Pediatric-Adapted Liking Survey (PALS): A Diet and Activity Screener in Pediatric Care
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Study Procedure and Measures
2.3. Data Analysis
3. Results
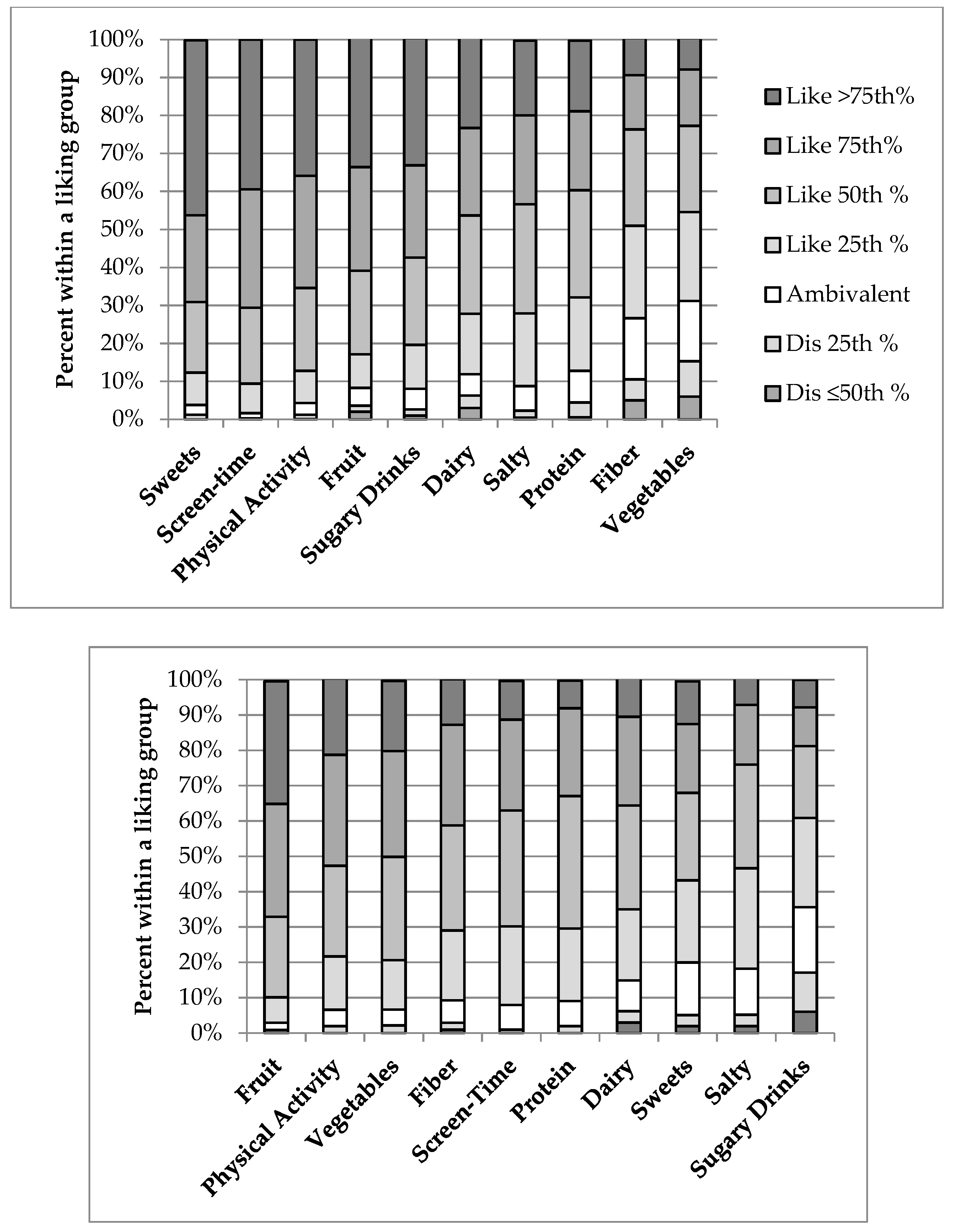
3.1. Relative Comparison of Parent and Child Food and Activity Liking
3.2. Internal Reliability of the HBI
3.3. Construct Validity of the HBI
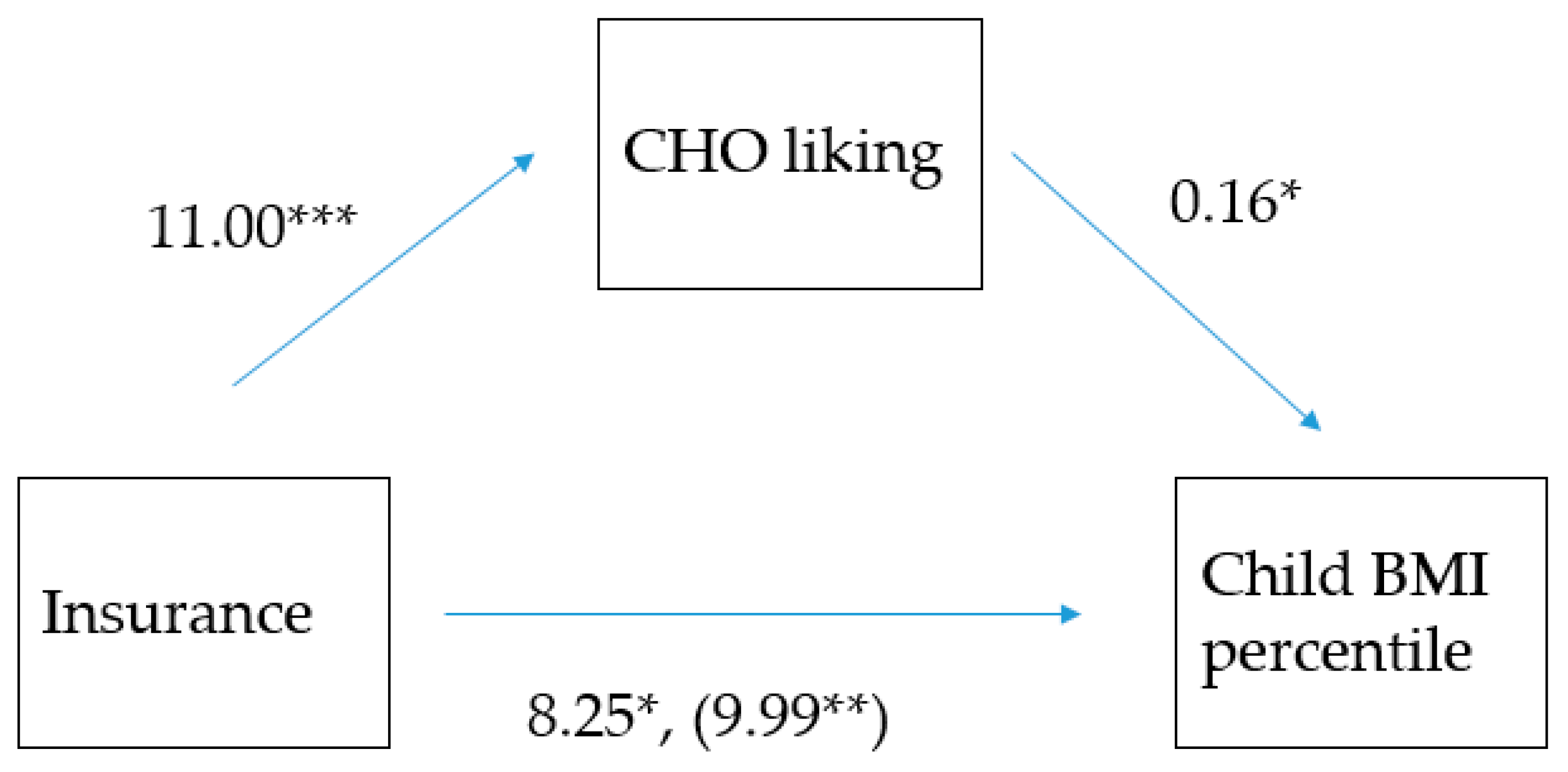
3.4. Concurrent Criterion Validity of the HBI
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Ng, M.; Fleming, T.; Robinson, M.; Thomson, B.; Graetz, N.; Margono, C.; Mullany, E.C.; Biryukov, S.; Abbafati, C.; Abera, S.F.; et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014, 384, 766–781. [Google Scholar] [CrossRef]
- Ogden, C.L.; Carroll, M.D.; Lawman, H.G.; Fryar, C.D.; Kruszon-Moran, D.; Kit, B.K.; Flegal, K.M. Trends in obesity prevalence among children and adolescents in the United States, 1988–1994 Through 2013–2014. JAMA 2016, 315, 2292–2299. [Google Scholar] [CrossRef]
- Institute of Medicine. Accelerating Progress in Obesity Prevention: Solving the Weight of the Nation; The National Academies Press: Washington, DC, USA, 2012; Available online: http://www.nationalacademies.org/hmd/Reports/2012/Accelerating-Progress-in-Obesity-Prevention.aspx (accessed on 1 June 2019).
- Division of Nutrition, Physical Activity, and Obesity, National Center for Chronic Disease Prevention and Health Promotion. Childhood Obesity Research Demonstration (CORD) 1.0. Available online: https://www.cdc.gov/obesity/strategies/healthcare/cord1.html (accessed on 1 June 2019).
- Kubicek, K.; Liu, D.; Beaudin, C.; Supan, J.; Weiss, G.; Lu, Y.; Kipke, M.D. A profile of nonurgent emergency department use in an urban pediatric hospital. Pediatr. Emerg. Care 2012, 28, 977–984. [Google Scholar] [CrossRef] [PubMed]
