Early Rehabilitation Program and Vitamin D Supplementation Improves Sensitivity of Balance and the Postural Control in Patients after Posterior Lumbar Interbody Fusion: A Randomized Trial
Abstract
1. Introduction
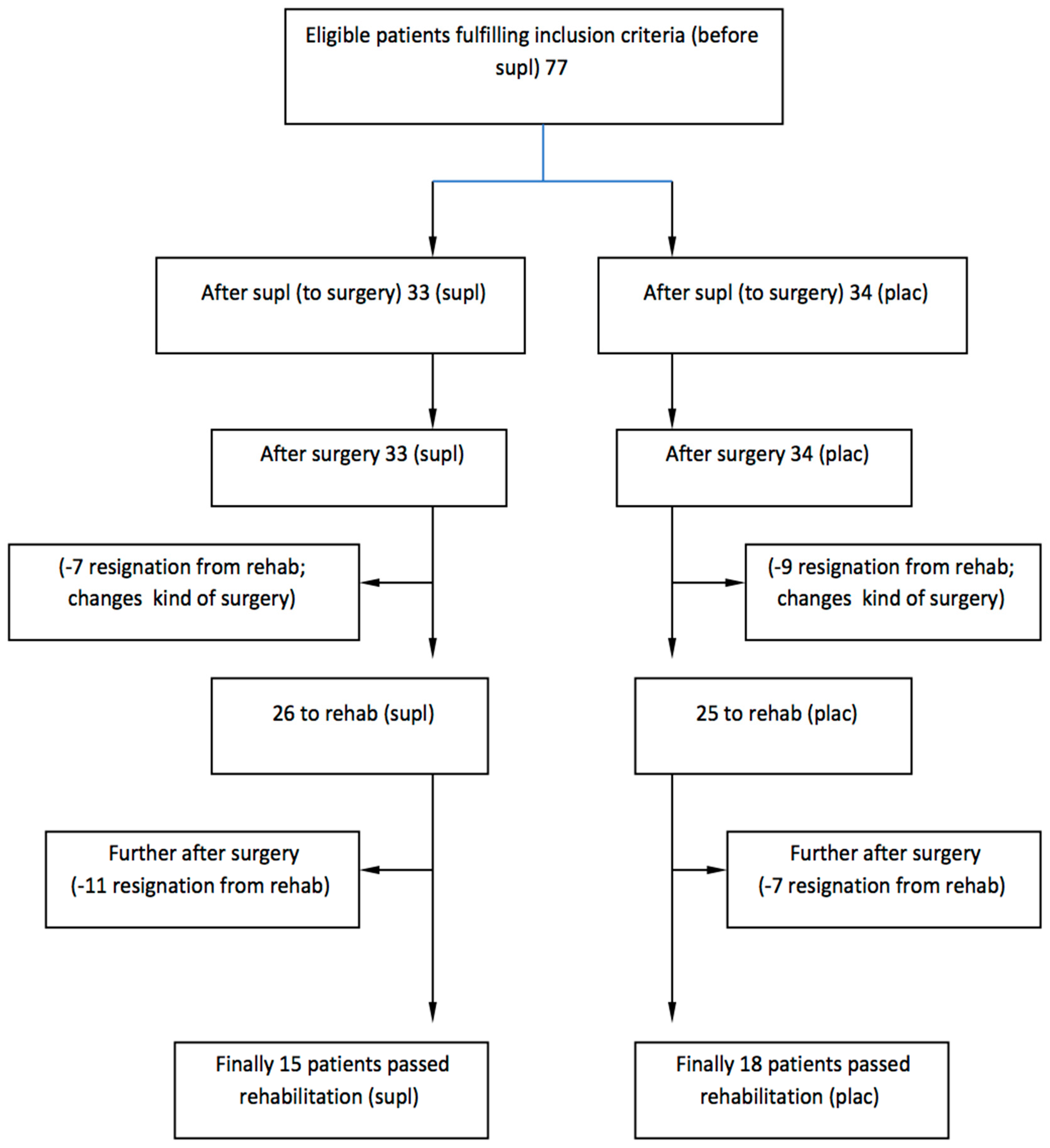
2. Materials and Methods
2.1. Design
2.2. Participants, Therapists, Centers
2.3. Intervention
2.4. Outcome Measures
2.4.1. Limits of Stability Test (LOS)
2.4.2. Postural Stability Test (PST)
2.4.3. Risk of Fall Test (RFT)
2.4.4. Rehabilitation Protocol
2.5. Data Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| PLIF | Posterior Lumbar Interbody Fusion |
| CRP | C-Reactive Protein |
| IL-6 | Interleukin 6 |
| BBS | The Biodex Balance System |
| PST | Postural Stability Test |
| LOS | Limits of Stability Test |
| RFT | Risk of Fall Test |
| MRI | magnetic resonance imaging |
References
- Tarnanen, S.P.; Neva, M.H.; Hakkinen, K.; Kankaanpaa, M.; Ylinen, J.; Kraemer, W.J.; Newton, R.U.; Hakkinen, A. Neutral spine control exercises in rehabilitation after lumbar spine fusion. J. Strength Cond Res. 2014, 28, 2018–2025. [Google Scholar] [CrossRef] [PubMed]
- Kawaguchi, Y.; Matsui, H.; Tsuji, H. Back muscle injury after posterior lumbar spine surgery. Part 2: Histologic and histochemical analyses in humans. Spine (Phila Pa 1976) 1994, 19, 2598–2602. [Google Scholar] [CrossRef] [PubMed]
- Kawaguchi, Y.; Yabuki, S.; Styf, J.; Olmarker, K.; Rydevik, B.; Matsui, H.; Tsuji, H. Back muscle injury after posterior lumbar spine surgery. Topographic evaluation of intramuscular pressure and blood flow in the porcine back muscle during surgery. Spine 1996, 21, 2683–2688. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.S.; Kang, K.C.; Chung, S.S.; Park, W.H.; Shin, W.J.; Seo, Y.G. How does back muscle strength change after posterior lumbar interbody fusion? J. Neurosurg. Spine 2017, 26, 163–170. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.T.; Tavera-Mendoza, L.E.; Laperriere, D.; Libby, E.; MacLeod, N.B.; Nagai, Y.; Bourdeau, V.; Konstorum, A.; Lallemant, B.; Zhang, R.; et al. Large-scale in silico and microarray-based identification of direct 1,25-dihydroxyvitamin D3 target genes. Mol. Endocrinol. 2005, 19, 2685–2695. [Google Scholar] [CrossRef] [PubMed]
- Beauchet, O.; Annweiler, C.; Verghese, J.; Fantino, B.; Herrmann, F.R.; Allali, G. Biology of gait control: Vitamin D involvement. Neurology 2011, 76, 1617–1622. [Google Scholar] [CrossRef] [PubMed]
- Gupta, R.; Sharma, U.; Gupta, N.; Kalaivani, M.; Singh, U.; Guleria, R.; Jagannathan, N.R.; Goswami, R. Effect of cholecalciferol and calcium supplementation on muscle strength and energy metabolism in vitamin D-deficient Asian Indians: A randomized, controlled trial. Clin. Endocrinol. 2010, 73, 445–451. [Google Scholar] [CrossRef] [PubMed]
