School-Based Interventions Targeting Nutrition and Physical Activity, and Body Weight Status of African Children: A Systematic Review
Abstract
1. Introduction
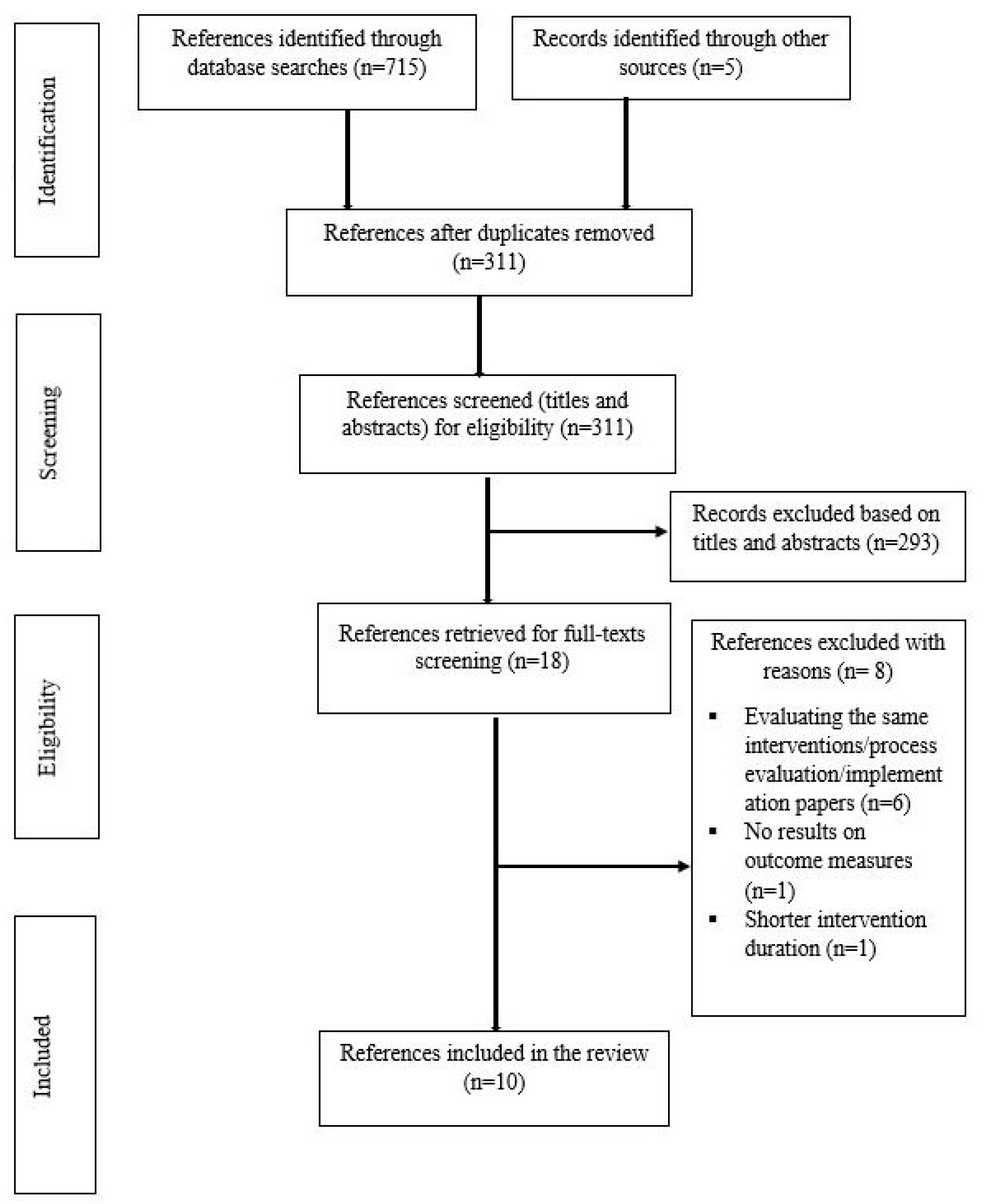
2. Materials and Methods
2.1. Inclusion Criteria, Data Sources and Selection of Relevant Studies
2.2. Data Extraction
2.3. Quality Assessment
2.4. Data Synthesis
2.5. Ethics Consideration
3. Results
3.1. Description of the Included Studies
3.1.1. Study Setting, Design, and Population
3.1.2. Intervention Characteristics
3.1.3. Intervention Outcomes and Measures
3.1.4. Theoretical Basis of Intervention
3.2. Methodological Quality of the Included Studies
3.3. Main Findings of Interventions
3.3.1. Weight Status
3.3.2. Physical Fitness, and PA Knowledge, Attitudes, Intentions and Behaviours
3.3.3. Nutrition Knowledge, Attitudes, Self-Efficacy and Behaviours
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Ng, M.; Fleming, T.; Robinson, M.; Thomson, B.; Graetz, N.; Margono, C.; Mullany, E.C.; Biryukov, S.; Abbafati, C.; Abera, S.F.; et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014, 384, 766–781. [Google Scholar] [CrossRef]
- UNICEF; World Health Organization; World Bank Group. Levels and Trends in Child Malnutrition; eSocialSciences: London, UK, 2016; pp. 1–8. [Google Scholar]
- Adom, T.; Kengne, A.P.; De Villiers, A.; Puoane, T. Prevalence of overweight and obesity among African primary school learners: A systematic review and meta-analysis. Obes. Sci. Pract. 2019, 5, 487–502. [Google Scholar] [CrossRef]
- Reilly, J.J. Health consequences of obesity. Arch. Dis. Child. 2003, 88, 748–752. [Google Scholar] [CrossRef]
- Noubiap, J.J.; Essouma, M.; Bigna, J.J.; Jingi, A.M.; Aminde, L.N.; Nansseu, J.R. Prevalence of elevated blood pressure in children and adolescents in Africa: A systematic review and meta-analysis. Lancet Public Health 2017, 2, e375–e386. [Google Scholar] [CrossRef]
- Agyemang, C.; Redekop, W.K.; Owusu-Dabo, E.; Bruijnzeels, M.A. Blood pressure patterns in rural, semi-urban and urban children in the Ashanti region of Ghana, West Africa. BMC Public Health 2005, 5, 114. [Google Scholar] [CrossRef][Green Version]
- Salman, Z.; Kirk, G.D.; DeBoer, M.D. High Rate of Obesity-Associated Hypertension among Primary Schoolchildren in Sudan. Int. J. Hypertens. 2011, 2011, 629492. [Google Scholar] [CrossRef]
- Harrabi, I.; Bouaouina, M.; Maatoug, J.; Gaha, R.; Ghannem, H. Prevalence of the metabolic syndrome among urban schoolchildren in Sousse, Tunisia. Int. J. Cardiol. 2009, 135, 130–131. [Google Scholar] [CrossRef]
- Jmal, L.; Jmal, A.; Abdennebi, M.; Feki, M.; Boukthir, S. Prevalence of Metabolic Syndrome in Tunisian Overweight and Obese Children. Tunis. Med. 2019, 97, 133–139. [Google Scholar]
- Jamoussi, H.; Mahjoub, F.; Sallemi, H.; Berriche, O.; Ounaissa, K.; Amrouche, C.; Blouza, S. Metabolic Syndrome in Tunisian Obese Children and Adolescents. Tunis. Med. 2012, 90, 36–40. [Google Scholar]
- Zeelie, A.; Moss, S.J.; Kruger, H.S. The relationship between body composition and selected metabolic syndrome markers in black adolescents in South Africa: The PLAY study. Nutrition 2010, 26, 1059–1064. [Google Scholar] [CrossRef]
