Comparison of Conventional and Individualized 1-MET Values for Expressing Maximum Aerobic Metabolic Rate and Habitual Activity Related Energy Expenditure
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Study Design
2.3. Anthropometric Data and Body Composition
2.4. Resting Metabolic Rate
2.5. Measurement of VO2max
2.6. Calculation of METmax and Estimation of Energy Expenditure
2.7. Physical Activity Level (PAL)
2.8. Statistics
3. Results
3.1. Participants
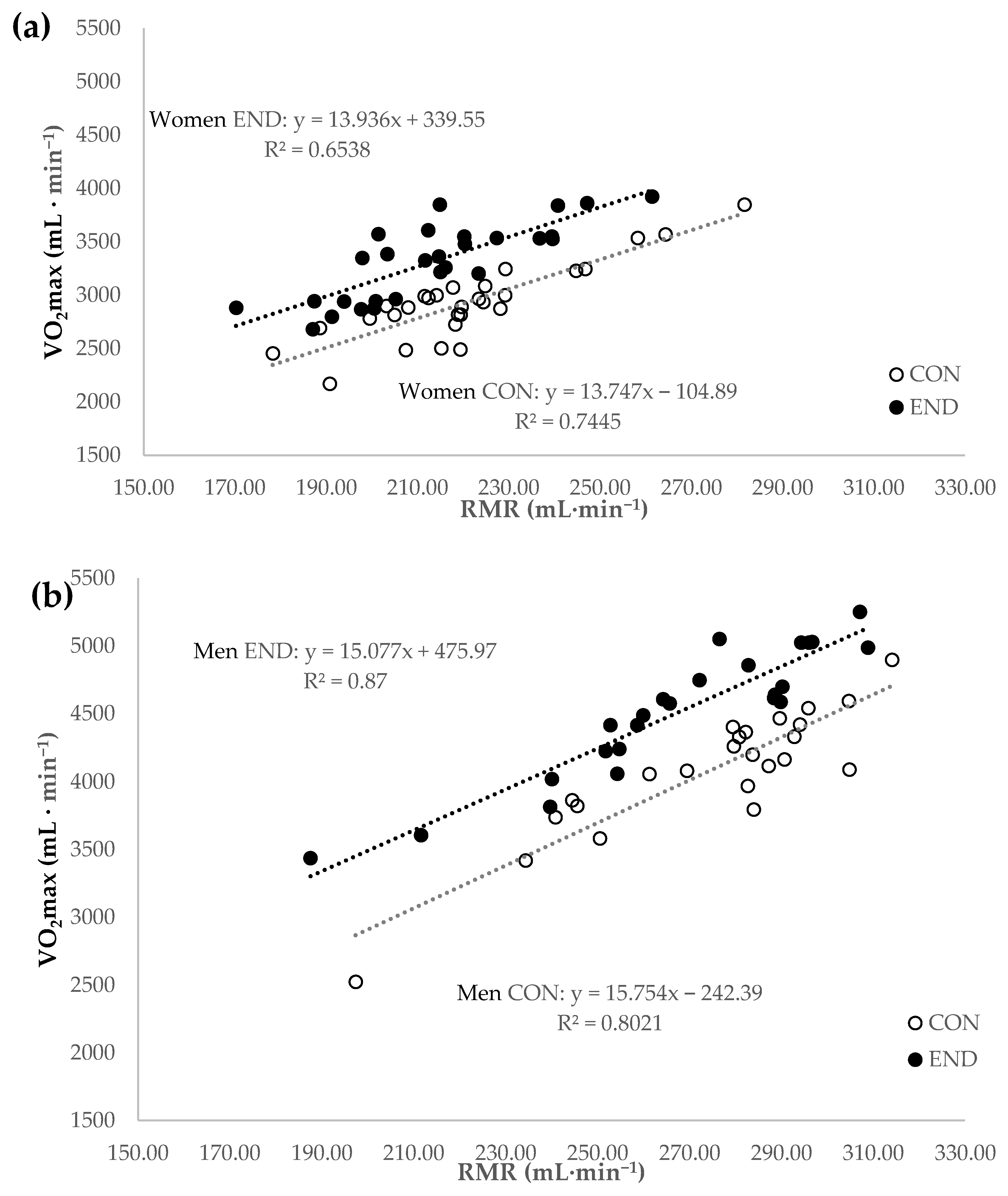
3.2. Calculation of METmax
3.3. Estimation of AEE/TEE
4. Discussion
4.1. Calculation of METmax
4.2. Estimation of AEE, TEE, and Physical Activity Level (PAL = TEE/RMR)
4.3. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Bassett, D.R.; Howley, E.T. Limiting factors for maximum oxygen uptake and determinants of endurance performance. Med. Sci. Sports Exerc. 2000, 32, 70–84. [Google Scholar] [CrossRef] [PubMed]
- Kodama, S.; Saito, K.; Tanaka, S.; Maki, M.; Yachi, Y.; Asumi, M.; Sugawara, A.; Totsuka, K.; Shimano, H.; Ohashi, Y.; et al. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: A meta-analysis. JAMA 2009, 301, 2024–2035. [Google Scholar] [CrossRef] [PubMed]
- Nevill, A.M.; Ramsbottom, R.; Williams, C. Scaling physiological measurements for individuals of different body size. Eur. J. Appl. Physiol. 1992, 65, 110–117. [Google Scholar] [CrossRef]
- Vanderburgh, P.M.; Katch, F.I. Ratio scaling of VO2max penalizes women with larger percent body fat, not lean body mass. Med. Sci. Sports Exerc. 1996, 28, 1204–1208. [Google Scholar] [CrossRef] [PubMed]
- Nevill, A.; Rowland, T.; Goff, D.; Martel, L.; Ferrone, L. Scaling or normalising maximum oxygen uptake to predict 1-mile run time in boys. Eur. J. Appl. Physiol. 2004, 92, 285–288. [Google Scholar] [CrossRef] [PubMed]
- Darveau, C.A.; Suarez, R.K.; Andrews, R.D.; Hochachka, P.W. Allometric cascade as a unifying principle of body mass effects on metabolism. Nature 2002, 417, 166–170. [Google Scholar] [CrossRef] [PubMed]
- Weibel, E.R. Physiology: The pitfalls of power laws. Nature 2002, 417, 131–132. [Google Scholar] [CrossRef] [PubMed]
- Nevill, A.M.; Stewart, A.D.; Olds, T.; Holder, R. Are adult physiques geometrically similar? The dangers of allometric scaling using body mass power laws. Am. J. Phys. Anthropol. 2004, 124, 177–182. [Google Scholar] [CrossRef]
