1. Introduction
Fragile X syndrome (FXS) is the most common form of inherited intellectual disability with a frequency of 1 in 5000 males and 1 in 4000–8000 females [
1]. The disorder is clinically characterized by highly variable cognitive disability, autism, seizures, delays in language development, anxiety disorders, aggression and attention-deficit/hyperactivity disorder (ADHD) [
1,
2]. Seizures are the most substantial medical problem in children with FXS occurring in ~8–16% of males and ~3–7% of females, typically in the first 5 years of life [
1]. Although FXS is not one of the 29 core conditions included in the newborn screening (NBS) guidelines developed by the American College of Medical Genetics, it is a high priority genetic disorder for which screening would be possible if there was an empirically-supported therapy [
3]. Findings from our laboratory indicate that soy-based diets increase seizure prevalence in a mouse model of FXS (
Fmr1KO mice) and are associated with increased febrile seizures, simple partial seizures, epilepsy comorbidity and autism phenotypes in a population of children with autism [
4,
5,
6]. Thus, we hypothesized that consumption of soy-based formula during infancy exacerbates seizures in neurodevelopmental disorders such as FXS.
There is a dearth of studies regarding the effects of soy consumption on infant development [
7,
8,
9,
10,
11,
12,
13]. Soy contains high levels of plant estrogens (phytoestrogens, isoflavones), which may mimic or antagonize natural estrogen activity. A substantial percentage (12%) of infant formulas are soy-based and have phytoestrogen levels in the range of 4.5–8 mg/kg/day [
7,
8,
9,
10,
11]. Taking into consideration body weight, infants fed soy-based formulas consume 6–11 times the amount of phytoestrogens necessary to produce hormone-like effects in adults [
14].
Current public health policies regarding soy-based infant formulas include positions from the American Academy of Pediatrics, “There is no conclusive evidence from animal, adult human, or infant populations that dietary soy isoflavones may adversely affect human development, reproduction, or endocrine function,” and the National Toxicology Program (NTP) Center for the Evaluation of Risks to Human Reproduction (CERHR), “The overall evidence was considered insufficient to reach a conclusion on whether the use of soy infant formula produces or does not produce developmental toxicity with infant exposure in girls or boys at recommended intake levels” [
15,
16]. These policies are in place for the general population, albeit there have been no studies specifically testing the effects of soy-based infant formulas in neurodevelopmental disabilities. Vulnerable populations, such as FXS, are likely more susceptible to the potential neurotoxic effects of high doses of bioactive dietary components.
It is not possible, at this time, to conduct a prospective evaluation of infant diet on FXS phenotypes as the average age of diagnosis is 35–37 months in boys and 42 months in girls [
17], which occurs long after children have transitioned from formula to solid food. If specific food products are determined to affect the prevalence or severity of seizures or other disease phenotypes in FXS, NBS could be employed to identify susceptible infants and inform decisions regarding infant feeding recommendations. We conducted a retrospective survey analysis to determine if there were associations between the consumption of soy-based infant formula and seizure history, cognitive ability and autistic behaviors in participants with FXS enrolled in the Fragile X Online Registry with Accessible Research Database (FORWARD), the largest registry of FXS participants [
18]. Previous FORWARD studies had not examined the impact of infant diet on disease outcomes. This analysis specifically examines associations between caregiver-reported use of soy-based infant formula and comorbid disorders, while comparing findings to prior data attained from the Simons Foundation Autism Research Initiative (SFARI) medical record database. We find significantly increased comorbidity of autism, GI problems and allergies in the FORWARD population associated with the use of soy-based infant formula. We emphasize that this study shows associations between soy-based infant formula and FXS comorbidities and not cause and effect relationships.
2. Materials and Methods
Ethics Approvals. Each participating clinic obtained institutional review board (IRB) approval from their institution before enrolling families in FORWARD. Those approvals provided that the clinics were allowed to contact families for participation in other research studies based on FORWARD consent form. Thus, this study did not need to be evaluated for IRB approval at the participating clinics as each clinic only provided packets to the families, who then contacted the University of Wisconsin Survey Center (UWSC) to participate. This study was reviewed by the UW Health Sciences IRB and determined to meet the criteria for exempt Human Subjects research in accordance with Category 2 defined under 45 CFR-46.