- Munthali, R.J.; Kagura, J.; Lombard, Z.; Norris, S.A. Childhood adiposity trajectories are associated with late adolescent blood pressure: Birth to twenty cohort. BMC Public Health 2016, 16, 665. [Google Scholar] [CrossRef]
- Reilly, J.J.; Kelly, J. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: Systematic review. Int. J. Obes. 2011, 35, 891–898. [Google Scholar] [CrossRef]
- Brown, T.; Summerbell, C. Systematic review of school-based interventions that focus on changing dietary intake and physical activity levels to prevent childhood obesity: An update to the obesity guidance produced by the National Institute for Health and Clinical Excellence. Obes. Rev. 2009, 10, 110–141. [Google Scholar] [CrossRef]
- Bleich, S.N.; Vercammen, K.A.; Zatz, L.Y.; Frelier, J.M.; Ebbeling, C.B.; Peeters, A. Interventions to prevent global childhood overweight and obesity: A systematic review. Lancet Diabetes Endocrinol. 2018, 6, 332–346. [Google Scholar] [CrossRef]
- Verstraeten, R.; Roberfroid, D.; Lachat, C.; Leroy, J.L.; Holdsworth, M.; Maes, L.; Kolsteren, P.W. Effectiveness of preventive school-based obesity interventions in low- and middle-income countries: A systematic review. Am. J. Clin. Nutr. 2012, 96, 415–438. [Google Scholar] [CrossRef]
- Waters, E.; de Silva-Sanigorski, A.; Burford, B.J.; Brown, T.; Campbell, K.J.; Gao, Y.; Armstrong, R.; Prosser, L.; Summerbell, C.D. Interventions for preventing obesity in children. Cochrane Database Syst. Rev. 2011. [Google Scholar] [CrossRef]
- Dobbins, M.; Husson, H.; Decorby, K.; Rl, L. School-based physical activity programs for promoting physical activity and fitness in children and adolescents aged 6 to 18. Cochrane Database Syst. Rev. 2013. [Google Scholar] [CrossRef]
- Kamath, C.C.; Vickers, K.S.; Ehrlich, A.; Mcgovern, L.; Johnson, J.; Singhal, V.; Paulo, R.; Hettinger, A.; Erwin, P.J.; Montori, V.M. Behavioral Interventions to Prevent Childhood Obesity: A Systematic Review and Metaanalyses of Randomized Trials. Clin. Rev. 2008, 93, 4606–4615. [Google Scholar] [CrossRef]
- Adom, T.; Puoane, T.; De Villiers, A.; Kengne, A.P. Protocol for systematic review of school-based interventions to prevent and control obesity in African learners. BMJ Open 2017, 7, e013540. [Google Scholar] [CrossRef]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef]
- Siegfried, N.; Clarke, M.; Volmink, J. Randomised controlled trials in Africa of HIV and AIDS: Descriptive study and spatial distribution. BMJ 2005, 331, 742. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Effective Public Health Practice Project. Quality Assessment Tool for Quantitative Studies; Effective Public Health Practice Project: Hamilton, ON, Canada, 1998. [Google Scholar]
- Uys, M.; Draper, C.E.; Hendricks, S.; De Villiers, A.; Fourie, J.; Steyn, N.P.; Lambert, E.V. Impact of a South African school-based intervention, HealthKick, on fitness correlates. Am. J. Health Behav. 2016, 40, 55–66. [Google Scholar] [CrossRef] [PubMed]
- De Villiers, A.; Steyn, N.P.; Draper, C.E.; Hill, J.; Gwebushe, N.; Lambert, E.V.; Lombard, C. Primary school children’s nutrition knowledge, self-efficacy, and behavior, after a three-year healthy lifestyle intervention (HealthKick). Ethn. Dis. 2016, 26, 171–180. [Google Scholar] [CrossRef]