- Chandler, I.; Rosenthal, L.; Carroll-Scott, A.; Peters, S.M.; McCaslin, C.; Ickovics, J.R. Adolescents who visit the emergency department are more likely to make unhealthy dietary choices: An opportunity for behavioral intervention. J. Health Care Poor Underserv. 2015, 26, 701–711. [Google Scholar] [CrossRef] [PubMed]
- Haber, J.J.; Atti, S.; Gerber, L.M.; Waseem, M. Promoting an obesity education program among minority patients in a single urban pediatric Emergency Department (ED). Int. J. Emerg. Med. 2015, 8, 38. [Google Scholar] [CrossRef]
- Prendergast, H.M.; Close, M.; Jones, B.; Furtado, N.; Bunney, E.B.; Mackey, M.; Marquez, D.; Edison, M. On the frontline: Pediatric obesity in the emergency department. J. Natl. Med. Assoc. 2011, 103, 922–925. [Google Scholar] [CrossRef]
- Vaughn, L.M.; Nabors, L.; Pelley, T.J.; Hampton, R.R.; Jacquez, F.; Mahabee-Gittens, E.M. Obesity screening in the pediatric emergency department. Pediatr. Emerg. Care 2012, 28, 548–552. [Google Scholar] [CrossRef]
- Brown, C.L.; Halvorson, E.E.; Cohen, G.M.; Lazorick, S.; Skelton, J.A. Addressing childhood obesity: opportunities for prevention. Pediatr. Clin. North Am. 2015, 62, 1241–1261. [Google Scholar] [CrossRef]
- Gori, D.; Guaraldi, F.; Cinocca, S.; Moser, G.; Rucci, P.; Fantini, M.P. Effectiveness of educational and lifestyle interventions to prevent paediatric obesity: Systematic review and meta-analyses of randomized and non-randomized controlled trials. Obes. Sci. Pract. 2017, 3, 235–248. [Google Scholar] [CrossRef]
- National Cancer Institute, Division of Cancer Control and Population Sciences. Register of Validated Short Dietary Assessment Instruments. Available online: https://epi.grants.cancer.gov/diet/shortreg/ (accessed on 1 June 2019).
- National Collaborative on Childhood Obesity Research. Available online: http://www.nccor.org/nccor-tools/measures/ (accessed on 1 June 2019).