- Janssen, H.C.; Samson, M.M.; Verhaar, H.J. Muscle strength and mobility in vitamin D-insufficient female geriatric patients: A randomized controlled trial on vitamin D and calcium supplementation. Aging Clin. Exp. Res. 2010, 22, 78–84. [Google Scholar] [CrossRef]
- Dzik, K.; Skrobot, W.; Kaczor, K.B.; Flis, D.J.; Karnia, M.; Libionka, W.; Antosiewicz, J.; Kloc, W.; Kaczor, J.J. Vitamin D Deficiency Is Associated with Muscle Atrophy and Reduced Mitochondrial Function in Patients with Chronic Low Back Pain. Oxidative Med. Cell. Longev. 2019, 2019, 6835341. [Google Scholar] [CrossRef]
- Mieszkowski, J.; Niespodzinski, B.; Kochanowicz, A.; Gmiat, A.; Prusik, K.; Prusik, K.; Kortas, J.; Ziemann, E.; Antosiewicz, J. The Effect of Nordic Walking Training Combined with Vitamin D Supplementation on Postural Control and Muscle Strength in Elderly People-A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2018, 15, 1951. [Google Scholar] [CrossRef]
- Van den Berghe, G.; Van Roosbroeck, D.; Vanhove, P.; Wouters, P.J.; De Pourcq, L.; Bouillon, R. Bone turnover in prolonged critical illness: Effect of vitamin D. J. Clin. Endocrinol. Metab. 2003, 88, 4623–4632. [Google Scholar] [CrossRef] [PubMed]
- Alamdari, A.; Mozafari, R.; Tafakhori, A.; Faghihi-Kashani, S.; Hafezi-Nejad, N.; Sheikhbahaei, S.; Naderi, N.; Ebadi, M.; Esteghamati, A. An inverse association between serum vitamin D levels with the presence and severity of impaired nerve conduction velocity and large fiber peripheral neuropathy in diabetic subjects. Neurol. Sci. 2015, 36, 1121–1126. [Google Scholar] [CrossRef] [PubMed]
- Warner, S.J.; Garner, M.R.; Nguyen, J.T.; Lorich, D.G. Perioperative vitamin D levels correlate with clinical outcomes after ankle fracture fixation. Arch. Orthop. Trauma Surg. 2016, 136, 339–344. [Google Scholar] [CrossRef] [PubMed]
- Breijawi, N.; Eckardt, A.; Pitton, M.B.; Hoelzl, A.J.; Giesa, M.; von Stechow, D.; Haid, F.; Drees, P. Bone mineral density and vitamin D status in female and male patients with osteoarthritis of the knee or hip. Eur. Surg. Res. 2009, 42, 1–10. [Google Scholar] [CrossRef] [PubMed]
- MacLaughlin, J.; Holick, M.F. Aging decreases the capacity of human skin to produce vitamin D3. J. Clin. Investig. 1985, 76, 1536–1538. [Google Scholar] [CrossRef] [PubMed]
- Andersen, R.; Molgaard, C.; Skovgaard, L.T.; Brot, C.; Cashman, K.D.; Chabros, E.; Charzewska, J.; Flynn, A.; Jakobsen, J.; Karkkainen, M.; et al. Teenage girls and elderly women living in northern Europe have low winter vitamin D status. Eur. J. Clin. Nutr. 2005, 59, 533–541. [Google Scholar] [CrossRef] [PubMed]
