Different and Unequal: A Qualitative Evaluation of Salient Factors Influencing Energy Intake in Adults with Overweight and Obesity
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
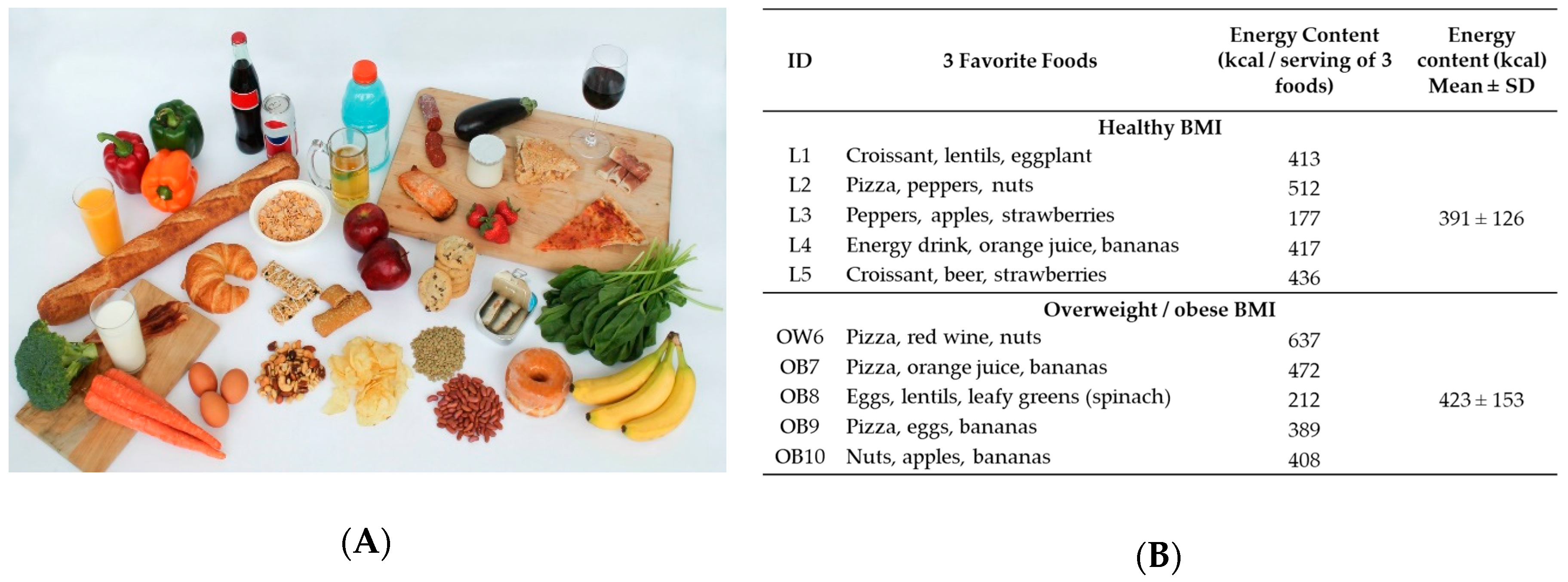
2.2. Key Informant Interviews and Focus Groups
2.3. Data Transcription and Analysis
3. Results
3.1. Population Characteristics
3.2. Food Preference: Link Between Pleasure and Healthfulness
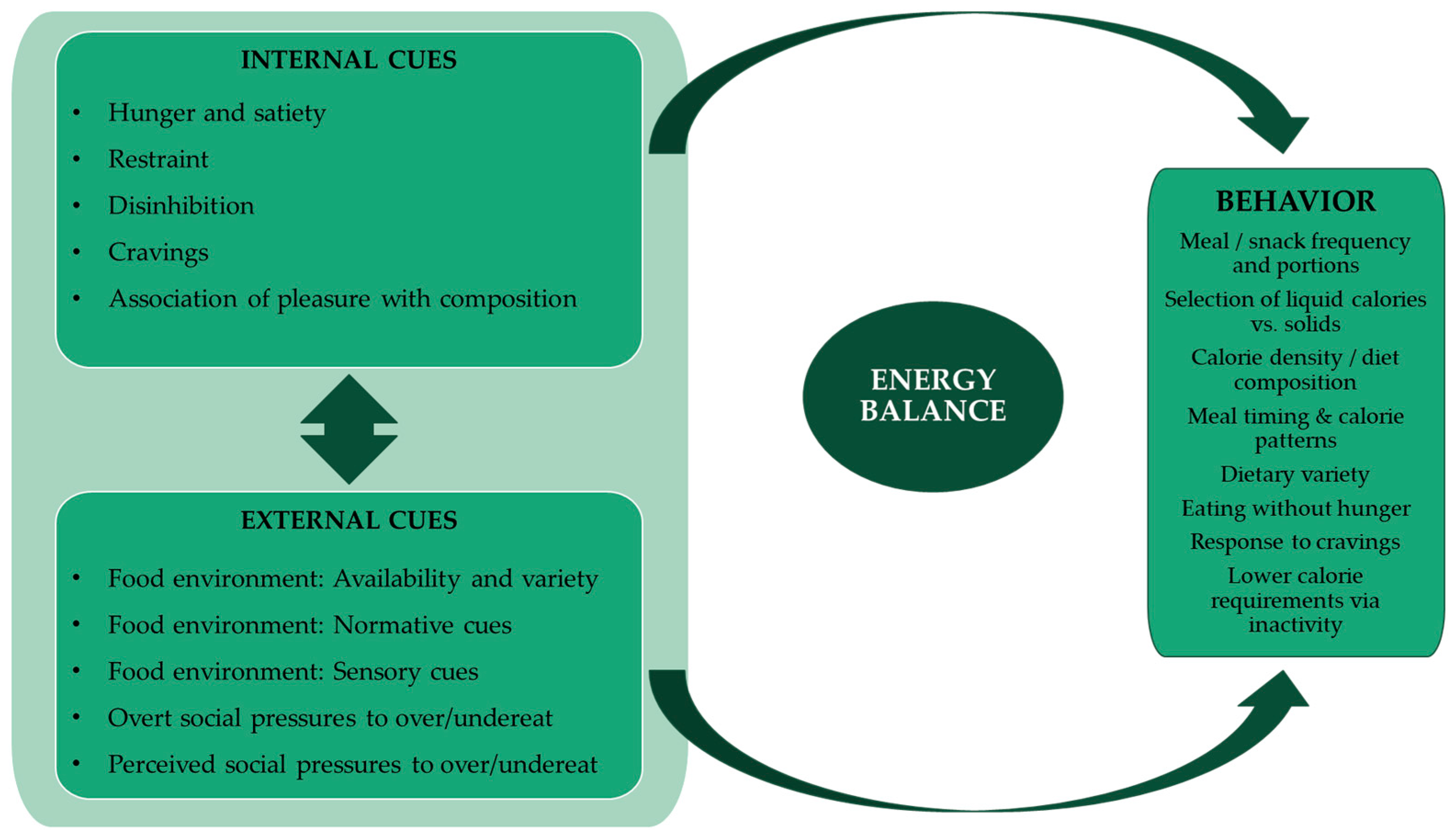
3.3. Internal Cues and Eating Behavior Responses
3.4. External Factors in Overeating
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Lean, M.E.J.; Astrup, A.; Roberts, S.B. Making progress on the global crisis of obesity and weight management. BMJ 2018, 361, k2538. [Google Scholar] [CrossRef] [PubMed]
- Emilien, C.; Hollis, J.H. A brief review of salient factors influencing adult eating behaviour. Nutr. Res. Rev. 2017, 30, 233–246. [Google Scholar] [CrossRef] [PubMed]
- Belfort-DeAguiar, R.; Seo, D. Food Cues and Obesity: Overpowering Hormones and Energy Balance Regulation. Curr. Obes. Rep. 2018, 7, 122–129. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.M.; Ditschun, T.L. Controlling satiety: How environmental factors influence food intake. Trends Food Sci. Technol. 2009, 20, 271–277. [Google Scholar] [CrossRef]
- Elliston, K.G.; Ferguson, S.G.; Schüz, N.; Schüz, B. Situational cues and momentary food environment predict everyday eating behavior in adults with overweight and obesity. Health Psychol. 2017, 36, 337–345. [Google Scholar] [CrossRef] [PubMed]
- Swinburn, B.; Vandevijvere, S.; Kraak, V.; Sacks, G.; Snowdon, W.; Hawkes, C.; Barquera, S.; Friel, S.; Kelly, B.; Kumanyika, S.; et al. Monitoring and benchmarking government policies and actions to improve the healthiness of food environments: A proposed Government Healthy Food Environment Policy Index. Obes. Rev. 2013, 14 (Suppl. 1), 24–37. [Google Scholar] [CrossRef] [PubMed]
