The Effect of Enteral Tube Feeding on Patients’ Health-Related Quality of Life: A Systematic Review
Abstract
1. Introduction
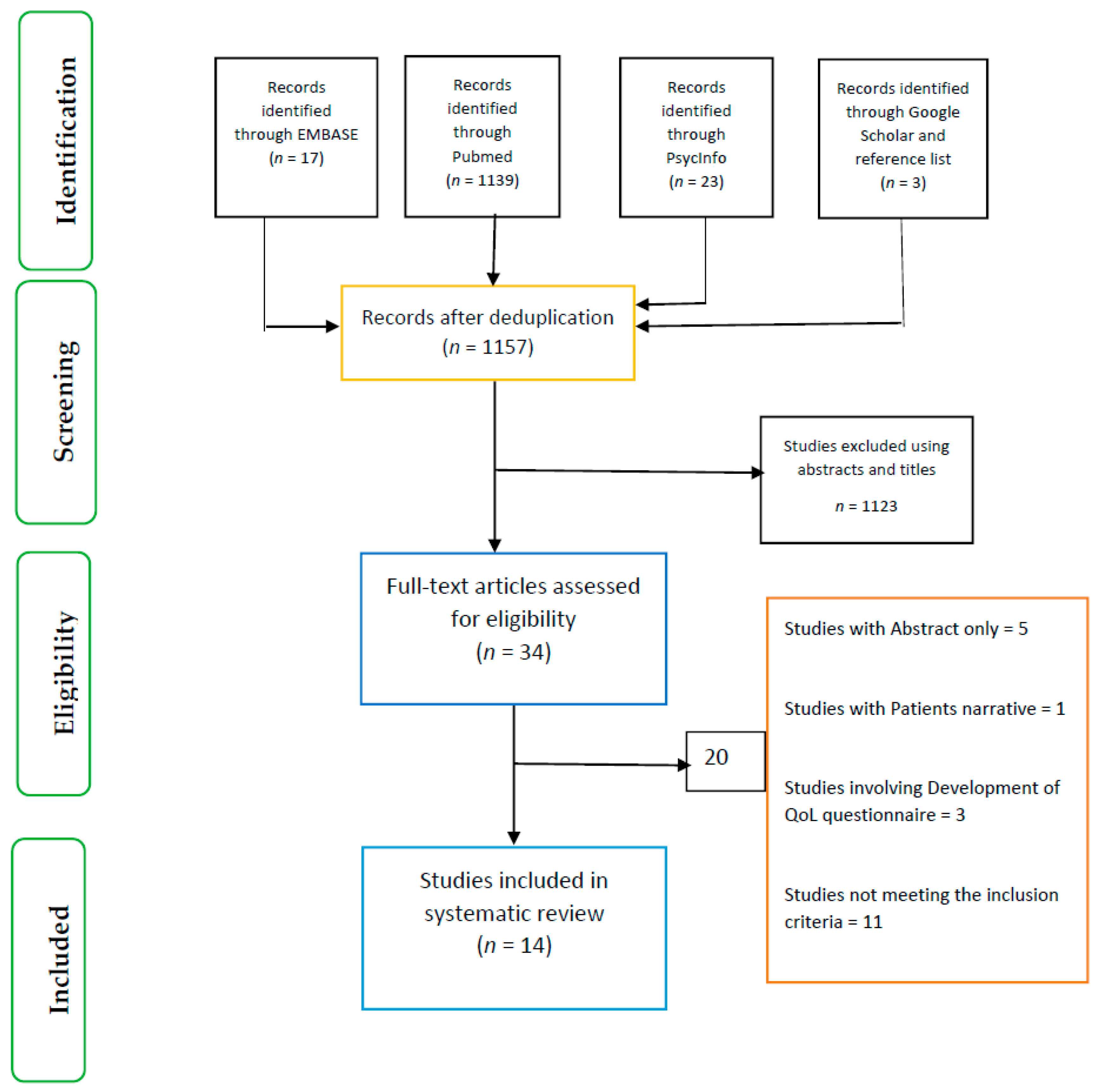
2. Method
2.1. Types of Studies
2.2. Participants and Interventions
2.3. Outcome Measures
2.4. Search Terms and Search Strategy
2.5. Inclusion and Exclusion Criteria
2.6. Quality Assessment
2.7. Data Extraction
3. Results
- The effect of early versus late enteral tube placement/feeding on QoL
- QoL of patients on gastrostomy compared with standard care
- The effect of enteral tube feeding on QoL
3.1. The Effect of Early Versus Late Enteral Tube Placement/Feeding on QoL
3.2. Quality of Life of Patients on Gastrostomy Compared with Standard Care
3.3. The Effect of Enteral Tube Feeding on Quality of Life
4. Discussion
4.1. Factors Influencing the Role of Enteral Tube Feeding on Patients’ QoL
4.2. Implications for Research and Practice
5. Limitations of the Review
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Ojo, O. The challenges of home enteral tube feeding: A global perspective. Nutrients 2015, 7, 2524–2538. [Google Scholar] [CrossRef]
- Best, C.; Hitchings, H. Enteral tube feeding–From hospital to home. Br. J. Nurs. 2010, 19, 174. [Google Scholar] [CrossRef]
- Dennis, M.S.; Lewis, S.C.; Warlow, C. Effect of timing and method of enteral tube feeding for dysphagic stroke patients (FOOD): A multicentre randomised controlled trial. Lancet 2005, 365, 764–772. [Google Scholar]
- Rowat, A. Malnutrition and dehydration after stroke. Nursing Stand. 2011, 26, 42–46. [Google Scholar] [CrossRef]
- Rowat, A. Enteral tube feeding for dysphagic stroke patients. Br. J. Nurs. 2015, 24, 138–144. [Google Scholar] [CrossRef]
- Lim, M.L.; Yong, B.Y.P.; Mar, M.Q.M.; Ang, S.Y.; Chan, M.M.; Lam, M.; Lopez, V. Caring for patients on home enteral nutrition: Reported complications by home carers and perspectives of community nurses. J. Clin. Nurs. 2018, 27, 2825–2835. [Google Scholar] [CrossRef]
- Chen, S.; Xian, W.; Cheng, S.; Zhou, C.; Zhou, H.; Feng, J.; Chen, L. Risk of regurgitation and aspiration in patients infused with different volumes of enteral nutrition. Asia Pac. J. Clin. Nutr. 2015, 24, 212–218. [Google Scholar] [CrossRef]
