Mediterranean Diet Adherence is Associated with Lower Prevalence of Functional Gastrointestinal Disorders in Children and Adolescents
Abstract
1. Introduction
2. Material and Methods
2.1. Study Population and Methods
2.2. Statistical Analysis
3. Results
3.1. Functional Gastrointestinal Disorder Prevalence in the Study Population.
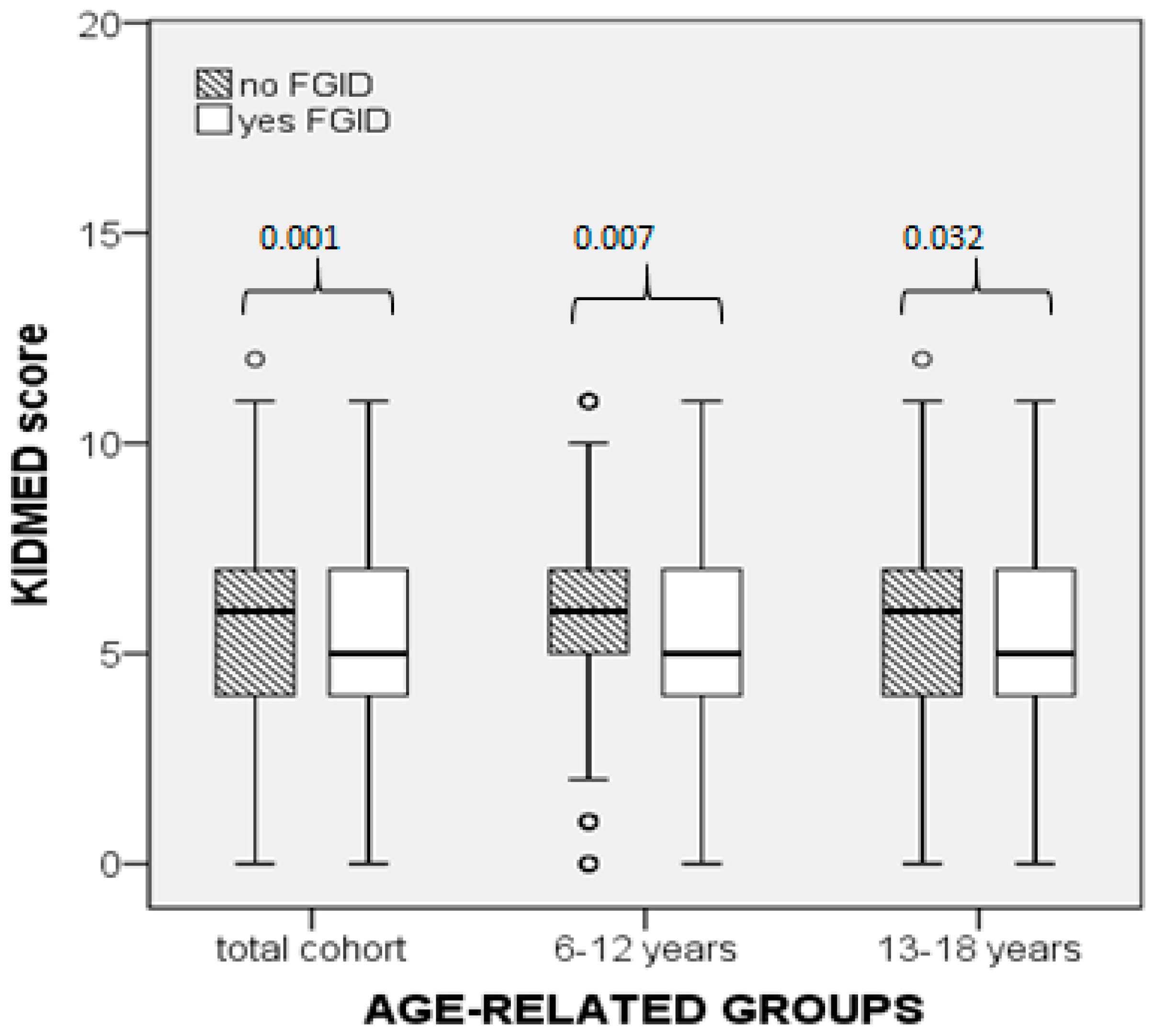
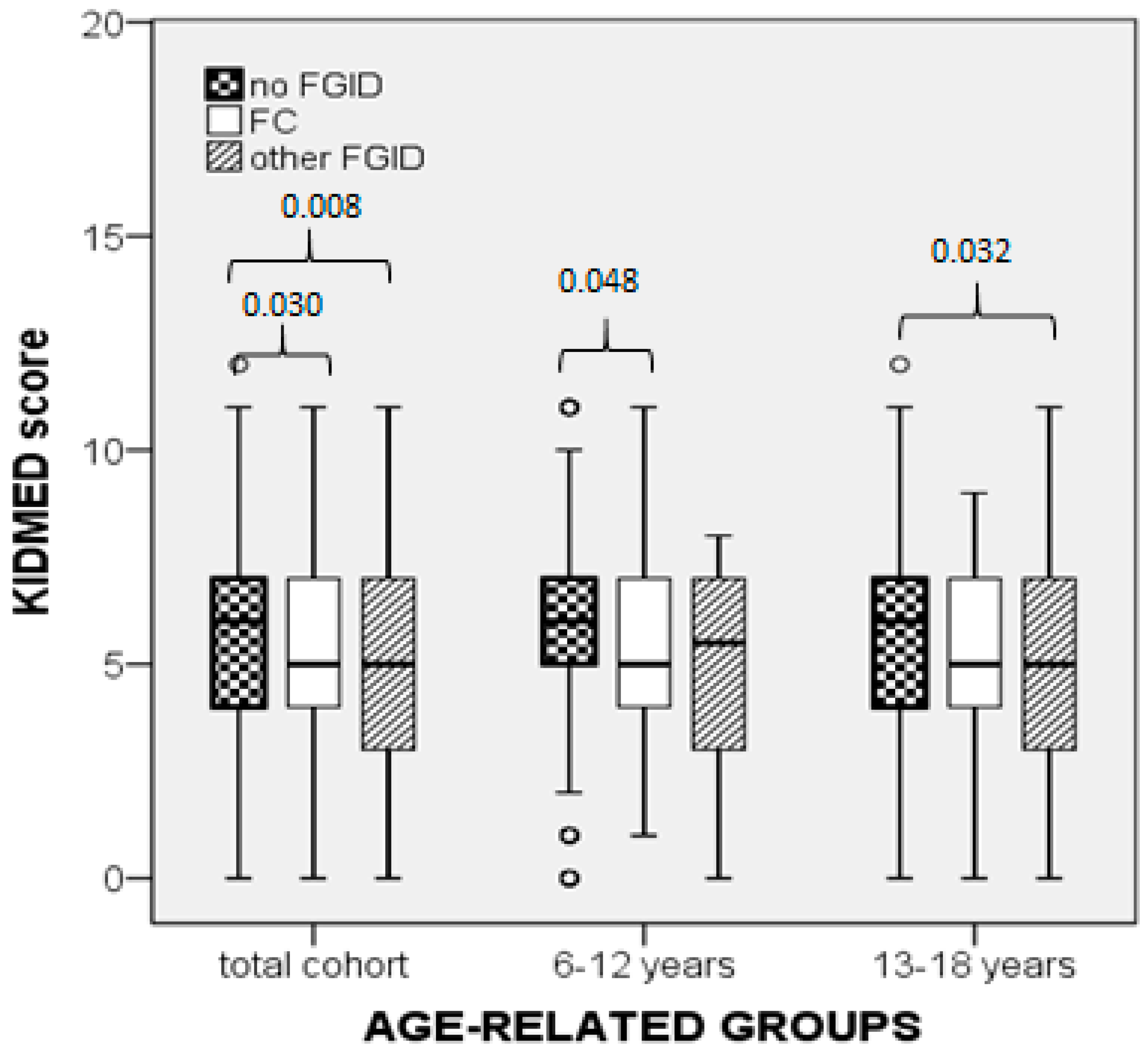
3.2. KIDMED Score Relation with Functional Gastrointestinal Disorder Prevalence
3.3. Mediterranean Diet Adherence Categories and Relation with the Prevalence of Functional Gastrointestinal Disorders
3.4. Multivariable Analysis Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Drossman, D. The functional gastrointestinal disorders and the Rome III Process. Gastroenterology 2006, 130, 1377–1390. [Google Scholar] [CrossRef] [PubMed]
- Scarpato, E.; Kolacek, S.; Jojkic-Pavkov, D.; Konjik, V.; Živković, N.; Roman, E.; Kostovski, A.; Zdraveska, N.; Altamimi, E.; Papadopoulou, A.; et al. Prevalence of Functional Gastrointestinal Disorders in Children and Adolescents in the Mediterranean Region of Europe. Clin. Gastroenterol. Hepatol. 2018, 16, 870–876. [Google Scholar] [CrossRef] [PubMed]
- Hoekman, R.; Rutten, J.M.T.M.; Lieger, A.M.; Benninga, M.A.; Dijkgraaf, M.G.W. Annual costs of care for pediatric Irritable Bowel Syndrome; Functional Abdominal Pain and Functional Abdominal Pain Syndrome. J. Pediatrics 2015, 167, 1103–1108. [Google Scholar] [CrossRef] [PubMed]
- Drossman, D.A.; Hasler, W.L. Rome IV-Functional GI Disorders: Disorders of Gut-Brain Interaction. Gastroenterology 2016, 150, 1257–1261. [Google Scholar] [CrossRef] [PubMed]
- Bonilla, S.; Saps, M. Early life events predispose the onset of childhood functional gastrointestinal disorders. Rev. De Gastro Mex 2013, 78, 82–91. [Google Scholar] [CrossRef] [PubMed]
- Hyams, J.S.; Di Lorenzo, C.; Saps, M.; Shulman, R.J.; Staiano, A.M.; van Tilburg, M. Childhood Functional Gastrointestinal Disorders: Child/Adolescent. Gastroenterology 2016, 150, 1456–1468. [Google Scholar] [CrossRef] [PubMed]
- Rasquin, A.; Di Lorenzo, C.; Forbes, D.; Guiralde, E.; Hyams, S.J.; Staiano, A.; Walker, L.S. Childhood Functional Gastrointestinal Disorders: Child/Adolescent. Gastroenterology 2006, 130, 1527–1537. [Google Scholar] [CrossRef] [PubMed]
