A Partially Hydrolyzed Whey Infant Formula Supports Appropriate Growth: A Randomized Controlled Non-Inferiority Trial
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Study Procedures and Formulas
2.3. Primary and Secondary Outcome Measures
2.4. Sample Size and Statistical Analysis
3. Results
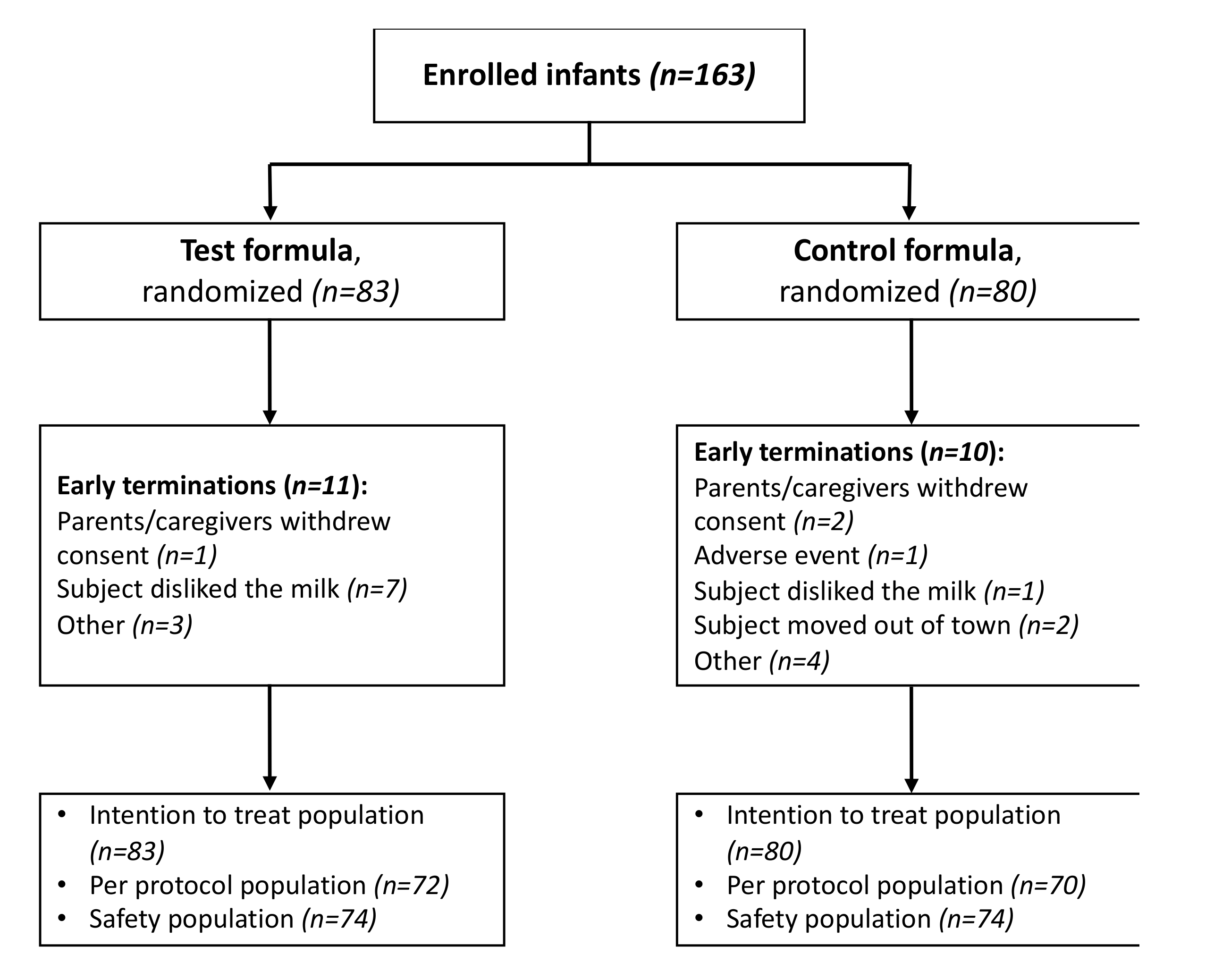
3.1. Study Population
3.2. Weight Gain and Growth
3.3. Formula Intake and Safety Parameters
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Innis, S.M. Impact of maternal diet on human milk composition and neurological development of infants. Am. J. Clin. Nutr. 2014, 99, 734S–741S. [Google Scholar] [CrossRef]
- Victora, C.G.; Bahl, R.; Barros, A.J.D.; França, G.V.A.; Horton, S.; Krasevec, J.; Murch, S.; Sankar, M.J.; Walker, N.; Rollins, N.C.; et al. Breastfeeding in the 21st century: Epidemiology, mechanisms, and lifelong effect. Lancet 2016, 387, 475–490. [Google Scholar] [CrossRef]
- Eidelman, A.I.; Schanler, R.J. Breastfeeding and the use of human milk. Pediatrics 2012, 129, e827–e841. [Google Scholar] [CrossRef]
- Chomtho, S.; Wells, J.C.K.; Williams, J.E.; Davies, P.S.W.; Lucas, A.; Fewtrell, M.S. Infant growth and later body composition: Evidence from the 4-component model. Am. J. Clin. Nutr. 2008, 87, 1776–1784. [Google Scholar] [CrossRef]
- Baird, J.; Fisher, D.; Lucas, P.; Kleijnen, J.; Roberts, H.; Law, C. Being big or growing fast: Systematic review of size and growth in infancy and later obesity. Br. Med. J. 2005, 331, 929. [Google Scholar] [CrossRef]
- Vandenplas, Y.; Bhatia, J.; Shamir, R.; Agostoni, C.; Turck, D.; Staiano, A.; Szajewska, H. Hydrolyzed formulas for allergy prevention. J. Pediatr. Gastroenterol. Nutr. 2014, 58, 549–552. [Google Scholar] [CrossRef]
- Von Berg, A.; Koletzko, S.; Grübl, A.; Filipiak-Pittroff, B.; Wichmann, H.E.; Bauer, C.P.; Reinhardt, D.; Berdel, D. The effect of hydrolyzed cow’s milk formula for allergy prevention in the first year of life: The German Infant Nutritional Intervention Study, a randomized double-blind trial. J. Allergy Clin. Immunol. 2003, 111, 533–540. [Google Scholar] [CrossRef]
- Alexander, D.D.; Cabana, M.D. Partially hydrolyzed 100% whey protein infant formula and reduced risk of atopic dermatitis: A meta-analysis. J. Pediatr. Gastroenterol. Nutr. 2010, 50, 422–430. [Google Scholar] [CrossRef]