- Ainsworth, B.E.; Haskell, W.L.; Herrmann, S.D.; Meckes, N.; Bassett, D.R.; Tudor-Locke, C.; Greer, J.L.; Vezina, J.; Whitt-Glover, M.C.; Leon, A.S. 2011 Compendium of Physical Activities: A second update of codes and MET values. Med. Sci. Sports Exerc. 2011, 43, 1575–1581. [Google Scholar] [CrossRef]
- Jetté, M.; Sidney, K.; Blümchen, G. Metabolic equivalents (METS) in exercise testing, exercise prescription, and evaluation of functional capacity. Clin. Cardiol. 1990, 13, 555–565. [Google Scholar] [CrossRef] [PubMed]
- Matthews, C.E.; Ainsworth, B.E.; Hanby, C.; Pate, R.R.; Addy, C.; Freedson, P.S.; Jones, D.A.; Macera, C.A. Development and testing of a short physical activity recall questionnaire. Med. Sci. Sports Exerc. 2005, 37, 986–994. [Google Scholar] [PubMed]
- Ishikawa-Takata, K.; Naito, Y.; Tanaka, S.; Ebine, N.; Tabata, I. Use of doubly labeled water to validate a physical activity questionnaire developed for the Japanese population. J. Epidemiol. 2011, 21, 114–121. [Google Scholar] [CrossRef] [PubMed]
- Adams, S.A.; Matthews, C.E.; Ebbeling, C.B.; Moore, C.G.; Cunningham, J.E.; Fulton, J.; Hebert, J.R. The effect of social desirability and social approval on self-reports of physical activity. Am. J. Epidemiol. 2005, 161, 389–398. [Google Scholar] [CrossRef] [PubMed]
- Conway, J.M.; Seale, J.L.; Jacobs, D.R.; Irwin, M.L.; Ainsworth, B.E. Comparison of energy expenditure estimates from doubly labeled water, a physical activity questionnaire, and physical activity records. Am. J. Clin. Nutr. 2002, 75, 519–525. [Google Scholar] [CrossRef] [PubMed]
- Leenders, N.Y.; Sherman, W.M.; Nagaraja, H.N.; Kien, C.L. Evaluation of methods to assess physical activity in free-living conditions. Med. Sci. Sports Exerc. 2001, 33, 1233–1240. [Google Scholar] [CrossRef] [PubMed]
- Seale, J.L.; Klein, G.; Friedmann, J.; Jensen, G.L.; Mitchell, D.C.; Smiciklas-Wright, H. Energy expenditure measured by doubly labeled water, activity recall, and diet records in the rural elderly. Nutr. Burbank Los Angel. Cty. Calif. 2002, 18, 568–573. [Google Scholar] [CrossRef]