- Wilson, K.; Hill, R.J. The role of food intolerance in functional gastrointestinal disorders in children. Aust. Fam. Physician 2014, 43, 686–689. [Google Scholar]
- Chumpitazi, B.P.; Weilder, E.M.; Lu, D.Y.; Tsai, C.M.; Shulman, R.J. Self perceived food intolerances are common and associated with clinical severity in childhood irritable bowel syndrome. J. Acad. Nutr. Diet. 2016, 116, 1458–1464. [Google Scholar] [CrossRef]
- Gibson, P.R.; Varney, J.; Malakar, S.; Muir, J.G. Food and functional bowel disease: Food components and irritable bowel syndrome. Gastroenterology 2015, 148, 1158–1174. [Google Scholar] [CrossRef]
- Metzler-Zebeli, B.U.; Canibe, N.; Montagne, L.; Freire, J.; Bosi, P.; Prates, J.A.M.; Tanghe, S.; Trevisi, P. Resistant starch reduces large intestinal pH and promotes fecal lactobacilli and bifidobacteria in pigs. Animal 2019, 13, 64–73. [Google Scholar] [CrossRef] [PubMed]
- Dahl, W.J.; Stewart, M.L. Position Statement of the Academy of Nutrition and Dietetics: Health implications of dietary fiber. J. Acad. Nutr. Diet. 2015, 115, 1861–1870. [Google Scholar] [CrossRef] [PubMed]
- Stewart, M.L.; Schroeder, N.M. Dietary treatments for childhood constipation: Efficacy of dietary fiber and whole grains. Nutr. Rev. 2013, 71, 98–109. [Google Scholar] [CrossRef] [PubMed]
- Weber, T.K.; Toporovski, M.S.; Tahan, S.; Neufeld, C.B.; de Morais, M.B. Dietary fiber mixture in pediatric patients with controlled chronic constipation. JPGN 2014, 58, 297–302. [Google Scholar] [CrossRef] [PubMed]
- Kokke, F.T.M.; Scholtens, P.A.M.J.; Alles, M.S.; Decates, T.S.; Fiselier, T.J.; Tolboom, J.J.; Kimpen, J.L.; Benninga, M.A. A dietary fiber mixture versus Lactulose in the treatment of childhood constipation: A double-blin randomized controlled trial. JPGN 2008, 47, 592–597. [Google Scholar] [CrossRef] [PubMed]
- Sung, V.; Hiscock, H.; Tang, M.L.K.; Mensah, F.K.; Nation, M.L.; Satzke, C.; Heine, R.G.; Stock, A.; Barr, R.G.; Wake, M. Treating Infant colic with the probiotic Lactobacillus reuteri: Double blind; placebo controlled randomised trial. BMJ 2014, 348, 2107–2118. [Google Scholar] [CrossRef] [PubMed]
- Newlove-Delgado, T.V.; Martin, A.E.; Abbott, R.A.; Bethel, A.; Thompson-Coon, J.; Whear, R.; Logan, S. Dietary interventions for recurrent abdominal pain in childhood. Cochrane Database Syst. Rev. 2017, 3, CD010972. [Google Scholar] [CrossRef] [PubMed]