- Naidoo, R.; Coopoo, Y.; Lambert, E.; Draper, C. Impact of a primary school-based nutrition and physical activity intervention on learners in KwaZulu-Natal, South Africa: A pilot study. S. Afr. J. Sport Med. 2009, 21, 7–12. [Google Scholar] [CrossRef]
- Draper, C.E.; De Kock, L.; Grimsrud, A.T.; Rudolph, M.; Nemutandani, S.; Kolbe-Alexander, T. Evaluation of a school-based physical activity intervention in Alexandra Township. S. Afr. J. Sport Med. 2010, 22, 12–19. [Google Scholar] [CrossRef]
- Jemmott, J.B., III; Jemmott, L.S.; O’Leary, A.; Ngwane, Z.; Icard, L.; Bellamy, S.; Jones, S.; Landis, R.J.; Heeren, G.A.; Tyler, J.C.; et al. Cognitive-behavioural health-promotion intervention increases fruit and vegetable consumption and physical activity among South African adolescents: A cluster-randomised controlled trial. Psychol. Health 2011, 26, 167–185. [Google Scholar] [CrossRef]
- Monyeki, M.A.; De Ridder, J.H.; Du Preez, S.M.; Toriola, A.; Malan, D.D.J. The effect of a ten month physical activity intervention programme on body composition of 9–13 year-old boys. Afr. J. Phys. Health Educ. Recreat. Danc. 2012, 18, 241–250. [Google Scholar]
- Harrabi, I.; Maatoug, J.; Gaha, M.; Kebaili, R.; Gaha, R.; Ghannem, H. School-based Intervention to Promote Healthy Lifestyles in Sousse, Tunisia. Indian J. Community Med. 2010, 35, 94–99. [Google Scholar] [CrossRef]
- Maatoug, J.; Fredj, S.B.; Msakni, Z.; Dendana, E.; Sahli, J.; Harrabi, I.; Chouikha, F.; Boughamoura, L.; Slama, S.; Farpour-Lambert, N.; et al. Challenges and results of a school-based intervention to manage excess weight among school children in Tunisia 2012–2014. Int. J. Adolesc. Med. Health 2015, 29. [Google Scholar] [CrossRef]
- Ghammam, R.; Maatoug, J.; Zammit, N.; Kebaili, R.; Boughammoura, L.; Al’Absi, M.; Lando, H.; Ghannem, H. Long term effect of a school based intervention to prevent chronic diseases in Tunisia, 2009–2015. Afr. Health Sci. 2017, 17, 1137–1148. [Google Scholar] [CrossRef]
- Regaieg, S.; Charfi, N.; Kamoun, M.; Ghroubi, S.; Rebai, H.; Elleuch, H.; Feki, M.M.; Abid, M. The effects of an exercise training program on body composition and aerobic capacity parameters in Tunisian obese children. Indian J. Endocrinol. Metab. 2013, 17, 1040–1045. [Google Scholar]
- Brown, E.C.; Buchan, D.S.; Baker, J.S.; Wyatt, F.B.; Bocalini, D.S.; Kilgore, L. A Systematised Review of Primary School Whole Class Child Obesity Interventions: Effectiveness, Characteristics, and Strategies. Biomed Res. Int. 2016. [Google Scholar] [CrossRef] [PubMed]
- Sharma, M. School-based interventions for childhood and adolescent obesity. Obes. Rev. 2006, 7, 261–269. [Google Scholar] [CrossRef]
- Bauer, K.W.; Neumark-Sztainer, D.; Fulkerson, J.A.; Hannan, P.J.; Story, M. Familial correlates of adolescent girls’ physical activity, television use, dietary intake, weight, and body composition. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 25. [Google Scholar] [CrossRef]
- McMinn, A.M.; Griffin, S.J.; Jones, A.P.; Van Sluijs, E.M.F. Family and home influences on children’s after-school and weekend physical activity. Eur. J. Public Health 2013, 23, 805–810. [Google Scholar] [CrossRef]
