Cardiac Changes in Patients on Long-Term Parenteral Nutrition
Abstract
1. Introduction
2. Methods
2.1. Study Population
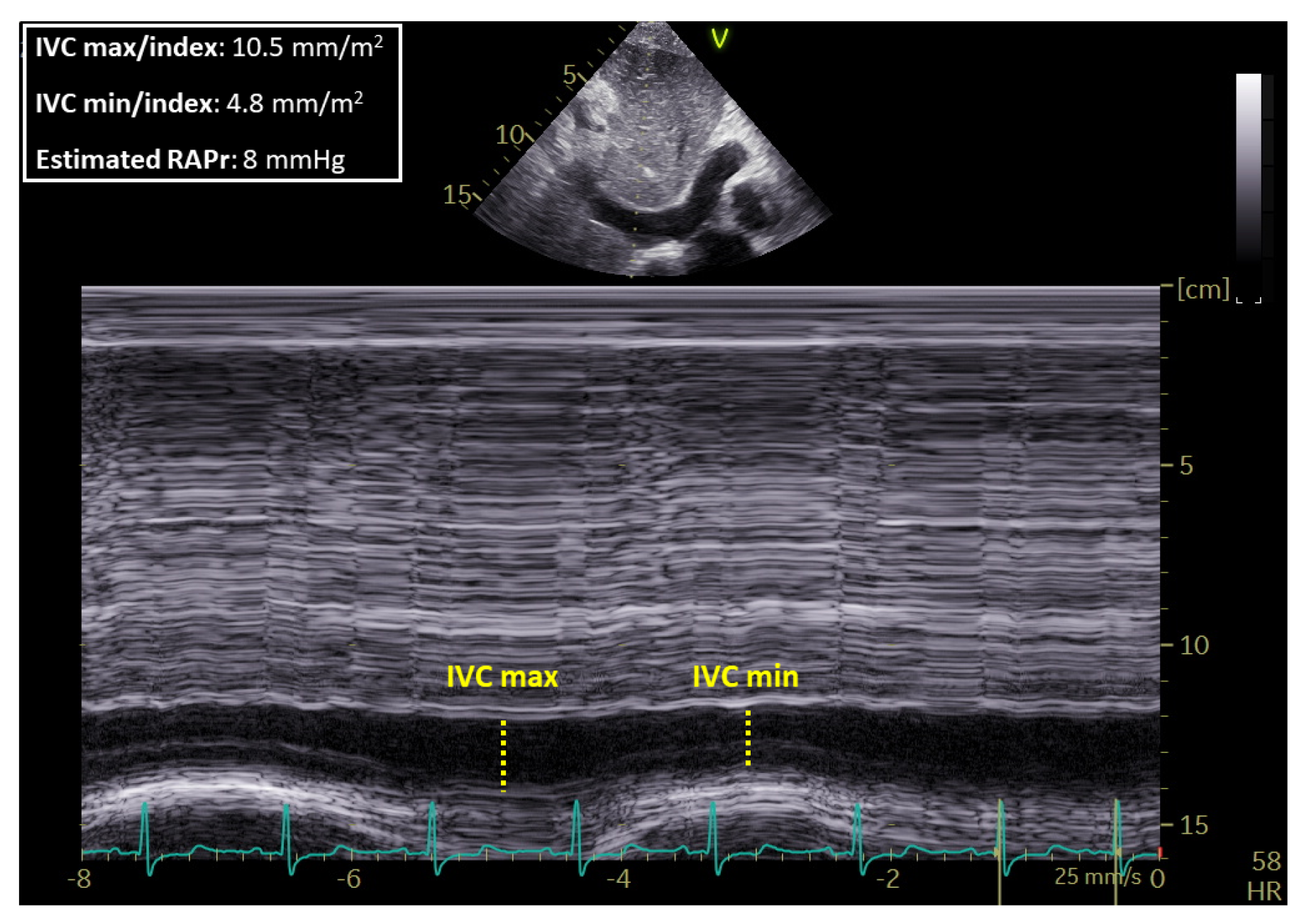
2.2. TTE
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Goor, D.A.; Lillehei, C.W. Congenital malformations of the heart. In Congenital Malformations of the Heart: Embryology, Anatomy, and Operative Considerations, 1st ed.; Grune & Stratton: New York, NY, USA, 1975; pp. 1–37. [Google Scholar]
- Ho, S.Y.; Nihoyannopoulos, P. Anatomy, echocardiography, and normal right ventricular dimensions. Heart 2006, 92 (Suppl. S1), i2–i13. [Google Scholar] [CrossRef] [PubMed]
- Voelkel, N.F.; Quaife, R.A.; Leinwand, L.A.; Barst, R.J.; McGoon, M.D.; Meldrum, D.R.; Dupuis, J.; Long, C.S.; Rubin, L.J.; Smart, F.W.; et al. Right ventricular function and failure: Report of a National Heart, Lung, and Blood Institute Working Group on Cellular and Molecular Mechanisms of Right Heart Failure. Circulation 2006, 114, 1883–1891. [Google Scholar] [CrossRef] [PubMed]
- Lorenz, C.H.; Walker, E.S.; Morgan, V.L.; Klein, S.S.; Graham, T.P., Jr. Normal human right and left ventricular mass, systolic function, and gender differences by cine magnetic resonance imaging. J. Cardiovasc. Magn. Reson. 1999, 1, 7–21. [Google Scholar] [CrossRef] [PubMed]
- Chin, K.M.; Kim, N.H.; Rubin, L.J. The right ventricle in pulmonary hypertension. Coron. Artery Dis. 2005, 16, 13–18. [Google Scholar] [CrossRef]
- Matarese, L.E. Nutritional and fluid optimization for patients with Short Bowel Syndrome. JPEN J. Parenter. Enter. Nutr. 2013, 37, 161–170. [Google Scholar] [CrossRef]
- Lembo, M.; Esposito, R.; Santoro, C.; Lo Iudice, F.; Schiano-Lomoriello, V.; Fazio, V.; Grimaldi, M.G.; Trimarco, B.; de Simone, G.; Galderisi, M. Three-dimensional echocardiographic ventricular mass/end-diastolic volume ratio in native hypertensive patients: Relation between stroke volume and geometry. J. Hypertens. 2018, 36, 1697–1704. [Google Scholar] [CrossRef]
- Buonauro, A.; Galderisi, M.; Santoro, C.; Canora, A.; Bocchino, M.L.; Lo Iudice, F.; Lembo, M.; Esposito, R.; Castaldo, S.; Trimarco, B.; et al. Obstructive sleep apnoea and right ventricular function: A combined assessment by speckle tracking and three-dimensional echocardiography. Int. J. Cardiol. 2017, 243, 544–549. [Google Scholar] [CrossRef]
- Galiè, N.; Humbert, M.; Vachiery, J.L.; Gibbs, S.; Lang, I.; Torbicki, A.; Simonneau, G.; Peacock, A.; VonkNoordegraaf, A.; Beghetti, M.; et al. ESC Scientific Document Group. 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: The Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur. Heart J. 2016, 37, 67–119. [Google Scholar] [PubMed]