- Bel-Serrat, S.; Julian-Almarcegui, C.; Gonzalez-Gross, M.; Mouratidou, T.; Bornhorst, C.; Grammatikaki, E.; Kersting, M.; Cuenca-Garcia, M.; Gottrand, F.; Molnar, D.; et al. Correlates of dietary energy misreporting among European adolescents: The healthy lifestyle in Europe by nutrition in adolescence (HELENA) study. Br. J. Nutr. 2016, 115, 1439–1452. [Google Scholar] [CrossRef]
- Arheiam, A.; Albadri, S.; Laverty, L.; Harris, R. Reasons for low adherence to diet-diaries issued to pediatric dental patients: A collective case study. Patient Prefer. Adher. 2018, 12, 1401–1411. [Google Scholar] [CrossRef] [PubMed]
- Tuorila, H.; Huotilainen, A.; Lähteenmäki, L.; Ollila, S.; Tuomi-Nurmi, S.; Urala, N. Comparison of affective rating scales and their relationship to variables reflecting food consumption. Food Qual. Prefer. 2008, 19, 51–61. [Google Scholar] [CrossRef]
- Lanfer, A.; Knof, K.; Barba, G.; Veidebaum, T.; Papoutsou, S.; de Henauw, S.; Soos, T.; Moreno, L.A.; Ahrens, W.; Lissner, L. Taste preferences in association with dietary habits and weight status in European children: Results from the IDEFICS study. Int. J. Obes. (Lond.) 2012, 36, 27–34. [Google Scholar] [CrossRef]
- Sharafi, M.; Perrachio, H.; Scarmo, S.; Huedo-Medina, T.B.; Mayne, S.T.; Cartmel, B.; Duffy, V.B. Preschool-adapted liking survey (PALS): A brief and valid method to assess dietary quality of preschoolers. Child. Obes. 2015, 11, 530–540. [Google Scholar] [CrossRef] [PubMed]
- Duffy, V.B.; Lanier, S.A.; Hutchins, H.L.; Pescatello, L.S.; Johnson, M.K.; Bartoshuk, L.M. Food preference questionnaire as a screening tool for assessing dietary risk of cardiovascular disease within health risk appraisals. J. Am. Diet Assoc. 2007, 107, 237–245. [Google Scholar] [CrossRef] [PubMed]
- Pallister, T.; Sharafi, M.; Lachance, G.; Pirastu, N.; Mohney, R.P.; MacGregor, A.; Feskens, E.J.; Duffy, V.; Spector, T.D.; Menni, C. Food preference patterns in a UK twin cohort. Twin Res. Hum. Genet. 2015, 18, 793–805. [Google Scholar] [CrossRef] [PubMed]
- Sharafi, M.; Duffy, V.B.; Miller, R.J.; Winchester, S.B.; Sullivan, M.C. Dietary behaviors of adults born prematurely may explain future risk for cardiovascular disease. Appetite 2016, 99, 157–167. [Google Scholar] [CrossRef] [PubMed]
- Smith, S.; Johnson, S.; Oldman, S.; Duffy, V. Pediatric-adapted liking survey: Feasible and reliable dietary screening in clinical practice. Caries Res. 2018, 53, 153–159. [Google Scholar] [CrossRef]
- Vaidya, A.; Oli, N.; Krettek, A.; Eiben, G. Preference of food-items and physical activity of peri-urban children in Bhaktapur. J. Nepal Health Res. Counc. 2017, 15, 150–158. [Google Scholar] [CrossRef]
- Beckerman, J.P.; Alike, Q.; Lovin, E.; Tamez, M.; Mattei, J. The development and public health implications of food preferences in children. Front. Nutr. 2017, 4, 66. [Google Scholar] [CrossRef]
- Wang, Y.; Beydoun, M.A.; Li, J.; Liu, Y.; Moreno, L.A. Do children and their parents eat a similar diet? Resemblance in child and parental dietary intake: Systematic review and meta-analysis. J. Epidemiol. Community Health 2011, 65, 177–189. [Google Scholar] [CrossRef] [PubMed]
- Lipsky, L.M.; Haynie, D.L.; Liu, A.; Nansel, T.R. Resemblance of diet quality in families of youth with type 1 diabetes participating in a randomized controlled behavioral nutrition intervention trial in Boston, MA (2010–2013): A secondary data analysis. J. Acad. Nutr. Diet. 2019, 119, 98–105. [Google Scholar] [CrossRef] [PubMed]
- Sharafi, M.; Rawal, S.; Fernandez, M.L.; Huedo-Medina, T.B.; Duffy, V.B. Taste phenotype associates with cardiovascular disease risk factors via diet quality in multivariate modeling. Physiol. Behav. 2018, 194, 103–112. [Google Scholar] [CrossRef] [PubMed]
- Nicklas, T.A.; Morales, M.; Linares, A.; Yang, S.J.; Baranowski, T.; De Moor, C.; Berenson, G. Children’s meal patterns have changed over a 21-year period: The Bogalusa heart study. J. Am. Diet. Assoc. 2004, 104, 753–761. [Google Scholar] [CrossRef] [PubMed]
- Alzaben, A.S.; MacDonald, K.; Robert, C.; Haqq, A.; Gilmour, S.M.; Yap, J.; Mager, D.R. Diet quality of children post-liver transplantation does not differ from healthy children. Pediatr. Transpl. 2017, 21. [Google Scholar] [CrossRef] [PubMed]
- Wilson, T.A.; Liu, Y.; Adolph, A.L.; Sacher, P.M.; Barlow, S.E.; Pont, S.; Sharma, S.; Byrd-Williams, C.; Hoelscher, D.M.; Butte, N.F. Behavior modification of diet and parent feeding practices in a community—Vs. primary care-centered intervention for childhood obesity. J. Nutr. Educ. Behav. 2018, 51, 150–161. [Google Scholar] [CrossRef] [PubMed]
- Thomson, J.L.; Tussing-Humphreys, L.M.; Goodman, M.H.; Landry, A.S. Diet quality in a nationally representative sample of American children by sociodemographic characteristics. Am. J. Clin. Nutr. 2019, 109, 127–138. [Google Scholar] [CrossRef] [PubMed]
- Craike, M.; Wiesner, G.; Hilland, T.A.; Bengoechea, E.G. Interventions to improve physical activity among socioeconomically disadvantaged groups: An umbrella review. Int. J. Behav. Nutr. Phys. Act. 2018, 15, 43. [Google Scholar] [CrossRef]
- King, A.C.; Powell, K.E.; Members, A.C. 2018 Physical Activity Guidelines Advisory Committee Scientific Report. Available online: https://health.gov/paguidelines/second-edition/report/ (accessed on 18 June 2019).