- Byrne, N.M.; Hills, A.P.; Hunter, G.R.; Weinsier, R.L.; Schutz, Y. Metabolic equivalent: One size does not fit all. J. Appl. Physiol. 2005, 99, 1112–1119. [Google Scholar] [CrossRef] [PubMed]
- Kozey, S.; Lyden, K.; Staudenmayer, J.; Freedson, P. Errors in MET estimates of physical activities using 3.5 mL x kg(-1) x min(-1) as the baseline oxygen consumption. J. Phys. Act. Health 2010, 7, 508–516. [Google Scholar] [CrossRef] [PubMed]
- Melzer, K.; Heydenreich, J.; Schutz, Y.; Renaud, A.; Kayser, B.; Mäder, U. Metabolic equivalent in adolescents, active adults and pregnant women. Nutrients 2016, 8, 438. [Google Scholar] [CrossRef]
- McMurray, R.G.; Soares, J.; Caspersen, C.J.; McCurdy, T. Examining variations of resting metabolic rate of adults: A public health perspective. Med. Sci. Sports Exerc. 2014, 46, 1352–1358. [Google Scholar] [CrossRef]
- Brooks, A.G.; Withers, R.T.; Gore, C.J.; Vogler, A.J.; Plummer, J.; Cormack, J. Measurement and prediction of METs during household activities in 35- to 45-year-old females. Eur. J. Appl. Physiol. 2004, 91, 638–648. [Google Scholar] [CrossRef] [PubMed]
- Gunn, S.M.; Brooks, A.G.; Withers, R.T.; Gore, C.J.; Plummer, J.L.; Cormack, J. The energy cost of household and garden activities in 55- to 65-year-old males. Eur. J. Appl. Physiol. 2005, 94, 476–486. [Google Scholar] [CrossRef] [PubMed]
- Gunn, S.M.; Brooks, A.G.; Withers, R.T.; Gore, C.J.; Owen, N.; Booth, M.L.; Bauman, A.E. Determining energy expenditure during some household and garden tasks. Med. Sci. Sports Exerc. 2002, 34, 895–902. [Google Scholar] [CrossRef] [PubMed]
- Withers, R.T.; Brooks, A.G.; Gunn, S.M.; Plummer, J.L.; Gore, C.J.; Cormack, J. Self-selected exercise intensity during household/garden activities and walking in 55 to 65-year-old females. Eur. J. Appl. Physiol. 2006, 97, 494–504. [Google Scholar] [CrossRef] [PubMed]
- Kwan, M.; Woo, J.; Kwok, T. The standard oxygen consumption value equivalent to one metabolic equivalent (3.5 mL/min/kg) is not appropriate for elderly people. Int. J. Food Sci. Nutr. 2004, 55, 179–182. [Google Scholar] [CrossRef] [PubMed]
- Savage, P.D.; Toth, M.J.; Ades, P.A. A Re-examination of the metabolic equivalent concept in individuals with coronary heart disease. J. Cardiopulm. Rehabil. Prev. 2007, 27, 143–148. [Google Scholar] [CrossRef] [PubMed]