- Löser, C.; Aschl, G.; Hébuterne, X.; Mathus-Vliegen, E.M.H.; Muscaritoli, M.; Niv, Y.; Skelly, R.H. ESPEN guidelines on artificial enteral nutrition-percutaneous endoscopic gastrostomy (PEG). Clin. Nutr. 2005, 24, 848–861. [Google Scholar]
- Bernstein, O.A.; Campbell, J.; Rajan, D.K.; Kachura, J.R.; Simons, M.E.; Beecroft, J.R.; Tan, K.T. Randomized Trial Comparing Radiologic Pigtail Gastrostomy and Peroral Image-Guided Gastrostomy: Intra- and Postprocedural Pain, Radiation Exposure, Complications, and Quality of Life. J. Vasc. Interv. Radiol. 2015, 26, 1680–1686. [Google Scholar] [CrossRef]
- Magné, N.; Marcy, P.Y.; Foa, C.; Falewee, M.N.; Schneider, M.; Demard, F.; Bensadoun, R.J. Comparison between nasogastric tube feeding and percutaneous fluoroscopic gastrostomy in advanced head and neck cancer patients. Eur. Arch. Oto-Rhino-Laryngol. 2001, 258, 89–92. [Google Scholar] [CrossRef]
- Ojo, O.; Brooke, J. Recent Advances in Enteral Nutrition. Nutrients 2016, 8, 709. [Google Scholar] [CrossRef]
- Bourgault, A.M.; Ipe, L.; Weaver, J.; Swartz, S.; O’Dea, P.J. Development of evidence-based guidelines and critical care nurses’ knowledge of enteral feeding. Crit. Care Nurse 2007, 27, 17–29. [Google Scholar]
- Ojo, O.; Brooke, J. Evaluation of the Role of Enteral Nutrition in Managing Patients with Diabetes: A Systematic Review. Nutrients 2014, 6, 5142–5152. [Google Scholar] [CrossRef]
- Wang, G.; Chen, H.; Liu, J.; Ma, Y.; Jia, H. A comparison of postoperative early enteral nutrition with delayed enteral nutrition in patients with esophageal cancer. Nutrients 2015, 7, 4308–4317. [Google Scholar] [CrossRef]
- Altomare, R.; Damiano, G.; Abruzzo, A.; Palumbo, V.D.; Tomasello, G.; Buscemi, S.; Lo Monte, A.I. Enteral Nutrition Support to Treat Malnutrition in Inflammatory Bowel Disease. Nutrients 2015, 7, 2125–2133. [Google Scholar] [CrossRef]
- Wanden-Berghe, C.; Nolasco, A.; Sanz-Valero, J.; Planas, M.; Cuerda, C. Health-related quality of life in patients with home nutritional support. J. Hum. Nutr. Diet. 2009, 22, 219–225. [Google Scholar] [CrossRef]
- Govindaraju, T.; Sahle, B.W.; McCaffrey, T.A.; McNeil, J.J.; Owen, A.J. Dietary Patterns and Quality of Life in Older Adults: A Systematic Review. Nutrients 2018, 10, 971. [Google Scholar] [CrossRef]
- EQ-5D Health Questionnaire. Available online: https://www.aaos.org/uploadedFiles/EQ5D3L.pdf (accessed on 31 December 2018).