- Zecevic, C.A.; Tremblay, L.; Lovsin, T.; Michel, L. Parental Influence on Young Children’s Physical Activity. Int. J. Pediatr. 2010, 2010, 1–9. [Google Scholar] [CrossRef]
- Lippevelde, W.; Van Verloigne, M.; Bourdeaudhuij, I.; De Brug, J.; Bjelland, M.; Lien, N.; Maes, L. Does parental involvement make a difference in school-based nutrition and physical activity interventions? A systematic review of randomized controlled trials. Int. J. Public Health 2012, 57, 673–678. [Google Scholar] [CrossRef]
- Golan, M.; Crow, S. Targeting Parents Exclusively in the Treatment of Childhood Obesity: Long-Term Results. Obes. Res. 2004, 12, 357–361. [Google Scholar] [CrossRef]
- Verjans-janssen, S.R.B.; Van De Kolk, I.; Van Kann, D.H.H.; Kremers, P.S.P.J.; Gerards, S.M.P.L. Effectiveness of school-based physical activity and nutrition interventions with direct parental involvement on children’s BMI and energy balance-related behaviors—A systematic review. PLoS ONE 2018, 13, e0204560. [Google Scholar] [CrossRef]
- World Health Organization. WHO Report of the Commission on Ending Childhood Obesity; World Health Organization: Geneva, Switzerland, 2016. [Google Scholar]
| Reference | Design, Setting and Population | Intervention Characteristics | Intervention Outcomes | Measures | Theoretical Basis | Overall Quality | |||
|---|---|---|---|---|---|---|---|---|---|
| Intervention Components | Duration, Follow-Up and Drop-Outs | Weight Status | Nutrition | PA | |||||
| Naidoo et al., 2009 [26] | Design: Cohort (one group pre- and post-test) Setting: Four primary schools in KwaZulu- Natal, South Africa Participants: 256 children in grade 6 from low- to middle- income settings. Boys/girls: 81/104 | Intervention: Diet, PA and school environment Concepts of PA and healthy eating habits were integrated with the existing curriculum. Programme was implemented by school personnel. Teachers were to advise and prompt children to make healthy choices. Schools were to establish health promoting environments by increasing the availability of healthy foods and decrease unhealthy foods at school/tuck shops. | Duration: 6 months Drop-outs: 71 (27.7%) | √ | √ | BMI, increased participation in sports and PA and the availability of healthy food choices. | No | Weak | |
| Draper et al., 2010 [27] | Design: Pre- and post-test study Setting: Five elementary/primary schools in Alexandra Township, Gauteng Province, South Africa Participants: 508 children in grade 4–6 Age: NR Boys/girls: NR | Intervention: PA Teachers provided physical education as part of an integrated curriculum (Healthnutz project) to children, while situational analysis and focus group discussions were conducted for teachers and research team monitors. | Duration: 6 months Follow-up: 4 months | √ | √ | Physical fitness, knowledge, self-efficacy and attitudes and weight. | No | Weak | |
| Harrabi et al., 2010 [30] | Design: Pre- and post-test quasi experiment Setting: Seventy-six classes from four public secondary schools in Tunisia Participants: 2200 children Age (range): 12–16 years Boys/girls: 1026/1174 | Intervention: Diet, PA and tobacco use This was delivered by project team, teachers and school doctors. Cognitive behavioural components of health knowledge and health promoting concepts such as tobacco use, PA, and healthy diet were integrated with the biological sciences and physical education curriculum. | Duration: 1 year Drop-outs: 138 (5.9%) | √ | √ | Knowledge, intentions, behaviours of PA and nutrition. | No | Weak | |