- Harris, J.A.; Benedict, F.G. A Biometric study of human basal metabolism. Proc. Natl. Acad. Sci. USA 1918, 4, 370–373. [Google Scholar] [CrossRef] [PubMed]
- Cunningham, J.J. Body composition as a determinant of energy expenditure: A synthetic review and a proposed general prediction equation. Am. J. Clin. Nutr. 1991, 54, 963–969. [Google Scholar] [CrossRef]
- Frankenfield, D.; Roth-Yousey, L.; Compher, C. Comparison of predictive equations for resting metabolic rate in healthy nonobese and obese adults: A systematic review. J. Am. Diet. Assoc. 2005, 105, 775–789. [Google Scholar] [CrossRef]
- Flack, K.D.; Siders, W.A.; Johnson, L.; Roemmich, J.N. Cross-validation of resting metabolic rate prediction wquations. J. Acad. Nutr. Diet. 2016, 116, 1413–1422. [Google Scholar] [CrossRef]
- Carver, T.E.; Christou, N.V.; Andersen, R.E. In vivo precision of the GE iDXA for the assessment of total body composition and fat distribution in severely obese patients. Obesity 2013, 21, 1367–1369. [Google Scholar] [CrossRef] [PubMed]
- Hind, K.; Oldroyd, B.; Truscott, J.G. In vivo precision of the GE Lunar iDXA densitometer for the measurement of total body composition and fat distribution in adults. Eur. J. Clin. Nutr. 2011, 65, 140–142. [Google Scholar] [CrossRef] [PubMed]
- Compher, C.; Frankenfield, D.; Keim, N.; Roth-Yousey, L. Evidence Analysis Working Group. Best practice methods to apply to measurement of resting metabolic rate in adults: A systematic review. J. Am. Diet. Assoc. 2006, 106, 881–903. [Google Scholar] [CrossRef] [PubMed]
- Weir, J.B.D.B. New methods for calculating metabolic rate with special reference to protein metabolism. J. Physiol. 1949, 109, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Marti, B.; Villiger, B.; Hintermann, M.; Lerch, R. Plötzlicher Herztod beim Sport: Sinnvolle Vorsorgeuntersuchungen und Präventionsmassnahmen. Schweizerische Zeitschrift für “Sportmedizin und Sporttraumatologie” 1998, 46, 83–85. [Google Scholar]
- Société canadienne de physiologie de l’exercice. Questionnaire sur l’aptitude à l’activité physique (Q-AAP). 2002. Available online: http://www.csep.ca/CMFiles/publications/parq/Q-AAP.pdf (accessed on 25 August 2016).