- Mandy van Reenen and Bas Janssen (2015) EQ-5D-5L User Guide Basic Information on How to Use the EQ-5D-5L Instrument Version 2.1. Available online: https://euroqol.org/wp-content/uploads/2016/09/EQ-5D-5L_UserGuide_2015.pdf (accessed on 31 December 2018).
- World Health Organisation (1996) WHOQOL-BREF Introduction, Administration, Scoring and Generic Version of the Assessment. Available online: File:///L:/World%20Health%20Organisation%20(WHO%20Quality%20of%20Life%20BREF)%20.pdf (accessed on 20 December 2018).
- Cuerda, M.C.; Apezetxea, A.; Carrillo, L.; Casanueva, F.; Cuesta, F.; Irles, J.A.; Lizan, L. Development and validation of a specific questionnaire to assess health-related quality of life in patients with home enteral nutrition: NutriQoL(R) development. Patient Prefer. Adher. 2016, 10, 2289–2296. [Google Scholar] [CrossRef]
- Day, T. Home enteral feeding and its impact on quality of life. Br. J. Community Nurs. 2017, 22, S14–S16. [Google Scholar] [CrossRef]
- White, H.; King, L. Enteral feeding pumps: Efficacy, safety, and patient acceptability. Med. Dev. Evid. Res. 2014, 7, 291–298. [Google Scholar] [CrossRef]
- Arevalo-Manso, J.J.; Martinez-Sanchez, P.; Juarez-Martin, B.; Fuentes, B.; Ruiz-Ares, G.; Sanz-Cuesta, B.E.; Parrilla-Novo, P.; Diez-Tejedor, E. Enteral tube feeding of patients with acute stroke: When does the risk of diarrhoea increase? Int. Med. J. 2014, 44, 1199–1204. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Prisma, G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 2009, 339, b2535. [Google Scholar] [CrossRef]
- Baker, J.; Janda, M.; Graves, N.; Bauer, J.; Banks, M.; Garrett, A.; Nicklin, J.L. Quality of life after early enteral feeding versus standard care for proven or suspected advanced epithelial ovarian cancer: Results from a randomised trial. Gynecol. Oncol. 2015, 137, 516–522. [Google Scholar] [CrossRef]
- Bannerman, E.; Pendlebury, J.; Phillips, F.; Ghosh, S. A cross-sectional and longitudinal study of health-related quality of life after percutaneous gastrostomy. Eur. J. Gastroenterol. Hepatol. 2000, 12, 1101–1109. [Google Scholar] [CrossRef]
- Critical Appraisal Skills Programme (CASP). CASP Checklists. 2018. Available online: https://casp-uk.net/casp-tools-checklists/ (accessed on 8 February 2019).