Study Design. We utilized a national registry of FXS families maintained by FORWARD to conduct the first case-control study evaluating associations between early childhood feeding practices and the severity of common FXS phenotypes (seizures, cognition and autistic behavior). The specific components of the study included the following: (1) design a questionnaire to assess demographics, infant feeding practices, frequency and severity of seizures, cognitive ability, autistic behaviors and comorbid diagnoses in a FXS population by parental survey; (2) recruit seizure (cases) and non-seizure (controls) full-mutation FXS participants to a retrospective case-control study examining associations between soy-based infant formula use and FXS phenotypes; and (3) examine associations between soy-based infant formula and clinical characteristics (i.e., frequency and severity of seizures, cognitive ability, autistic behaviors) while accounting for duration of use of soy-based infant formula and potentially confounding factors, such as food allergies. Hypotheses included the following: (1) soy-based infant formula will be associated with increased frequency and severity of seizures in FXS, (2) soy-based infant formula will be associated with decreased cognitive ability in FXS, and (3) soy-based infant formula will be associated with elevated autistic behaviors in FXS.
Questionnaire. A 55-point questionnaire was designed to assess demographics, infant feeding practices, frequency and severity of seizures, and comorbid diagnoses. Questions were adapted from the Center for Disease Control and Prevention (CDC) Infant Feeding Practices II, the Fragile X Clinical & Research Consortium (FXCRC) parent report form, and the SFARI medical records database questionnaires. In addition, cognitive ability and autistic behaviors were assessed by adapting questions from well-established tools into the questionnaire. Cognitive tools included the Ages and Stages Questionnaire (ASQ) for 36-months, and autistic tools included the Modified Checklist for Autism in Toddlers, Revised (M-CHAT-R), and the Social Responsiveness Scale (SRS) parental survey. The primary endpoint of interest examined was seizure history. The primary predictor variable was the type of infant milk (casein, soy, breast) consumed. Questions regarding variables of interest were embedded in the survey to discourage participant knowledge of the study hypothesis. Demographic information on gender, age, race/ethnicity was collected. Existing data in FORWARD could not be used in this study because their coordinating center is not allowed to provide data at an individual level to investigators due to the rarity of the disorder.
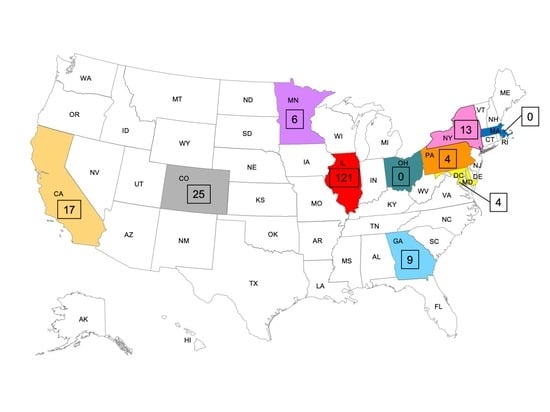
Study Population & Participant Recruitment. The FXCRC was established in 2006 with support from the National Fragile X Foundation (NFXF) and subsequently expanded in 2009 with support by a grant from the Centers for Disease Control and Prevention (CDC) and consists of 22 FXS clinics and research facilities across the United States. The FXCRC developed FORWARD in 2011 to facilitate multisite data collection on individuals with FXS and to assist researchers in identifying participants who may be interested in and meet the eligibility criteria for specific research projects [
18]. More than 1350 of the registrants are full-mutation FXS, and 1102 have a completed Clinical Report Form with seizure history. The study population included full-mutation FXS individuals enrolled in FORWARD and whose parents/caregivers had previously agreed to be contacted for research studies. Per FORWARD internal review board (IRB) guidelines, participants must be contacted directly by clinic directors for participation in research studies. Thus, for recruitment, participants in FORWARD with a history of seizures were identified as well as 4-fold more control participants. Controls were FXS participants without a reported history of seizures. Cases and controls were reasonably balanced on age and sex. The Principal Investigator, at the UW-Madison, contacted the clinical directors at all FORWARD sites and invited them to participate in the study. Individual clinics that agreed to participate in the study were provided a list of eligible participants associated with their site by the staff at FORWARD. The clinics sent parents/guardians a letter that informed them of the proposed study, invited them to participate, and emphasized the voluntary and confidential nature of the research. The letter requested that the primary caregiver of the participant with FXS return an enclosed card with their contact information to the UWSC for participation in the project.
