Energy Metabolism and Intermittent Fasting: The Ramadan Perspective
Abstract
1. Introduction
2. Energy Expenditure (EE)
2.1. Short-Term Fasting
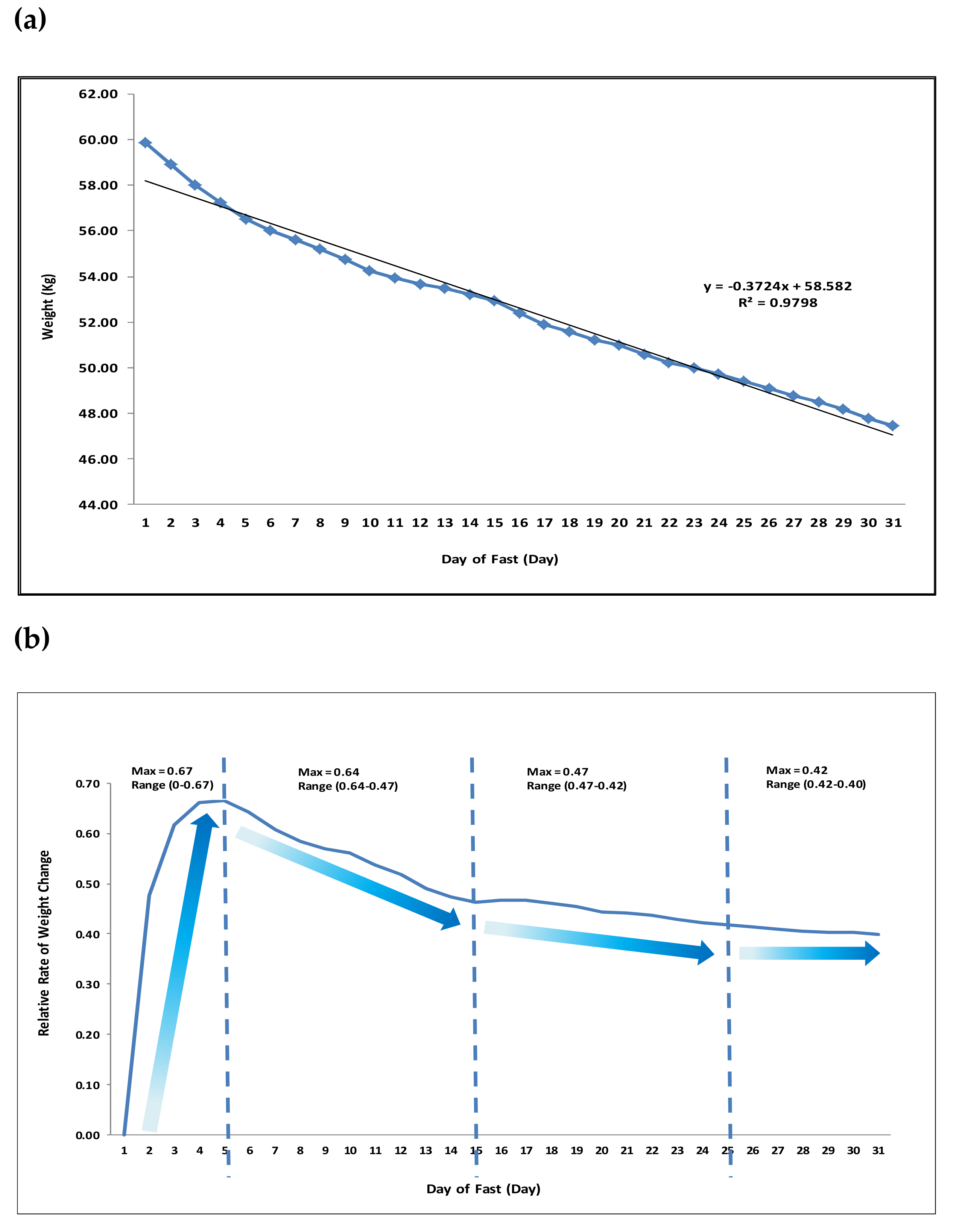
2.2. Prolonged Fasting-Some Historic Examples
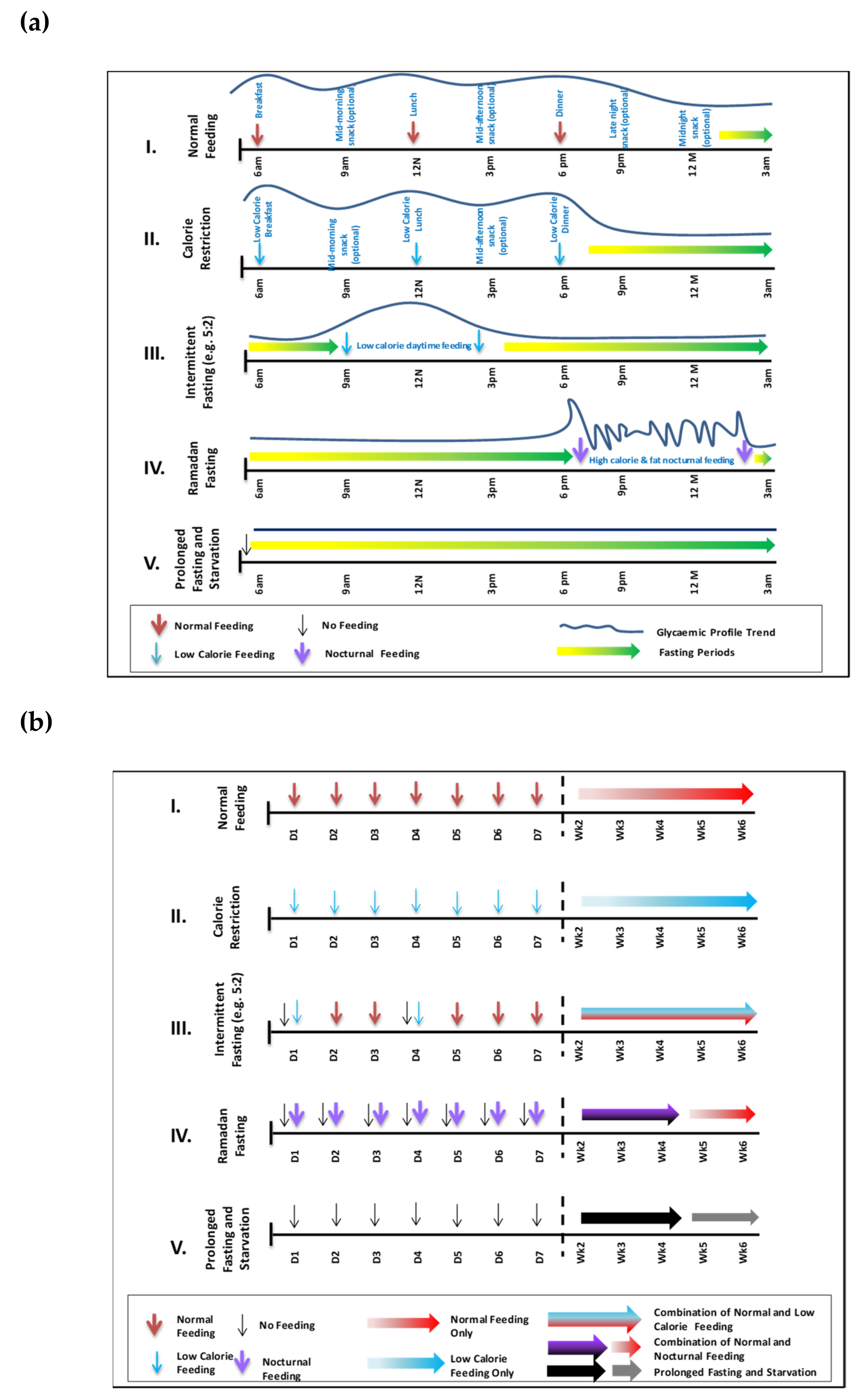
3. The Ramadan Fast: A Shift from Normal Eating Patterns
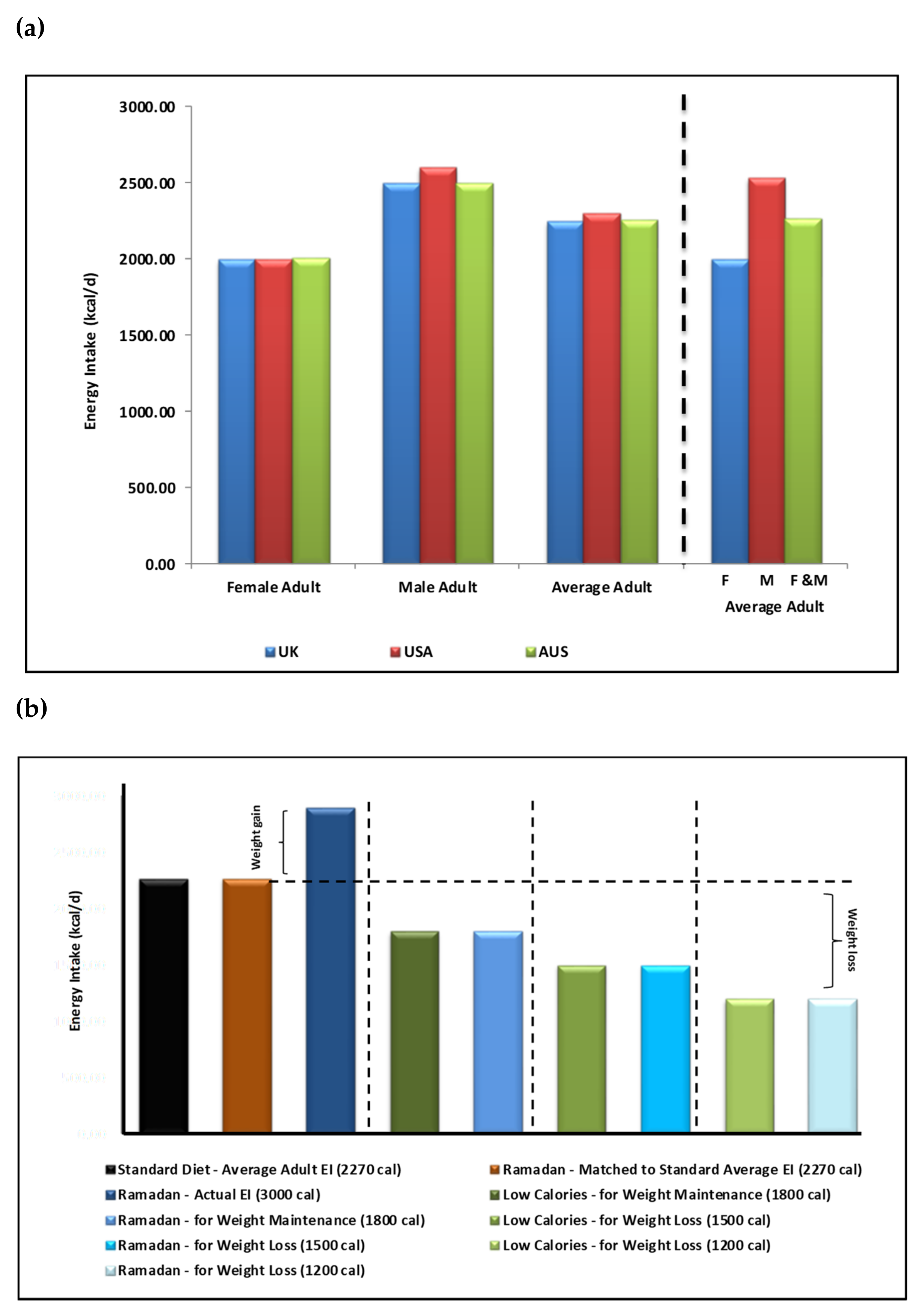
4. The Ramadan Diet
5. Weight and Body Composition Changes During Ramadan Fasting
6. Energy Expenditure During Ramadan Fasting
6.1. Resting Metabolic Rate (RMR) During Ramadan Fasting
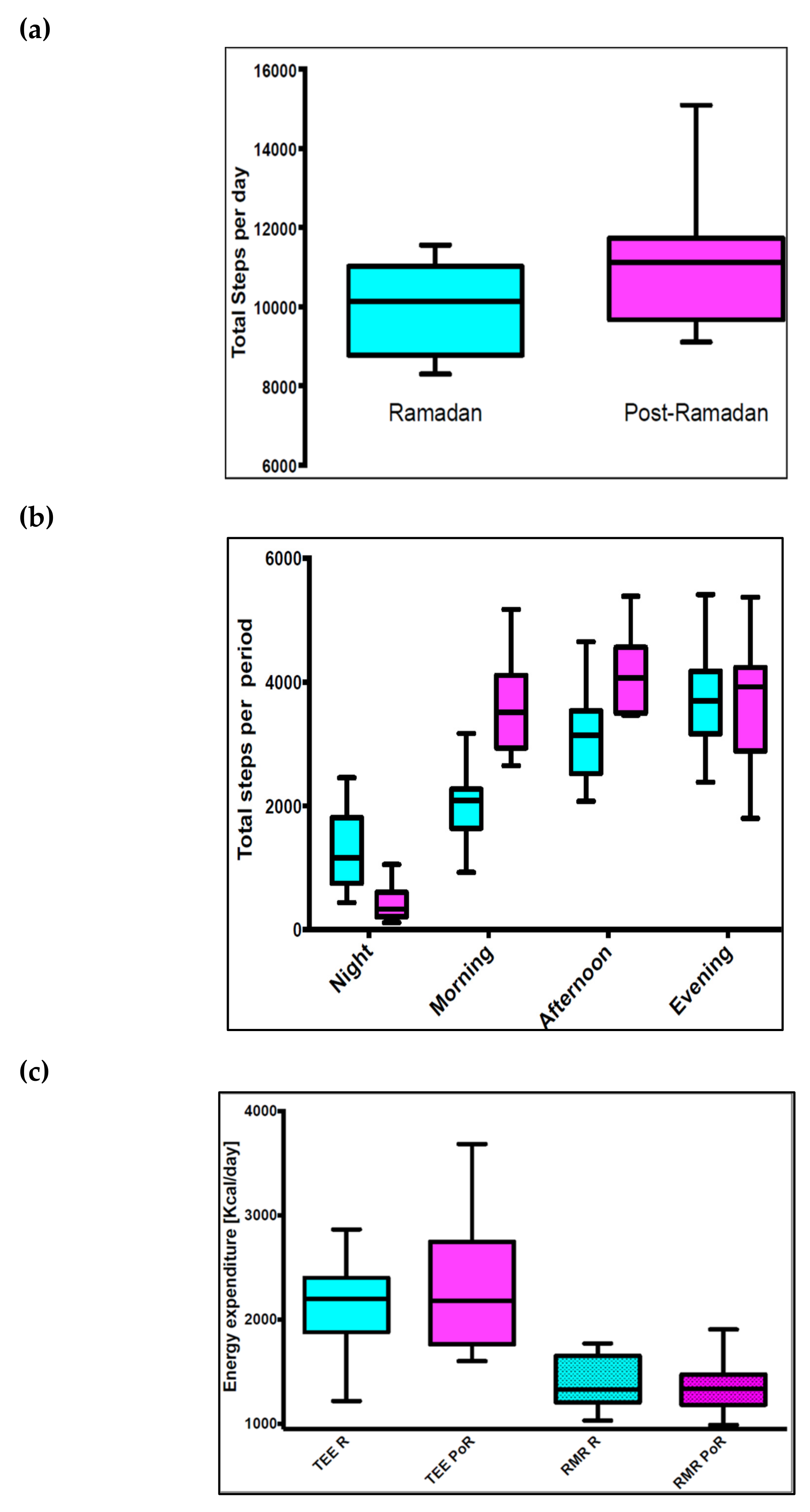
6.2. Activity Energy Expenditure (AEE) During Ramadan Fasting
6.3. Thermic Effect Of Food (TEF) During Ramadan Fasting
6.4. Fuel Utilization During Ramadan Fasting
6.5. Total Energy Expenditure (TEE) During Ramadan Fasting
7. Discussion and Concluding Remarks
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Patterson, R.E.; Laughlin, G.A.; LaCroix, A.Z.; Hartman, S.J.; Natarajan, L.; Senger, C.M.; Martínez, M.E.; Villaseñor, A.; Sears, D.D.; Marinac, C.R. Intermittent Fasting and Human Metabolic Health. J. Acad. Nutr. Diet. 2015, 115, 1203–1212. [Google Scholar] [CrossRef]
- Ali, M.M. The Holy Quran; King Fahd Complex for the Printing of the Holy Quran: Medina, Saudi Arabia, 2011; pp. 183–185. [Google Scholar]
- Horne, B.D.; Muhlestein, J.B.; Anderson, J.L. Health effects of intermittent fasting: Hormesis or harm? A systematic review. Am. J. Clin. Nutr. 2015, 102, 464–470. [Google Scholar] [CrossRef]
- Jane, L.; Atkinson, G.; Jaime, V.; Hamilton, S.; Waller, G.; Harrison, S. Intermittent fasting interventions for the treatment of overweight and obesity in adults aged 18 years and over: A systematic review protocol. JBI Database Syst. Rev. Implement Rep. 2015, 13, 60–68. [Google Scholar] [CrossRef]