- Morton, R.P.; Crowder, V.L.; Mawdsley, R.; Ong, E.; Izzard, M. Elective gastrostomy, nutritional status and quality of life in advanced head and neck cancer patients receiving chemoradiotherapy. ANZ J. Surg. 2009, 79, 713–718. [Google Scholar] [CrossRef]
- Hossein, S.M.; Leili, M.; Hossein, A.M. Acceptability and outcomes of percutaneous endoscopic gastrostomy (PEG) tube placement and patient quality of life. Turk. J. Gastroenterol. 2011, 22, 128–133. [Google Scholar] [CrossRef]
- Kurien, M.; Andrews, R.E.; Tattersall, R.; McAlindon, M.E.; Wong, E.F.; Johnston, A.J.; Sanders, D.S. Gastrostomies Preserve But Do Not Increase Quality of Life for Patients and Caregivers. Clin. Gastroenterol. Hepatol. 2017, 15, 1047–1054. [Google Scholar] [CrossRef]
- Rogers, S.N.; Thomson, R.; O’Toole, P.; Lowe, D. Patients experience with long-term percutaneous endoscopic gastrostomy feeding following primary surgery for oral and oropharyngeal cancer. Oral. Oncol. 2007, 43, 499–507. [Google Scholar] [CrossRef]
- Salas, S.; Baumstarck-Barrau, K.; Alfonsi, M.; Digue, L.; Bagarry, D.; Feham, N.; Zanaret, M. Impact of the prophylactic gastrostomy for unresectable squamous cell head and neck carcinomas treated with radio-chemotherapy on quality of life: Prospective randomized trial. Radiother. Oncol. 2009, 93, 503–509. [Google Scholar] [CrossRef]
- Donohoe, C.L.; Healy, L.A.; Fanning, M.; Doyle, S.L.; Hugh, A.M.; Moore, J.; Reynolds, J.V. Impact of supplemental home enteral feeding postesophagectomy on nutrition, body composition, quality of life, and patient satisfaction. Dis. Esophagus 2017, 30, 1–9. [Google Scholar] [CrossRef]
- Guo, Z.; Wu, R.; Zhu, W.; Gong, J.; Zhang, W.; Li, Y.; Li, J. Effect of exclusive enteral nutrition on health-related quality of life for adults with active Crohn’s disease. Nutr. Clin. Pract. 2013, 28, 499–505. [Google Scholar] [CrossRef] [PubMed]
- Loeser, C.; von Herz, U.; Kuchler, T.; Rzehak, P.; Muller, M.J. Quality of life and nutritional state in patients on home enteral tube feeding. Nutrition 2003, 19, 605–611. [Google Scholar] [CrossRef]
- Roberge, C.; Tran, M.; Massoud, C.; Poiree, B.; Duval, N.; Damecour, E.; Henry-Amar, M. Quality of life and home enteral tube feeding: A French prospective study in patients with head and neck or oesophageal cancer. Br. J. Cancer 2000, 82, 263–269. [Google Scholar] [CrossRef]
- Schneider, S.M.; Pouget, I.; Staccini, P.; Rampal, P.; Hebuterne, X. Quality of life in long-term home enteral nutrition patients. Clin. Nutr. 2000, 19, 23–28. [Google Scholar] [CrossRef]
- Wu, Z.; Wu, M.; Wang, Q.; Zhan, T.; Wang, L.; Pan, S.; Chen, G. Home enteral nutrition after minimally invasive esophagectomy can improve quality of life and reduce the risk of malnutrition. Asia. Pac. J. Clin. Nutr. 2018, 27, 129–136. [Google Scholar]
- Zeng, J.; Hu, J.; Chen, Q.; Feng, J. Home enteral nutrition’s effects on nutritional status and quality of life after esophagectomy. Asia. Pac. J. Clin. Nutr. 2017, 26, 804–810. [Google Scholar]
- Kumar, S.; Langmore, S.; Goddeau, R.P., Jr.; Alhazzani, A.; Selim, M.; Caplan, L.R.; Schlaug, G. Predictors of percutaneous endoscopic gastrostomy tube placement in patients with severe dysphagia from an acute-subacute hemispheric infarction. J. Stroke Cerebrovasc. Dis. Off. J. Natl. Stroke Assoc. 2012, 21, 114–120. [Google Scholar] [CrossRef]
- National Institute for Health and Care Excellence (2006) Nutrition Support for Adults: Oral Nutrition Support, Enteral Tube Feeding and Parenteral Nutrition. Available online: Nice.org.uk/guidance/cg32 (accessed on 1 March 2019).