Recruitment Sample Size Justification. During the study design phase, FORWARD had a total of 122 enrolled participants with a seizure history (cases). By recruiting all cases with a seizure history (
n = 122) and 4-fold more non-seizure controls (
n = 488) to the study, estimating a 50% response rate (
n = 61 cases;
n = 244 controls), and assuming that the non-seizure population had a 20% usage rate of soy-based infant formula similar to the SFARI population [
5], the proposed sample size would be able to detect with 80% (90%) power a 16 (19) percentage point difference in the proportion of soy-based formula use among cases versus controls, with a one-sided test of type I error of 0.05. Based on prior recruiting studies through FORWARD, a 50% response rate was deemed very conservative. Parents of FXS individuals are a highly motivated group that enthusiastically volunteer to participate in research projects to further therapeutic interventions for their children. There is a long history of collaboration and trust between these families and the clinician members of FORWARD that sent out the initial invitations for study participation. An expectation of 36% (39%) soy use among cases was reasonable as previous analysis of autism participants in the SFARI database indicated a 44% rate of soy-based infant formula use in participants reporting simple partial seizures [
5].
Data Collection. Data collection occurred in two phases because the identities of FORWARD participants were not directly available to the Principal Investigator and included a four-wave mail survey strategy to ensure maximum response rates. Phase 1 consisted of sending prepared sample collection packets to 10 FXS clinics across the United States. The packets were designed to only need a printed address label attached to each packet (postage was already provided for each packet) A copy of the packet that was used for Rush University Medical Center is provided in
Appendix A. Phase 2 consisted of (1) mailing the questionnaire (
Fragile X Syndrome Nutrition Study,
Appendix B) with a cover letter from the Principal Investigator containing a
$2 bill pre-incentive and a postage-paid return envelope; (2) mailing a thank you postcard reminder 5–7 days after the initial mailing; and (3) sending full mailings (same as the first, but without the
$2 bill and a slightly differently worded cover letter) to non-responders from the first two mailings 3–4 weeks after the initial survey packets were sent. The UWSC mailed the questionnaires and incentives, tracked responses, and provided an electronic dataset to the Principal Investigator. The informed consent document was embedded in the questionnaire to ensure return of the signed documents.
Data Analysis. Data were analyzed in accordance with STROBE guidelines. Percentages, means, standard error of the means (SEM), odds ratios (OR), and 95% confidence intervals (CI) were computed to describe the population. Fisher exact test (if less than 5 outcomes per cell) or Pearson’s uncorrected chi-square tests were used to examine the null hypotheses that the prevalence of comorbidities in FXS are the same in infants fed soy-based infant formula or not. Student’s t-tests were used to compare the means of two populations. Statistical significance was defined as p < 0.05. A Bonferroni correction was not applied for multiple comparisons. The number of participants for each comparison is reported in the corresponding tables. This manuscript addresses the hypothesis that soy-based infant formula is associated with increased frequency and severity of seizures in FXS. Subsequent manuscripts will address the other study hypotheses regarding cognitive ability and specific autistic behaviors as well the association of comorbidities with breast milk.
4. Discussion
There is little knowledge regarding how early life feeding is associated with neurological development, particularly in neurodevelopmental disorders. To fill this gap, we conducted the first study examining associations between infant feeding practices, specifically soy-based infant formula, and disease outcomes in children with FXS using FORWARD as a sampling frame to collect new data through parental surveys. This unique study population, with a high prevalence of seizures compared to the general population, allowed for a smaller cohort size. Published estimates of formula intolerance range from 2–7.5%; yet, 12% of infants are fed soy-based formula suggesting that nonstandard, soy-based formulas are used excessively [
16]. Infants with FXS are often hypotonic and have initial poor latch and suck with breastfeeding, as well as frequent recurrent emesis because of reflux [
1]. We found that 25% of FORWARD participants in this survey study reported use of soy-based infant formula. We also found associations between the consumption of soy-based infant formula and increased comorbidity of autism, GI problems and allergies. The data did not reach statistical significance to corroborate prior retrospective analysis of medical record data from the SFARI population where the prevalence of seizures in autistic children fed soy-based infant formula was higher [
5]. However, line item analysis of the Aberrant Behavior Checklist (ABC) in the SFARI population indicated that several autistic behaviors were exacerbated in autistic children reported to have consumed soy-based infant formula [
6], and analysis of comorbid conditions in the SFARI population indicated associations between soy-based formula and increased allergies, ADHD and bipolar disorder [
25]. Overall, these findings from FORWARD FXS and SFARI autism populations strongly suggest that early-life feeding with soy-based infant formula is associated with adverse neurological outcomes in these developmental disabilities. It remains to be determined if babies destined to have more severe disability (autism, seizures, etc.) are harder to breastfeed (will not latch on, hyper, colic) and have more feeding intolerance and potentially more severe problems with gastroesophageal reflux (GERD) and bowel dysregulation, leading to the increased use of formula including soy formula.