- Michalsen, A.; Li, C. Fasting therapy for treating and preventing disease—Current state of evidence. Forsch. Komplementmed. 2013, 20, 444–453. [Google Scholar] [CrossRef]
- Omodei, D.; Fontana, L. Calorie restriction and prevention of age-associated chronic disease. FEBS Lett. 2011, 585, 1537–1542. [Google Scholar] [PubMed]
- Willcox, B.J.; Willcox, D.C. Caloric restriction, caloric restriction mimetics, and healthy aging in Okinawa: Controversies and clinical implications. Curr. Opin. Clin. Nutr. Metab. Care 2014, 17, 51–58. [Google Scholar] [CrossRef]
- Mattson, M.P.; Longo, V.D.; Harvie, M. Impact of intermittent fasting on health and disease processes. Ageing Res. Rev. 2017, 39, 46–58. [Google Scholar] [CrossRef] [PubMed]
- Desgorces, F.D.; Breuillard, C.; Police, C.; Neveux, N.; Cottart, C.H.; Blanc, M.C.; Toussaint, J.F.; Noirez, P. Short-term Effects of Diet and Activity Changes on Inflammation and Insulin Resistance. Int. J. Sports Med. 2016, 37, 1032–1037. [Google Scholar] [CrossRef] [PubMed]
- Michalsen, A. Prolonged fasting as a method of mood enhancement in chronic pain syndromes: A review of clinical evidence and mechanisms. Curr. Pain Headache Rep. 2010, 14, 80–87. [Google Scholar] [CrossRef] [PubMed]
- Nematy, M.; Alinezhad-Namaghi, M.; Rashed, M.M.; Mozhdehifard, M.; Sajjadi, S.S.; Akhlaghi, S.; Sabery, M.; Mohajeri, S.A.; Shalaey, N.; Moohebati, M.; et al. Effects of Ramadan fasting on cardiovascular risk factors: A prospective observational study. Nutr. J. 2012, 11, 69. [Google Scholar] [CrossRef] [PubMed]