- Dunn, S. Maintaining adequate hydration and nutrition in adult enteral tube feeding. Br. J. Community Nurs. 2015, 20, S16–S23. [Google Scholar] [CrossRef]
- Kurien, M.; White, S.; Simpson, G.; Grant, J.; Sanders, D.S.; McAlindon, M.E. Managing patients with gastrostomy tubes in the community: Can a dedicated enteral feed dietetic service reduce hospital readmissions? Eur. J. Clin. Nutr. 2012, 66, 757–760. [Google Scholar] [CrossRef]
- Reeves, A.; White, H.; Sosnowski, K.; Leveritt, M.; Desbrow, B.; Jones, M. Multidisciplinary evaluation of a critical care enteral feeding algorithm. Nutr. Diet. 2012, 69, 242–249. [Google Scholar] [CrossRef]
- Apezetxea, A.; Carrillo, L.; Casanueva, F.; Cuerda, C.; Cuesta, F.; Irles, J.A.; Virgili, M.N.; Layola, M.; Lizán, L. The NutriQoL questionnaire for assessing health related quality of life (HRQoL) in patients with home enteral nutrition (HEN): Validation and first results. Nutr. Hosp. 2016, 33, 1260–1267. [Google Scholar] [CrossRef]
- Martin, L.; Blomberg, J.; Lagergren, P. Patients’ perspectives of living with a percutaneous endoscopic gastrostomy (PEG). BMC Gastroenterol. 2012, 12, 126. [Google Scholar] [CrossRef]
- Alivizatos, V.; Gavala, V.; Alexopoulos, P.; Apostolopoulos, A.; Bajrucevic, S. Feeding Tube-related Complications and Problems in Patients Receiving Long-term Home Enteral Nutrition. Indian J. Palliat. Care 2012, 18, 31–33. [Google Scholar] [CrossRef]
- Apezetxea, A.; Carrillo, L.; Casanueva, F.; de la Cuerda, C.; Cuesta, F.; Irles, J.A.; Lizán, L. Rasch analysis in the development of the NutriQoL(R) questionnaire, a specific health-related quality of life instrument for home enteral nutrition. J. Patient Rep. Outcomes 2018, 2, 25. [Google Scholar] [CrossRef] [PubMed]
| Patient/Population | Intervention | Comparator | Outcomes of Interest | Combining Search Terms |
|---|---|---|---|---|
| Patients on enteral tube feeding | Enteral nutrition | Control | Quality of life | |
| Patients on enteral tube feeding OR Enteral feeding OR Enteral nutrition OR Feeding, enteral OR Nutrition, enteral | Nutrition, Enteral OR Enteral feeding OR Feeding, Enteral OR Tube feeding OR Feeding, Tube OR Gastric feeding tubes OR Feeding tube, Gastric OR Feeding tubes, Gastric OR Gastric feeding tube OR Tube, Gastric feeding OR Tubes, Gastric feeding | Control OR Standard diet OR Normal diet as tolerated OR Baseline values | Life quality OR Health-related quality of life OR Health-related quality of life OR HRQoL OR QoL | Column 1 AND Column 2 AND Column 3 |
| Study Reference | Country of Study | Study Type/Design | Sample Size | Age (Years) | Aim/Objective | Interventions Including Type of Tube and/or Enteral Feeding | Results of QoL Scores Following Interventions | Conclusion |
|---|---|---|---|---|---|---|---|---|
| The effect of early versus late enteral tube placement/feeding on QoL | ||||||||
| Baker et al. (2015) [26] | Australia | Phase III multicenter, randomized clinical trial | Intervention N = 53 Standard care N = 56 Total N = 109 | Mean (SD) Intervention: 61.8 (11.4) Standard care: 63.7 (12.7) | Whether early postoperative enteral nutrition for malnourished women with advanced epithelial ovarian cancer can improve their QoL compared to Standard care | Nasojejunal tube: Early enteral feeding versus Standard care | Baseline EQ5D Index (SD) Intervention = 0.70 (0.20) Standard care = 0.65 (0.22) 6 weeks Postoperatively EQ5D Index: Intervention = 0.78 (0.22) Standard care = 0.76 (0.15) 30 days Post-chemotherapy EQ5D Index Intervention = 0.85 (0.13) Standard care = 0.78 (0.16) Baseline VAS (SD) Intervention = 60 (23) Standard care = 51 (20) 6 weeks Postoperatively VAS (SD) Intervention = 69 (20) Standard care = 61 (21) 30 days Post-chemotherapy VAS Intervention = 72.8 (15.2) Standard care = 65.2 (19.2) | Early enteral feeding did not significantly improve patient’s QoL compared to standard care but may improve nutritional status |