- Chumpitazi, B.P.; Hollister, E.B.; Oezguen, N.; Tsai, C.M.; McMeans, A.R.; Luna, R.A.; Savidge, T.C.; Versalovic, J.; Shulman, R.J. Gut microbiota influences low fermentable substrate diet efficacy in children with irritable bowel syndrome. Gut Microbes 2014, 5, 165–175. [Google Scholar] [CrossRef] [PubMed]
- Trichopoulou, A.; Lagiou, P. Healthy traditional Mediterranean diet: An expression of culture, history and lifestyle. Nutr. Rev. 1997, 55, 383–389. [Google Scholar] [CrossRef]
- Iaccarino Idelson, P.; Scalfi, L.; Valerio, G. Adherence to the Mediterranean Diet in children and adolesents: A systematic review. Nutr. Metab. Cardiovasc Dis. 2017, 27, 283–299. [Google Scholar] [CrossRef] [PubMed]
- Bouzios, I.; Chouliaras, G.; Chrousos, G.P.; Roma, E.; Gemou-Engesaeth, V. Functional gastrointestinal disorders in Greek Children based on ROME III criteria: Identifying the child at risk. Neurogastroenterol. Motil. 2017, 29, e12951. [Google Scholar] [CrossRef] [PubMed]
- Serra-Majem, L.; Ribas, L.; Ngo, J.; Ortega, R.M.; Garcia, A.; Perez-Rodrigo, C.; Aranceta, J. Food, Youth and the Mediterranean Diet in Spain. Development of KIDMED; Mediterranean Diet Quality Index in children and adolescents. Public Health Nutr. 2004, 7, 931–935. [Google Scholar] [CrossRef] [PubMed]
- Caplan, A.; Walker, L.S.; Rasquin, A. Development and preliminary validation of the Questionnaire on Pediatric Gastrointestinal Symptoms to assess functional gastrointestinal disorders in children and adolescents. JPGN 2005, 41, 296–304. [Google Scholar] [CrossRef] [PubMed]
- Caplan, A.; Walker, L.S.; Rasquin, A. Validation of the Pediatric Rome II Criteria for functional gastrointestinal symptoms using the Questionnaire on Pediatric Gastrointestinal Symptoms. JPGN 2005, 41, 305–316. [Google Scholar] [CrossRef] [PubMed]
- Walker, L.S.; Lipani, T.A.; Greene, J.W.; Caines, K.; Stutts, J.; Polk, D.B.; Caplan, A.; Rasquin-Weber, A. Recurrent abdominal pain: Subtypes based on the Rome II criteria for pediatric functional gastrointestinal disorders. JPGN 2004, 38, 187–191. [Google Scholar] [CrossRef]