- Stephenson, J.; Zesiewicz, T.; Gooch, C.; Wecker, L.; Sullivan, K.; Jahan, I.; Kim, S.H. Gait and balance in adults with Friedreich’s ataxia. Gait Posture 2015, 41, 603–607. [Google Scholar] [CrossRef] [PubMed]
- Arnold, B.L.; Schmitz, R.J. Examination of Balance Measures Produced by the Biodex Stability System. J. Athl. Train. 1998, 33, 323–327. [Google Scholar]
- Shin, K.Y.; Park, K.K.; Moon, S.H.; Yang, I.H.; Choi, H.J.; Lee, W.S. Vitamin D deficiency adversely affects early post-operative functional outcomes after total knee arthroplasty. Knee Surgery Sports Traumatol. Arthrosc. 2016, 25, 3424–3430. [Google Scholar] [CrossRef]
- Stoker, G.E.; Buchowski, J.M.; Chen, C.T.; Kim, H.J.; Park, M.S.; Riew, K.D. Hypovitaminosis D and Cervical Disk Herniation among Adults Undergoing Spine Surgery. Glob. Spine J. 2013, 3, 231–236. [Google Scholar] [CrossRef]
- Pludowski, P.; Ducki, C.; Konstantynowicz, J.; Jaworski, M. Vitamin D status in Poland. Pol. Arch. Med. Wewn 2016, 126, 530–539. [Google Scholar] [CrossRef]
- Pludowski, P.; Grant, W.B.; Bhattoa, H.P.; Bayer, M.; Povoroznyuk, V.; Rudenka, E.; Ramanau, H.; Varbiro, S.; Rudenka, A.; Karczmarewicz, E.; et al. Vitamin d status in central europe. Int. J. Endocrinol. 2014, 2014, 589587. [Google Scholar] [CrossRef]
- Sun, X.; Cao, Z.B.; Tanisawa, K.; Taniguchi, H.; Kubo, T.; Higuchi, M. Effects of chronic endurance exercise training on serum 25(OH)D concentrations in elderly Japanese men. Endocrine 2018, 59, 330–337. [Google Scholar] [CrossRef]
- Pereira-Santos, M.; Costa, P.R.; Assis, A.M.; Santos, C.A.; Santos, D.B. Obesity and vitamin D deficiency: A systematic review and meta-analysis. Obes. Rev. 2015, 16, 341–349. [Google Scholar] [CrossRef]
- Lappe, J.M.; Travers-Gustafson, D.; Davies, K.M.; Recker, R.R.; Heaney, R.P. Vitamin D and calcium supplementation reduces cancer risk: Results of a randomized trial. Am. J. Clin. Nutr. 2007, 85, 1586–1591. [Google Scholar] [CrossRef]
- Dhesi, J.K.; Bearne, L.M.; Moniz, C.; Hurley, M.V.; Jackson, S.H.; Swift, C.G.; Allain, T.J. Neuromuscular and psychomotor function in elderly subjects who fall and the relationship with vitamin D status. J. Bone Miner. Res. 2002, 17, 891–897. [Google Scholar] [CrossRef]
- Clark, S.; Rose, D.J.; Fujimoto, K. Generalizability of the limits of stability test in the evaluation of dynamic balance among older adults. Arch. Phys. Med. Rehabil. 1997, 78, 1078–1084. [Google Scholar] [CrossRef]