- Steiner, T.; Wehrlin, J.P. Does hemoglobin mass increase from age 16 to 21 and 28 in elite endurance athletes? Med. Sci. Sports Exerc. 2011, 43, 1735–1743. [Google Scholar] [CrossRef] [PubMed]
- Robergs, R.A.; Dwyer, D.; Astorino, T. Recommendations for improved data processing from expired gas analysis indirect calorimetry. Sports Med. Auckl. N. Z. 2010, 40, 95–111. [Google Scholar] [CrossRef] [PubMed]
- Borg, G. Perceived exertion as an indicator of somatic stress. Scand. J. Rehabil. Med. 1970, 2, 92–98. [Google Scholar] [PubMed]
- Taylor, H.L.; Buskirk, E.; Henschel, A. Maximal oxygen intake as an objective measure of cardio-respiratory performance. J. Appl. Physiol. 1955, 8, 73–80. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, H.; Monahan, K.D.; Seals, D.R. Age-predicted maximal heart rate revisited. J. Am. Coll. Cardiol. 2001, 37, 153–156. [Google Scholar] [CrossRef]
- Howley, E.T.; Bassett, D.R.; Welch, H.G. Criteria for maximal oxygen uptake: Review and commentary. Med. Sci. Sports Exerc. 1995, 27, 1292–1301. [Google Scholar] [CrossRef] [PubMed]
- Myers, J.; Arena, R.; Franklin, B.; Pina, I.; Kraus, W.E.; McInnis, K.; Balady, G.J.; American Heart Association Committee on Exercise, Cardiac Rehabilitation, and Prevention of the Council on Clinical Cardiology, the Council on Nutrition, Physical Activity, and Metabolism, and the Council on Cardiovascular Nursing. Recommendations for clinical exercise laboratories: A scientific statement from the American heart association. Circulation 2009, 119, 3144–3161. [Google Scholar] [PubMed]
- Physical Activity Guidelines Advisory Committee report, 2008. To the Secretary of Health and Human Services. Part A: Executive summary. Nutr. Rev. 2009, 67, 114–120. [CrossRef] [PubMed]
- Human Energy Requirements: Report of a Joint FAO/WHO/UNU Expert Consultation Rome, 17–24 October 2001; FAO Food and Nutrition Technical Report Series; United Nations University: Rome, Italy, 2004; ISBN 978-92-5-105212-9.
- Brage, S.; Brage, N.; Ekelund, U.; Luan, J.; Franks, P.W.; Froberg, K.; Wareham, N.J. Effect of combined movement and heart rate monitor placement on physical activity estimates during treadmill locomotion and free-living. Eur. J. Appl. Physiol. 2006, 96, 517–524. [Google Scholar] [CrossRef] [PubMed]
- Manore, M.M.; Thompson, J.L. Energy requirements of the athlete: Assessment and evidence of energy efficiency. In Clinical Sports Nutrition; Burke, L.M., Deakin, V., Eds.; McGraw-Hill Australia Pty Ltd.: North Ryde, Australia, 2010; pp. 96–115. [Google Scholar]
- Thompson, D.; Batterham, A.M.; Bock, S.; Robson, C.; Stokes, K. Assessment of low-to-moderate intensity physical activity thermogenesis in young adults using synchronized heart rate and accelerometry with branched-equation modeling. J. Nutr. 2006, 136, 1037–1042. [Google Scholar] [CrossRef] [PubMed]
- Butte, N.F.; Wong, W.W.; Adolph, A.L.; Puyau, M.R.; Vohra, F.A.; Zakeri, I.F. Validation of cross-sectional time series and multivariate adaptive regression splines models for the prediction of energy expenditure in children and adolescents using doubly labeled water. J. Nutr. 2010, 140, 1516–1523. [Google Scholar] [CrossRef] [PubMed]