| Jemmott et al., 2011 [28] | Design: RCT Setting: 18 schools (14 urban and four rural) in Eastern Cape Province, South Africa Participants: 1057 children in grade 6 Age (mean): 12.4 years; 9–17 years Boys/girls: 558/499 | Intervention Diet, PA and cognitive-behavioural health Consisted of 12 one-hour modules, with two modules delivered during each of the six sessions on six consecutive school days; extracurricular sessions held at the end of the school day and included interactive exercises, games, brainstorming, role-playing and group discussions. Homework approach to involve parents or caregivers. | Duration: 13 months Drop-outs: 35 (3.3%) | √ | √ | Nutrition and PA knowledge, attitudes, self-efficacy and behaviours. | Social cognitive theory and the theory of planned behaviour | Strong | |
| Monyeki et al., 2012 [29] | Design: NR Setting: Two primary schools in Gauteng Province, South Africa Participants: 322 children Age (range): 9–13 years Boys: 322 | Intervention: PA Two 30 min exercise sessions per week during school hours. Lessons consisted of warm-up with stretching exercises, speed, strength, balance and cool down exercises. Intervention was provided by a trained physical education teacher. | Duration: 10 mo | √ | BMI and body fat. | No | Weak | ||
| Regaieg et al., 2013 [33] | Design: RCT Setting: Elementary schools in Sfax, Tunisia. Participants: 28 obese children Age (range): 12–14 years Boys/girls:16/12 | Intervention: PA Four extracurricular sessions (two sessions on weekdays and two on weekends) of 60 min per week aerobic exercises in addition to regular physical education that was provided by the schools. Exercises were performed under the supervision of a cardiologist. | Duration: 4 months Drop-outs: 0% | √ | BMI, weight, waist circumference and FFM. | No | Weak | ||
| Maatoug et al., 2015 [31] | Design: Quasi-experiment Settings: Six schools in Sousse, Tunisia Participants: 585 obese and overweight children in grades 7 and 8 Age: 13.1 ± 0.9 y and 13.5 ± 0.9 years in intervention and control groups Boys/girls: 236/349 | Intervention: Diet and PA School personnel including PA teachers and parents were trained on the relevance of healthy behaviours in obesity management. Schools were provided with PA equipment. Children were motivated to engage in regular PA and follow healthy diets in collective interactive sessions twice a week, with each session lasting one hour, as well as individual sessions for obese children. Intervention was facilitated by a dietician, psychologist, medical doctor and teachers (“Contrepoids” program). | Duration: 1 year Follow-up: 4 months Drop-outs: 180 (30.8%) | √ | BMI and zBMI. | No | Weak | ||