| Morton et al. (2009) [29] | New Zealand | Retrospective chart review over a 24-month period. | N = 36 | Median = 52 | To examine the factors associated with PEG insertion and the effects of PEG use on QoL and functional outcomes in head and neck cancer (HNC) patients receiving chemoradiotherapy | PEG insertion: (1) tube inserted before treatment or within 1 month of commencement of treatment (2) tube inserted 1 month or more after start of treatment | Patients who still had PEG in situ at the time of the survey had a significantly worse total QoL score (p = 0.006) Overall QoL Score: Nutrition mode at time of study = 0.363 (p = 0.063) PEG in situ at time of study = 0.518 (p = 0.006) Longer PEG duration predicted poor overall QoL (p < 0.01) | Early PEG insertion and shorter PEG duration are associated with more favorable QoL-related outcomes |
| Quality of Life of patients on gastrostomy compared with standard care | ||||||||
| Bannerman et al. (2000) [27] | United Kingdom | Cross-sectional and prospective cohorts | Prospective study: N = 54 | Median = 58 | To determine the impact of gastrostomy on QoL | Patients were assessed prior to gastrostomy (endoscopic or radiological) placement at baseline, 1, 6 and 12 months | No significant difference in SF-36 scores at the time of tube placement and 1, 6, 12 months follow-up (p > 0.05), except for physical function score (Mean ± SD) Baseline scores = 43.8 (34.9) 6 months = 14.7 (20.9) p = 0.01. No significant difference in the proportion of patients showing that gastronomy had a positive impact on their QoL (p > 0.05). Based on the PEG-Qu assessment, at 6 and 12 months: 71% and 75% of patients respectively expressed a positive overall effect on their QoL | Most patients can cope adequately with the care of gastrostomy, despite considerable impairment of physical function. QoL of patients fed via gastrostomy is independent of nutritional outcome. Overall, the positive impact of gastrostomy on QoL was perceived in 55% of patients and 80% carers |
| Hossein et al. (2011) [30] | Iran | Cross-sectional study | N = 100 | Mean (SD) 59.73 ± 18.16 | To assess the perspectives of patients regarding the acceptability of PEG tube placement and evaluate the outcomes | PEG tube | QoL index scores (Mean) Pre-PEG: 19.25 ± 11.85 6 months after: 32.08 ± 27.74 When comparing the mean QoL index scores before and after PEG placement there was significant improvement (p < 0.005) after PEG placement | PEG tube is a minimally invasive gastrostomy method with low morbidity and mortality rates, and is easy to follow-up and to replace when blockage occurs |
| Kurien et al. (2017) [31] | United Kingdom | Prospective multicenter cohort study | N = 100 (patients) N = 100 (caregivers) N = 200 (control) | Mean (SD) Patients: 67 (14.7) Caregivers: 65 (12.2) Control: 60 (10.1) | To determine how gastrostomies affect QoL in patients and caregivers | PEG (55%) + RIG (45%) | Baseline (before gastrostomy) versus 3 months post insertion (Mean ± SD) No significant longitudinal changes in mean EuroQoL index scores for patients (0.70 before vs. 0.710 after; p = 0.83) or caregivers (0.95 before vs. 0.95 after; p = 0.32) following gastrostomy insertion | QoL did not significantly improve after gastrostomy insertion for patients or caregivers. Gastrostomies may help maintain QoL |