- Sahin, S.B.; Ayaz, T.; Ozyurt, N.; Ilkkilic, K.; Kirvar, A.; Sezgin, H. The impact of fasting during Ramadan on the glycemic control of patients with type 2 diabetes mellitus. Exp. Clin. Endocrinol. Diabetes 2013, 121, 531–534. [Google Scholar] [PubMed]
- Roky, R.; Chapotot, F.; Hakkou, F.; Benchekroun, M.T.; Buguet, A. Sleep during Ramadan intermittent fasting. J. Sleep Res. 2001, 10, 319–327. [Google Scholar] [CrossRef] [PubMed]
- BaHammam, A.; Alrajeh, M.; Albabtain, M.; Bahammam, S.; Sharif, M. Circadian pattern of sleep, energy expenditure, and body temperature of young healthy men during the intermittent fasting of Ramadan. Appetite 2010, 54, 426–429. [Google Scholar] [CrossRef]
- Parnell, J.A.; Reimer, R.A. Weight loss during oligofructose supplementation is associated with decreased ghrelin and increased peptide YY in overweight and obese adults. Am. J. Clin. Nutr. 2009, 89, 1751–1759. [Google Scholar] [CrossRef]
- Patel, S.R.; Hu, F.B. Short sleep duration and weight gain: A systematic review. Obesity 2008, 16, 643–653. [Google Scholar] [CrossRef]
- Haouari, M.; Haouari-Oukerro, F.; Sfaxi, A.; Rayana, M.B.; Kaabachi, N.; Mbazaa, A. How Ramadan fasting affects caloric consumption, body weight, and circadian evolution of cortisol serum levels in young, healthy male volunteers. Horm. Metab. Res. 2008, 40, 575–577. [Google Scholar] [CrossRef]
- Kul, S.; Savaş, E.; Öztürk, Z.A.; Karadağ, G. Does Ramadan fasting alter body weight and blood lipids and fasting blood glucose in a healthy population? A meta-analysis. J. Relig. Health 2014, 53, 929–942. [Google Scholar] [CrossRef] [PubMed]
- Sadeghirad, B.; Motaghipisheh, S.; Kolahdooz, F.; Zahedi, M.J.; Haghdoost, A.A. Islamic fasting and weight loss: A systematic review and meta-analysis. Public Health Nutr. 2014, 17, 396–406. [Google Scholar] [CrossRef]