- Santarpia, L.; Pagano, M.C.; Pasanisi, F.; Contaldo, F. Home artificial nutrition: An update seven years after the regional regulation. Clin. Nutr. 2014, 33, 872–878. [Google Scholar] [CrossRef] [PubMed]
- Violante, G.; Alfonsi, L.; Santarpia, L.; Cillis, M.C.; Negro, G.; De Caprio, C.; Russo, N.; Contaldo, F.; Pasanisi, F. Adult home parenteral nutrition: A clinical evaluation after a 3-year experience in a Southern European centre. Eur. J. Clin. Nutr. 2006, 60, 58–61. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Pironi, L.; Arends, J.; Bozzetti, F.; Cuerda, C.; Gillanders, L.; Jeppesen, P.B.; Joly, F.; Kelly, D.; Lal, S.; Staun, M.; et al. ESPEN guidelines on chronic intestinal failure in adults. Clin. Nutr. 2016, 35, 247–307. [Google Scholar] [CrossRef] [PubMed]
- Bielawska, B.; Allard, J.P. Parenteral Nutrition and Intestinal Failure. Nutrients 2017, 9, 466. [Google Scholar] [CrossRef] [PubMed]
- Wanten, G.; Calder, P.C.; Forbes, A. Managing adult patients who need home parenteral nutrition. BMJ 2011, 342, 1447. [Google Scholar] [CrossRef] [PubMed]
- O’Keefe, S.J.; Peterson, M.E.; Fleming, C.R. Octreotide as an adjunct to home parenteral nutrition in the management of permanent end-jejunostomy syndrome. JPEN J. Parenter. Enter. Nutr. 1994, 18, 26–34. [Google Scholar]
- Tappenden, K.A. Intestinal adaptation following resection. JPEN J. Parenter. Enter. Nutr. 2014, 38, 23–31. [Google Scholar] [CrossRef] [PubMed]
- Reque, J.; Quiroga, B.; Ruiz, C.; Villaverde, M.T.; Vega, A.; Abad, S.; Panizo, N.; López-Gómez, J.M. Pulmonary hypertension is an independent predictor of cardiovascular events and mortality in haemodialysis patients. Nephrology 2016, 21, 321–326. [Google Scholar] [CrossRef] [PubMed]
- Dini, F.L.; Galderisi, M.; Mondillo, S.; De Tommasi, S.M. The right ventricle: Role of Doppler echocardiography in the clinical practice. Ital. Heart J. Suppl. 2004, 5, 757. [Google Scholar] [PubMed]
- Whitlock, M.; Garg, A.; Gelow, J.; Jacobson, T.; Broberg, C. Comparison of left and right atrial volume by echocardiography versus cardiac magnetic resonance imaging using the area-length method. Am. J. Cardiol. 2010, 106, 1345–1350. [Google Scholar] [CrossRef] [PubMed]
- Lai, W.W.; Gauvreau, K.; Rivera, E.S.; Saleeb, S.; Powell, A.J.; Geva, T. Accuracy of guideline recommendations for two-dimensional quantification of the right ventricle by echocardiography. Int. J. Cardiovasc. Imaging 2008, 24, 691–698. [Google Scholar] [CrossRef] [PubMed]
| Variable | HPN Patients (n = 26) | Controls (n = 26) | p-Value |
|---|---|---|---|
| Sex (M/F) | 11/15 | 11/15 | |
| Age (years) | 49.65 ± 18.81 | 50.44 ± 17.24 | 0.81 |
| Body Weight (kg) | 53.05 ± 12.70 | 62.50 ± 12.47 | 0.01 |