- Høst, A.; Koletzko, B.; Dreborg, S.; Muraro, A.; Wahn, U.; Aggett, P.; Bresson, J.L.; Hernell, O.; Lafeber, H.; Michaelsen, K.F.; et al. Dietary products used in infants for treatment and prevention of food allergy. Joint statement of the european society for paediatric allergology and clinical immunology (ESPACI) committee on hypoallergenic formulas and the european society for paediatric. Arch. Dis. Child. 1999, 81, 80–84. [Google Scholar] [CrossRef]
- Koletzko, S.; Niggemann, B.; Arato, A.; Dias, J.A.; Heuschkel, R.; Husby, S.; Mearin, M.L.; Papadopoulou, A.; Ruemmele, F.M.; Staiano, A.; et al. Diagnostic approach and management of cow’s-milk protein allergy in infants and children: Espghan gi committee practical guidelines. J. Pediatr. Gastroenterol. Nutr. 2012, 55, 221–229. [Google Scholar] [CrossRef]
- Mihatsch, W.A.; Högel, J.; Pohlandt, F. Hydrolysed protein accelerates the gastrointestinal transport of formula in preterm infants. Acta Paediatr. Int. J. Paediatr. 2001, 90, 196–198. [Google Scholar] [CrossRef]
- Koopman, R.; Crombach, N.; Gijsen, A.P.; Walrand, S.; Fauquant, J.; Kies, A.K.; Lemosquet, S.; Saris, W.H.M.; Boirie, Y.; Van Loon, L.J.C. Ingestion of a protein hydrolysate is accompanied by an accelerated in vivo digestion and absorption rate when compared with its intact protein. Am. J. Clin. Nutr. 2009, 90, 106–115. [Google Scholar] [CrossRef] [PubMed]
- Corvaglia, L.; Mariani, E.; Aceti, A.; Galletti, S.; Faldella, G. Extensively hydrolyzed protein formula reduces acid gastro-esophageal reflux in symptomatic preterm infants. Early Hum. Dev. 2013, 89, 453–455. [Google Scholar] [CrossRef] [PubMed]
- Vandenplas, Y.; Cruchet, S.; Faure, C.; Lee, H.; Di Lorenzo, C.; Staiano, A.; Chundi, X.; Aw, M.; Gutierrez-Castrellon, P.; Asery, A.; et al. When should we use partially hydrolysed formulae for frequent gastrointestinal symptoms and allergy prevention? Acta Paediatr. 2014, 103, 689–695. [Google Scholar] [CrossRef] [PubMed]
- Billeaud, C.; Guillet, J.; Sandler, B. Gastric emptying in infants with or without gastro-oesophageal reflux according to the type of milk. Eur. J. Clin. Nutr. 1990, 44, 577–583. [Google Scholar] [PubMed]
- EU Commission Commission Delegated Regulation (EU) 2016/127. Off. J. Eur. Union 2016, 20–30. Available online: https://eur-lex.europa.eu/legal-content/EN/TXT/PDF/?uri=CELEX:32016R0127&from=EN (accessed on 5 October 2020).
- WHO Multicentre Growth Reference Study Group. WHO Child Growth Standards: Length/Height-for-Age, Weight-for-Age, Weight-for-Length, Weight-for-Height and Body Mass Index-for-Age: Methods and Development; World Health Organization: Geneva, Switzerland, 2006. [Google Scholar]