- Piaggi, P.; Vinales, K.L.; Basolo, A.; Santini, F.; Krakoff, J. Energy expenditure in the etiology of human obesity: Spendthrift and thrifty metabolic phenotypes and energy-sensing mechanisms. J. Endocrinol. Investig. 2018, 41, 83–89. [Google Scholar] [CrossRef] [PubMed]
- Gibney, E.R. Energy expenditure in disease: Time to revisit? Proc. Nutr. Soc. 2000, 59, 199–207. [Google Scholar] [CrossRef]
- Heymsfield, S.B.; Harp, J.B.; Rowell, P.N.; Nguyen, A.M.; Pietrobelli, A. How much may I eat? Calorie estimates based upon energy expenditure prediction equations. Obes. Rev. 2006, 7, 361–370. [Google Scholar] [CrossRef] [PubMed]
- Poehlman, E.T.; Melby, C.L.; Goran, M.I. The impact of exercise and diet restriction on daily energy expenditure. Sports Med. 1991, 11, 78–101. [Google Scholar] [CrossRef]
- Lessan, N.; Saadane, I.; Alkaf, B.; Hambly, C.; Buckley, A.J.; Finer, N.; Speakman, J.R.; Barakat, M.T. The effects of Ramadan fasting on activity and energy expenditure. Am. J. Clin. Nutr. 2018, 107, 54–61. [Google Scholar] [CrossRef] [PubMed]
- McMurray, R.G.; Soares, J.; Caspersen, C.J.; McCurdy, T. Examining variations of resting metabolic rate of adults: A public health perspective. Med. Sci. Sports Exerc. 2014, 46, 1352–1358. [Google Scholar] [CrossRef]
- National Research Council. Diet and Health: Implications for Reducing Chronic Disease Risk; The National Academies Press: Washington, DC, USA, 1989. [Google Scholar]
- De Jonge, L.; Bray, G.A. The thermic effect of food and obesity: A critical review. Obes. Res. 1997, 5, 622–631. [Google Scholar] [CrossRef]
- El Ati, J.; Beji, C.; Danguir, J. Increased fat oxidation during Ramadan fasting in healthy women: An adaptative mechanism for body-weight maintenance. Am. J. Clin. Nutr. 1995, 62, 302–307. [Google Scholar] [CrossRef]
