Use of Mid-Upper Arm Circumference (MUAC) to Predict Malnutrition among Sri Lankan Schoolchildren
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Participants
2.2. Anthropometric Assessment
2.3. Statistical Analysis
3. Results
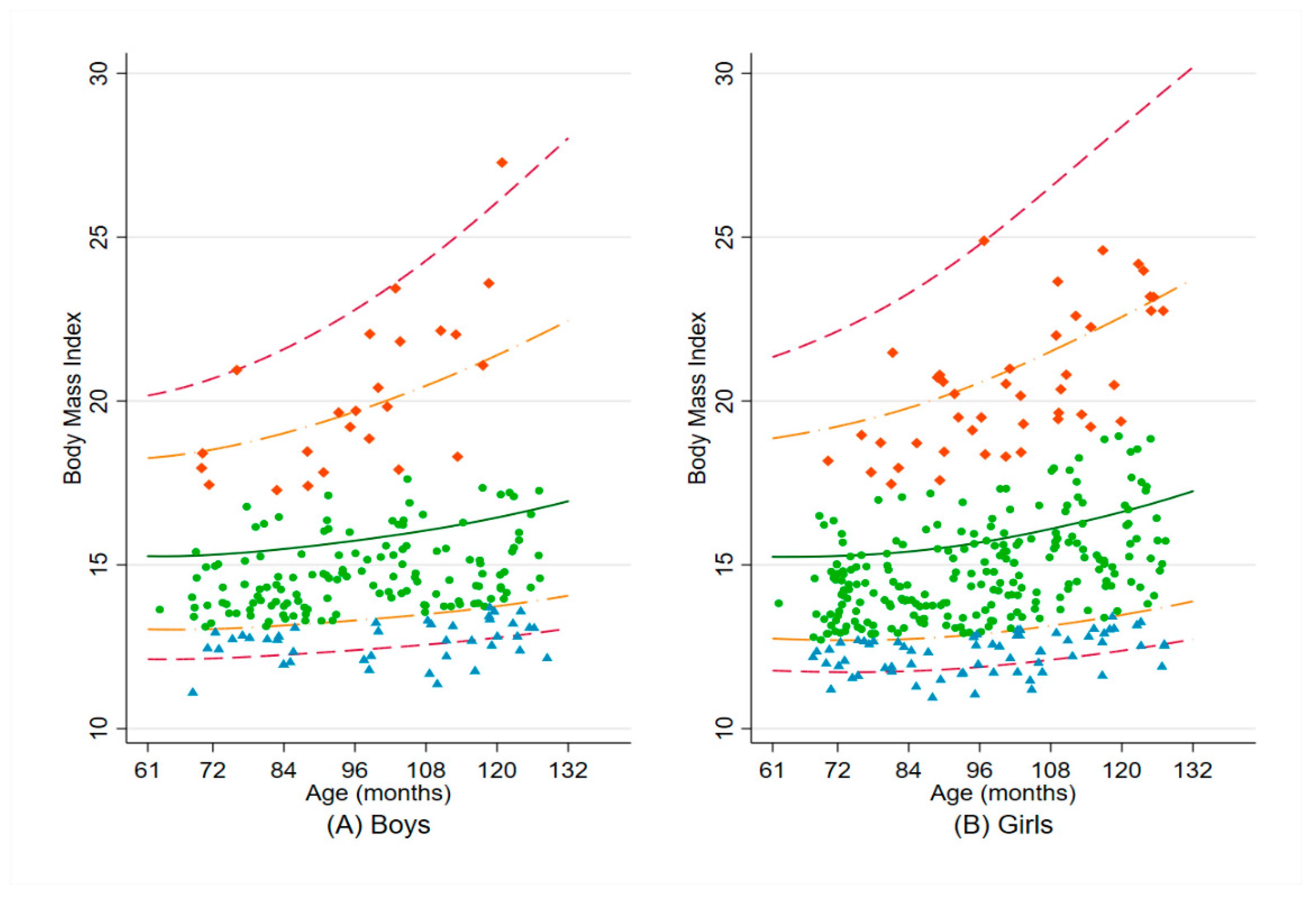
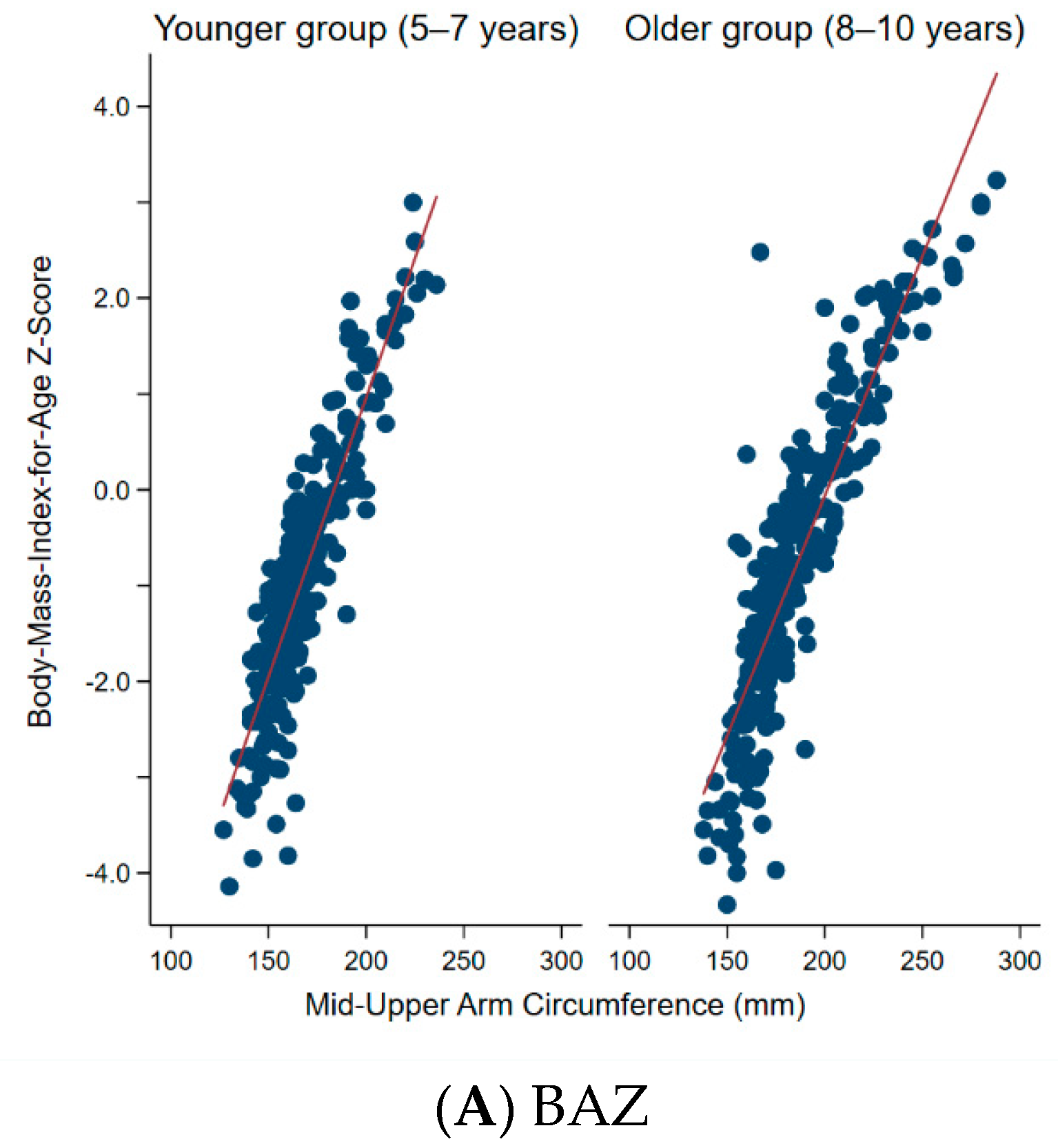