- American Academy of Pediatrics Task Force. Clinical Testing of Infant Formulas With Respect to Nutritional Suitability for Term Infants. Available online: http://wayback.archive-it.org/7993/20170722090324/https://www.fda.gov/Food/GuidanceRegulation/GuidanceDocumentsRegulatoryInformation/InfantFormula/ucm170649.htm (accessed on 30 June 2020).
- Puccio, G.; Alliet, P.; Cajozzo, C.; Janssens, E.; Corsello, G.; Sprenger, N.; Wernimont, S.; Egli, D.; Gosoniu, L.; Steenhout, P. Effects of infant formula with human milk oligosaccharides on growth and morbidity: A randomized multicenter trial. J. Pediatr. Gastroenterol. Nutr. 2017, 64, 624–631. [Google Scholar] [CrossRef] [PubMed]
- WHO. WHO Child Growth Standards. Dev. Med. Child Neurol. 2009, 51, 1002. [Google Scholar] [CrossRef]
- Wu, S.L.; Ding, D.; Fang, A.P.; Chen, P.Y.; Chen, S.; Jing, L.P.; Chen, Y.M.; Zhu, H.L. Growth, gastrointestinal tolerance and stool characteristics of healthy term infants fed an infant formula containing hydrolyzed whey protein (63%) and intact casein (37%): A randomized clinical trial. Nutrients 2017, 9, 1254. [Google Scholar] [CrossRef]
- Florendo, K.N.; Bellflower, B.; van Zwol, A.; Cooke, R.J. Growth in preterm infants fed either a partially hydrolyzed whey or an intact casein/whey preterm infant formula. J. Perinatol. 2009, 29, 106–111. [Google Scholar] [CrossRef]
- Rzehak, P.; Sausenthaler, S.; Koletzko, S.; Reinhardt, D.; von Berg, A.; Krämer, U.; Berdel, D.; Bollrath, C.; Grübl, A.; Cp, B.; et al. Long-term effects of feeding hydrolyzed protein infant formulas on growth extended follow-up to 10 y of age. Am. J. Clin. Nutr. 2009, 89, 1846–1856. [Google Scholar] [CrossRef] [PubMed]
- Exl, B.M.; Deland, U.; Secretin, M.C.; Preysch, U.; Wall, M.; Shmerling, D.H. Improved general health status in an unselected infant population following an allergen-reduced dietary intervention programme: The ZUFF-STUDY-PROGRAMME - Part II: Infant growth and health status to age 6 months. Eur. J. Nutr. 2000, 39, 145–156. [Google Scholar] [CrossRef] [PubMed]
- Wen, S.; Zhijian, W.; Mei, Z.; Qiao, X.; Yucong, C.; Meilian, D.; Hongwu, C.; Xiulan, W.; Meizhen, T.; Qianjun, L.; et al. Preventive Effect of Prenatal Education and Partially Hydrolyzed Whey Formula on Infantile Allergy: A Prospective Study. Chin. J. Perinatol. Med. 2015, 18, 904–909. [Google Scholar]
- Mennella, J.A.; Ventura, A.K.; Beauchamp, G.K. Differential growth patterns among healthy infants fed protein hydrolysate or cow-milk formulas. Pediatrics 2011, 127, 110–118. [Google Scholar] [CrossRef] [PubMed]