- Alsubheen, S.A.; Ismail, M.; Baker, A.; Blair, J.; Adebayo, A.; Kelly, L.; Chandurkar, V.; Cheema, S.; Joanisse, D.R.; Basset, F.A. The effects of diurnal Ramadan fasting on energy expenditure and substrate oxidation in healthy men. Br. J. Nutr. 2017, 118, 1023–1030. [Google Scholar] [CrossRef]
- Lamri-Senhadji, M.Y.; El Kebir, B.; Belleville, J.; Bouchenak, M. Assessment of dietary consumption and time-course of changes in serum lipids and lipoproteins before, during and after Ramadan in young Algerian adults. Singapore Med. J. 2009, 50, 288–294. [Google Scholar]
- Bakhotmah, B.A. The puzzle of self-reported weight gain in a month of fasting (Ramadan) among a cohort of Saudi families in Jeddah, Western Saudi Arabia. Nutr. J. 2011, 10, 84. [Google Scholar] [CrossRef]
- Al-Hourani, H.M.; Atoum, M.F. Body composition, nutrient intake and physical activity patterns in young women during Ramadan. Singapore Med. J. 2007, 48, 906–910. [Google Scholar] [PubMed]
- Deranged Physiology. Available online: https://derangedphysiology.com/main/required-reading/endocrinology-metabolism-and-nutrition/Chapter%20318/physiological-adaptation-prolonged-starvation (accessed on 10 March 2019).
- Berg, J.M.; Tymoczko, J.L.; Stryer, L. Food Intake and Starvation Induce Metabolic Changes. In Biochemistry, 5th ed.; W.H. Freeman and Company: New York, NY, USA, 2002. [Google Scholar]
- Benedict, F.G. Chemical and Physiological Studies of a Man Fasting Thirtyone Days. Proc. Natl. Acad. Sci. USA 1915, 1, 228–231. [Google Scholar] [CrossRef] [PubMed]
- Kerndt, P.R.; Naughton, J.L.; Driscoll, C.E.; Loxterkamp, D. Fasting: The history, pathophysiology and complications. West. J. Med. 1982, 137, 379–399. [Google Scholar]