- Hegde, D.; Mehra, S.; Babu, S.; Ballal, A. A Study to Assess the Functional Outcome of Decompression and Posterior Lumbar Interbody Fusion of Low Grade Spondylolisthesis of Lumbar Vertebra. J. Clin. Diagn. Res. 2017, 11, RC01–RC03. [Google Scholar] [CrossRef]
- Abbott, A.D.; Tyni-Lenne, R.; Hedlund, R. Early rehabilitation targeting cognition, behavior, and motor function after lumbar fusion: A randomized controlled trial. Spine 2010, 35, 848–857. [Google Scholar] [CrossRef]
- Dzik, K.; Skrobot, W.; Flis, D.J.; Karnia, M.; Libionka, W.; Kloc, W.; Kaczor, J.J. Vitamin D supplementation attenuates oxidative stress in paraspinal skeletal muscles in patients with low back pain. Eur. J. Appl. Physiol. 2018, 118, 143–151. [Google Scholar] [CrossRef]
- Riemann, B.L.; Lephart, S.M. The sensorimotor system, Part I: The physiologic basis of functional joint stability. J. Athl. Train. 2002, 37, 71–79. [Google Scholar]
- Khan, S.; Chang, R. Anatomy of the vestibular system: A review. NeuroRehabilitation 2013, 32, 437–443. [Google Scholar]
- Tarnanen, S.; Neva, M.H.; Kautiainen, H.; Ylinen, J.; Pekkanen, L.; Kaistila, T.; Vuorenmaa, M.; Hakkinen, A. The early changes in trunk muscle strength and disability following lumbar spine fusion. Disabil. Rehabil. 2013, 35, 134–139. [Google Scholar] [CrossRef]

| Week | Intervention |
|---|---|
| I | Instruction on ergonomic behavior during daily activities; instruction about deep trunk stabilization; and movements of the upper and lower limbs were performed while maintaining a neutral posture. |
| II–III | The same exercise as above but with increased challenge. Previous exercises were difficult; continuing deep stabilization with dissociated exercises; patients performed exercises in a closed chain at the wall in a standing position, which prepared them to plank, and balance exercises. |
| IV | Balance exercises with sensorimotor discs. |
| V | Additional isometric contractions of stabilizing muscles, changes in sequence and duration of movements. |
| Vit D Supplemented (EG) | Control Group (CG) | rANOVA | ||||||
|---|---|---|---|---|---|---|---|---|
| Baseline (n = 15) | After 5 weeks of supplementation (n = 15) | Baseline (n = 18) | After 5 weeks of supplementation (n = 18) | Time | ηp2 | Group x time interaction | ηp2 | |
| General | 0.35 (0.15) | 0.27 * (0.08) | 0.34 (0.20) | 0.32 (0.18) | p = 0.01 | 0.19 | p = 0.47 | 0.02 |
| AP | 0.21 (0.07) | 0.19 (0.08) | 0.32 (0.16) | 0.25 * (0.15) | p = 0.00 | 0.25 | p = 0.04 | 0.13 |
| ML | 0.12 (0.09) | 0.11 (0.08) | 0.16 (0.09) | 0.14 (0.07) | p = 0.45 | 0.02 | p = 0.88 | 0.00 |
| RFT | 1.03 (0.50) | 0.91 (0.38) | 1.16 (0.69) | 1.01 (0.39) | p = 0.20 | 0.06 | p = 0.81 | 0.00 |