- Mennella, J.A.; Griffin, C.E.; Beauchamp, G.K. Flavor Programming during Infancy. Pediatrics 2004, 113, 840–845. [Google Scholar] [CrossRef] [PubMed]
- Foltz, M.; Ansems, P.; Schwarz, J.; Tasker, M.C.; Lourbakos, A.; Gerhardt, C.C. Protein hydrolysates induce CCK release from enteroendocrine cells and act as partial agonists of the CCK 1 receptor. J. Agric. Food Chem. 2008, 56, 837–843. [Google Scholar] [CrossRef] [PubMed]
- Diepvens, K.; Häberer, D.; Westerterp-Plantenga, M. Different proteins and biopeptides differently affect satiety and anorexigenic/orexigenic hormones in healthy humans. Int. J. Obes. 2008, 32, 510–518. [Google Scholar] [CrossRef]
| Test Formula | Control Formula | |
|---|---|---|
| Energy (kcal) | 66 | 66 |
| Intact protein (g) | 1.4 | |
| Casein | 0.57 | |
| Whey | 0.85 | |
| Whey protein hydrolysate (g) | 1.6 | |
| Fat (g) | 3.5 | 3.5 |
| DHA (mg) | 6.9 | 6.9 |
| AA (mg) | 6.9 | 6.9 |
| Carbohydrates GOS (g) | 7.0 0.2 | 7.0 0.4 |
| Ca (mg) | 50 | 56 |
| P (mg) | 30 | 31 |
| Na (mg) | 20 | 23 |
| Fe (mg) | 0.78 | 0.77 |
| Vitamin D (μg) | 1.2 | 1.1 |
| Group | ||
|---|---|---|
| Test (N = 83) | Control (N = 80) | |
| Infant characteristics | ||
| Age at baseline (days), mean (SD) | 66.9 (7.5) | 67.1 (7.5) |
| Gender (female), n (%) | 41 (49.4) | 39 (48.8) |
| Weight at baseline (g), mean (SD) | 5223 (694) 1 | 5443 (639) |
| Length at baseline (cm), mean (SD) | 59.12 (2.34) | 59.26 (2.94) |
| Head Circumference at baseline (cm), mean (SD) | 38.90 (1.31) | 38.74 (1.23) |
| Birth weight (g), mean (SD) | 3206 (398) | 3159 (392) |
| Gestational age (weeks), mean (SD) | 38.3 (1.1) | 38.3 (1.1) |
| Caesarean delivery, n (%) | 55 (66.3) | 52 (65.0) |
| Maternal characteristics | ||
| Age at baseline (years), mean (SD) | 32.9 (6.4) | 32.7 (5.8) |
| Parity (primiparous), n (%) | 41 (49.4) | 34 (42.5) |
| BMI at baseline (kg/m2), mean (SD) | 26.03 (4.74) | 27.07 (5.07) |
| Education, n (%) | ||
| ≤12 years | 28 (33.7) 1 | 29 (36.2) |
| 13–16 years | 53 (63.9) 1 | 40 (50.0) |
| >16 years | 2 (2.4) 1 | 11 (13.8) |
| Smoking during pregnancy, n (%) | 22 (26.5) | 16 (20.0) |
| Single pregnancy, n (%) | 75 (90.4) | 72 (90.0) |
| Population | Group | Weight Gain (g/d) Baseline—3rd Follow-Up | Difference between Groups (Test vs. Control) | p-Value | |
|---|---|---|---|---|---|
| LS mean (SE) | Estimate | 95% CI | |||
| PP | Test (n = 72) | 24.06 (2.635) | −0.474 | −2.460, 1.512 | 0.637 |
| Control (n = 70) | 24.54 (2.513) | ||||
| ITT | Test (n = 83) | 23.91 (2.789) | −0.641 | −2.480, 1.399 | 0.535 |
| Control (n = 80) | 24.55 (2.659) | ||||