- Spriggs, E.I. The Fasting Treatment of Diabetes. Br. Med. J. 1916, 1, 841–845. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Cahill, G.F., Jr. Starvation in man. N. Engl. J. Med. 1970, 282, 668–675. [Google Scholar] [CrossRef]
- Danielsson, E.J.D.; Lejbman, I.; Akeson, J. Fluid deficits during prolonged overnight fasting in young healthy adults. Acta Anaesthesiol. Scand. 2019, 63, 195–199. [Google Scholar] [CrossRef]
- Korbonits, M.; Blaine, D.; Elia, M.; Powell-Tuck, J. Metabolic and hormonal changes during the refeeding period of prolonged fasting. Eur. J. Endocrinol. 2007, 157, 157–166. [Google Scholar] [CrossRef] [PubMed]
- Müller, M.J.; Enderle, J.; Pourhassan, M.; Braun, W.; Eggeling, B.; Lagerpusch, M.; Glüer, C.C.; Kehayias, J.J.; Kiosz, D.; Bosy-Westphal, A. Metabolic adaptation to caloric restriction and subsequent refeeding: The Minnesota Starvation Experiment revisited. Am. J. Clin. Nutr. 2015, 102, 807–819. [Google Scholar] [CrossRef]
- Al Junaibi, A.; Abdulle, A.; Sabri, S.; Hag-Ali, M.; Nagelkerke, N. The prevalence and potential determinants of obesity among school children and adolescents in Abu Dhabi, United Arab Emirates. Int. J. Obes. 2013, 37, 68–74. [Google Scholar] [CrossRef][Green Version]
- National Health Services (NHS). Available online: https://www.nhs.uk/live-well/eat-well/the-eatwell-guide/ (accessed on 20 March 2019).
- Office of Disease Prevention and Health Promotion. Available online: https://health.gov/dietaryguidelines/2015/guideline/appendix 2/ (accessed on 20 March 2019).
- Balancing Energy in and Out; Nutrition Australia. 2018. Available online: http://www.nutritionaustralia.org/national/resource/balancing-energy-and-out (accessed on 14 March 2019).