- Cohen, D.A. Obesity and the built environment: Changes in environmental cues cause energy imbalances. Int. J. Obes. 2008, 32, S137–S142. [Google Scholar] [CrossRef] [PubMed]
- Karl, J.P.; Roberts, S.B. Energy Density, Energy Intake, and Body Weight Regulation in Adults. Adv. Nutr. 2014, 5, 835–850. [Google Scholar] [CrossRef]
- McCrory, M.A.; Burke, A.; Roberts, S.B. Dietary (sensory) variety and energy balance. Physiol. Behav. 2012, 107, 576–583. [Google Scholar] [CrossRef] [PubMed]
- Sørensen, L.B.; Møller, P.; Flint, A.; Martens, M.; Raben, A. Effect of sensory perception of foods on appetite and food intake: A review of studies on humans. Int. J. Obes. Relat. Metab. Disord. J. Int. Assoc. Study Obes. 2003, 27, 1152–1166. [Google Scholar] [CrossRef]
- Levitsky, D.A.; Iyer, S.; Pacanowski, C.R. Number of foods available at a meal determines the amount consumed. Eat. Behav. 2012, 13, 183–187. [Google Scholar] [CrossRef] [PubMed]
- Tordoff, M.G. Obesity by choice: The powerful influence of nutrient availability on nutrient intake. Am. J. Physiol.-Regul. Integr. Comp. Physiol. 2002, 282, R1536–R1539. [Google Scholar] [CrossRef] [PubMed]
- Rolls, B.J. What is the role of portion control in weight management? Int. J. Obes. 2014, 38, S1–S8. [Google Scholar] [CrossRef] [PubMed]
- Alpert, P.T. Portion Size: A Disconnect Among Americans? Home Health Care Manag. Pract. 2012, 24, 59–61. [Google Scholar] [CrossRef]
- Ordabayeva, N.; Chandon, P. In the eye of the beholder: Visual biases in package and portion size perceptions. Appetite 2016, 103, 450–457. [Google Scholar] [CrossRef] [PubMed]
- Monteiro, C.A. Nutrition and health. The issue is not food, nor nutrients, so much as processing. Public Health Nutr. 2009, 12, 729–731. [Google Scholar] [CrossRef]
- DiMeglio, D.P.; Mattes, R.D. Liquid versus solid carbohydrate: Effects on food intake and body weight. Int. J. Obes. Relat. Metab. Disord. J. Int. Assoc. Study Obes. 2000, 24, 794–800. [Google Scholar] [CrossRef]