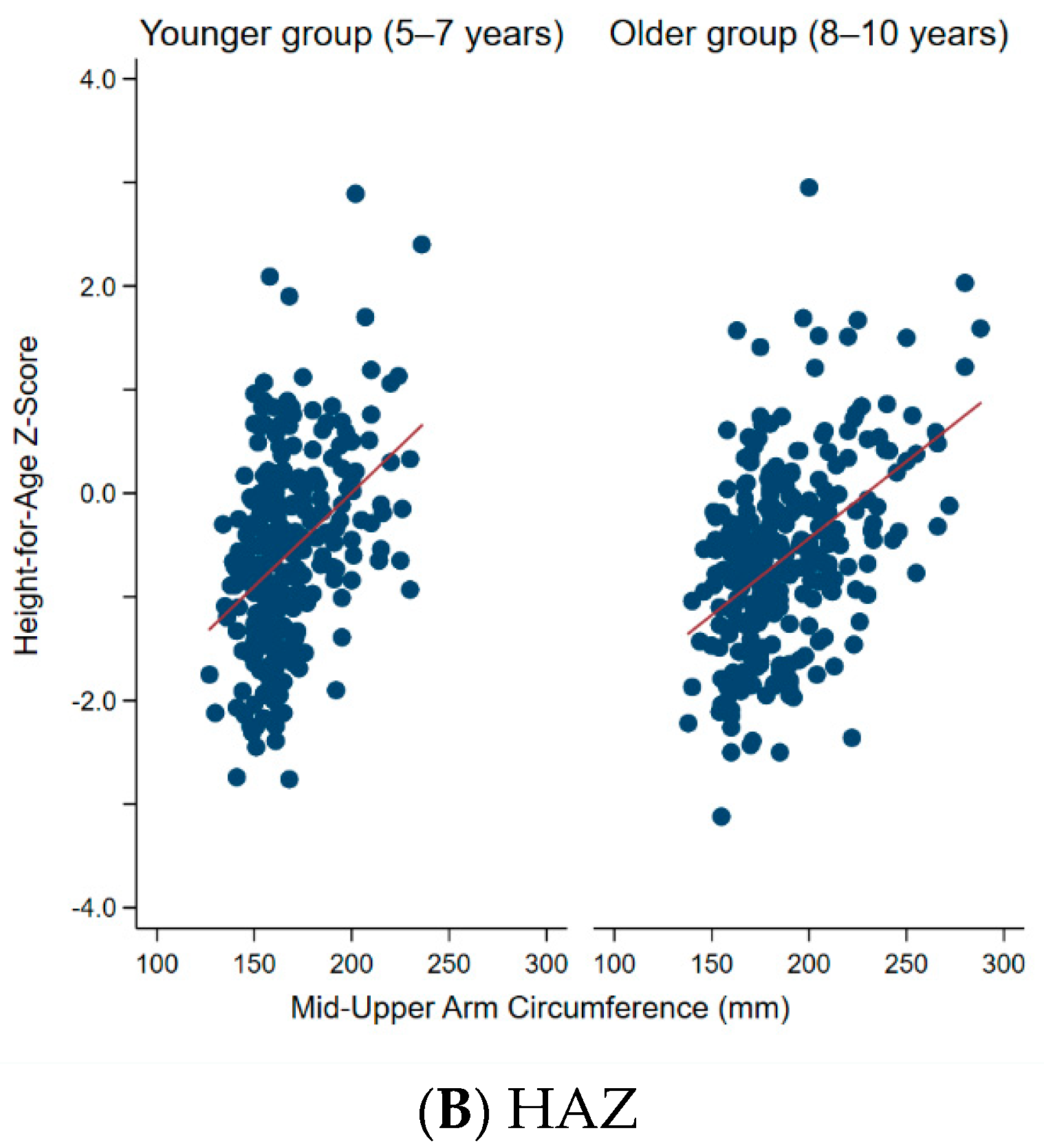
3.1. Correlations between MUAC and BAZ and HAZ
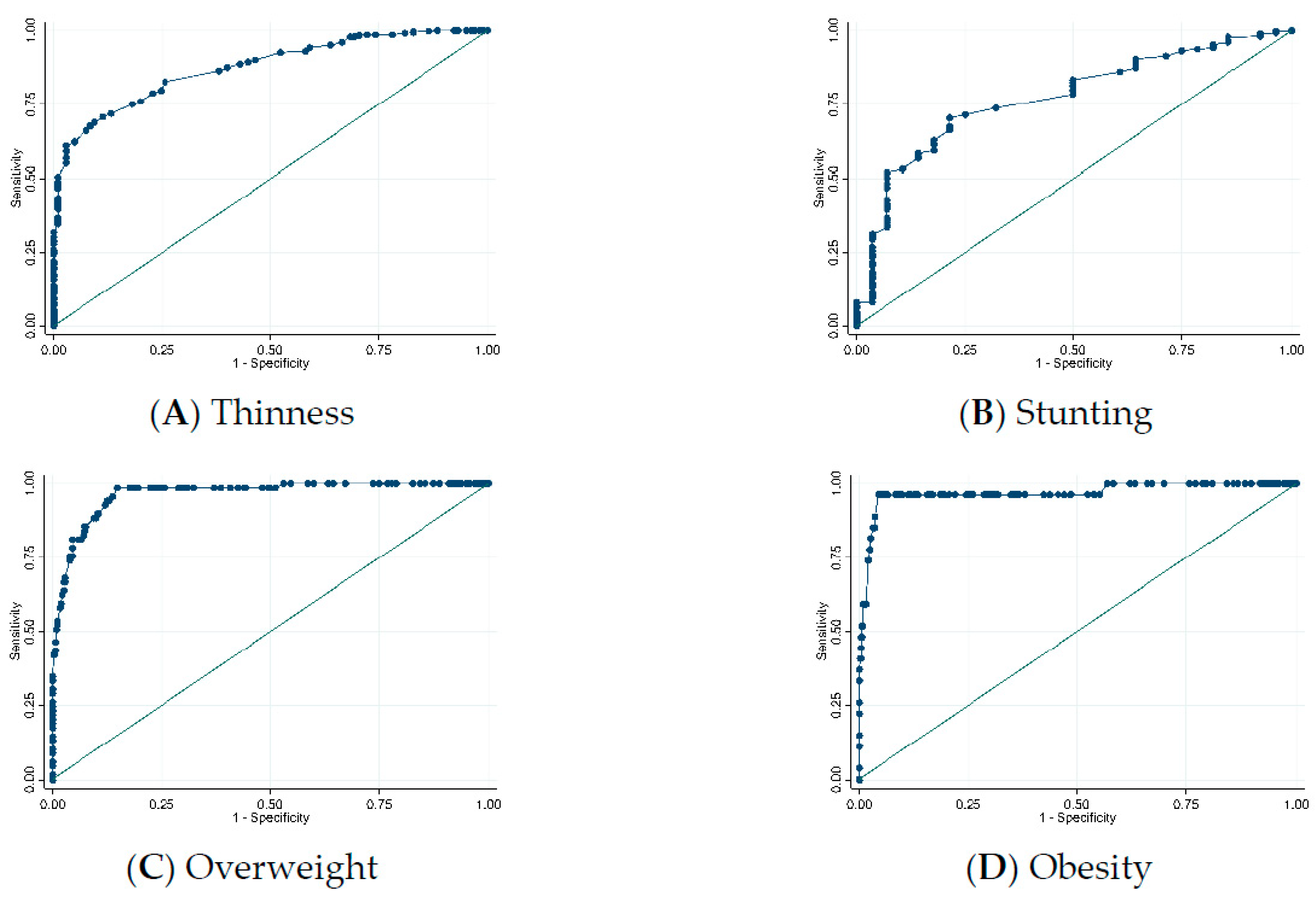
3.2. Ability of MUAC to Correctly Identify Thinness, Overweight, and Obesity
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Black, R.E.; Victora, C.G.; Walker, S.P.; Bhutta, Z.A.; Christian, P.; de Onis, M.; Ezzati, M.; Grantham-McGregor, S.; Katz, J.; Martorell, R.; et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 2013, 382, 427–451. [Google Scholar] [CrossRef]
- Shinsugi, C.; Gunasekara, D.; Gunawardena, N.K.; Subasinghe, W.; Miyoshi, M.; Kaneko, S.; Takimoto, H. Double burden of maternal and child malnutrition and socioeconomic status in urban Sri Lanka. PLoS ONE 2019, 14, e0224222. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health. Nutrition and Indigenous Medicine. Annual Health Bulletin 2015. Available online: http://www.health.gov.lk/moh_final/english/public/elfinder/files/publications/AHB/2017/AHB%202015.pdf (accessed on 15 May 2019).
