||
| Level 1 | ||||||
| Residual | εij | 0.147 *** (0.008) | 0.049 *** (0.004) | 0.044 *** (0.004) | 0.044 *** (0.004) | 0.046 *** (0.004) |
| FA (C) | ζ3i | 0.002 (0.004) | 0.001 (0.003) | 0.001 (0.004) | ||
| Level 2 | ||||||
| Intercept | ζ0i | 0.846 *** (0.092) | 0.874 *** (0.093) | 0.843 *** (0.090) | 0.844 *** (0.090) | 0.457 *** (0.050) |
| Time (linear) | ζ1i | 0.030 *** (0.004) | 0.028 *** (0.004) | 0.027 *** (0.004) | 0.026 *** (0.004) | |
| Time (quad) | ζ2i | 0.013 *** (0.003) | 0.013 *** (0.003) | 0.013 *** (0.003) | 0.010 ** (0.003) | |
| Fit Statistics | ||||||
| Deviance | 1443.129 | 1013.281 | 944.070 | 933.623 | 825.881 | |
| AIC | 1449.129 | 1027.281 | 968.070 | 965.623 | 861.881 | |
| BIC | 1463.536 | 1060.898 | 1025.195 | 1041.790 | 947.569 |
| Timepoint M ± SD | YFAS Score | Body Weight (kg) | Timepoint M ± SD | Change in YFAS Score | Change in Weight (kg) |
|---|---|---|---|---|---|
| Month 0 | 2.39 ± 1.58 b,c,d,e N = 182 | 99.57 ± 13.95 b,c,d,e N = 182 | Months 0–4 (Phase 1) | −0.882 ± 1.47 g,h,i N = 178 | −8.83 ± 4.75 g,h,i N = 182 |
| Month 4 | 1.56 ± 1.1 a N = 178 | 90.74 ± 13.56 a N = 182 | Months 4–10 (Phase 2, 1st half) | 0.044 ± 1.23 f N = 161 | −0.789 ± 4.51 f,h,i N = 180 |
| Month 10 | 1.60 ± 1.29 a N = 164 | 89.90 ± 14.8 a N = 180 | Months 10–16 (Phase 2, 2nd half) | 0.252 ± 1.10 f N = 153 | 1.93 ± 3.08 f,g N = 174 |
| Month 16 | 1.79 ± 1.46 a N = 163 | 91.65 ± 15.38 a N = 174 | Months 16–22 (Phase 3) | 0.073 ± 1.11 f N = 161 | 1.80 ± 3.79 f,b N = 174 |
| Month 22 | 1.92 ± 1.51 a N = 177 | 93.67 ± 15.38 a N = 182 | - | - | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gordon, E.L.; Merlo, L.J.; Durning, P.E.; Perri, M.G. Longitudinal Changes in Food Addiction Symptoms and Body Weight among Adults in a Behavioral Weight-Loss Program. Nutrients 2020, 12, 3687. https://doi.org/10.3390/nu12123687
Gordon EL, Merlo LJ, Durning PE, Perri MG. Longitudinal Changes in Food Addiction Symptoms and Body Weight among Adults in a Behavioral Weight-Loss Program. Nutrients. 2020; 12(12):3687. https://doi.org/10.3390/nu12123687
Chicago/Turabian StyleGordon, Eliza L., Lisa J. Merlo, Patricia E. Durning, and Michael G. Perri. 2020. "Longitudinal Changes in Food Addiction Symptoms and Body Weight among Adults in a Behavioral Weight-Loss Program" Nutrients 12, no. 12: 3687. https://doi.org/10.3390/nu12123687
APA StyleGordon, E. L., Merlo, L. J., Durning, P. E., & Perri, M. G. (2020). Longitudinal Changes in Food Addiction Symptoms and Body Weight among Adults in a Behavioral Weight-Loss Program. Nutrients, 12(12), 3687. https://doi.org/10.3390/nu12123687