- Herman, C.P.; Polivy, J. A boundary model for the regulation of eating. Res. Publ. Assoc. Res. Nerv. Ment. Dis. 1984, 62, 141–156. [Google Scholar] [CrossRef]
- Schachter, S. Some extraordinary facts about obese humans and rats. Am. Psychol. 1971, 26, 129–144. [Google Scholar] [CrossRef]
- Bailey, J. First steps in qualitative data analysis: Transcribing. Fam. Pract. 2008, 25, 127–131. [Google Scholar] [CrossRef]
- Gan, Y.; Tong, X.; Li, L.; Cao, S.; Yin, X.; Gao, C.; Herath, C.; Li, W.; Jin, Z.; Chen, Y.; et al. Consumption of fruit and vegetable and risk of coronary heart disease: A meta-analysis of prospective cohort studies. Int. J. Cardiol. 2015, 183, 129–137. [Google Scholar] [CrossRef] [PubMed]
- Bertoia, M.L.; Mukamal, K.J.; Cahill, L.E.; Hou, T.; Ludwig, D.S.; Mozaffarian, D.; Willett, W.C.; Hu, F.B.; Rimm, E.B. Changes in Intake of Fruits and Vegetables and Weight Change in United States Men and Women Followed for Up to 24 Years: Analysis from Three Prospective Cohort Studies. PLoS Med. 2015, 12, e1001878. [Google Scholar] [CrossRef] [PubMed]
- Qin, L.-Q.; Xu, J.-Y.; Han, S.-F.; Zhang, Z.-L.; Zhao, Y.-Y.; Szeto, I.M. Dairy consumption and risk of cardiovascular disease: An updated meta-analysis of prospective cohort studies. Asia Pac. J. Clin. Nutr. 2015, 24, 90–100. [Google Scholar] [PubMed]
- Shin, J.Y.; Xun, P.; Nakamura, Y.; He, K. Egg consumption in relation to risk of cardiovascular disease and diabetes: A systematic review and meta-analysis. Am. J. Clin. Nutr. 2013, 98, 146–159. [Google Scholar] [CrossRef] [PubMed]
- Imamura, F.; O’Connor, L.; Ye, Z.; Mursu, J.; Hayashino, Y.; Bhupathiraju, S.N.; Forouhi, N.G. Consumption of sugar sweetened beverages, artificially sweetened beverages, and fruit juice and incidence of type 2 diabetes: Systematic review, meta-analysis, and estimation of population attributable fraction. BMJ 2015, 351, h3576. [Google Scholar] [CrossRef] [PubMed]