| Rogers et al. (2007) [32] | United Kingdom | Cross-sectional survey | N = 243 | Mean (SD) 65 (12) | To devise, pilot and survey a PEG specific questionnaire and relate outcomes to QoL | PEG | Global measures score (0–100) QoL (Mean; SE) as measured by UW-QoL Never had PEG: 63 (1) PEG removed at 7 months: 68 (3) Still has PEG at 34 months: 41 (4) | Patients with PEGs reported significant deficits in all UW-QOL domains compared to non-PEG or PEG-removed patients and reported a much poorer QoL |
| Salas et al. (2009) [33] | France | Randomized, controlled study | N = 39 No systematic gastrostomy (standard group) = 18 Systematic gastrostomy (experimental group) = 21 | Mean (SD) Standard = 60.0 ± 4.5 Experimental = 58.7 ± 7.7 | To assess the impact of prophylactic gastrostomy on the 6-month QoL, and to determine the factors related to this QoL | Systematic percutaneous gastrostomy versus no systematic gastrostomy | QoL at Inclusion SF36 Score Standard: 49.4 ± 25.1 Experiment: 59.2 ± 21.8 (p = 0.19) EORTC (QLQ-C30): Standard: 57.8 ± 25.8 Experiment: 63.0 ± 24.1 (p = 0.37) QoL at 6 months was significantly higher in the group receiving systematic prophylactic gastrostomy (p = 10−3) | Prophylactic gastrostomy improves post-treatment QoL for unresectable head and HNC, after adjusting for other potential predictive QoL factors |
| The effect of Enteral tube feeding on QoL | ||||||||
| Donohoe et al. (2017) [34] | Ireland | Prospective cohort study | N = 149 | Mean (SD) 62 ± 9 | To analyze the impact of supplemental HEN post-esophageal cancer surgery on quality of life | HEN | QoL measured at baseline, preoperatively, and at 1, 3, and 6 months Mean Global QoL decreased (p < 0.01) from 82 to 72. Global QoL (follow-up long-term) was not significantly different in those with <10% vs. >10% weight respectively (68.7 ± 20.6 vs. 70.95 ± 17.5, p = 0.519). With persistent weight loss (3–6 months postoperative, n = 12) there was clinically relevant decrease in QoL in physical (76.7 vs. 87.5, p = 0.066) and social function (76.4 vs. 87.8, p = 0.034) | Weight loss and negative consequences on QoL occurs despite supplemental enteral nutrition in majority of patients |
| Guo et al. (2013) [35] | China | Uncontrolled pilot clinical trial | N = 13 | Mean (SD) 26.1 (3.8) | To determine the effect of exclusive enteral nutrition (EEN) on patients QoL in adults with active Crohn’s disease | Enteral nutrition | There were significant improvements in total IBDQ scores after 4-week EEN treatment (Mean ± SD) 128.3 ± 15.8 to 182.9 ± 24.2 (p < 0.001) | A 4-week treatment of EEN improves QoL significantly in adults with active Crohn’s disease and was acceptable by most patients |
| Loeser et al. (2003) [36] | Germany | Prospective cross-sectional (Study 1) Prospective longitudinal (Study 2: follow-up 4 months) | Cross-sectional N = 155 Longitudinal N = 56 | Mean (SD) 64.3 ± 13.1 | To assess QoL in patients on HETF. | HETF HETF/PEG insertion | Study 1: When compared with EORTC reference data, functional scales were lower in HETF patients and QoL was significantly lower in non-competent patients. Study 2: QLQ-C30 (N = 26) PEG insertion: 44.2 ± 19.7 2 months: 46.5 ± 16.0 4 months: 50.6 ± 1 Lower QoL was observed in non-competent than in competent patients | QoL is decreased in patients on HETF. Part of this explained by malnutrition. HETF can prevent further weight loss and improve some aspects of QoL |