| De Villiers et al., 2016 [25] a | Design: Cluster RCT Setting: 16 primary schools (eight urban and eight rural) in low SES settings in Western Cape, South Africa Participants: 998 children in grade 4 Boys/girls: 471/526 | Intervention: Diet and PA HealthKick activities included the improvement of the school nutrition environment by developing healthy school nutrition policies, promoting the availability of healthier food options, initiation of vegetable gardens at schools and providing nutrition education support. Teachers were given training and resources, and were to organise an additional 15 min of PA per day and at least one healthy eating activity per month. Intervention was integrated with the existing nutrition curriculum. | Duration: 3 years | √ | √ | Nutrition behaviour, self-efficacy, overweight and obesity. | Socioecological theory | Weak | |
| Uys et al., 2016 [24] a | Design: Cluster RCT Setting: 16 primary schools (eight urban and eight rural) in low SES settings Participants: 998 children in grade 4 Boys/girls: 471/526 | Intervention: Diet and PA This was implemented by the intervention schools that were also given a toolkit containing teachers’ manual, curriculum manual, a resource box and PA resource bin (HealthKick). | Duration: 3 years | √ | Physical fitness levels and PA-related knowledge, attitudes and behaviours. | Socioecological theory | Weak | ||
| Ghamman et al. 2017 [32] | Design: Quasi-experiment Setting: 17 schools in Sousse, Tunisia Participants: 4003 children in grades 7 and 9 Age: 11–16 years Boys/girls: 1933/2070 | Intervention: Diet and PA Educational events were organised at least three times in a school year for children, parents and teachers. Classroom sessions were organised by teachers and consisted of interactive lessons of healthy eating, the benefits of regular PA, and ways to incorporate PA into usual activities. After-school soccer games were organised both within and between the schools to encourage PA. Programmes were delivered by student leaders, project team and teachers (“Together in Health”). | Duration: 3 years Follow-up: 1 year | √ | √ | √ | Weight status, PA, screen time behaviours, fruit and vegetable intake and fast food intake. | No | Weak |
| Reference and Outcome | Change Over Time in I and C and I vs. C | Intervention Effects as Reported in Primary Studies | Main Findings | ||||
|---|---|---|---|---|---|---|---|
| ∆I | ∆C | p-Value | ∆I–∆C | p-Value | |||
| Naidoo et al., 2009 [26] † | PA and sports participation increased significantly post-intervention (p < 0.05). Healthy food and drinks choices were available. | ||||||
| Number of sports participated in (average) | 10.0 * | ||||||
| PA > 5 times/week after school (%) | 20.0 * | ||||||
| Boys | |||||||
| Sit ups | +2.0 | ||||||
| Sit and reach (cm) | +0.29 | ||||||
| Standing broad jump (m) | +1.0 | ||||||
| BMI (kg/m2) | +0.8 | ||||||
| Girls | |||||||
| Sit ups | +1.0 | ||||||
| Sit and reach (cm) | +0.89 | ||||||
| Standing broad jump (m) | +0.0 | ||||||
| BMI (kg/m2) | +0.65 | ||||||
| Draper et al., 2010 [27] | Intervention improved self-efficacy for PA in the experimental group but not the controls (p < 0.05). PA knowledge improved in both the intervention and control groups. There was no effect on overall physical fitness scores. However, significant effects on sit and reach (p < 0.001), sit ups (p < 0.02), and shuttle run (p < 0.0001) between intervention and control groups were reported. Weight of children in the intervention significantly decreased, while change was reported for height. | ||||||