| Height (cm) | 163.57 ± 8.70 | 165.34 ± 9.16 | 0.99 |
| BMI (kg/m2) | 19.71 ± 3.86 | 22.83 ± 4.03 | 0.01 |
| BSA (m2) | 1.57 ± 0.23 | 1.68 ± 0.18 | 0.05 |
| SBP (mmHg) | 117.88 ± 30.38 | 125.63 ± 14.01 | 0.34 |
| DBP (mmHg) | 68.06 ± 12.76 | 77.08 ± 9.65 | 0.02 |
| HR (bpm) | 80.46 ± 19.35 | 80.73 ± 14.90 | 0.87 |
| HPN duration (months) | 70 (19–96) | ||
| Iv volumes (mL) | 1621 ± 501 | ||
| Iv volumes/Body Weight (mL/kg) | 29.34 ± 12.35 |
| Variable | HPN Patients (n = 26) | Controls (n = 26) | p-Value |
|---|---|---|---|
| TRGrad. (mmHg) | 25.44 ± 9.86 | 22.62 ± 5.72 | 0.71 |
| sPAP (mmHg) | 32.70 ± 11.51 | 28.97 ± 6.60 | 0.51 |
| IVCmax_Index (mm/m2) | 10.3 ± 2.84 | 7.80 ± 2.25 | 0.006 |
| IVCmin_Index (mm/m2) | 4.46 ± 3.81 | 2.38 ± 2.61 | 0.04 |
| CI_ivc (%) | 58.18 ± 33.87 | 70.41 ± 29.46 | 0.27 |
| RAPr (mmHg) | 7.39 ± 2.96 | 5.57 ± 1.62 | 0.01 |
| RA volume (mL) | 28.29 ± 13.85 | 28.90 ± 10.89 | 0.99 |
| RAvol_Index (mL/m2) | 17.53 ± 6.22 | 17.00 ± 5.63 | 0.98 |
| RAdiam. (mm) | 3.28 ± 0.58 | 3.19 ± 0.62 | 0.84 |
| RAdiam Index (mm/m2) | 2.11 ± 0.38 | 1.93 ± 0.36 | 0.15 |
| RVDbasal diam (mm) | 32.99 ± 5.83 | 33.76 ± 5.26 | 0.94 |
| RVDbasal diam Index (mm/m2) | 21.13± 3.20 | 20.06 ± 2.77 | 0.62 |
| RVDmean (mm) | 29.42 ± 5.62 | 29.58 ± 6.59 | 1.00 |
| RVDmean Index (mm/m2) | 18.84 ± 3.13 | 17.47 ± 2.92 | 0.46 |
| RVDlong (mm) | 56.96 ± 6.58 | 63.62 ± 8.22 | 0.002 |
| RVDlong Index (mm/m2) | 36.58 ± 4.00 | 37.78 ± 3.80 | 0.78 |
| TAPSE (mm) | 21.46 ± 3.90 | 22.73 ± 3.46 | 0.42 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Santarpia, L.; Esposito, R.; Vaccaro, A.; Alfonsi, L.; Pagano, M.C.; Santoro, C.; Marra, M.; Contaldo, F.; Galderisi, M.; Pasanisi, F. Cardiac Changes in Patients on Long-Term Parenteral Nutrition. Nutrients 2019, 11, 1587. https://doi.org/10.3390/nu11071587
Santarpia L, Esposito R, Vaccaro A, Alfonsi L, Pagano MC, Santoro C, Marra M, Contaldo F, Galderisi M, Pasanisi F. Cardiac Changes in Patients on Long-Term Parenteral Nutrition. Nutrients. 2019; 11(7):1587. https://doi.org/10.3390/nu11071587
Chicago/Turabian StyleSantarpia, Lidia, Roberta Esposito, Andrea Vaccaro, Lucia Alfonsi, Maria Carmen Pagano, Ciro Santoro, Maurizio Marra, Franco Contaldo, Maurizio Galderisi, and Fabrizio Pasanisi. 2019. "Cardiac Changes in Patients on Long-Term Parenteral Nutrition" Nutrients 11, no. 7: 1587. https://doi.org/10.3390/nu11071587
APA StyleSantarpia, L., Esposito, R., Vaccaro, A., Alfonsi, L., Pagano, M. C., Santoro, C., Marra, M., Contaldo, F., Galderisi, M., & Pasanisi, F. (2019). Cardiac Changes in Patients on Long-Term Parenteral Nutrition. Nutrients, 11(7), 1587. https://doi.org/10.3390/nu11071587