- Mariscal-Arcas, M.; Rivas, A.; Velasco, J.; Ortega, M.; Caballero, A.M.; Olea-Serrano, F. Evaluation of the Mediterranean Diet Quality Index (KIDMED) in children and adolescents in Southern Spain. Public Health Nutr. 2008, 12, 1408–1412. [Google Scholar] [CrossRef]
- Štefan, L.; Prosoli, R.; Juranko, D.; Čule, M.; Milinović, I.; Novak, D.; Sporiš, G. The reliability of the Mediterranean Diet Quality Index (KIDMED) Questionnaire. Nutrients 2017, 9, 419. [Google Scholar] [CrossRef]
- Kontogianni, M.D.; Vidra, N.; Farmaki, A.E.; Koinaki, S.; Belogianni, K.; Sofrona, S.; Magkanari, F.; Yannakoulia, M. Adherence rates to the Mediteranean Diet are low in a representative sample of Greek children and adolescents. J. Nutr. 2008, 138, 1951–1956. [Google Scholar] [CrossRef]
- Noale, M.; Nardi, M.; Limongi, F.; Siviero, P.; Caregaro, L.; Crepaldi, G.; Maggi, S.; Mediterranean Diet Foundation Study Group. Adolescents in southern regions of Italy adhere to the Mediterranean diet more than those in the northern regions. Nutr. Res. 2014, 34, 771–779. [Google Scholar] [CrossRef]
- Novak, D.; Stefan, L.; Prosoli, R.; Emeljanovas, A.; Miezene, B.; Milanovic, I.; Radisavljević-Janić, S. Mediterranean Diet and its correlates among adolescents in non-Mediterranean European countries: A population based study. Nutrients 2017, 9, 177. [Google Scholar] [CrossRef]
- García Cabrera, S.; Herrera Fernández, N.; Rodríguez Hernández, C.; Nissensohn, M.; Román-Viñas, B.; Serra-Majem, L. KIDMED test: Prevalence of low adherence to the Mediterranean Diet in children and young; A systematic review. Nutr. Hosp. 2015, 32, 2390–2399. [Google Scholar] [CrossRef] [PubMed]
- Calatayud-Saez, F.M.; Calatayud Moscoso Del Prado, B.; Gallego Fernandez-Pacheco, J.G.; Gonzalez-Martin, C.; Alguacil Merino, L.F. Mediterranean diet and childhood asthma. Allergol. Immunopathol. (Madr) 2016, 44, 99–105. [Google Scholar] [CrossRef] [PubMed]
- Esteban-Cornejo, I.; Izquierdo-Gomez, R.; Gomez-Martinez, S.; Padilla-Moledo, C.; Castro-Pinero, J.; Marcos, A.; Veiga, O.L. Adherence to the Mediterranean diet and academic performance in youth: The UP&DOWN study. Eur. J. Nutr. 2016, 55, 1133–1140. [Google Scholar] [CrossRef] [PubMed]
- Calatayud, F.M.; Calatayud, B.; Gallego, J.G.; Gonzalez-Martin, C.; Alguacil, L.F. Effects of Mediterranean diet in patients with recurring colds and frequent complications. Allergol. Immunopathol. (Madr) 2017, 45, 417–424. [Google Scholar] [CrossRef]
