Relationship between Dietary Habits, Food Attitudes and Food Security Status among Adults Living within the United States Three Months Post-Mandated Quarantine: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
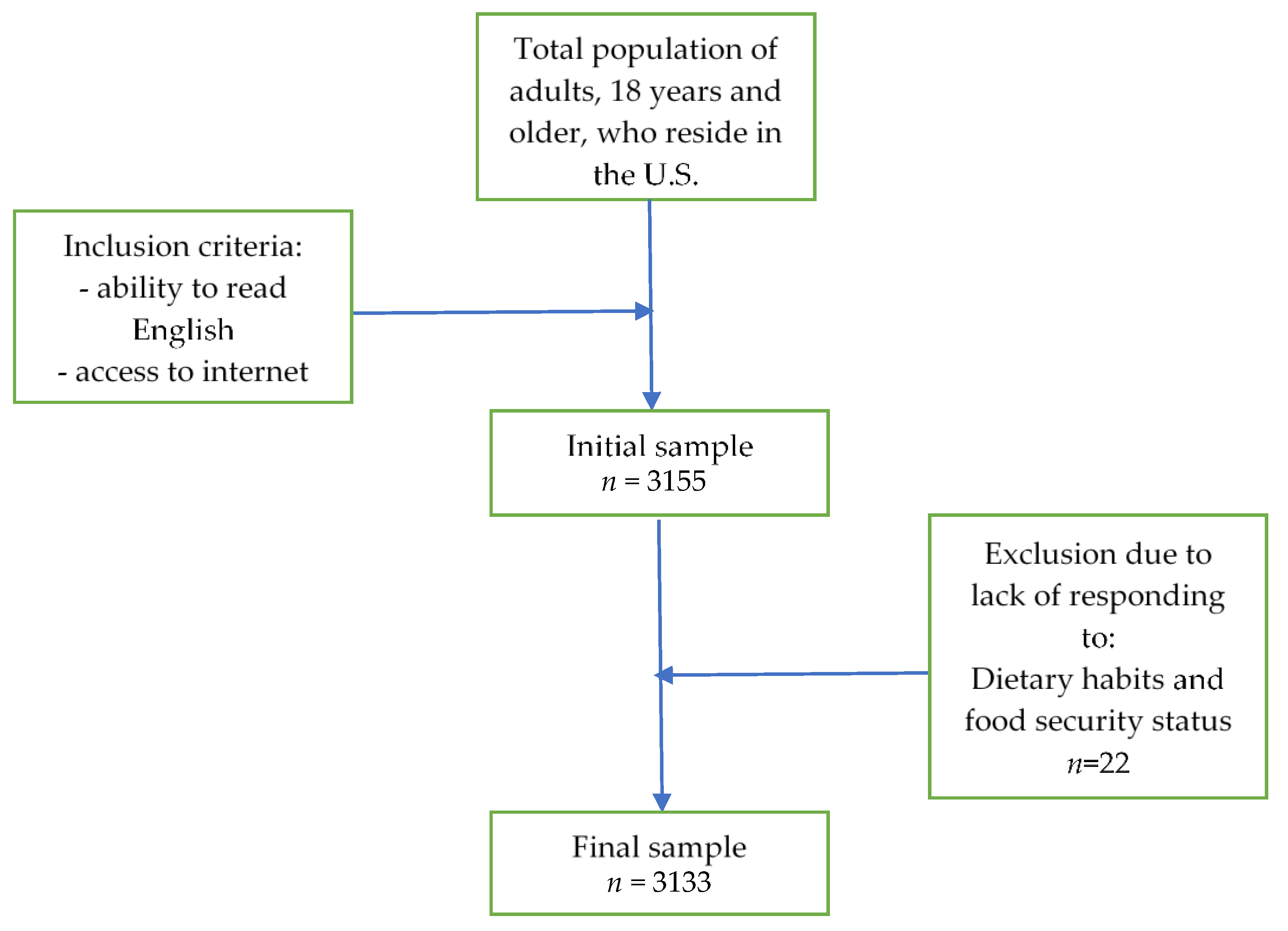
2.1. Study Design and Participants
2.2. Questionnaire
2.2.1. Lifestyle Habits
2.2.2. Dietary Habits
2.2.3. Food Attitudes
2.2.4. Food Security
2.3. Statistical Analysis
3. Results
3.1. Study Population
Health Characteristics and Anthropometrics