- Micha, R.; Wallace, S.K.; Mozaffarian, D. Red and processed meat consumption and risk of incident coronary heart disease, stroke, and diabetes mellitus: A systematic review and meta-analysis. Circulation 2010, 121, 2271–2283. [Google Scholar] [CrossRef] [PubMed]
- Mozaffarian, D. Dietary and Policy Priorities for Cardiovascular Disease, Diabetes, and Obesity: A Comprehensive Review. Circulation 2016, 133, 187–225. [Google Scholar] [CrossRef]
- Afshin, A.; Micha, R.; Khatibzadeh, S.; Mozaffarian, D. Consumption of nuts and legumes and risk of incident ischemic heart disease, stroke, and diabetes: A systematic review and meta-analysis. Am. J. Clin. Nutr. 2014, 100, 278–288. [Google Scholar] [CrossRef]
- Chowdhury, R.; Stevens, S.; Gorman, D.; Pan, A.; Warnakula, S.; Chowdhury, S.; Ward, H.; Johnson, L.; Crowe, F.; Hu, F.B.; et al. Association between fish consumption, long chain omega 3 fatty acids, and risk of cerebrovascular disease: Systematic review and meta-analysis. BMJ 2012, 345, e6698. [Google Scholar] [CrossRef]
- Baliunas, D.O.; Taylor, B.J.; Irving, H.; Roerecke, M.; Patra, J.; Mohapatra, S.; Rehm, J. Alcohol as a risk factor for type 2 diabetes: A systematic review and meta-analysis. Diabetes Care 2009, 32, 2123–2132. [Google Scholar] [CrossRef]
- Saldana, J. The Coding Manual for Qualitative Researchers, 3rd ed.; SAGE Publications Ltd.: Los Angeles, CA, USA; London, UK, 2015; ISBN 978-1-4739-0249-7. [Google Scholar]
- Fade, S.A.; Swift, J.A. Qualitative research in nutrition and dietetics: Data analysis issues. J. Hum. Nutr. Diet. 2011, 24, 106–114. [Google Scholar] [CrossRef] [PubMed]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Using NVIVO in Qualitative Research (Advances in Experimental Medicine and Biology): Lyn Richards: 9780761965251: Amazon.com: Books. Available online: https://www.amazon.com/Qualitative-Research-Advances-Experimental-Medicine/dp/0761965254 (accessed on 1 May 2019).