An important goal of this project was to account for potentially confounding issues instigating the use of soy-based infant formula. The Infant Feeding and Early Development (IFED) Study found that the top-rated maternal reasons for use of soy-based formula include: “I fed my other child(ren) soy formula” (54%), “I think soy is healthier than other types of formula” (54%), “I suspect my baby had milk intolerance or my family has trouble digesting cow’s milk” (52%), “My family and friends recommended it” (27%), “I chose soy formula for religious reasons” (17%), “Health care provider recommended soy” (15%), “I prefer a dairy-free diet” (12%), “My child had colic or other digestive problem” (7%), “I suspected my baby had a food allergy or intolerance (other than milk)” (7%), and “Family follows a vegan diet” (1%) [
12]. In the IFED population, 70% of mothers were Black, and 57% had a high school education or less. In contrast, in FORWARD, the highest ranked reasons for the use of soy-based infant formula were medical-related, particularly GI issues. In the soy cohort, 61% of infants exhibited GI problems within 2 weeks of age, and the initiation of soy-based formula started at the same time or after the GI problems. These data suggest that a high rate of GI problems in newborns with FXS necessitates alternate feeding strategies including the use of soy-based infant formula. Thus, early GI problems are a potentially confounding issue here. It is possible that the GI issues and resulting effects on nutritional intake produced the increased prevalence of autism, and that soy is simply a marker (correlate) of the underlying cause of the GI problems.
The strengths of this study design include: (1) this study is the first to link parent-reported data on infant feeding practices of children with FXS to disease phenotypes in those children; (2) FORWARD offers a unique study population with a high prevalence of seizures compared to the general population allowing for smaller cohort sizes; (3) the caregivers are a highly motivated group of parents eager to participate in research studies; and (4) FORWARD is an established FXS registry.
The limitations of this study include the following: (1) A limitation of all retrospective studies is the inability to fully evaluate the temporality of the relationships examined. Although a longitudinal approach would better enable evaluation of causality, it is currently impossible in this population because most participants are not diagnosed with FXS until three years of age after infant formula has been discontinued. (2) Another limitation is recall bias. Parents were asked to answer a series of questions regarding infant feeding and the frequency and severity of seizures, which may have occurred years earlier. The selection of questions was chosen with great care as to yield more accurate measures, and recall bias regarding infant formula usage was not expected to be a problem as parents typically switch formulas for specific reasons such as GI problems or allergies. (3) Another limitation is parental report of seizure type, which was not accurate as families are not trained in classifying seizures and doctors may not have told the parents which type(s) of seizures their child had. These data are best attained by review of the medical records. (4) Another limitation is response rates leading to concerns that that the case sample is not representative of the population of children with FXS experiencing seizures. We observed a low response rate (19%) at the phase 1 level and a high response rate (89%) at the phase 2 level. The majority (61%) of the completed questionnaires were from a single clinic (Rush University Medical Center). We could not address the Phase 1 response rate issue due to FORWARD IRB regulations that precluded our inability to contact participants until after they returned contact information to the UWSC. Moving forward, we plan to increase participant response by conducting the survey online through the NFXF whereby consent is attained through voluntary participation in an online survey. (5) Another limitation is potential selection bias. Many participants switch from breast milk to cow milk formula to soy-based formula, and the need for multiple dietary changes may be due to a more severe FXS phenotype.
In a clinical setting, parents seek medical attention for their infants with FXS at the onset of developmental delays. Population-wide NBS is not performed in the U.S. because there is no treatment. Hence, most children are three years or older before diagnosis. Considering the dearth of treatments for FXS and the high comorbidity of early-life GI problems, our findings warrant further investigation. There are alternatives to soy-based infant formula that could be implemented in the clinic for infants with FXS experiencing problems with breastfeeding and cow milk-based formulas. However, NBS for FXS would be required to enable an early diagnosis and choice of infant feeding.