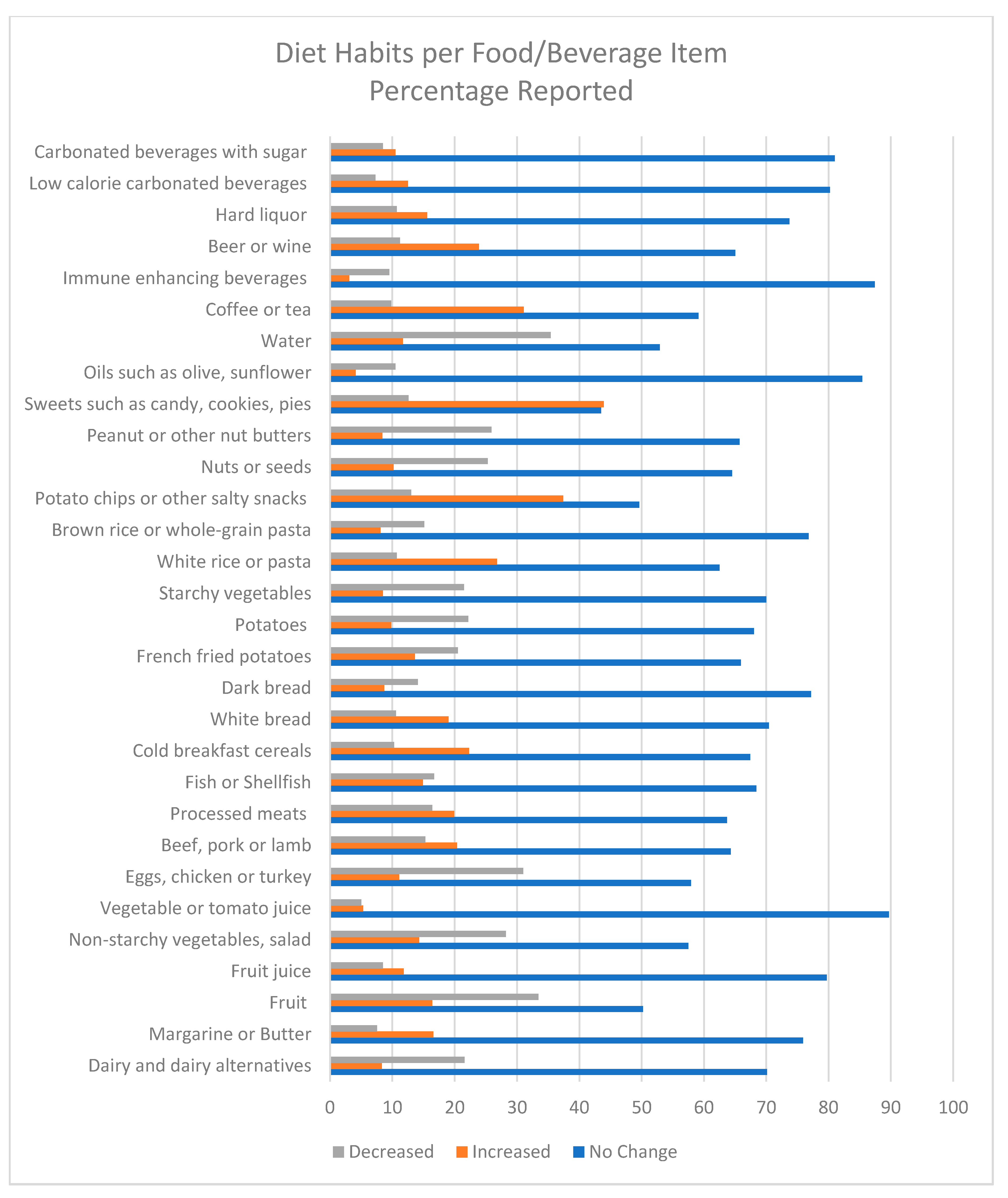
3.2. Dietary Habits
3.3. Association between Food Security Status and Food Attitudes on Dietary Habits
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at John Hopkins University (JHU). Available online: https://coronavirus.jhu.edu/map.html (accessed on 21 October 2020).
- Centers for Disease Control and Prevention. Coronavirus Disease (COVID-19) Cases in the U.S. Available online: https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html (accessed on 21 October 2020).