| Daily Formula Intake by Body Weight (mL/g/d) | ||||||
|---|---|---|---|---|---|---|
| PP Population | ITT Population | |||||
| Study Visit | Test | Control | Test | Control | ||
| LS Mean (95% CI) | LS Mean (95% CI) | p-Value | LS Mean (95% CI) | LS Mean (95% CI) | p-Value | |
| Follow-up 1 | 1.00 (0.96, 1.04) | 1.02 (0.97, 1.06) | 0.651 | 1.00 (0.96, 1.05) | 1.01 (0.97, 1.05) | 0.807 |
| Follow-up 2 | 0.95 (0.90, 0.99) | 0.98 (0.94, 1.02) | 0.268 | 0.95 (0.90, 0.99) | 0.98 (0.94, 1.03) | 0.239 |
| Follow-up 3 | 0.92 (0.89, 0.96) | 0.93 (0.89, 0.97) | 0.808 | 0.92 (0.89, 0.96) | 0.93 (0.89, 0.97) | 0.808 |
| Weekly formula intake (mL) | ||||||
| PP population | ITT population | |||||
| Test | Control | Test | Control | |||
| Median | Median | p-value | Median | Median | p-value | |
| Follow-up 1 | 5757.5 | 6492.5 | <0.001 | 5797.5 | 6455.0 | 0.001 |
| Follow-up 2 | 6107.5 | 6880.0 | <0.001 | 6107.5 | 6860.0 | <.001 |
| Follow-up 3 | 6420.0 | 7040.0 | 0.002 | 6420.0 | 7040.0 | 0.002 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Karaglani, E.; Thijs-Verhoeven, I.; Gros, M.; Chairistanidou, C.; Zervas, G.; Filoilia, C.; Kampani, T.-M.; Miligkos, V.; Matiatou, M.; Valaveri, S.; et al. A Partially Hydrolyzed Whey Infant Formula Supports Appropriate Growth: A Randomized Controlled Non-Inferiority Trial. Nutrients 2020, 12, 3056. https://doi.org/10.3390/nu12103056
Karaglani E, Thijs-Verhoeven I, Gros M, Chairistanidou C, Zervas G, Filoilia C, Kampani T-M, Miligkos V, Matiatou M, Valaveri S, et al. A Partially Hydrolyzed Whey Infant Formula Supports Appropriate Growth: A Randomized Controlled Non-Inferiority Trial. Nutrients. 2020; 12(10):3056. https://doi.org/10.3390/nu12103056
Chicago/Turabian StyleKaraglani, Eva, Inge Thijs-Verhoeven, Marjan Gros, Christina Chairistanidou, Giorgos Zervas, Christina Filoilia, Tarek-Michail Kampani, Vasileios Miligkos, Maria Matiatou, Stavroula Valaveri, and et al. 2020. "A Partially Hydrolyzed Whey Infant Formula Supports Appropriate Growth: A Randomized Controlled Non-Inferiority Trial" Nutrients 12, no. 10: 3056. https://doi.org/10.3390/nu12103056
APA StyleKaraglani, E., Thijs-Verhoeven, I., Gros, M., Chairistanidou, C., Zervas, G., Filoilia, C., Kampani, T.-M., Miligkos, V., Matiatou, M., Valaveri, S., Sakellariou, A., Babilis, G., Bos, R., & Manios, Y. (2020). A Partially Hydrolyzed Whey Infant Formula Supports Appropriate Growth: A Randomized Controlled Non-Inferiority Trial. Nutrients, 12(10), 3056. https://doi.org/10.3390/nu12103056






