Families’ Perception of Classic Ketogenic Diet Management in Acute Medical Conditions: A Web-Based Survey
Abstract
1. Introduction
2. Materials and Methods
3. Results
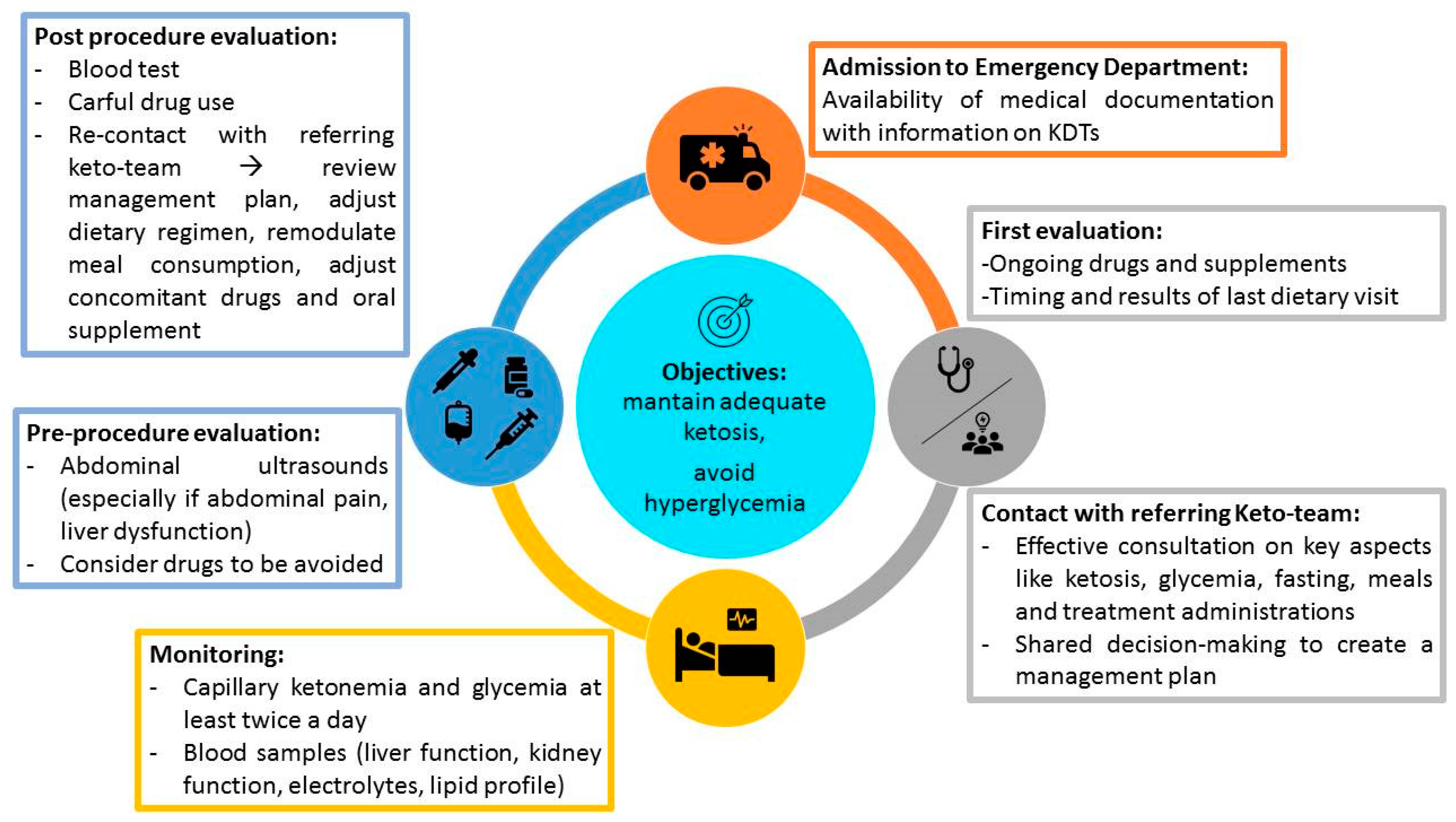
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| KDTs | Ketogenic dietary therapies |
| DRE | drug-resistant epilepsy |
| KD | Ketogenic diet |
| cKD | Classic ketogenic diet |
| DRE | Drug-resistant epilepsy |
| GLUT1DS | GLUT1 transporter deficiency syndrome |
| ER | Emergency room |
References
- Martin-McGill, K.J.; Jackson, C.F.; Bresnahan, R.; Levy, R.G.; Cooper, P.N. Ketogenic Diets for Drug-Resistant Epilepsy. Cochrane Database Syst. Rev. 2018, 11, CD001903. [Google Scholar] [CrossRef] [PubMed]
- Kwan, P.; Arzimanoglou, A.; Berg, A.T.; Brodie, M.J.; Allen Hauser, W.; Mathern, G.; Moshé, S.L.; Perucca, E.; Wiebe, S.; French, J. Definition of drug resistant epilepsy: Consensus proposal by the ad hoc Task Force of the ILAE Commission on Therapeutic Strategies. Epilepsia 2010, 51, 1069–1077. [Google Scholar] [CrossRef] [PubMed]
- Berg, A.T.; Shinnar, S.; Levy, S.R.; Testa, F.M.; Smith-Rapaport, S.; Beckerman, B. Early development of intractable epilepsy in children: A prospective study. Neurology 2001, 56, 1445–1452. [Google Scholar] [CrossRef]
- Pong, A.W.; Geary, B.R.; Engelstad, K.M.; Natarajan, A.; Yang, H.; De Vivo, D.C. Glucose transporter type I deficiency syndrome: Epilepsy phenotypes and outcomes. Epilepsia 2012, 53, 1503–1510. [Google Scholar] [CrossRef] [PubMed]
- Daci, A.; Bozalija, A.; Jashari, F.; Krasniqi, S. Individualizing Treatment Approaches for Epileptic Patients with Glucose Transporter Type1 (GLUT-1) Deficiency. Int. J. Mol. Sci. 2018, 19, 122. [Google Scholar] [CrossRef] [PubMed]
- Freeman, J.M.; Kossof, E.H.; Hartman, A.L. The ketogenic diet: One decade later. Pediatrics 2007, 119, 535–543. [Google Scholar] [CrossRef] [PubMed]
- Kossoff, E.H.; Zupec-Kania, B.A.; Auvin, S.; Ballaban-Gil, K.R.; Christina Bergqvist, A.G.; Blackford, R.; Buchhalter, J.R.; Caraballo, R.H.; Cross, J.H.; Dahlin, M.G.; et al. Optimal clinical management of children receiving dietary therapies for epilepsy: Updated recommendations of the International Ketogenic Diet Study Group. Epilepsia Open 2018, 3, 175–192. [Google Scholar] [CrossRef] [PubMed]