- Crouter, S.E.; Churilla, J.R.; Bassett, D.R. Accuracy of the Actiheart for the assessment of energy expenditure in adults. Eur. J. Clin. Nutr. 2008, 62, 704–711. [Google Scholar] [CrossRef]
- Brage, S.; Westgate, K.; Franks, P.W.; Stegle, O.; Wright, A.; Ekelund, U.; Wareham, N.J. Estimation of free-living energy expenditure by heart rate and movement sensing: A doubly-labelled water study. PLoS ONE 2015, 10, e0137206. [Google Scholar] [CrossRef]
- Villars, C.; Bergouignan, A.; Dugas, J.; Antoun, E.; Schoeller, D.A.; Roth, H.; Maingon, A.C.; Lefai, E.; Blanc, S.; Simon, C. Validity of combining heart rate and uniaxial acceleration to measure free-living physical activity energy expenditure in young men. J. Appl. Physiol. 2012, 113, 1763–1771. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for Behavioral Sciences; Lawrence Erlbaum Associates: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Boudreaux, B.D.; Hebert, E.P.; Hollander, D.B.; Williams, B.M.; Cormier, C.L.; Naquin, M.R.; Gillan, W.W.; Gusew, E.E.; Kraemer, R.R. Validity of wearable activity monitors during cycling and resistance exercise. Med. Sci. Sports Exerc. 2018, 50, 624–633. [Google Scholar] [CrossRef]
- Lee, J.-M.; Kim, Y.; Welk, G.J. Validity of consumer-based physical activity monitors. Med. Sci. Sports Exerc. 2014, 46, 1840–1848. [Google Scholar] [CrossRef] [PubMed]
- Nelson, M.B.; Kaminsky, L.A.; Dickin, D.C.; Montoye, A.H.K. Validity of consumer-based physical activity monitors for specific activity types. Med. Sci. Sports Exerc. 2016, 48, 1619–1628. [Google Scholar] [CrossRef] [PubMed]
- Roos, L.; Taube, W.; Beeler, N.; Wyss, T. Validity of sports watches when estimating energy expenditure during running. BMC Sports Sci. Med. Rehabil. 2017, 9, 22. [Google Scholar] [CrossRef] [PubMed]
- Forse, R.A. Comparison of gas exchange measurements with a mouthpiece, face mask, and ventilated canopy. JPEN J. Parenter. Enteral Nutr. 1993, 17, 388–391. [Google Scholar] [CrossRef] [PubMed]
- Boulay, M.R.; Serresse, O.; Almeras, N.; Tremblay, A. Energy expenditure measurement in male cross-country skiers: Comparison of two field methods. Med. Sci. Sports Exerc. 1994, 26, 248–253. [Google Scholar] [CrossRef] [PubMed]
- Drenowatz, C.; Eisenmann, J.C.; Pivarnik, J.M.; Pfeiffer, K.A.; Carlson, J.J. Differences in energy expenditure between high- and low-volume training. Eur. J. Sport Sci. 2013, 13, 422–430. [Google Scholar] [CrossRef] [PubMed]
- Koshimizu, T.; Matsushima, Y.; Yokota, Y.; Yanagisawa, K.; Nagai, S.; Okamura, K.; Komatsu, Y.; Kawahara, T. Basal metabolic rate and body composition of elite Japanese male athletes. J. Med. Investig. JMI 2012, 59, 253–260. [Google Scholar] [CrossRef]
- LaForgia, J.; Withers, R.T.; Williams, A.D.; Murch, B.J.; Chatterton, B.E.; Schultz, C.G.; Leaney, F. Effect of 3 weeks of detraining on the resting metabolic rate and body composition of trained males. Eur. J. Clin. Nutr. 1999, 53, 126–133. [Google Scholar] [CrossRef]