| Sit and reach (cm) | +4.40 | −10.50 | <0.001 | ||||
| Sit ups (in 30 s) | +1.80 | +0.30 | <0.02 | ||||
| Shuttle run (seconds) | −2.30 | +1.40 | <0.0001 | ||||
| Long jump (cm) | +9.70 | +14.6 | NS | ||||
| Ball throw (m) | −1.10 | +0.10 | NS | ||||
| PA self-efficacy | +0.30 | −0.01 | <0.05 | ||||
| PA knowledge | +0.56 | +0.47 | NS | ||||
| Harrabi et al., 2010 [30] | Nutrition knowledge and intention improved significantly in the intervention compared to the control group. The percentage of children with increased intake of fruits and vegetables increased in both groups, although significant in the controls. PA intention (p < 0.001) and behaviour (p < 0.001) improved in the intervention group. No significant differences in BMI in both groups. | ||||||
| What to eat for breakfast (%) | +25.1 | +1.2 | +22.9 | 0.0001 | |||
| Intention to eat breakfast (%) | +8.2 | +2.9 | +7.3 | 0.0001 | |||
| Fruit and vegetable intake ≥ 5 times/day (%) | +10.1 | +9.6 | −2.5 | NS | |||
| Intention to engage in PA daily (%) | +9.1 | +1.7 | +3.5 | ||||
| PA duration ≥ 30 min for at least six days a week (%) | +18.4 | +9.7 | −1.0 | 0.0001 | |||
| Jemmott et al., 2011 a [28] | More participants in health-promotion intervention than controls met 5-a-Day fruit (p = 0.003) and vegetable (p = 0.0001) intake, and PA guidelines (p = 0.0001). Health-promotion knowledge, attitude and intention increased (all p < 0.0001) in the intervention group. | ||||||
| Fruit and vegetable intake ≥ 5 times/day in the past 30 days (5-a-Day) (%) | +2.83 | −5.70 | 0.008 | +0.16 | |||
| Mean servings of fruit per day in the past 30 days | +0.49 | +0.33 | 0.003 | +0.19 | |||
| Mean servings of vegetables/day in the past 30 days | +0.98 | +0.17 | 0.0001 | +0.24 | |||
| Meeting PA guidelines in the past 7 days (%) | +7.10 | +7.10 | 0.0001 | +0.27 | |||
| Health knowledge | +3.48 | +1.38 | 0.0001 | +1.03 | |||
| Attitude toward health-promoting behaviour | +1.14 | +0.69 | 0.0001 | +0.89 | |||
| Intention for health-promoting behaviour | +1.02 | +0.54 | 0.0001 | +0.81 | |||
| Monyeki et al., 2012 [29] | Non-significant decreasing trends in BMI and percentage body fat (p = 0.32) in intervention group, whereas BMI tended to be stable with an increasing percentage body fat by age in the control group. | ||||||
| Body fat at age 12 y (%) | −0.32 | +1.62 | NS | ||||
| Body fat at age 13 y (%) | −1.03 | +2.31 | NS | ||||
| Regaieg et al., 2013 [33] | Significant decreases in BMI, FM and waist circumference in intervention (p < 0.001). In the controls, a non-significant increase (p = 0.11) in waist circumference was observed. There were increases in FFM in both groups, but this was higher in the intervention. | ||||||
| Weight (kg) | +0.70 | +2.60 | <0.001 | ||||
| BMI (kg/m2) | −0.60 | +0.50 | <0.01 | ||||
| FM (%) | −4.30 | −0.20 | <0.01 | ||||
| Waist circumference (cm) | −1.70 | +0.70 | <0.001 | ||||
| Maatoug et al., 2015 [31] | BMI z-score decreased significantly from pre-intervention to post-intervention and from post-intervention to 4-mo follow-up in the intervention group. In the control group, BMI z-score decreased significantly from pre- to post- intervention but nor from post- to follow-up. | ||||||