- Herman, C.P.; Polivy, J. External cues in the control of food intake in humans: The sensory-normative distinction. Physiol. Behav. 2008, 94, 722–728. [Google Scholar] [CrossRef] [PubMed]
- Herman, C.P. The social facilitation of eating. A review. Appetite 2015, 86, 61–73. [Google Scholar] [CrossRef] [PubMed]
- Herman, C.P.; Polivy, J. Normative influences on food intake. Physiol. Behav. 2005, 86, 762–772. [Google Scholar] [CrossRef] [PubMed]
- Herman, C.P.; Olmsted, M.P.; Polivy, J. Obesity, externality, and susceptibility to social influence: An integrated analysis. J. Personal. Soc. Psychol. 1983, 45, 926–934. [Google Scholar] [CrossRef]
- Hays, N.P.; Roberts, S.B. Aspects of eating behaviors “disinhibition” and “restraint” are related to weight gain and BMI in women. Obesity 2008, 16, 52–58. [Google Scholar] [CrossRef]
- Williamson, D.A.; Lawson, O.J.; Brooks, E.R.; Wozniak, P.J.; Ryan, D.H.; Bray, G.A.; Duchmann, E.G. Association of body mass with dietary restraint and disinhibition. Appetite 1995, 25, 31–41. [Google Scholar] [CrossRef]
- Lindroos, A.K.; Lissner, L.; Mathiassen, M.E.; Karlsson, J.; Sullivan, M.; Bengtsson, C.; Sjöström, L. Dietary intake in relation to restrained eating, disinhibition, and hunger in obese and nonobese Swedish women. Obes. Res. 1997, 5, 175–182. [Google Scholar] [CrossRef]
- Rodin, J. Current status of the internal-external hypothesis for obesity: What went wrong? Am. Psychol. 1981, 36, 361–372. [Google Scholar] [CrossRef]
- Christakis, N.A.; Fowler, J.H. The spread of obesity in a large social network over 32 years. N. Engl. J. Med. 2007, 357, 370–379. [Google Scholar] [CrossRef] [PubMed]
- Trumbo, P.; Schlicker, S.; Yates, A.A.; Poos, M. Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids. J. Acad. Nutr. Diet. 2002, 102, 1621–1630. [Google Scholar] [CrossRef]
- Bissell, P.; Peacock, M.; Blackburn, J.; Smith, C. The discordant pleasures of everyday eating: Reflections on the social gradient in obesity under neo-liberalism. Soc. Sci. Med. 2016, 159, 14–21. [Google Scholar] [CrossRef] [PubMed]
- Christiansen, B.; Borge, L.; Fagermoen, M.S. Understanding everyday life of morbidly obese adults-habits and body image. Int. J. Qual. Stud. Health Well-Being 2012, 7, 17255. [Google Scholar] [CrossRef]
- Williams, R.A.; Roe, L.S.; Rolls, B.J. Assessment of satiety depends on the energy density and portion size of the test meal. Obesity 2014, 22, 318–324. [Google Scholar] [CrossRef] [PubMed]
- Rolls, B.J. Dietary energy density: Applying behavioural science to weight management. Nutr. Bull. 2017, 42, 246–253. [Google Scholar] [CrossRef] [PubMed]
- Tey, S.L.; Brown, R.C.; Gray, A.R.; Chisholm, A.W.; Delahunty, C.M. Long-term consumption of high energy-dense snack foods on sensory-specific satiety and intake. Am. J. Clin. Nutr. 2012, 95, 1038–1047. [Google Scholar] [CrossRef]
- Després, J.P.; Lemieux, I.; Prud’homme, D. Treatment of obesity: Need to focus on high risk abdominally obese patients. BMJ 2001, 322, 716–720. [Google Scholar] [CrossRef]
- Ludwig, D.S. The glycemic index: Physiological mechanisms relating to obesity, diabetes, and cardiovascular disease. JAMA 2002, 287, 2414–2423. [Google Scholar] [CrossRef]
- Berthoud, H.-R.; Zheng, H. Modulation of taste responsiveness and food preference by obesity and weight loss. Physiol. Behav. 2012, 107, 527–532. [Google Scholar] [CrossRef]
- Deckersbach, T.; Das, S.K.; Urban, L.E.; Salinardi, T.; Batra, P.; Rodman, A.M.; Arulpragasam, A.R.; Dougherty, D.D.; Roberts, S.B. Pilot randomized trial demonstrating reversal of obesity-related abnormalities in reward system responsivity to food cues with a behavioral intervention. Nutr. Diabetes 2014, 4, e129. [Google Scholar] [CrossRef] [PubMed]
| Group | Age Mean ± SD | Gender N Female (Male) | BMI Mean ± SD |
|---|---|---|---|
| Interviews: Healthy BMI (L, n = 5) | 59 ± 17 | 4 (1) | 21.6 ± 2.5 |
| Interviews: Overweight/Obese BMI (OW/OB, n = 5) | 59 ± 13 | 2 (3) | 32.2 ± 4.0 |
| Focus group 1 Overweight BMI (FG1OW, n = 7) | 61 ± 18 | 5 (2) | 26.0 ± 1.2 |
| Focus group 2 Overweight/Obese BMI (FG2OWOB, n = 3) | 42 ± 7 | 1 (2) | 30.5 ± 2.3 |
| Focus group 3: Overweight/Obese BMI (FG3OWOB, n = 4) | 63 ± 13 | 4 (0) | 29.3 ± 2.8 |
| Factor | Description | Healthy BMI | Overweight/Obese BMI |
|---|---|---|---|