- Varesio, C.; Pasca, L.; Parravicini, S.; Zanaboni, M.P.; Ballante, E.; Masnada, S.; Ferraris, C.; Bertoli, S.; Tagliabue, A.; Veggiotti, P.; et al. Quality of life in chronic Ketogenic diet treatment: The GLUT1DS population perspective. Nutrients 2019, 11, 1650. [Google Scholar] [CrossRef] [PubMed]
- Schwantje, M.; Verhagen, L.M.; van Hasselt, P.M.; Fuchs, S.A. Glucose transporter type 1 deficiency syndrome and the ketogenic diet. J. Inherit. Metab. Dis. 2020, 43, 216–222. [Google Scholar] [CrossRef] [PubMed]
- Hosain, S.A.; La Vega-Talbott, M.; Solomon, G.E. Ketogenic diet in pediatric epilepsy patients with gastrostomy feeding. Pediatr. Neurol. 2005, 32, 81–83. [Google Scholar] [CrossRef] [PubMed]
- Van Gelder, M.M.h.J.; Bretveld, R.W.; Roeleveld, N. Web-based Questionnaires: The future in Epidemiology? Am. J. Epidemiol. 2010, 172, 1292–1298. [Google Scholar] [CrossRef] [PubMed]
- Ferraris, C.; Guglielmetti, M.; Tamagni, E.; Trentani, C.; De Giorgis, V.; Pasca, L.; Varesio, C.; Ferraro, O.E.; Tagliabue, A. Use of Remote Monitoring by E-mail for Long-Term Management of the Classic Ketogenic Diet. Nutrients 2020, 12, 1833. [Google Scholar] [CrossRef]
- Çağlar, A.; Edizer, S.; Sarıtaş, S.; Çelik, F.Ç.; Önder, M.; Er, A.; Ulusoy, E.; Akgül, F.; Ünalp, A.; Yılmaz, Ü.; et al. Pediatric emergency department visit characteristics of the patients on the ketogenic diet. Epilepsy Behav. 2019, 99, 106446. [Google Scholar] [CrossRef]
- Kloka, J.; Kranepuhl, S.; Zacharowki, K.; Raimann, F.J. Total intravenous anesthesia in GLUT1 Deficiency syndrome patient: A case report. Am. J. Case Rep. 2019, 20, 647–650. [Google Scholar] [CrossRef]
- Ammentorp, J.; Mainz, J.; Sabroe, S. Parents’ Priorities and Satisfaction with acute pediatric care. Arch. Pediatr. Adolesc. Med. 2005, 159, 127–131. [Google Scholar] [CrossRef]
- Jaroter, H.; DlKatz, N.R. Meta-analysis of correlates of provider behavior in medical encounters. Med. Care 1988, 26, 657–675. [Google Scholar] [CrossRef]
| 1. How old is your child? |
|
| 2. Which is the diagnosis of your child? |
|
| 3. How long has your child been on KD? |
|
| 4. Does your child have a percutaneous endoscopic gastrostomy? |
|
| 5. Does your child utilize a pre-generated ketogenic formula? |
|
| 6. Which side effects attributable to KD did your child manifest? |
|
| 7. When undergoing KD, did your child need an admission to the ER? |
|
| 8. Which was the reason why your child was taken to the ER? |
|