- Guenther, P.M.; Kirkpatrick, S.I.; Reedy, J.; Krebs-Smith, S.M.; Buckman, D.W.; Dodd, K.W.; Casavale, K.O.; Carroll, R.J. The healthy eating index-2010 is a valid and reliable measure of diet quality according to the 2010 dietary guidelines for Americans. J. Nutr. 2014, 144, 399–407. [Google Scholar] [CrossRef]
- Rabinowitz, A.N.; Martin, J. Community food security in Connecticut: An evaluation and ranking of 169 towns; Zwick Center Outreach Report. 2012. Available online: https://ideas.repec.org/p/ags/ucozfr/154264.html (accessed on 18 June 2019).
- U.S. Department of Health and Human Services; U.S. Department of Agriculture. 2015–2020 Dietary Guidelines for Americans, 8th ed.; U.S. Department of Health and Human Services: Washington, DC, USA; U.S. Department of Agriculture: Washington, DC, USA, 2015. Available online: http://health.gov/dietaryguidelines/2015/guidelines/ (accessed on 1 June 2019).
- Centers for Disease Control and Prevention. Healthy Weight. BMI Percentile Calculator for Child and Teen. Available online: https://www.cdc.gov/healthyweight/bmi/calculator.html (accessed on 14 July 2019).
- Centers for Disease Control and Prevention. About Child & Teen BMI. Available online: https://www.cdc.gov/healthyweight/assessing/bmi/childrens_bmi/about_childrens_bmi.html#interpreted%20the%20same%20way (accessed on 14 July 2019).
- Collins, M.E. Body figure perceptions and preferences among preadolescent children. Int. J. Eat. Disord. 1991, 10, 199–208. [Google Scholar] [CrossRef]
- Marshall, S.; Burrows, T.; Collins, C.E. Systematic review of diet quality indices and their associations with health-related outcomes in children and adolescents. J. Hum. Nutr. Diet. 2014, 27, 577–598. [Google Scholar] [CrossRef] [PubMed]
- Hebestreit, A.; Intemann, T.; Siani, A.; De Henauw, S.; Eiben, G.; Kourides, Y.A.; Kovacs, E.; Moreno, L.A.; Veidebaum, T.; Krogh, V.; et al. Dietary patterns of European children and their parents in association with family food environment: results from the I. family study. Nutrients 2017, 9, 126. [Google Scholar] [CrossRef] [PubMed]
- Yee, A.Z.; Lwin, M.O.; Ho, S.S. The influence of parental practices on child promotive and preventive food consumption behaviors: A systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 47. [Google Scholar] [CrossRef] [PubMed]
- Bogl, L.H.; Silventoinen, K.; Hebestreit, A.; Intemann, T.; Williams, G.; Michels, N.; Molnar, D.; Page, A.S.; Pala, V.; Papoutsou, S.; et al. Familial resemblance in dietary intakes of children, adolescents, and parents: Does dietary quality play a role? Nutrients 2017, 9, 892. [Google Scholar] [CrossRef] [PubMed]
- Mennella, J.A.; Bobowski, N.K.; Reed, D.R. The development of sweet taste: From biology to hedonics. Rev. Endocr. Metab. Disord. 2016, 17, 171–178. [Google Scholar] [CrossRef]
- Wang, J.; Shang, L.; Light, K.; O’Loughlin, J.; Paradis, G.; Gray-Donald, K. Associations between added sugar (solid vs. liquid) intakes, diet quality, and adiposity indicators in Canadian children. Appl. Physiol. Nutr. Metab. 2015, 40, 835–841. [Google Scholar] [CrossRef] [PubMed]
- Verloigne, M.; Van Lippevelde, W.; Bere, E.; Manios, Y.; Kovacs, E.; Grillenberger, M.; Maes, L.; Brug, J.; De Bourdeaudhuij, I. Individual and family environmental correlates of television and computer time in 10- to 12-year-old European children: The ENERGY-project. BMC Public Health 2015, 15, 912. [Google Scholar] [CrossRef]
- Yao, C.A.; Rhodes, R.E. Parental correlates in child and adolescent physical activity: A meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 10. [Google Scholar] [CrossRef]
- Rhodes, R.E.; Lim, C. Promoting parent and child physical activity together: Elicitation of potential intervention targets and preferences. Health Educ. Behav. 2018, 45, 112–123. [Google Scholar] [CrossRef]
- Bolton, K.A.; Jacka, F.; Allender, S.; Kremer, P.; Gibbs, L.; Waters, E.; de Silva, A. The association between self-reported diet quality and health-related quality of life in rural and urban Australian adolescents. Aust. J. Rural Health 2016, 24, 317–325. [Google Scholar] [CrossRef]
- Hiza, H.A.; Casavale, K.O.; Guenther, P.M.; Davis, C.A. Diet quality of Americans differs by age, sex, race/ethnicity, income, and education level. J. Acad. Nutr. Diet. 2013, 113, 297–306. [Google Scholar] [CrossRef]
- Golley, R.K.; Hendrie, G.A.; McNaughton, S.A. Scores on the dietary guideline index for children and adolescents are associated with nutrient intake and socio-economic position but not adiposity. J. Nutr. 2011, 141, 1340–1347. [Google Scholar] [CrossRef] [PubMed]
- Andreyeva, T.; Tripp, A.S.; Schwartz, M.B. Dietary quality of Americans by Supplemental Nutrition Assistance Program participation status: A systematic review. Am. J. Prev. Med. 2015, 49, 594–604. [Google Scholar] [CrossRef]
- Robson, S.M.; Couch, S.C.; Peugh, J.L.; Glanz, K.; Zhou, C.; Sallis, J.F.; Saelens, B.E. Parent diet quality and energy intake are related to child diet quality and energy intake. J. Acad. Nutr. Diet. 2016, 116, 984–990. [Google Scholar] [CrossRef] [PubMed]