| 25-0HD [nmol • L−1] | 48.37 (9.51) | 75.10 * (10.25) | 51.35 (18.05) | 49.46 (11.84) | p = 0.00 | 0.52 | p = 0.00 | 0.59 |
| Vit D Supplemented (EG) | Control Group (CG) | rANOVA | ||||||
|---|---|---|---|---|---|---|---|---|
| After operation (n = 15) | After 5 weeks of rehabilitation (n = 15) | After operation (n = 18) | After 5 weeks of rehabilitation (n = 18) | Time | ηp2 | Group x time interaction | ηp2 | |
| General | 0.31 (0.08) | 0.23 * (0.08) | 0.33 (0.18) | 0.29 (0.11) | p = 0.02 | 0.17 | p = 0.46 | 0.02 |
| AP | 0.26 (0.18) | 0.19 * (0.08) | 0.24 (0.08) | 0.22 (0.09) | p = 0.03 | 0.15 | p = 0.19 | 0.05 |
| ML | 0.13 (0.07) | 0.07 * (0.04) | 0.13 (0.08) | 0.13 (0.07) | p = 0.05 | 0.14 | p = 0.04 | 0.14 |
| Risk | 0.91 (0.38) | 1.03 (0.38) | 1.01 (0.39) | 1.08 (0.63) | p = 0.12 | 0.08 | p = 0.74 | 0.00 |
| 25-0H-D [nmol • L−1] | 75.10 (10.25) | 67.11 (11.45) | 49.46 (11.84) | 43.62 (11.92) | p = 0.00 | 0.34 | p = 0.57 | 0.01 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Skrobot, W.; Liedtke, E.; Krasowska, K.; Dzik, K.P.; Flis, D.J.; Samoraj-Dereszkiewicz, A.; Libionka, W.; Kortas, J.; Kloc, W.; Antosiewicz, J.; et al. Early Rehabilitation Program and Vitamin D Supplementation Improves Sensitivity of Balance and the Postural Control in Patients after Posterior Lumbar Interbody Fusion: A Randomized Trial. Nutrients 2019, 11, 2202. https://doi.org/10.3390/nu11092202
Skrobot W, Liedtke E, Krasowska K, Dzik KP, Flis DJ, Samoraj-Dereszkiewicz A, Libionka W, Kortas J, Kloc W, Antosiewicz J, et al. Early Rehabilitation Program and Vitamin D Supplementation Improves Sensitivity of Balance and the Postural Control in Patients after Posterior Lumbar Interbody Fusion: A Randomized Trial. Nutrients. 2019; 11(9):2202. https://doi.org/10.3390/nu11092202
Chicago/Turabian StyleSkrobot, Wojciech, Ewelina Liedtke, Katarzyna Krasowska, Katarzyna P. Dzik, Damian J. Flis, Anna Samoraj-Dereszkiewicz, Witold Libionka, Jakub Kortas, Wojciech Kloc, Jedrzej Antosiewicz, and et al. 2019. "Early Rehabilitation Program and Vitamin D Supplementation Improves Sensitivity of Balance and the Postural Control in Patients after Posterior Lumbar Interbody Fusion: A Randomized Trial" Nutrients 11, no. 9: 2202. https://doi.org/10.3390/nu11092202
APA StyleSkrobot, W., Liedtke, E., Krasowska, K., Dzik, K. P., Flis, D. J., Samoraj-Dereszkiewicz, A., Libionka, W., Kortas, J., Kloc, W., Antosiewicz, J., & Kaczor, J. J. (2019). Early Rehabilitation Program and Vitamin D Supplementation Improves Sensitivity of Balance and the Postural Control in Patients after Posterior Lumbar Interbody Fusion: A Randomized Trial. Nutrients, 11(9), 2202. https://doi.org/10.3390/nu11092202