- Centers for Disease Control and Prevention. The President’s Coronavirus Guidelines for America. Available online: https://www.whitehouse.gov/wp-content/uploads/2020/03/03.16.20_coronavirus-guidance_8.5x11_315PM.pdf (accessed on 26 September 2020).
- U.S. Department of Labor. News Release Bureau of Labor Statistics. Available online: https://www.bls.gov/news.release/pdf/empsit.pdf (accessed on 21 October 2020).
- Raifman, J.; Bor, J.; Venkataramani, A. Unemployment insurance and food insecurity among people who lost employment in the wake of COVID-19. medRxiv 2020. [Google Scholar] [CrossRef]
- Feeding America. The Impact of the Coronavirus on Food Insecurity. 2020. Available online: https://www.feedingamerica.org/sites/default/files/2020-04/Brief_Impact%20of%20Covid%20on%20Food%20Insecurity%204.22%20%28002%29.pdf (accessed on 21 October 2020).
- Kinsey, E.W.; Kinsey, D.; Rundle, A.G. COVID-19 and Food Insecurity: An Uneven Patchwork of Responses. J. Urban Health 2020, 97, 332–335. [Google Scholar] [CrossRef]
- The Pan American Health Organization. Food Security in a Pandemic. Available online: https://www.paho.org/disasters/index.php?option=com_docman&view=download&category_slug=tools&alias=533-pandinflu-leadershipduring-tool-7&Itemid=1179&lang=en (accessed on 16 May 2020).
- Food and Agriculture Organization of the United Nations. Q&A COVID-19 Pandemic—Impact on Food and Agriculture. Available online: http://www.fao.org/2019-ncov/q-and-a/impact-on-food-and-agriculture/en/ (accessed on 16 May 2020).
- Naja, F.; Hamadeh, R. Nutrition amid the COVID-19 pandemic: A multi-level framework for action. Eur. J. Clin. Nutr. 2020, 74, 1117–1121. [Google Scholar] [CrossRef]
- Górnicka, M.; Drywień, M.E.; Zielinska, M.A.; Hamułka, J. Dietary and Lifestyle Changes During COVID-19 and the Subsequent Lockdowns among Polish Adults: A Cross-Sectional Online Survey PLifeCOVID-19 Study. Nutrients 2020, 12, 2324. [Google Scholar] [CrossRef]
- Ben-Hassen, T.; El Bilali, H.; Allahyari, M.S. Impact of COVID-19 on Food Behavior and Consumption in Qatar. Sustainability 2020, 12, 6973. [Google Scholar] [CrossRef]
- Sidor, A.; Rzymski, P. Dietary Choices and Habits during COVID-19 Lockdown: Experience from Poland. Nutrients 2020, 12, 1657. [Google Scholar] [CrossRef]
- Di Renzo, L.; Gualtieri, P.; Pivari, F.; Soldati, L.; Attinà, A.; Cinelli, G.; Leggeri, C.; Caparello, G.; Barrea, L.; Scerbo, F.; et al. Eating habits and lifestyle changes during COVID-19 lockdown: An Italian survey. J. Transl. Med. 2020, 18, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Roy, D.; Tripathy, S.; Kar, S.K.; Sharma, N.; Verma, S.K.; Kaushal, V. Study of knowledge, attitude, anxiety & perceived mental healthcare need in Indian population during COVID-19 pandemic. Asian J. Psychiatry 2020, 51, 102083. [Google Scholar] [CrossRef]
- Scarmozzino, F.; Visioli, F. Covid-19 and the Subsequent Lockdown Modified Dietary Habits of Almost Half the Population in an Italian Sample. Foods 2020, 9, 675. [Google Scholar] [CrossRef]
- Di Renzo, L.; Gualtieri, P.; Cinelli, G.; Bigioni, G.; Soldati, L.; Attinà, A.; Bianco, F.F.; Caparello, G.; Camodeca, V.; Carrano, E.; et al. Psychological Aspects and Eating Habits during COVID-19 Home Confinement: Results of EHLC-COVID-19 Italian Online Survey. Nutrients 2020, 12, 2152. [Google Scholar] [CrossRef]
- Pellegrini, M.; Ponzo, V.; Rosato, R.; Scumaci, E.; Goitre, I.; Benso, A.; Belcastro, S.; Crespi, C.; De Michieli, F.; Ghigo, E.; et al. Changes in Weight and Nutritional Habits in Adults with Obesity during the “Lockdown” Period Caused by the COVID-19 Virus Emergency. Nutrients 2020, 12, 2016. [Google Scholar] [CrossRef] [PubMed]
- Deschasaux-Tanguy, M.; Druesne-Pecollo, N.; Esseddik, Y.; De Edelenyi, F.S.; Alles, B.; Andreeva, V.A.; Baudry, J.; Charreire, H.; Deschamps, V.; Egnell, M.; et al. Diet and physical activity during the COVID-19 lockdown period (March-May 2020): Results from the French NutriNet-Sante cohort study. medRxiv 2020. [Google Scholar] [CrossRef]
- Rodríguez-Pérez, C.; Molina-Montes, E.; Verardo, V.; Artacho, R.; García-Villanova, B.; Guerra-Hernández, E.J.; Ruíz-López, M.D. Changes in Dietary Behaviours during the COVID-19 Outbreak Confinement in the Spanish COVIDiet Study. Nutrients 2020, 12, 1730. [Google Scholar] [CrossRef]
- Researchmatch.org. 2020 ReseachMatch and Vanderbilt University Medical Center. Available online: https://www.researchmatch.org/ (accessed on 9 September 2020).