- Reddavide, R.; Rotolo, O.; Caruso, M.; Stasi, E.; Notarnicola, M.; Miraglia, C.; Antonio, N.; Tiziana, M.; Gian, L.D.A.; Francesco, D.M.; et al. The role of diet in the prevention and treatment of Inflammatory Bowel Diseases. Acta Biomed. 2018, 89 (Suppl. 9), 60–75. [Google Scholar] [CrossRef]
- Elmaliklis, I.N.; Liveri, A.; Ntelis, B.; Paraskeva, K.; Goulis, I.; Koutelidakis, A.E. Increased Functional Foods’ Consumption and Mediterranean Diet adherence may have a protective effect in the appearance of gastrointestinal diseases: A case-control study. Medicines 2019, 6, 50. [Google Scholar] [CrossRef] [PubMed]
- Zito, F.P.; Polese, B.; Vozzella, L.; Gala, A.; Genovese, D.; Verlezza, V.; Medugno, F.; Santini, A.; Barrea, L.; Cargiolli, M.; et al. Good adherence to Mediterranean diet can prevent gastrointestinal symptoms: A survey from Southern Italy. World J. Gastrointest Pharm. 2016, 7, 564–571. [Google Scholar] [CrossRef] [PubMed]
- Strisciuglio, C.; Giugliano, F.; Martinelli, M.; Cenni, S.; Greco, L.; Staiano, A.; Miele, E. Impact of environmental and familial factors in a cohort of pediatric patients with inflammatory bowel disease. JPGN 2017, 64, 569–574. [Google Scholar] [CrossRef] [PubMed]
- Hu, F.B. Dietary pattern analysis: A new direction in nutritional epidemiology. Curr. Opin. Lipidol. 2002, 13, 3–9. [Google Scholar] [CrossRef]
- De Filippis, F.; Pellegrini, N.; Vannini, L.; Jeffery, I.B.; La Storia, A.; Laghi, L.; Serrazanetti, D.I.; Di Cagno, R.; Ferrocino, I.; Lazzi, C.; et al. High-level adherence to a Mediterranean diet beneficially impacts the gut microbiota and associated metabolome. Gut 2015, 65, 1–10. [Google Scholar] [CrossRef]
- Del Chierico, F.; Vernocchi, P.; Dallapiccola, B.; Putignani, L. Mediterranean diet and health: Food effects on gut microbiota and disease control. Int. J. Mol. Sci. 2014, 15, 11678–11699. [Google Scholar] [CrossRef] [PubMed]
- David, L.A.; Maurice, C.F.; Carmody, R.N.; Gootenberg, D.B.; Button, J.E.; Wolfe, B.E.; Ling, A.V.; Devlin, A.S.; Varma, Y.; Fischbach, M.A.; et al. Diet rapidly and reproducibly alters the human gut microbiome. Nature 2014, 505, 559–563. [Google Scholar] [CrossRef] [PubMed]