| Hunger and satiety | Awareness and actions when hunger is experienced | L1: “So I don’t ever really get that hungry cause I’m always kind of, like I’ll take food with me. So I try to avoid getting really hungry because then I know I’ll probably, I might overeat.” L2: “I don’t eat ‘til I’m stuffed so if there is too much food I will, you know, cut it down. I don’t like that feeling of like basically you have to undo your pants.” | OB7: “I don’t have much patience and I do feel hungry frequently and that is probably a problem. I even, yeah I sometimes think of hunger as being the root of my inability to lose weight and I occasionally glance at the ads for products that are being developed that allege that they address hunger. If I could safely take something or even eat in a certain way that would just make me less hungry during the course of the day I would jump at it…I see hunger as being kind of at the root of the problem, the inability to lose weight.“ FG1OW: “I try and drink water but it never works.” |
| Restraint | Behaviors to prevent overeating | L1: “I don’t buy them all the time, it is a favorite but I just don’t buy it all the time.” L5 (formerly overweight): “I try to eat healthy, so and I have been for a while but, ya know so I try not even to see these foods that like, that taste good um, cause it’s tempting but, um my taste buds gravitate towards croissants and beer and strawberries.” | OB7: "I try to keep really tempting stuff out of my house and out of my reach.” OB9: "I would’ve circled the donut but I’m trying to lose my belly so I’m refraining from eating donuts.” |
| Disinhibition | Behaviors to enable overeating | L2: “I can indulge a little bit more on the weekends than I do during the week.” L5 (formerly overweight): “I maybe only drink beer maybe once or twice a month. Um, a croissant maybe I’ll have a couple times a month. Um, so just like on a rare occasion. Oh but strawberries I eat that on a regular basis.” | OW6: “At times I certainly eat too much… you make whatever amount … there is and you just eat it. I think that is very common. And maybe I have an idea in my mind what that should be. So it’s maybe more of my brain than in my stomach.” OB10: “I guess I normally those foods are not available to me so I probably see somebody eating um, like some barbeque ribs so I say to me “I try that” or um some potato chips. “Oh I’ll try some of those” or potato salad, you know, I’ll get a scoop of that. But yeah, I guess I’m influenced by what other people eat.” |
| Cravings | Awareness and actions relating to cravings | L2: “The thing that I really enjoy the most and I don’t buy it because I will eat the whole bag are Cheese Curls. That is my indulgence. I love Cheese Curls!… If I buy them I will only buy a small package because as I said I will eat the whole thing.” L3: “I’ve also allowed myself to indulge more in these healthy, you know, sometimes raspberries can be expensive, I’m not buying any ice cream so um….so I permit myself to indulge in the things that I like.” | OB10: “I’ll get up and I’ll feel hungry, well not necessarily hungry but I feel like eating something and most of the time it’s not necessarily hungry.” OB8: “Uhhh. Yea, if it’s something I really enjoy, I don’t have to be hungry to eat it. I would just eat it. Not out of need to eat it … like my cottage cheese… So I might go in the fridgerator and grab the tub of cottage cheese and I might sit down there and eat it.” |
| Association between pleasure and food composition | Tension between food perceived as healthy, and food palatability | L3: “I’d say [health] that’s probably primary, that is, within the range of healthy food, then taste, and um for both of us but that is keeping within the range of healthy food… I rarely cook food that I don’t like.” L5 (formerly overweight): “Yeah definitely, I mean if it doesn’t taste good it’s like, I’m really less likely to eat it. So the taste is very important but sometimes I will choose the healthier thing even though, um something else like I know it would taste better, you know what I mean. So that’s kind of tough, um it’s been tough for me to do that.” | FG1OW: “They’re [selected foods] high sugar, high carbs, all the good stuff.” FG1OW: “Ohhh.You can add that to the unhealthy group. That tastes good.” OW6: “Well there are things I enjoy like pizza I am not eating because I don’t think it is as healthy as I would like it to be.“ |
| External Cues | Description | Healthy BMI | Overweight/Obese BMI | |
|---|---|---|---|---|
| Food environment: Availability and variety | Modifying eating behavior according to available amounts and variety of food | L2: “I mean even when I go out to eat I, you know, try to stay away from like the starchy foods. I try to, you know, have instead of a potato I usually have a double serving of vegetables.” L5 (formerly overweight): “And there’s so many choices so that’s also something that you have to deal with.” | OW6: “I’ll eat it now if it’s available. You know, if I walked through some reception party, yes, always.” FG1OW: At celebrations–“And everybody makes something different. Something that we usually don’t have.” | |