- Centers for Disease Control and Prevention. Defining adult overweight and obesity. 2020. Available online: https://www.cdc.gov/obesity/adult/defining.html (accessed on 21 October 2020).
- Alomari, M.A.; Khabour, O.F.; Alzoubi, K.H. Changes in physical activity and sedentary behavior amid confinement: The bksq-covid-19 project. Risk Manag. Healthc. Policy 2020, 13, 1757–1764. [Google Scholar] [CrossRef]
- Dana-Farber Cancer Institute. Dana-Farber Cancer Institute Eating Habits Questionnaire. Available online: http://rtips.cancer.gov/rtips/viewProduct.do?viewMode=product&productId=173387 (accessed on 15 March 2020).
- Lavrakas, P. Encyclopedia of Survey Research Methods; SAGE Publications, Inc.: Thousand Oaks, CA, USA, 2008; pp. 759–762. [Google Scholar] [CrossRef]
- O’Reilly-Shah, V.N. Factors influencing healthcare provider respondent fatigue answering a globally administered in-app survey. PeerJ 2017, 5, e3785. [Google Scholar] [CrossRef]
- Hingle, M.D.; Kandiah, J.; Maggi, A. Practice Paper of the Academy of Nutrition and Dietetics: Selecting Nutrient-Dense Foods for Good Health. J. Acad. Nutr. Diet. 2016, 116, 1473–1479. [Google Scholar] [CrossRef]
- United States Department of Agriculture Health and Human Services. 2015–2020 Dietary Guidelines for Americans, 8th ed.; 2015. Available online: http://health.gov/dietaryguidelines/2015/guidelines/ (accessed on 6 January 2017).
- Gearhardt, A.N.; Corbin, W.R.; Brownell, K.D. Preliminary validation of the Yale Food Addiction Scale. Appetite 2009, 52, 430–436. [Google Scholar] [CrossRef]
- Smith, S.; Malinak, D.; Chang, J.; Perez, M.; Perez, S.; Settlecowski, E.; Rodriggs, T.; Hsu, M.; Abrew, A.; Aedo, S. Implementation of a food insecurity screening and referral program in student-run free clinics in San Diego, California. Prev. Med. Rep. 2017, 5, 134–139. [Google Scholar] [CrossRef]
- Bickel, G.; Nord, M.; Price, C.; Hamilton, W.; Cook, J. Guide to Measuring Household Food Security. 2000. Available online: https://alliancetoendhunger.org/wp-content/uploads/2018/03/USDA-guide-to-measuring-food-security.pdf (accessed on 23 June 2020).
- Pourhoseingholi, M.A.; Baghestani, A.R.; Vahedi, M. How to control confounding effects by statistical analysis. Gastroenterol. Hepatol. Bed Bench 2012, 5, 79–83. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Lawrence Earlbaum Associates: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Fabrigar, L.R.; Wegener, D.T.; MacCallum, R.C.; Strahan, E.J. Evaluating the use of exploratory factor analysis in psychological research. Psychol. Methods 1999, 4, 272–299. [Google Scholar] [CrossRef]
- Lakens, D. Calculating and reporting effect sizes to facilitate cumulative science: A practical primer for t-tests and ANOVAs. Front. Psychol. 2013, 4, 863. [Google Scholar] [CrossRef] [PubMed]
- Lauren, B.N.; Silver, E.R.; Faye, A.S.; Baidal, J.W.; Ozanne, E.M.; Hur, C. Predictors of household food insecurity in the United States during the COVID-19 pandemic. medRxiv 2020, 88. [Google Scholar] [CrossRef]
- Wolfson, J.A.; Leung, C.W. Food Insecurity and COVID-19: Disparities in Early Effects for US Adults. Nutrients 2020, 12, 1648. [Google Scholar] [CrossRef]
- Coleman-Jensen, A.; Gregory, C.A.; Rabbitt, M.P. Definitions of food insecurity. USDA Econ. Res. Serv. 2018. Available online: https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-us/definitions-of-food-security.aspx (accessed on 23 March 2019).