- Mitsou, E.K.; Kakali, A.; Antonopoulou, S.; Mountzouris, K.C.; Yannakoulia, M.B.; Panagiotakos, D.B.; Kyriacou, A. Adherence to the Mediterranean diet is associated with the gut microbiota pattern and gastrointestinal characteristics in an adult population. Br. J. Nutr. 2017, 117, 1645–1655. [Google Scholar] [CrossRef] [PubMed]
- Simpson, H.L.; Campbell, B.J. Review article: Dietary fibre-microbiota interactions. Aliment. Pharm. 2015, 42, 158–179. [Google Scholar] [CrossRef] [PubMed]
- Shortt, C.; Hasselwander, O.; Meynier, A.; Nauta, A.; Fernández, E.N.; Putz, P.; Rowland, I.; Swann, J.; Türk, J.; Vermeiren, J.; et al. Systematic review of the effects of the intestinal microbiota on selected nutrients and non-nutrients. Eur. J. Nutr. 2018, 57, 25–49. [Google Scholar] [CrossRef] [PubMed]
- Jin, Q.; Black, A.; Kales, S.N.; Vattem, D.; Ruiz-Canela, M.; Sotos-Prieto, M. Metabolomics and microbiomes as potential tools to evaluate the effects of the Mediterranean diet. Nutrients 2019, 11, 207. [Google Scholar] [CrossRef] [PubMed]
- Ranasinghe, N.; Devanarayana, N.M.; Rajindrajith, S.; Perera, M.S.; Nishanthinie, S.; Warnakulasuriya, T.; de Zoysa, P.T. Functional gastrointestinal diseases and psychological maladjustment, personality traits and quality of life. BMC Gastroenterol. 2018, 18, 33. [Google Scholar] [CrossRef] [PubMed]
- Duncan, L.; Georgiades, K.; Wang, L.; Comeau, J.; Ferro, M.A.; Van Lieshout, R.; Szatmari, P.; Bennett, K.; MacMillan, H.L.; Lipman, E.L.; et al. The 2014 Ontario Child Health Study Emotional Behavioural Scales (OCHS-EBS) Part I: A Checklist for dimensional measurement of selected DSM-5 disorders. Can. J. Psychiatry 2018. [Google Scholar] [CrossRef] [PubMed]
- Georgiades, K.; Duncan, L.; Wang, L.; Comeau, J.; Boyle, M.H.; 2014 Ontario Child Health Study Team. Six-Month Prevalence of Mental Disorders and Service Contacts among Children and Youth in Ontario: Evidence from the 2014 Ontario Child Health Study. Can. J. Psychiatry 2019, 64, 246–255. [Google Scholar] [CrossRef]
| FGID Groups & Subgroups | Cohort | Age-Related Subgroups | ||
|---|---|---|---|---|
| ESC | HSS | p * | ||
| n | 835 | 387 | 448 | |
| Non-FGID | 651 (78.0) | 320 (82.7) | 331 (73.9) | 0.001 |
| FGID | 184 (22.0) | 67 (17.3) | 117 (26.1) | |
| FC | 122 (14.6) | 54 (14.0) | 68 (15.1) | 0.625 |