- Victora, C.G.; Adair, L.; Fall, C.; Hallal, P.C.; Martorell, R.; Richter, L.; Sachdev, H.S. Maternal and child undernutrition: Consequences for adult health and human capital. Lancet 2008, 371, 340–357. [Google Scholar] [CrossRef]
- Williams, J.; Wake, M.; Hesketh, K.; Maher, E.; Waters, E. Health-related quality of life of overweight and obese children. JAMA 2005, 293, 70–76. [Google Scholar] [CrossRef] [PubMed]
- Weiss, R.; Dziura, J.; Burgert, T.S.; Tamborlane, W.V.; Taksali, S.E.; Yeckel, C.W.; Allen, K.; Lopes, M.; Savoye, M.; Morrison, J.; et al. Obesity and the metabolic syndrome in children and adolescents. N. Engl. J. Med. 2004, 350, 2362–2374. [Google Scholar] [CrossRef] [PubMed]
- Reilly, J.J.; Kelly, J. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: Systematic review. Int. J. Obes. 2011, 35, 891–898. [Google Scholar] [CrossRef] [PubMed]
- Goossens, S.; Bekele, Y.; Yun, O.; Harczi, G.; Ouannes, M.; Shepherd, S. Mid-upper arm circumference based nutrition programming: Evidence for a new approach in regions with high burden of acute malnutrition. PLoS ONE 2012, 7, e49320. [Google Scholar] [CrossRef] [PubMed]
- Tang, A.M.; Dong, K.; Deitchler, M.; Chung, M.; Maalouf-Manasseh, Z.; Tumilowicz, A.; Wanke, C. Use of Cutoffs for Mid-Upper Arm Circumference (MUAC) as an Indicator or Predictor of Nutritional and Health-Related Outcomes in Adolescents and Adults: A Systematic Review; Food and Nutrition Technical Assistance III Project (FANTA III)/FHI 360: Washington, DC, USA, 2013.
- Wieringa, F.T.; Gauthier, L.; Greffeuille, V.; Som, S.V.; Dijkhuizen, M.A.; Laillou, A.; Chamnan, C.; Berger, J.; Poirot, E. Identification of acute malnutrition in children in Cambodia requires both mid upper arm circumference and weight-for-height to offset gender bias of each indicator. Nutrients 2018, 10, 786. [Google Scholar] [CrossRef] [PubMed]
- Mwangome, M.K.; Fegan, G.; Fulford, T.; Prentice, A.M.; Berkley, J.A. Mid-upper arm circumference at age of routine infant vaccination to identify infants at elevated risk of death: A retrospective cohort study in the Gambia. Bull. World Health Org. 2012, 90, 887–894. [Google Scholar] [CrossRef] [PubMed]
- Mramba, L.; Ngari, M.; Mwangome, M.; Muchai, L.; Bauni, E.; Walker, A.S.; Gibb, D.M.; Fegan, G.; Berkley, J.A. A growth reference for mid upper arm circumference for age among school age children and adolescents, and validation for mortality: Growth curve construction and longitudinal cohort study. Br. Med. J. 2017, 358, j3423. [Google Scholar] [CrossRef] [PubMed]
- Weng, C.-H.; Tien, C.-P.; Li, C.-I.; L’Heureux, A.; Liu, C.-S.; Lin, C.-H.; Lin, C.-C.; Lai, S.-W.; Lai, M.-M.; Lin, W.-Y. Mid-upper arm circumference, calf circumference and mortality in Chinese long-term care facility residents: A prospective cohort study. BMJ Open 2018, 8, e020485. [Google Scholar] [CrossRef] [PubMed]
- Craig, E.; Bland, R.; Ndirangu, J.; Reilly, J.J. Use of mid-upper arm circumference for determining overweight and overfatness in children and adolescents. Arch. Dis. Child. 2014, 99, 763–766. [Google Scholar] [CrossRef] [PubMed]
- Talma, H.; van Dommelen, P.; Schweizer, J.J.; Bakker, B.; Kist-van Holthe, J.E.; Chinapaw, J.M.M.; Hirasing, R.A. Is mid-upper arm circumference in Dutch children useful in identifying obesity? Arch. Dis. Child. 2019, 104, 159–165. [Google Scholar] [CrossRef] [PubMed]
- Sharma, A.; Sharma, K.; Mathur, K.P. Growth pattern and prevalence of obesity in affluent schoolchildren of Delhi. Public Health Nutr. 2007, 10, 485–491. [Google Scholar] [CrossRef] [PubMed]
- de Onis, M.; Onyango, A.W.; Borghi, E.; Siyam, A.; Nishida, C.; Siekmann, J. Development of a WHO growth reference for school-aged children and adolescents. Bull. World Health Org. 2007, 85, 660–667. [Google Scholar] [CrossRef] [PubMed]
- Cashin, K.; Oot, L. Guide to Anthropometry: A Practical Tool for Program Planners, Managers, and Implementers; Food and Nutrition Technical Assistance III Project (FANTA III)/FHI 360: Washington, DC, USA, 2018.