- United States Department of Agriculture. Will COVID-19 Threaten Availability and Affordability of Our Food? Available online: https://www.usda.gov/media/blog/2020/04/16/will-covid-19-threaten-availability-and-affordability-our-food (accessed on 26 September 2020).
- Bakalis, S.; Valdramidis, V.P.; Argyropoulos, D.; Ahrné, L.; Chen, J.; Cullen, P.; Cummins, E.; Datta, A.K.; Emmanouilidis, C.; Foster, T.; et al. Perspectives from CO+RE: How COVID-19 changed our food systems and food security paradigms. Curr. Res. Food Sci. 2020, 3, 166–172. [Google Scholar] [CrossRef]
- Czeisler, M.É.; Lane, R.I.; Petrosky, E.; Wiley, J.F.; Christensen, A.; Njai, R.; Weaver, M.D.; Robbins, R.; Facer-Childs, E.R.; Barger, L.K.; et al. Mental Health, Substance Use, and Suicidal Ideation During the COVID-19 Pandemic—United States, June 24–30, 2020. MMWR. Morb. Mortal. Wkly. Rep. 2020, 69, 1049–1057. [Google Scholar] [CrossRef]
- Msc, J.D.T.; Watson, H.J.; Thornton, L.M.; Borg, S.; Ma, R.E.F.; Ba, C.M.M.; Bs, L.E.H.; Van Furth, E.F.; Peat, C.M.; Bulik, C.M. Early impact of COVID-19 on individuals with self-reported eating disorders: A survey of ~1,000 individuals in the United States and the Netherlands. Pre-print. Int. J. Eat. Disord. 2020. [Google Scholar] [CrossRef]
- Food Insights. 2020 Food and Health Survey. Available online: https://foodinsight.org/2020-food-and-health-survey/ (accessed on 26 September 2020).
- Mehta, V. The Impact of COVID-19 on the Dietary Habits of Middle-Class Population in Mulund; AIJR Prepr: Mumbai, India, 2020; pp. 1–10. [Google Scholar]
- Laguna, L.; Fiszman, S.; Puerta, P.; Chaya, C.; Tárrega, A. The impact of COVID-19 lockdown on food priorities. Results from a preliminary study using social media and an online survey with Spanish consumers. Food Qual. Prefer. 2020, 86, 104028. [Google Scholar] [CrossRef]
- Hall, G.; Laddu, D.R.; Phillips, S.A. A tale of two pandemics: How will COVID-19 and global trends in physical inactivity and sedentary behavior affect one another? [published online ahead of print, 2020 Apr 8]. Prog. Cardiovasc. Dis. 2020. [Google Scholar] [CrossRef]
- Althubaiti, A. Information bias in health research: Definition, pitfalls, and adjustment methods. J. Multidiscip. Health 2016, 9, 211–217. [Google Scholar] [CrossRef]
| Y1 = b0 + b1X1 + b2X2 +… + bkXk | |
|---|---|
| where | |
| Y1 represents | Dietary habits |
| b0, b1 and bk represent | Estimate regression parameters |
| X1 X2 and Xk represent | k predictors (demographics, lifestyle habits, food attitudes, and food security status) |
| Variables | No. of Responses (%) |
|---|---|
| Sex | N = 3101 |
| Male | 614 (19.8%) |
| Female | 2462 (79.4%) |
| Other | 25 (0.8%) |
| Race/Ethnicity | N = 3099 |
| African American | 158 (5.1%) |
| Asian | 89 (2.9%) |
| White | 2620 (84.5%) |
| Hispanic | 87 (2.8%) |
| Native American | 11 (0.4%) |
| Other | 134 (4.3%) |
| Age | N = 3106 |
| 18–24 years | 206 (6.6%) |
| 25–29 years | 300 (9.7%) |
| 30–49 years | 946 (30.5%) |
| 50–59 years | 548 (17.6%) |
| 60–69 years | 647 (20.8%) |