| BMI (kg/m2) | +0.25 | +0.49 *** | |||||
| BMI z score | −0.13 *** | −0.18 *** | |||||
| De Villiers et al., 2016 a [25] | Nutrition knowledge (p = 0.011) and self-efficacy (p = 0.039) significantly improved in the intervention group as compared with the controls. The intervention did not improve nutrition behaviour (p = 0.743) nor weight status of the children. | ||||||
| Nutrition knowledge | +2.52 | +0.60 | +1.92 ** | ||||
| Nutrition behaviour | −0.52 | −0.60 | NS | +0.09 | |||
| Self-efficacy | +0.36 | −0.35 | +0.71 * | ||||
| Overweight (%) | +1.00 | +1.00 | |||||
| Obesity (%) | −4.00 | +7.00 | |||||
| Uys et al., 2016 a [24] | Intervention did not improve overall physical fitness and determinants of PA behaviour. PA knowledge improved in both intervention (p < 0.005) and control ((p < 0.001) groups. Additionally, improvement was only observed in the sit-ups score of children in the intervention group (p < 0.05). | ||||||
| PA knowledge | −0.48 * | ||||||
| PA behaviour | −0.44 | ||||||
| PA self-efficacy | −0.38 | ||||||
| Sit and reach (cm) | −1.29 | ||||||
| Sit ups (in 30 s) | +1.62 * | ||||||
| Shuttle run (seconds) | +3.32 | ||||||
| Long jump (cm) | −5.75 | ||||||
| Ghamman et al., 2017 [32] | Overall, higher proportion of children (p = 0.010), boys (p = 0.021) and those ≥ 14 years (p = 0.004) in the intervention group met the recommended daily PA post-intervention, whereas, in the controls, an increase was observed only at follow-up (p = 0.023). Further, more children in the intervention group reported eating five fruits and vegetables daily (p = 0.02). Overweight prevalence reduced in the intervention group (p = 0.036). | ||||||
| Fruit and vegetable intake ≥ 5 times/day (%) | +3.2 * | −5.2 ** | |||||
| Fast food consumption ≥ 4 times/week (%) | −0.8 | +5.1 *** | |||||
| Meeting recommended PA (%) | −3.6 * | +0.1 | |||||
| Weekday screen time > 2 hr/day (%) | +1.4 | −2.1 | |||||
| Weekend screen day > 2 hr/day | −0.1 | −7.0 *** | |||||
| Prevalence of overweight (%) | −2.6 * | −1.0 | |||||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Adom, T.; De Villiers, A.; Puoane, T.; Kengne, A.P. School-Based Interventions Targeting Nutrition and Physical Activity, and Body Weight Status of African Children: A Systematic Review. Nutrients 2020, 12, 95. https://doi.org/10.3390/nu12010095
Adom T, De Villiers A, Puoane T, Kengne AP. School-Based Interventions Targeting Nutrition and Physical Activity, and Body Weight Status of African Children: A Systematic Review. Nutrients. 2020; 12(1):95. https://doi.org/10.3390/nu12010095
Chicago/Turabian StyleAdom, Theodosia, Anniza De Villiers, Thandi Puoane, and André Pascal Kengne. 2020. "School-Based Interventions Targeting Nutrition and Physical Activity, and Body Weight Status of African Children: A Systematic Review" Nutrients 12, no. 1: 95. https://doi.org/10.3390/nu12010095
APA StyleAdom, T., De Villiers, A., Puoane, T., & Kengne, A. P. (2020). School-Based Interventions Targeting Nutrition and Physical Activity, and Body Weight Status of African Children: A Systematic Review. Nutrients, 12(1), 95. https://doi.org/10.3390/nu12010095