| Roberge et al. (2000) [37] | France | Prospective study | N = 39 | Mean = 58 | To evaluate the impact of HETF on QoL in patients treated for head and neck or esophageal cancer. Evaluations were carried out 1st week and 3rd week post hospital discharge | HETF/PEG insertion | QLQ-C30 Mean (SD) Global health status: 45(19). Overall, QoL slightly improved 3 weeks post-discharge; some symptoms significantly improved (p < 0.05): constipation, coughing, social functioning and body image/sexuality | Home enteral tube feeding is a physically well accepted technique although some of the patients may experience psychosocial distress |
| Schneider et al. (2000) [38] | France | Cross-sectional study | N = 38 | Mean (SEM) 56 ± 5 | To assess both the QoL of long-term patients on HEN (for 25 ± 5 months) and the evolution of QoL after initiation of HEN | HEN vs. general population | EQ-5D index HEN: 0.54 ± 0.07 vs. General: 0.85 ± 0.0 (p < 0.05) Visual Analogue Scale HEN: 54.1 ± 4.2 vs. General: 82.5 ± 0.3 (p < 0.05) SF-36 (Mental Component Scale) HEN: 46.2 ± 2.6 vs. General: 51.8 ± 0.3 SF-36 (Physical Component Scale) HEN: 37.1 ± 2.1 vs. General: 46.5 ± 1.2 (p < 0.05) | QoL is poor in HEN patients compared to age and sex matched general population. Most patients describe an improvement in their QoL following the initiation of HEN |
| Wu et al. (2018) [39] | China | Single-center, prospective, non-randomized study | N = 142 | Median (Range) Minimally invasive esophagectomy/laparoscopic jejunal feeding tube+HEN (MIE): 62 (45–80) Open esophagectomy/ nasojejunal feeding tube (OE): 61 (43–80) | To investigate the effect of 3 months HEN on QoL and nutritional status of esophageal cancer patients who were preoperatively malnourished. | MIE vs. OE | QoL (Global health status) (Mean ± SD) Preoperative MIE:69.9 (9.1) OE:70.1(10.3), p = 0.546 2 weeks MIE: 19.6 (7.5) OE: 18.4 (7.0), p = 0.821 3 months MIE: 55.7 (7.4) OE: 41.8 (7.0), p = 0.001 | MIE and subsequent treatment with 3 months HEN can improve QoL and reduce the risk of malnutrition in preoperatively malnourished patients |
| Zeng et al. (2017) [40] | China | Non-Randomized Clinical trial | N = 60 HEN: N = 30 Control (Standard Care): N = 30 | Mean (SD) HEN: 61.7 ± 8.4 Control: 59.3 ± 10.4 | To characterize the effect of HEN on nutritional status and QoL of esophageal cancer patients who underwent Ivor Lewis esophagectomy for cancer | HEN vs. standard care | Combined use of QLQ-C30 and QLQ-ES18 Compared to the control group, the HEN group achieved higher Global QoL scores, and most of their functional index scores were better. However, 24 weeks after surgery, QoL indexes did not differ significantly between the two groups | HEN can reduce the incidence of malnutrition or latent malnutrition and help restore QoL in the patients with esophageal cancer in the early period (24 weeks) after surgery |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ojo, O.; Keaveney, E.; Wang, X.-H.; Feng, P. The Effect of Enteral Tube Feeding on Patients’ Health-Related Quality of Life: A Systematic Review. Nutrients 2019, 11, 1046. https://doi.org/10.3390/nu11051046
Ojo O, Keaveney E, Wang X-H, Feng P. The Effect of Enteral Tube Feeding on Patients’ Health-Related Quality of Life: A Systematic Review. Nutrients. 2019; 11(5):1046. https://doi.org/10.3390/nu11051046
Chicago/Turabian StyleOjo, Omorogieva, Edel Keaveney, Xiao-Hua Wang, and Ping Feng. 2019. "The Effect of Enteral Tube Feeding on Patients’ Health-Related Quality of Life: A Systematic Review" Nutrients 11, no. 5: 1046. https://doi.org/10.3390/nu11051046
APA StyleOjo, O., Keaveney, E., Wang, X.-H., & Feng, P. (2019). The Effect of Enteral Tube Feeding on Patients’ Health-Related Quality of Life: A Systematic Review. Nutrients, 11(5), 1046. https://doi.org/10.3390/nu11051046