- Shang, L.; O’Loughlin, J.; Tremblay, A.; Gray-Donald, K. The association between food patterns and adiposity among Canadian children at risk of overweight. Appl. Physiol. Nutr. Metab. 2014, 39, 195–201. [Google Scholar] [CrossRef] [PubMed]
- Cagiran Yilmaz, F.; Cagiran, D.; Ozcelik, A.O. Adolescent obesity and its association with diet quality and cardiovascular risk factors. Ecol. Food Nutr. 2019, 58, 207–218. [Google Scholar] [CrossRef] [PubMed]
- Archero, F.; Ricotti, R.; Solito, A.; Carrera, D.; Civello, F.; Di Bella, R.; Bellone, S.; Prodam, F. Adherence to the Mediterranean diet among school children and adolescents living in northern Italy and unhealthy food behaviors associated to overweight. Nutrients 2018, 10. [Google Scholar] [CrossRef] [PubMed]
- Mellendick, K.; Shanahan, L.; Wideman, L.; Calkins, S.; Keane, S.; Lovelady, C. Diets rich in fruits and vegetables are associated with lower cardiovascular disease risk in adolescents. Nutrients 2018, 10. [Google Scholar] [CrossRef] [PubMed]
- Murakami, K. Associations between nutritional quality of meals and snacks assessed by the Food Standards Agency nutrient profiling system and overall diet quality and adiposity measures in British children and adolescents. Nutrition 2018, 49, 57–65. [Google Scholar] [CrossRef] [PubMed]
- Xu, F.; Cohen, S.A.; Greaney, M.L.; Greene, G.W. The association between US adolescents’ Weight status, weight perception, weight satisfaction, and their physical activity and dietary behaviors. Int. J. Environ. Res. Public Health 2018, 15. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Kubik, M.Y.; Fulkerson, J.A. Diet quality and fruit, vegetable, and sugar-sweetened beverage consumption by household food insecurity among 8- to 12-year-old children during summer months. J. Acad. Nutr. Diet. 2019. [Google Scholar] [CrossRef] [PubMed]
- Hunt, E.T.; Brazendale, K.; Dunn, C.; Boutte, A.K.; Liu, J.; Hardin, J.; Beets, M.W.; Weaver, R.G. Income, race and its association with obesogenic behaviors of U.S. children and adolescents, NHANES 2003–2006. J. Community Health 2019, 44, 507–518. [Google Scholar] [CrossRef] [PubMed]
- Ambrosini, G.L.; Emmett, P.M.; Northstone, K.; Howe, L.D.; Tilling, K.; Jebb, S.A. Identification of a dietary pattern prospectively associated with increased adiposity during childhood and adolescence. Int. J. Obes. (Lond.) 2012, 36, 1299–1305. [Google Scholar] [CrossRef] [PubMed]
- Elmesmari, R.; Martin, A.; Reilly, J.J.; Paton, J.Y. Comparison of accelerometer measured levels of physical activity and sedentary time between obese and non-obese children and adolescents: A systematic review. BMC Pediatr. 2018, 18, 106. [Google Scholar] [CrossRef] [PubMed]
- Vanhelst, J.; Beghin, L.; Duhamel, A.; De Henauw, S.; Ruiz, J.R.; Kafatos, A.; Androutsos, O.; Widhalm, K.; Mauro, B.; Sjostrom, M.; et al. Do adolescents accurately evaluate their diet quality? The HELENA study. Clin. Nutr. 2017, 36, 1669–1673. [Google Scholar] [CrossRef] [PubMed]
- Leung, C.W.; DiMatteo, S.G.; Gosliner, W.A.; Ritchie, L.D. Sugar-sweetened beverage and water intake in relation to diet quality in U.S. children. Am. J. Prev. Med. 2018, 54, 394–402. [Google Scholar] [CrossRef] [PubMed]
- De Miguel-Etayo, P.; Moreno, L.A.; Santabarbara, J.; Martin-Matillas, M.; Azcona-San Julian, M.C.; Marti Del Moral, A.; Campoy, C.; Marcos, A.; Garagorri, J.M.; Group, E.S. Diet quality index as a predictor of treatment efficacy in overweight and obese adolescents: The EVASYON study. Clin. Nutr. 2019, 38, 782–790. [Google Scholar] [CrossRef] [PubMed]
- Arsenault, B.J.; Lamarche, B.; Despres, J.P. Targeting overconsumption of sugar-sweetened beverages vs. overall poor diet quality for cardiometabolic diseases risk prevention: place your bets! Nutrients 2017, 9. [Google Scholar] [CrossRef] [PubMed]
- Tovar, A.; Chui, K.; Hyatt, R.R.; Kuder, J.; Kraak, V.I.; Choumenkovitch, S.F.; Hastings, A.; Bloom, J.; Economos, C.D. Healthy-lifestyle behaviors associated with overweight and obesity in US rural children. BMC Pediatr. 2012, 12, 102. [Google Scholar] [CrossRef]
- Sugiyama, T.; Horino, M.; Inoue, K.; Kobayashi, Y.; Shapiro, M.F.; McCarthy, W.J. Trends of child’s weight perception by children, parents, and healthcare professionals during the time of terminology change in childhood obesity in the United States, 2005–2014. Child. Obes. 2016, 12, 463–473. [Google Scholar] [CrossRef] [PubMed]
- Sisson, S.B.; Shay, C.M.; Broyles, S.T.; Leyva, M. Television-viewing time and dietary quality among U.S. children and adults. Am. J. Prev. Med. 2012, 43, 196–200. [Google Scholar] [CrossRef] [PubMed]
- Strasburger, V.C.; Jordan, A.B.; Donnerstein, E. Health effects of media on children and adolescents. Pediatrics 2010, 125, 756–767. [Google Scholar] [CrossRef] [PubMed]