| Other-FGID | 62 (7.4) | 13 (3.6) | 49 (10.9) | <0.001 |
| MDA | Cohort | Age-Related Subgroups | ||
|---|---|---|---|---|
| ESC | HSS | p (Fisher’s Exact Test) * | ||
| n | 835 | 387 | 448 | |
| Good (n, (%)) | 186 (22.2) | 82 (21.2) | 104 (23.2) | 0.505 |
| Average (n, (%)) | 505 (60.4) | 250 (64.6) | 255 (56.9) | 0.028 |
| Poor (n, (%)) | 144 (17.2) | 55 (14.2) | 89 (19.9) | 0.035 |
| Age Groups & Subgroups | Subjects with FGID (n) | FGID Prevalence in the MDA-Related Categories | |||
|---|---|---|---|---|---|
| Good (n (%)) | Average (n (%)) | Poor (n (%)) | p (Fisher’s Exact Test) | ||
| Total | 184 | 29 (15.8) | 115 (62.8) | 40 (21.7) | 0.025 |
| ESC | 67 | 6 (9.0) | 49 (73.1) | 12 (17.9) | 0.025 |
| HSS | 117 | 23 (19.7) | 66 (56.4) | 28 (23.9) | 0.335 |
| Independent Variables | FGID | FC | ||||
|---|---|---|---|---|---|---|
| B | p | Exp(B) | B | p | Exp(B) | |
| KIDMED score | −0.113 | 0.001 | 0.893 | −0.097 | 0.021 | 0.907 |
| Age subgroups | 0.499 | 0.004 | 1.646 | 0.234 | 0.247 | 1.264 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Agakidis, C.; Kotzakioulafi, E.; Petridis, D.; Apostolidou, K.; Karagiozoglou-Lampoudi, T. Mediterranean Diet Adherence is Associated with Lower Prevalence of Functional Gastrointestinal Disorders in Children and Adolescents. Nutrients 2019, 11, 1283. https://doi.org/10.3390/nu11061283
Agakidis C, Kotzakioulafi E, Petridis D, Apostolidou K, Karagiozoglou-Lampoudi T. Mediterranean Diet Adherence is Associated with Lower Prevalence of Functional Gastrointestinal Disorders in Children and Adolescents. Nutrients. 2019; 11(6):1283. https://doi.org/10.3390/nu11061283
Chicago/Turabian StyleAgakidis, Charalampos, Evangelia Kotzakioulafi, Dimitrios Petridis, Konstantina Apostolidou, and Thomai Karagiozoglou-Lampoudi. 2019. "Mediterranean Diet Adherence is Associated with Lower Prevalence of Functional Gastrointestinal Disorders in Children and Adolescents" Nutrients 11, no. 6: 1283. https://doi.org/10.3390/nu11061283
APA StyleAgakidis, C., Kotzakioulafi, E., Petridis, D., Apostolidou, K., & Karagiozoglou-Lampoudi, T. (2019). Mediterranean Diet Adherence is Associated with Lower Prevalence of Functional Gastrointestinal Disorders in Children and Adolescents. Nutrients, 11(6), 1283. https://doi.org/10.3390/nu11061283