| 9. Did the medical staff who intervened in the ER take into consideration that your child was undergoing KD? |
|
| 10. Was ketonemia monitored during the admission to the ER? |
|
| 11. Did your child undergo surgical procedures during KD treatment? |
|
| 12. Did the medical staff who intervened in the ER/surgery ward show a basic knowledge of KD? |
|
| 13. Did the medical staff who intervened in the ER askfor a phone contact with the referring centre/general doctor to share the indications regarding KD treatment? |
|
| 14. Whenever a surgical procedure has been scheduled, were there pre-or post- surgical complications? |
|
| 15. In light of the scheduled surgical procedure and the ongoing KD treatment, were there specific precautions provided? |
|
| 16. Did you inform the referring epileptologist with regard to the acute medical situation which occurred? |
|
| 17. Do you have a list of replacement drugs (without glucose) to be carried with you or do you ask for information to the referring doctor? |
|
| 18. Do you think it could be useful to share with patients and families and medical specialists updated guidelines on KD management in the acute setting? |
|
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pasca, L.; Varesio, C.; Ferraris, C.; Guglielmetti, M.; Trentani, C.; Tagliabue, A.; Veggiotti, P.; De Giorgis, V. Families’ Perception of Classic Ketogenic Diet Management in Acute Medical Conditions: A Web-Based Survey. Nutrients 2020, 12, 2920. https://doi.org/10.3390/nu12102920
Pasca L, Varesio C, Ferraris C, Guglielmetti M, Trentani C, Tagliabue A, Veggiotti P, De Giorgis V. Families’ Perception of Classic Ketogenic Diet Management in Acute Medical Conditions: A Web-Based Survey. Nutrients. 2020; 12(10):2920. https://doi.org/10.3390/nu12102920
Chicago/Turabian StylePasca, Ludovica, Costanza Varesio, Cinzia Ferraris, Monica Guglielmetti, Claudia Trentani, Anna Tagliabue, Pierangelo Veggiotti, and Valentina De Giorgis. 2020. "Families’ Perception of Classic Ketogenic Diet Management in Acute Medical Conditions: A Web-Based Survey" Nutrients 12, no. 10: 2920. https://doi.org/10.3390/nu12102920
APA StylePasca, L., Varesio, C., Ferraris, C., Guglielmetti, M., Trentani, C., Tagliabue, A., Veggiotti, P., & De Giorgis, V. (2020). Families’ Perception of Classic Ketogenic Diet Management in Acute Medical Conditions: A Web-Based Survey. Nutrients, 12(10), 2920. https://doi.org/10.3390/nu12102920