- Bauer, K.W.; Nelson, M.C.; Boutelle, K.N.; Neumark-Sztainer, D. Parental influences on adolescents’ physical activity and sedentary behavior: Longitudinal findings from Project EAT-II. Int. J. Behav. Nutr. Phys. Act. 2008, 5, 12. [Google Scholar] [CrossRef] [PubMed]
- Labonte, M.E.; Kirkpatrick, S.I.; Bell, R.C.; Boucher, B.A.; Csizmadi, I.; Koushik, A.; L’Abbe, M.R.; Massarelli, I.; Robson, P.J.; Rondeau, I.; et al. Dietary assessment is a critical element of health research—Perspective from the partnership for advancing nutritional and dietary assessment in Canada. Appl. Physiol. Nutr. Metab. 2016, 41, 1096–1099. [Google Scholar] [CrossRef] [PubMed]
- Garnier, S.; Vallee, K.; Lemoine-Morel, S.; Joffroy, S.; Drapeau, V.; Tremblay, A.; Auneau, G.; Mauriege, P. Food group preferences and energy balance in moderately obese postmenopausal women subjected to brisk walking program. Appl. Physiol. Nutr. Metab. 2015, 40, 741–748. [Google Scholar] [CrossRef] [PubMed]
- Beheshti, R.; Jones-Smith, J.C.; Igusa, T. Taking dietary habits into account: A computational method for modeling food choices that goes beyond price. PLoS ONE 2017, 12, e0178348. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.H.; Shelley, M.; Liu, C.T.; Chang, Y.C. Assessing the association of food preferences and self-reported psychological well-being among middle-aged and older adults in contemporary china-results from the china health and nutrition survey. Int. J. Environ. Res. Public Health 2018, 15. [Google Scholar] [CrossRef]
- Fletcher, S.; Wright, C.; Jones, A.; Parkinson, K.; Adamson, A. Tracking of toddler fruit and vegetable preferences to intake and adiposity later in childhood. Matern. Child Nutr. 2017, 13. [Google Scholar] [CrossRef] [PubMed]
- Ramsay, S.A.; Rudley, M.; Tonnemaker, L.E.; Price, W.J. A comparison of college students’ reported fruit and vegetable liking and intake from childhood to adulthood. J. Am. Coll. Nutr. 2017, 36, 28–37. [Google Scholar] [CrossRef]
- Park, H.; Shin, Y.; Kwon, O.; Kim, Y. Association of sensory liking for fat with dietary intake and metabolic syndrome in korean adults. Nutrients 2018, 10. [Google Scholar] [CrossRef]
- Charlot, K.; Malgoyre, A.; Bourrilhon, C. Proposition for a shortened version of the leeds food preference questionnaire (LFPQ). Physiol. Behav. 2019, 199, 244–251. [Google Scholar] [CrossRef] [PubMed]
- Potter, C.; Griggs, R.L.; Ferriday, D.; Rogers, P.J.; Brunstrom, J.M. Individual variability in preference for energy-dense foods fails to predict child BMI percentile. Physiol. Behav. 2017, 176, 3–8. [Google Scholar] [CrossRef] [PubMed]
- Low, J.Y.Q.; Lacy, K.E.; McBride, R.L.; Keast, R.S.J. The associations between oral complex carbohydrate sensitivity, BMI, liking, and consumption of complex carbohydrate based foods. J. Food Sci. 2018, 83, 2227–2236. [Google Scholar] [CrossRef] [PubMed]
- Ledikwe, J.H.; Ello-Martin, J.; Pelkman, C.L.; Birch, L.L.; Mannino, M.L.; Rolls, B.J. A reliable, valid questionnaire indicates that preference for dietary fat declines when following a reduced-fat diet. Appetite 2007, 49, 74–83. [Google Scholar] [CrossRef]
- Lowenstein, L.M.; Perrin, E.M.; Berry, D.; Vu, M.B.; Pullen Davis, L.; Cai, J.; Tzeng, J.P.; Ammerman, A.S. Childhood obesity prevention: Fathers’ reflections with healthcare providers. Child. Obes. 2013, 9, 137–143. [Google Scholar] [CrossRef] [PubMed]
- Groele, B.; Glabska, D.; Gutkowska, K.; Guzek, D. Mother’s fruit preferences and consumption support similar attitudes and behaviors in their children. Int. J. Environ. Res. Public Health 2018, 15. [Google Scholar] [CrossRef] [PubMed]
- Vollmer, R.L.; Baietto, J. Practices and preferences: Exploring the relationships between food-related parenting practices and child food preferences for high fat and/or sugar foods, fruits, and vegetables. Appetite 2017, 113, 134–140. [Google Scholar] [CrossRef] [PubMed]
- Nekitsing, C.; Hetherington, M.M.; Blundell-Birtill, P. Developing healthy food preferences in preschool children through taste exposure, sensory learning, and nutrition education. Curr. Obes. Rep. 2018, 7, 60–67. [Google Scholar] [CrossRef]
- Marty, L.; Miguet, M.; Bournez, M.; Nicklaus, S.; Chambaron, S.; Monnery-Patris, S. Do hedonic- versus nutrition-based attitudes toward food predict food choices? A cross-sectional study of 6- to 11-year-olds. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 162. [Google Scholar] [CrossRef]
- Jalkanen, H.; Lindi, V.; Schwab, U.; Kiiskinen, S.; Venalainen, T.; Karhunen, L.; Lakka, T.A.; Eloranta, A.M. Eating behaviour is associated with eating frequency and food consumption in 6-8 year-old children: The physical activity and nutrition in children (PANIC) study. Appetite 2017, 114, 28–37. [Google Scholar] [CrossRef]
- Duffy, V.B.; Smith, S. Leveraging Technology to Deliver Tailored SNAP-Ed Messages. Available online: https://snaped.fns.usda.gov/success-stories/leveraging-technology-deliver-tailored-snap-ed-messages (accessed on 14 July 2019).