| Food environment: Normative cues | Response to environmental indicators of eating (e.g., portion size, dietary guidelines) | L5 (formerly overweight): “I won’t want a portion that’s too big, it’s like if you’re at a restaurant they give you so much, it’s like I really don’t need that much, maybe I could like bring leftovers, I’ll bring some of it home or whatever. So it‘s portion definitely.” L3: “I’m pretty aware of what stuff you ought to eat and what stuff you ought to avoid and I try to make our meals healthy.“ | OB10: “Um eating well, eating healthy and also um, um, portion size is a big thing to me and I struggle with it…Well if they say this is a single serving and I believe it, I’m like “that can’t be a single serving” so I tend to eat more than recommendations, you know, so having said this is a single serving, I’ll probably eat three times that amount… Right, it’s too little. And so I struggle with portion sizes. So I tend, that’s why I try to eat things that are health in my mind so I can eat a little bit more because its healthy.“ OB8: “Oh, I think nutrition is important because you have to be careful that you’re not eating too much fat. You have to be careful that you’re not eating foods that are high in salt content, high in sugar content. And you gotta eat a balance of food. A balance of green, leafy vegetables, squash and green peppers. You have to eat that balance of food because that’s where your nutrition’s gonna come from, a balance of food.” | |
| Food environment: Sensory cues | Characteristics of food that modify eating behavior | L5: “How healthy it is or unhealthy, um that’s the top priority.“ L2: “It’s the corn, chicken cutlet, it has cheese in it. It looked good so I bought it.” | OB8: “Cause food’s gotta taste good in order to enjoy it. Has to taste good, has to be appealing. I try to go, if I go to restaurants, I’m going to restaurants that are known for the quality of their food.” FG3OWOB: “I think eating things that I find delicious and just enjoyable. I mean I eat, I love eating. I love food. And just… I get a lot of pleasure. You know, eating well to me can be like having a ginormous salad with all kinds of goodies in it or it can mean having a nice hot slice of pizza. It doesn’t necessarily…not so much defined by how nutritious it is, but is it something that makes me feel happy. And sometimes I feel like a salad makes me happy. Sometimes I feel like a donut makes me happy, or what have you. But that it’s satisfying and, you know, kind of like you finish it and you’re like “okay, that was worth it”.” | |
| Overt social pressures to overeat or undereat | Comments and behaviors of family, friends and others that influence overeating or undereating | Overeat | L2: When eating out–“And they watch what I eat too and they’re like “Oh, so you’re not having potatoes, you’re just having vegetables”.” L3: “But at a celebration I feel like I ought to have a drink, again I will go ask for seltzer with lime because everybody assumes you’re drinking a gin and tonic.” | OB9: “It depends on the situation. Like if I’m somewhere and I know I’m gonna be insulting them if I don’t eat it. I’d swallow without chewing. That’s about it and I’d never try again. Like I tried salad before and never again. Like little things like that. Roast beef at a friend’s house and I didn’t want to be insulting and say “oh I don’t eat that.” So I just swallowed it and didn’t even chew it.“ FG2OWOB: “It’s Southern culture, you can’t go somewhere and not eat.” |
| Undereat | L3: “My doctor told me “don’t eat things with added sugar”.” L5: “A lot of it was comments, so it’s just like crazy because I would never say those things to people. You know sometimes there’s reasons that they’re struggling with their weight or whatever it is and it’s not just like so black and white. Like, oh you’re being lazy. There’s other reasons that could be happening. And so yeah there was comments but there was also like ya know implications, ya know people implying things. Um yeah people can just be a little too blunt, sometimes.” | OB9: “Well both her mother and my father’s mother were obese. She I think is terrified that I’m going to be obese and so ever since I was eleven years old she’s hounded me about weight and, you know, are you sure you’re going to eat all of that? And I could go on. …I see them maybe twice a year because of distance, and I enjoy being with them but I always worry, you know, I’m afraid of like … is she watching everything I eat? And silently judging me or later going to tell me…yeah.” | ||