| >70 years | 459 (14.8%) |
| Education level | N = 3106 |
| No schooling completed | 2 (0.1%) |
| Some high school, no diploma | 9 (0.3%) |
| High school graduate, diploma, or the equivalent (for example, GED) | 71 (2.3%) |
| Some college credit, no degree | 351 (11.3%) |
| Trade/technical/vocational training | 63 (2.0%) |
| Associate degree | 189 (6.1%) |
| Bachelor’s degree | 1062 (34.2%) |
| Master’s degree | 942 (30.3%) |
| Professional degree | 137 (4.4%) |
| Doctorate degree | 280 (9.0%) |
| Current employment status | N = 3103 |
| Full time | 1333 (43.0%) |
| Part time | 361 (11.6%) |
| Unemployed | 542 (17.5%) |
| Other | 867 (27.9%) |
| Marital status | N = 3103 |
| Married | 1567 (50.5%) |
| Single | 908 (29.3%) |
| Widowed | 125 (4.0%) |
| Divorced | 401 (12.9%) |
| Other | 102 (3.3%) |
| People live in the household besides yourself | N = 3114 |
| None | 630 (20.2%) |
| 1 | 1314 (42.2%) |
| 2 | 525 (16.9%) |
| 3 | 363 (11.7%) |
| 4 | 146 (4.7%) |
| 5 or more | 104 (3.3%) |
| Did not respond | 32 (1.0%) |
| Currently staying at home ×% of the time | N = 3105 |
| Less than 25% | 0 (0%) |
| 25–49% | 132 (4.3%) |
| 50–75% | 404 (13.0%) |
| 75–95% | 2465 (79.4%) |
| Never left the house | 104 (3.3%) |
| Residence | N = 3098 |
| New England (Connecticut, Maine, Massachusetts, Rhode Island, Vermont) | 119 (3.8%) |
| Mid-Atlantic (New Jersey, New York, Pennsylvania) | 393 (12.7%) |
| South Atlantic (Delaware, Florida, Georgia, Maryland, North Carolina, South Carolina, Virginia, Washington DC, West Virginia) | 710 (22.9%) |
| East North Central (Illinois, Indiana, Michigan, Ohio, Wisconsin) | 573 (18.5%) |
| East South Central (Alabama, Kentucky, Mississippi, Tennessee) | 268 (8.7%) |
| West North Central (Iowa, Kansas, Minnesota, Missouri, Nebraska, North Dakota, South Dakota) | 242 (7.8%) |
| West South Central (Arkansas, Louisiana, Texas) | 161 (5.2%) |
| Mountain (Arizona, Colorado, Idaho, Montana, Nevada, New Mexico, Utah, Wyoming) | 202 (6.5%) |
| Pacific (Alaska, California, Hawaii, Oregon, Washington) | 430 (13.9%) |
| Variables | No. of Responses (%) |
|---|---|
| BMI (kg/m2) | N = 3040 |
| < 18 | 37 (1.2%) |
| 18.5–24.9 | 538 (17.7%) |
| 25–29.9 | 1033 (34.0%) |
| 30–34.9 | 733 (24.1%) |
| 35–39.9 | 357 (11.7%) |
| 40–44.9 | 194 (6.4%) |
| >45 | 146 (4.8%) |
| Weight change | N = 3110 |
| No change | 1336 (43.0%) |
| Increased | 1182 (38.0%) |
| Decreased | 592 (19.0%) |
| Activity | N = 3103 |
| No change | 1102 (35.5%) |
| Increased | 1326 (42.7%) |
| Decreased | 675 (21.8%) |
| Tried a diet | N = 3123 |
| No | 2587 (82.8%) |
| Yes | 536 (17.2%) |
| Nutritional supplement intake | N = 3119 |
| No | 2474 (79.3%) |
| Yes | 645 (20.7%) |
| Supplements currently taking | N = 646 |
| Multi-vitamin | 47 (7.3%) |
| Vitamin B complex | 5 (0.8%) |
| Vitamin C | 22 (3.4%) |
| Vitamin D | 26 (4.0%) |
| Other | 47 (7.3%) |
| Two supplements | 150 (23.2%) |
| Three supplements | 111 (17.2%) |
| Four or more supplements | 238 (36.8%) |
| Medical conditions | N = 1960 |
| Cancer | 24 (1.2%) |