- Chaput, J.P.; Katzmarzyk, P.T.; Barnes, J.D.; Fogelholm, M.; Hu, G.; Kuriyan, R.; Kurpad, A.; Lambert, E.V.; Maher, C.; Maia, J.; et al. Mid-upper arm circumference as a screening tool for identifying children with obesity: A 12-country study. Pediatr. Obes. 2017, 12, 439–445. [Google Scholar] [CrossRef] [PubMed]
| Variables | Total | Younger Group (5–7 Years) | Older Group (8–10 Years) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Boys (n = 94) | Girls (n = 165) | Boys (n = 108) | Girls (n = 171) | |||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| Age (years) | 7.6 | 1.5 | 6.2 | 0.7 | 6.2 | 0.7 | 8.9 | 0.8 | 8.8 | 0.8 |
| Height (cm) | 123.7 | 9.2 | 117.0 | 7.0 | 116.7 | 5.8 | 130.7 | 5.9 | 129.7 | 6.8 |
| Weight (kg) | 23.4 | 6.7 | 20.1 | 4.3 | 19.6 | 4.2 | 26.3 | 6.4 | 26.9 | 7.1 |
| BAZ | −0.8 | 1.5 | −0.9 | 1.3 | −0.9 | 1.4 | −1.0 | 1.7 | −0.6 | 1.5 |
| HAZ | −0.6 | 0.9 | −0.7 | 1.1 | −0.5 | 0.8 | −0.6 | 0.9 | −0.7 | 0.9 |
| MUAC (mm) | 177.8 | 26.6 | 167.9 | 19.4 | 167.8 | 21.3 | 185.0 | 29.5 | 188.3 | 27.2 |
| Birth weight (%) | ||||||||||
| <2500 g | 14.9 | 12.8 | 20.0 | 9.3 | 14.6 | |||||
| ≥2500 g | 82.9 | 87.2 | 78.8 | 83.3 | 84.2 | |||||
| Missing | 2.2 | 0.0 | 1.2 | 7.4 | 1.2 | |||||
| Variables | Cutoff (mm) | Sensitivity | Specificity | AUC |
|---|---|---|---|---|
| Thinness | 167.5 | 0.69 | 0.90 | 0.80 |
| Overweight | 190.5 | 0.99 | 0.85 | 0.92 |
| Obesity | 218.0 | 0.96 | 0.96 | 0.96 |
| Stunting | 162.5 | 0.70 | 0.79 | 0.74 |
| With Stratification by Age Group and Birth Weight: | ||||
| Thinness | ||||
| 5–7 years | 158.5 | 0.76 | 0.85 | 0.80 |
| 8–10 years | 171.5 | 0.82 | 0.95 | 0.89 |
| Birth weight < 2500 g | 175.5 | 0.45 | 1.00 | 0.72 |
| Birth weight ≥ 2500 g | 166.5 | 0.72 | 0.91 | 0.82 |
| Overweight | ||||
| 5–7 years | 190.5 | 1.00 | 0.94 | 0.97 |
| 8–10 years | 205.5 | 0.95 | 0.92 | 0.93 |
| Birth weight < 2500 g | 194.0 | 1.00 | 0.97 | 0.99 |
| Birth weight ≥ 2500 g | 190.5 | 0.98 | 0.84 | 0.91 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shinsugi, C.; Gunasekara, D.; Takimoto, H. Use of Mid-Upper Arm Circumference (MUAC) to Predict Malnutrition among Sri Lankan Schoolchildren. Nutrients 2020, 12, 168. https://doi.org/10.3390/nu12010168
Shinsugi C, Gunasekara D, Takimoto H. Use of Mid-Upper Arm Circumference (MUAC) to Predict Malnutrition among Sri Lankan Schoolchildren. Nutrients. 2020; 12(1):168. https://doi.org/10.3390/nu12010168
Chicago/Turabian StyleShinsugi, Chisa, Deepa Gunasekara, and Hidemi Takimoto. 2020. "Use of Mid-Upper Arm Circumference (MUAC) to Predict Malnutrition among Sri Lankan Schoolchildren" Nutrients 12, no. 1: 168. https://doi.org/10.3390/nu12010168
APA StyleShinsugi, C., Gunasekara, D., & Takimoto, H. (2020). Use of Mid-Upper Arm Circumference (MUAC) to Predict Malnutrition among Sri Lankan Schoolchildren. Nutrients, 12(1), 168. https://doi.org/10.3390/nu12010168