- Hamdy, O.; Yuson, B.N.M.; Reda, W.H.; Slim, I.; Jamoussi, H.; Omar, M. DaR Practical Guidelines; the Ramadan Nutrition Plan (RNP) for Patients with Diabetes; International Diabetes Federation and the DAR International Alliance: Brussels, Belgium, 2016; pp. 81–85. [Google Scholar]
- Vasan, S.; Thomas, N.; Bharani, A.M.; Abraham, S.; Job, V.; John, B.; Karol, R.; Kavitha, M.L.; Thomas, K.; Seshadri, M.S. A double-blind, randomized, multicenter study evaluating the effects of pioglitazone in fasting Muslim subjects during Ramadan. J. Diabetes Dev. Ctries. 2006, 26, 70–76. [Google Scholar]
- Lessan, N.; Hannoun, Z.; Hasan, H.; Barakat, M.T. Glucose excursions and glycaemic control during Ramadan fasting in diabetic patients: Insights from continuous glucose monitoring (CGM). Diabetes Metab. 2015, 41, 28–36. [Google Scholar] [CrossRef]
- Hajek, P.; Myers, K.; Dhanji, A.R.; West, O.; McRobbie, H. Weight change during and after Ramadan fasting. J. Public Health 2012, 34, 377–381. [Google Scholar] [CrossRef] [PubMed]
- Finch, G.M.; Day, J.E.; Welch, D.A.; Rogers, P.J. Appetite changes under free-living conditions during Ramadan fasting. Appetite 1998, 31, 159–170. [Google Scholar] [CrossRef]
- Fernando, H.A.; Zibellini, J.; Harris, R.A.; Seimon, R.V.; Sainsbury, A. Effect of Ramadan Fasting on Weight and Body Composition in Healthy Non-Athlete Adults: A Systematic Review and Meta-Analysis. Nutrients 2019, 11, 478. [Google Scholar] [CrossRef] [PubMed]
- Racinais, S.; Périard, J.D.; Li, C.K.; Grantham, J. Activity patterns, body composition and muscle function during Ramadan in a Middle-East Muslim country. Int. J. Sports Med. 2012, 33, 641–646. [Google Scholar] [CrossRef]
- Poh, B.K.; Zawiah, H.; Ismail, M.N.; Henry, C.J.K. Changes in body weight, dietary intake and activity pattern of adolescents during Ramadan. Malays. J. Nutr. 1996, 2, 1–10. [Google Scholar]
- Lean, M.E.; Garthwaite, P. Weight loss and longevity. Ann. Intern. Med. 1995, 123, 892. [Google Scholar] [CrossRef]
- Ramadan Nutrition Plan. Diabetes and Ramadan International Alliance (DaR). 2016. Available online: https://www.daralliance.org/daralliance/en/dr/about-rnp.html (accessed on 28 March 2019).
- Shadman, Z.; Akhoundan, M.; Poorsoltan, N.; Khoshniat Nikoo, M.; Larijani, B.; Akhgar Zhand, C.; Soleymanzadeh, M.; Alsadat Seyed Rohani, Z.; Jamshidi, Z. Nutritional Education Needs in Relation to Ramadan Fasting and Its Complications in Tehran, Iran. Iran. Red Crescent Med. J. 2016, 18, e26130. [Google Scholar] [CrossRef]
- Shadman, Z.; Poorsoltan, N.; Akhoundan, M.; Larijani, B.; Soleymanzadeh, M.; Akhgar Zhand, C.; Seyed Rohani, Z.A.; Khoshniat Nikoo, M. Ramadan major dietary patterns. Iran. Red Crescent Med. J. 2014, 16, e16801. [Google Scholar] [CrossRef]
- Leiper, J.B.; Molla, A.M.; Molla, A.M. Effects on health of fluid restriction during fasting in Ramadan. Eur. J. Clin. Nutr. 2003, 57, 30–38. [Google Scholar] [CrossRef] [PubMed]
- Carroll, H.A.; Templeman, I.; Chen, Y.C.; Edinburgh, R.M.; Burch, E.K.; Jewitt, J.T.; Povey, G.; Robinson, T.D.; Dooley, W.L.; Jones, R.; et al. Effect of acute hypohydration on glycemic regulation in healthy adults: A randomized crossover trial. J. Appl. Physiol. 2019, 126, 422–430. [Google Scholar] [CrossRef] [PubMed]
- Turin, T.C.; Ahmed, S.; Shommu, N.S.; Afzal, A.R.; Al Mamun, M.; Qasqas, M.; Rumana, N.; Vaska, M.; Berka, N. Ramadan fasting is not usually associated with the risk of cardiovascular events: A systematic review and meta-analysis. J. Family Community Med. 2016, 23, 73–81. [Google Scholar] [CrossRef] [PubMed]
| Ref. | Year | Study Cohort | Gender & Age (Years) | Reported Observations |
|---|---|---|---|---|
| [14] | 2010 | Healthy adults 1-week pre-Ramadan baseline (BL) as well as first and second week of Ramadan (R1) and (R2); n = 7). | Males; 21 ± 3 | SenseWear Pro Armband measurements indicated EE and METs significantly lower during Ramadan and a shift in circadian patterns (of body temperature, a delay in bedtime and an increase in total sleep time and nap time) during Ramadan. No significant difference in the number of meals. |