| Depression | 274 (13.9%) |
| Diabetes (high blood sugar) | 52 (2.7%) |
| Diverticulosis/Diverticulitis | 10 (0.5%) |
| Gastric reflux | 80 (4.1%) |
| Heart disease | 143 (7.3%) |
| IBS/D | 47 (2.4%) |
| Liver disease (cirrhosis, fatty liver) | 4 (0.2%) |
| Lung disease | 17 (0.9%) |
| Nausea/Vomiting | 9 (0.5%) |
| Other | 294 (15.0%) |
| 2 conditions | 604 (30.8%) |
| 3 or more conditions | 402 (20.5%) |
| Total Dietary Habits Score | Coef. | Std. Err. | t | p > |t| | (95% Conf. Interval) | |
|---|---|---|---|---|---|---|
| Food attitudes score | 1.07 | 0.07 | 15.22 | 0.000 * | 0.93 | 1.21 |
| Food security score | 1.06 | 0.15 | 7.22 | 0.000 * | 0.77 | 1.34 |
| Sex: female | 0.97 | 0.37 | −2.62 | 0.009 * | −1.69 | −0.24 |
| Ethnicity | −0.74 | 0.19 | −3.98 | 0.000 * | −1.10 | −0.37 |
| Residence | −0.06 | 0.06 | −0.96 | 0.34 | −0.18 | 0.06 |
| Education | 0.07 | 0.09 | 0.73 | 0.46 | −0.11 | 0.25 |
| Employment | −0.06 | 0.14 | −0.42 | 0.67 | −0.33 | 0.21 |
| Marital status | 0.26 | 0.14 | 1.91 | 0.06 | −0.01 | 0.53 |
| % of time spent at home | 1.26 | 0.28 | 4.45 | 0.000 * | 0.70 | 1.81 |
| Age range | −1.02 | 0.13 | −8.08 | 0.000 * | −1.26 | −0.77 |
| Household size | −0.07 | 0.12 | −0.57 | 0.57 | −0.31 | 0.17 |
| BMI | 0.06 | 0.02 | 2.73 | 0.006 * | 0.02 | 0.11 |
| Weight change | 0.60 | 0.25 | 2.39 | 0.017 * | 0.11 | 1.10 |
| Medical conditions | −0.01 | 0.04 | −0.35 | 0.73 | −0.09 | 0.06 |
| Tried a diet | 0.88 | 0.48 | 1.86 | 0.06 | −0.05 | 1.82 |
| Nutritional supplement intake | 2.16 | 0.43 | 5.05 | 0.000 * | 1.32 | 3.00 |
| Total activity score | 1.14 | 0.07 | 16.27 | 0.000 * | 1.00 | 1.28 |
| Food attitudes * Food security | −0.10 | 0.03 | −3.58 | 0.000 * | −0.16 | −0.05 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bin Zarah, A.; Enriquez-Marulanda, J.; Andrade, J.M. Relationship between Dietary Habits, Food Attitudes and Food Security Status among Adults Living within the United States Three Months Post-Mandated Quarantine: A Cross-Sectional Study. Nutrients 2020, 12, 3468. https://doi.org/10.3390/nu12113468
Bin Zarah A, Enriquez-Marulanda J, Andrade JM. Relationship between Dietary Habits, Food Attitudes and Food Security Status among Adults Living within the United States Three Months Post-Mandated Quarantine: A Cross-Sectional Study. Nutrients. 2020; 12(11):3468. https://doi.org/10.3390/nu12113468
Chicago/Turabian StyleBin Zarah, Aljazi, Juliana Enriquez-Marulanda, and Jeanette Mary Andrade. 2020. "Relationship between Dietary Habits, Food Attitudes and Food Security Status among Adults Living within the United States Three Months Post-Mandated Quarantine: A Cross-Sectional Study" Nutrients 12, no. 11: 3468. https://doi.org/10.3390/nu12113468
APA StyleBin Zarah, A., Enriquez-Marulanda, J., & Andrade, J. M. (2020). Relationship between Dietary Habits, Food Attitudes and Food Security Status among Adults Living within the United States Three Months Post-Mandated Quarantine: A Cross-Sectional Study. Nutrients, 12(11), 3468. https://doi.org/10.3390/nu12113468