- Sadeghirad, B.; Duhaney, T.; Motaghipisheh, S.; Campbell, N.R.; Johnston, B.C. Influence of unhealthy food and beverage marketing on children’s dietary intake and preference: A systematic review and meta-analysis of randomized trials. Obes. Rev. 2016, 17, 945–959. [Google Scholar] [CrossRef] [PubMed]
- De Wild, V.W.T.; de Graaf, C.; Jager, G. Use of different vegetable products to increase preschool-aged children’s preference for and intake of a target vegetable: A randomized controlled trial. J. Acad. Nutr. Diet. 2017, 117, 859–866. [Google Scholar] [CrossRef] [PubMed]
- Magarey, A.; Mauch, C.; Mallan, K.; Perry, R.; Elovaris, R.; Meedeniya, J.; Byrne, R.; Daniels, L. Child dietary and eating behavior outcomes up to 3.5 years after an early feeding intervention: The NOURISH RCT. Obesity (Silver Spring) 2016, 24, 1537–1545. [Google Scholar] [CrossRef] [PubMed]
- Cunningham-Sabo, L.; Lohse, B. Cooking with Kids positively affects fourth graders’ vegetable preferences and attitudes and self-efficacy for food and cooking. Child. Obes. 2013, 9, 549–556. [Google Scholar] [CrossRef] [PubMed]
- Wall, D.E.; Least, C.; Gromis, J.; Lohse, B. Nutrition education intervention improves vegetable-related attitude, self-efficacy, preference, and knowledge of fourth-grade students. J. Sch. Health 2012, 82, 37–43. [Google Scholar] [CrossRef] [PubMed]
- Ebneter, D.S.; Latner, J.D.; Nigg, C.R. Is less always more? The effects of low-fat labeling and caloric information on food intake, calorie estimates, taste preference, and health attributions. Appetite 2013, 68, 92–97. [Google Scholar] [CrossRef]
- Carbonneau, E.; Bradette-Laplante, M.; Lamarche, B.; Provencher, V.; Begin, C.; Robitaille, J.; Desroches, S.; Vohl, M.C.; Corneau, L.; Lemieux, S. Development and validation of the food liking questionnaire in a French-Canadian population. Nutrients 2017, 9, 1337. [Google Scholar] [CrossRef]
- Scarmo, S.; Henebery, K.; Peracchio, H.; Cartmel, B.; Lin, H.; Ermakov, I.V.; Gellermann, W.; Bernstein, P.S.; Duffy, V.B.; Mayne, S.T. Skin carotenoid status measured by resonance Raman spectroscopy as a biomarker of fruit and vegetable intake in preschool children. Eur. J. Clin. Nutr. 2012, 66, 555–560. [Google Scholar] [CrossRef]
- Freitas, A.; Albuquerque, G.; Silva, C.; Oliveira, A. Appetite-related eating behaviours: An overview of assessment methods, determinants and effects on children’s weight. Ann. Nutr. Metab. 2018, 73, 19–29. [Google Scholar] [CrossRef]
- Fernandez-Alvira, J.M.; Bammann, K.; Eiben, G.; Hebestreit, A.; Kourides, Y.A.; Kovacs, E.; Michels, N.; Pala, V.; Reisch, L.; Russo, P.; et al. Prospective associations between dietary patterns and body composition changes in European children: The IDEFICS study. Public Health Nutr. 2017, 20, 3257–3265. [Google Scholar] [CrossRef]
- Weber, D.R.; Moore, R.H.; Leonard, M.B.; Zemel, B.S. Fat and lean BMI reference curves in children and adolescents and their utility in identifying excess adiposity compared with BMI and percentage body fat. Am. J. Clin. Nutr. 2013, 98, 49–56. [Google Scholar] [CrossRef] [PubMed]
- Oldman, S. Improving Diet & Physical Activity Behaviors through Tailored Mhealth Messages: Application to Childhood Obesity Prevention in a Pediatric Emergency Department. Master’s Thesis, Health Promotion Sciences, University of Connecticut, Mansfield, CT, USA, 2018. [Google Scholar]
- U.S. Department of Agriculture. SNAP-Ed Connection. Available online: https://snaped.fns.usda.gov/ (accessed on 14 July 2019).

| n = 925 | % | |
|---|---|---|
| Age (Avg. 10.9 years) | ||
| 5–<9 year | 356 | 38 |
| 9–<13 year | 257 | 28 |
| 13–17 year | 312 | 34 |
| Sex | ||
| Male | 463 | 50.1 |
| Female | 462 | 49.9 |
| Race/Ethnicity | ||
| Caucasian | 357 | 38.6 |
| Black | 133 | 14.4 |
| Hispanic | 344 | 37.2 |
| Other | 91 | 9.8 |
| Insurance | ||
| Private | 382 | 41.3 |
| Public | 507 | 54.8 |
| Self pay | 16 | 1.7 |
| Other | 20 | 2.2 |
| Income Level *,a | ||
| <$21,432 | 26 | 2.8 |
| $21,433–41,186 | 288 | 31.1 |
| $41,187–68,212 | 245 | 26.5 |
| $68,213–112,262 | 313 | 33.8 |
| >$112,263 | 29 | 3.1 |
| Food Insecurity *,b | ||
| Greatest risk | 574 | 62.1 |
| Higher than average risk | 102 | 11 |
| Lower than average risk | 134 | 14.5 |
| Lowest risk | 99 | 10.7 |
| Question | Test Statistic |
|---|---|
| Reliability | |
| How internally consistent is the total index? | Cronbach’s Alpha |
| What are the relationships among the index components? | Pearson’s r correlations between each component |
| Which components have the most influence on the total index? | Pearson’s r correlations between each component and the total index |
| Construct and Concurrent Criterion Validity | |
| Does the index score foods and behaviors based on those recommended by the 2015 Dietary Guidelines? | Descriptive statistics |