| [24] | 2018 | Healthy adults during Ramadan and non-Ramadan periods. RMR (n = 29, 16 female) Activity (total steps per day) (n = 11, 5 female); TEE (n = 10, 5 female). | Female and male; 33 ± 9 | Indirect calorimetry; (a) activity during and post- Ramadan; no significant difference, (b) activity pattern: morning & afternoon significantly lower during Ramadan. Nocturnal activity was higher during Ramadan, (c) TEE & RMR during and post-Ramadan: no significant difference; main factor influencing TEE was body weight. |
| [28] | 1995 | Healthy adults, 2 days pre-Ramadan (T1); the 2nd day (T2), and the 28th day (T3) of fasting; & 1 month after, (n = 16). | Female; 25–39 | Indirect calorimetry; calculations from metabolic chamber; REE unchanged during and post-Ramadan, compared with pre- Ramadan. EE throughout the circadian cycle was dramatically affected during fasting with a significant decrease observed from 11am to 5pm during Ramadan. Nightly EE values did not change significantly. |
| [29] | 2017 | Healthy fasting (FAST, n = 9) and non-fasting (CNT, n = 8) adults pre and post-Ramadan. FAST group additionally assessed at days 10, 20 & 30 of Ramadan (am) & (pm). | Male; FAST: 32 ± 8 and CNT: 35 ± 9 | Indirect calorimetry; significant group × time interaction, reduced body mass and adiposity in FAST, without changing lean mass; for CNT subjects, remained unchanged. Ramadan fasting induces diurnal metabolic adjustments (morning v. evening) with no carryover effect observed throughout Ramadan fasting despite the extended daily fasting period and changes in body composition. |
| Ref | Year | Study Cohort | Gender & Age (Years) | Reported Observations |
|---|---|---|---|---|
| [18] | 2014 | Healthy fasting adults with normal body weight; n = 1476; 553 female and 923 male) | Female and male; ≥18 | In the female subgroup, body weight (SMD = −0.04, 95% CI = −0.20, 0.12) remained unchanged, while in males, Ramadan fasting resulted in weight loss (SMD = −0.24, 95% CI = −0.36, −0.12, p = 0.001). |
| [28] | 1995 | Healthy fasting adults, two days pre-Ramadan (T1); second (T2) and 28th day (T3) of Ramadan; and 1 month post-Ramadan (T4); n = 16 | Female; 25–39 | Total daily energy intake, body weight, fat mass and fat free mass remain unchanged. REE pattern change; lower during the fasting day versus night but no significant change overall. |
| [29] | 2017 | Healthy fasting (FAST, n = 9) and non-fasting (CNT, n = 8) adults pre and post-Ramadan. FAST group additionally assessed at days 10, 20 & 30 of Ramadan both (am) and (pm). | Male; FAST: 32 ± 8, CNT: 35 ± 9 | Significant group × time interaction revealed reduced body mass and adiposity in FAST, without changing lean mass, whereas CNT subjects remained unchanged. Although RF induces diurnal metabolic adjustments (morning v. evening), no carryover effect was observed throughout Ramadan fasting despite the extended daily fasting period and changes in body composition. |
| [30] | 2009 | Healthy fasting adults, n = 46; 24 female and 22 male. | Female and male; 24 ± 3 | Total energy intake was higher during Ramadan (13 and 11 MJ/day) than before and after Ramadan (11 and 9 MJ/day) in men and women, respectively. |
| [31] | 2011 | 173 families fasting Ramadan | Female and male; age unspecified | 59.5% reported weight gain post-Ramadan; 40% attributed food types, 31.2% attributed to relative lack of physical exercise and 14.5% referred that to increase in food consumption. 65.2% of those with increased expenditure reported weight gain. |
| [32] | 2007 | Healthy fasting adults at one-week pre-Ramadan (T1), first week (T2), end of second week (T3), and end of last week (T4) of Ramadan; n = 57 | Female; 22 ± 4 | Body weight and BMI decreased significantly during Ramadan fasting. The mean physical activity level was not significantly different. The overall activity patterns remained similar; 1.54 pre-and 1.51 during Ramadan |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lessan, N.; Ali, T. Energy Metabolism and Intermittent Fasting: The Ramadan Perspective. Nutrients 2019, 11, 1192. https://doi.org/10.3390/nu11051192
Lessan N, Ali T. Energy Metabolism and Intermittent Fasting: The Ramadan Perspective. Nutrients. 2019; 11(5):1192. https://doi.org/10.3390/nu11051192
Chicago/Turabian StyleLessan, Nader, and Tomader Ali. 2019. "Energy Metabolism and Intermittent Fasting: The Ramadan Perspective" Nutrients 11, no. 5: 1192. https://doi.org/10.3390/nu11051192
APA StyleLessan, N., & Ali, T. (2019). Energy Metabolism and Intermittent Fasting: The Ramadan Perspective. Nutrients, 11(5), 1192. https://doi.org/10.3390/nu11051192