| Perceived social pressures to overeat or undereat | Feelings about being judged by others that influence overeating or undereating | Overeat | L1: “But I actually don’t like talking and eating. I mean I do it, you do it in certain settings. But I feel like you’re not paying attention to what you’re eating when you do that and you’re just more into the conversation, you’re just kind of putting everything in your mouth.” Same participant: “So I actually prefer not to do that. I actually prefer to eat alone, cause then I’m like really focused on the food and how much I’m eating and I can actually taste it and enjoy it.” L5: “Um, but depends on the setting like, if I’m out to eat with my friends and they’re all eating dessert, then I’m more likely to get something like that. Um, I guess it depends on the setting, if it’s in a restaurant or at home. Um, like when I’m on my own I’ll just basically eat mostly healthy.” | OB7: “I just think when one is alone, you know you can sort of dive in be you know, be ravenous not you know perhaps make a tiny bit of a mess. Not be a complete pig but still if one is alone, one doesn’t have to pay attention, if one is in public one has to be a little more delicate in one‘s eating activities. Yeah I think I’m a little better mannered when I’m out in public than I am by myself yeah.” OB9: “Yes, nobody’s there to judge you. Nobody’s there to force you to eat something you don’t want to eat. It’s comfortable eating.” |
| Undereat | “L3: And I really didn’t need to lose weight but you know, you have a coffee break and everybody is just talking about the Atkins diet. You go out to lunch and everybody is talking about the Atkins diet. It’s like, “okay, I think I’m on the Atkins diet”. I lasted one day. One day haha. I thought “this is just bizarre”.” L5 (formerly overweight): “I wasn’t happy with my weight. I wasn’t happy with ya know, people do treat you differently if you know they see something that is a problem, that’s like, oh you need to fix that. And like for me it was my weight and I was just self-conscious and I was just tired of family and friends like making comments, ya know implying things. So it was just like, ok I’m sick of this I need to do this and I need to feel good about myself.” | OB7: “I think one naturally kind of pays attention to sort of how energetic, how ravenous somebody is. So I may try to you know be a little more polite when I’m with others than I might be with myself. And if, I will notice someone who doesn’t enjoy food as much as I do.” OW6: “And the comments actually we made this big joke…because she kept saying “you look fabulous” and I said, you know, there are three stages of life.I read this: youth, middle age, and you look fabulous. But no one is saying like “you’ve lost weight”. I don’t think hardly anyone is saying that but they keep saying “how fabulous!” and its why. That’s what they are talking about. And it’s just kind of funny.” | ||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dao, M.C.; Messer, E.; Conigliaro, T.; Sakaida, K.; Ouellette, A.F.; Himaras, V.; Thiron, S.; Roberts, S.B. Different and Unequal: A Qualitative Evaluation of Salient Factors Influencing Energy Intake in Adults with Overweight and Obesity. Nutrients 2019, 11, 1365. https://doi.org/10.3390/nu11061365
Dao MC, Messer E, Conigliaro T, Sakaida K, Ouellette AF, Himaras V, Thiron S, Roberts SB. Different and Unequal: A Qualitative Evaluation of Salient Factors Influencing Energy Intake in Adults with Overweight and Obesity. Nutrients. 2019; 11(6):1365. https://doi.org/10.3390/nu11061365
Chicago/Turabian StyleDao, Maria Carlota, Ellen Messer, Teresa Conigliaro, Kylie Sakaida, Alexis F. Ouellette, Victoria Himaras, Sophie Thiron, and Susan B. Roberts. 2019. "Different and Unequal: A Qualitative Evaluation of Salient Factors Influencing Energy Intake in Adults with Overweight and Obesity" Nutrients 11, no. 6: 1365. https://doi.org/10.3390/nu11061365
APA StyleDao, M. C., Messer, E., Conigliaro, T., Sakaida, K., Ouellette, A. F., Himaras, V., Thiron, S., & Roberts, S. B. (2019). Different and Unequal: A Qualitative Evaluation of Salient Factors Influencing Energy Intake in Adults with Overweight and Obesity. Nutrients, 11(6), 1365. https://doi.org/10.3390/nu11061365