| Does the index allow for sufficient variation in scores among individual? | Measures of central tendency, histogram, normality testing (Kolmogorov-Smirnov) |
| What is the underlying structure of the index (i.e., > 1 dimension)? | Principal component analysis and plot; derived factors to explain >50% of variance |
| Does the index distinguish between groups with known differences (i.e., concurrent criterion validity)? | Descriptive statistics, ANOVA with post-hoc analysis, ANCOVA, multiple regression analysis between demographic characteristics, PA liking and child’s BMI-P |
| 5–<18 Years | 5–<9 Years | 9–<13 Years | 13–<18 Years | |||||
|---|---|---|---|---|---|---|---|---|
| Count | % * | Count | % * | Count | % * | Count | % * | |
| 5th–<85th percentile | ||||||||
| Male | 275 | 29.7 | 102 | 28.7 | 74 | 28.8 | 99 | 31.7 |
| Female | 277 | 29.9 | 110 | 30.9 | 59 | 23.0 | 108 | 34.6 |
| Total | 552 | 59.6 | 212 | 59.6 | 133 | 51.8 | 207 | 66.3 |
| 85th–<95th percentile | ||||||||
| Male | 68 | 7.4 | 22 | 6.2 | 31 | 12.1 | 15 | 4.8 |
| Female | 82 | 8.9 | 27 | 7.6 | 23 | 8.9 | 32 | 10.3 |
| Total | 150 | 16.2 | 49 | 13.8 | 54 | 21.0 | 47 | 15.1 |
| ≥95th percentile | ||||||||
| Male | 105 | 11.4 | 48 | 13.5 | 35 | 13.6 | 22 | 7.1 |
| Female | 91 | 9.8 | 28 | 7.9 | 30 | 11.7 | 33 | 10.6 |
| Total | 196 | 21.2 | 76 | 21.4 | 65 | 25.3 | 55 | 17.7 |
| Child | Parent | Effect Size | |||||
|---|---|---|---|---|---|---|---|
| Mean | SD | Variance | Mean | SD | Variance | Cohen’s d | |
| Vegetables | 19.5 | 40.5 | 1636.6 | 48.4 | 30.6 | 938.3 | 0.8 * |
| Fruits | 56.9 | 33.1 | 1098.0 | 60.5 | 27.4 | 749.7 | 0.1 |
| Protein | 40.9 | 35.3 | 1242.7 | 37.9 | 27.9 | 778.6 | 0.1 |
| Sweet drinks | 55.0 | 33.3 | 1108.7 | 14.1 | 39.6 | 1565.5 | 1.1 * |
| Screen time | 64.3 | 26.5 | 701.6 | 39.9 | 27.7 | 768.0 | 0.9 * |
| Sweets | 64.4 | 31.2 | 974.2 | 31.0 | 36.3 | 1317.7 | 1.0 * |
| Fiber | 23.6 | 38.4 | 1476.7 | 41.6 | 30.6 | 936.4 | 0.5 |
| Salty | 44.1 | 32.1 | 1028.4 | 28.3 | 30.6 | 933.4 | 0.5 |
| PA | 59.5 | 29.8 | 888.1 | 49.3 | 30.7 | 940.4 | 0.3 |
| Dairy | 45.6 | 36.7 | 1346.3 | 35.5 | 34.6 | 1198.1 | 0.3 |
| Child | Parent | |||||||
|---|---|---|---|---|---|---|---|---|
| Characteristic * | Mean HBI | n | SD | p-Value | Mean HBI | n | SD | p-Value |
| Gender | ||||||||
| Male | −53.8 | 449 | 40.1 | 0.002 ** | 13.0 | 449 | 44.8 | 0.280 |
| Female | −45.3 | 439 | 43.0 | 16.2 | 439 | 43.9 | ||
| Race/Ethnicity | ||||||||
| White | −41.1 | 341 | 42.3 | 0.000 ** | 23.0 | 341 | 43.1 | <0.001 ** |
| Af. Amer./Black | −55.2 | 129 | 39.3 | 0.006 † | 10.1 | 129 | 43.3 | 0.023 † |
| Hispanic/Latino | −55.5 | 330 | 40.7 | 0.000 † | 8.7 | 330 | 44.2 | <0.001 † |
| Insurance Type | ||||||||
| Private | −44.0 | 364 | 40.4 | 0.001 ** | 23.7 | 364 | 41.3 | <0.001 ** |
| Public | −53.7 | 490 | 41.9 | 7.3 | 490 | 45.0 | ||
| Income Level | ||||||||
| $21,433–41,186 | −58.9 | 277 | 40.9 | 0.000 ** | 4.8 | 277 | 45.2 | <0.001 * |
| $41,187–68,212 | −47.4 | 234 | 41.5 | 0.015 a | 14.7 | 234 | 41.3 | 0.075 |
| $68,213–112,262 | −41.8 | 301 | 41.0 | 0.000 a | 24.4 | 301 | 42.3 | <0.001 a |
| Food Insecurity | ||||||||
| Greatest risk | −54.2 | 552 | 40.9 | 0.000 ** | 7.8 | 552 | 43.5 | <0.001 ** |
| >than avg. risk | −46.1 | 99 | 42.1 | 0.272 | 19.7 | 99 | 46.4 | 0.058 |
| <than avg. risk | −40.7 | 125 | 39.0 | 0.005 b | 27.9 | 125 | 39.9 | <0.001 b |
| Lowest risk | −36.8 | 97 | 44.6 | 0.001 b | 27.3 | 97 | 42.3 | <0.001 b |
| BMI Percentile | ||||||||
| Normal weight | −49.6 | 523 | 40.7 | 14.8 | 523 | 44.3 | ||
| Overweight | −46.6 | 149 | 42.4 | 0.716 ^ | 12.0 | 149 | 40.7 | 0.767 ^ |
| Obese | −49.0 | 189 | 42.7 | 0.984 ^ | 15.1 | 189 | 44.5 | 0.996 ^ |
| Overall | −49.4 | 908 | 42.1 | --- | 14.5 | 904 | 43.9 | --- |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vosburgh, K.; Smith, S.R.; Oldman, S.; Huedo-Medina, T.; Duffy, V.B. Pediatric-Adapted Liking Survey (PALS): A Diet and Activity Screener in Pediatric Care. Nutrients 2019, 11, 1641. https://doi.org/10.3390/nu11071641
Vosburgh K, Smith SR, Oldman S, Huedo-Medina T, Duffy VB. Pediatric-Adapted Liking Survey (PALS): A Diet and Activity Screener in Pediatric Care. Nutrients. 2019; 11(7):1641. https://doi.org/10.3390/nu11071641
Chicago/Turabian StyleVosburgh, Kayla, Sharon R. Smith, Samantha Oldman, Tania Huedo-Medina, and Valerie B. Duffy. 2019. "Pediatric-Adapted Liking Survey (PALS): A Diet and Activity Screener in Pediatric Care" Nutrients 11, no. 7: 1641. https://doi.org/10.3390/nu11071641
APA StyleVosburgh, K., Smith, S. R., Oldman, S., Huedo-Medina, T., & Duffy, V. B. (2019). Pediatric-Adapted Liking Survey (PALS): A Diet and Activity Screener in Pediatric Care. Nutrients, 11(7), 1641. https://doi.org/10.3390/nu11071641