- Sato, A.; Shimoyama, Y.; Ishikawa, T.; Murayama, N. Dietary thiamin and riboflavin intake and blood thiamin and riboflavin concentrations in college swimmers undergoing intensive training. Int. J. Sport Nutr. Exerc. Metab. 2011, 21, 195–204. [Google Scholar] [CrossRef]
- Herring, J.L.; Molé, P.A.; Meredith, C.N.; Stern, J.S. Effect of suspending exercise training on resting metabolic rate in women. Med. Sci. Sports Exerc. 1992, 24, 59–65. [Google Scholar] [CrossRef]
- Trappe, T.A.; Gastaldelli, A.; Jozsi, A.C.; Troup, J.P.; Wolfe, R.R. Energy expenditure of swimmers during high volume training. Med. Sci. Sports Exerc. 1997, 29, 950–954. [Google Scholar] [CrossRef] [PubMed]
- Rehrer, N.J.; Hellemans, I.J.; Rolleston, A.K.; Rush, E.; Miller, B.F. Energy intake and expenditure during a 6-day cycling stage race. Scand. J. Med. Sci. Sports 2010, 20, 609–618. [Google Scholar] [CrossRef] [PubMed]
- Desgorces, F.D.; Chennaoui, M.; Drogou, C.; Guezennec, C.Y.; Gomez-Merino, D. Relationships between leptin levels and carbohydrate intake during rowing training. J. Sports Med. Phys. Fit. 2008, 48, 83–89. [Google Scholar]
- Zogg, S.; Dürr, S.; Maier, S.; Tomatis, L.; Uehli, K.; Miedinger, D.; Leuppi, J.D. Relationship between domain-specific physical activity and different body composition measures in a working population. J. Occup. Environ. Med. 2014, 56, 1074–1081. [Google Scholar] [CrossRef] [PubMed]
- Mueller, S.M.; Herter-Aeberli, I.; Cepeda-Lopez, A.C.; Flück, M.; Jung, H.H.; Toigo, M. The effect of body composition and serum inflammatory markers on the functional muscle-bone unit in premenopausal women. Int. J. Obes. 2017, 41, 1203–1206. [Google Scholar] [CrossRef] [PubMed]
- Mountjoy, M.; Sundgot-Borgen, J.K.; Burke, L.M.; Ackerman, K.E.; Blauwet, C.; Constantini, N.; Lebrun, C.; Lundy, B.; Melin, A.K.; Meyer, N.L.; et al. IOC consensus statement on relative energy deficiency in sport (RED-S): 2018 update. Br. J. Sports Med. 2018, 52, 687–697. [Google Scholar] [CrossRef] [PubMed]
- Howley, E.T. To the Editor. J. Phys. Act. Health 2011, 8, 141–142. [Google Scholar] [CrossRef]
- Subar, A.F.; Freedman, L.S.; Tooze, J.A.; Kirkpatrick, S.I.; Boushey, C.; Neuhouser, M.L.; Thompson, F.E.; Potischman, N.; Guenther, P.M.; Tarasuk, V.; et al. Addressing current criticism regarding the value of self-report dietary data. J. Nutr. 2015, 145, 2639–2645. [Google Scholar] [CrossRef]

| Women | Men | |||
|---|---|---|---|---|
| CON (n = 29) | END (n = 28) | CON (n = 24) | END (n = 24) | |
| Age (years) | 27.6 ± 4.1 | 39.0 ± 6.1 | 27.0 ± 5.2 | 26.6 ± 5.0 |
| Body mass (kg) | 60.7 ± 6.7 | 59.6 ± 6.3 | 72.0 ± 7.4 | 70.8 ± 7.3 |
| Height (cm) | 167 ± 6 | 169 ± 6 | 178 ± 6 | 180 ± 6 |
| BMI (kg∙m−2) | 21.7 ± 1.6 | 20.8 ± 1.5 2 | 22.7 ± 2.2 | 21.8 ± 1.8 |
| Fat mass (%) | 27.1 ± 5.5 | 23.7 ± 4.4 2 | 15.9 ± 5.5 | 15.2 ± 4.7 |
| FFM (kg) | 45.0 ± 4.9 | 46.2 ± 4.9 | 61.3 ± 5.7 | 60.8 ± 7.2 |
| PAL 1 | 1.8 ± 0.2 | 2.1 ± 0.2 4 | 1.8 ± 0.3 | 1.9 ± 0.3 |
| RMR | ||||
| (kcal∙day−1) | 1505 ± 155 | 1457 ± 148 | 1873 ± 186 | 1824 ± 198 |
| (kcal∙kg−1·day−1) | 24.9 ± 1.9 | 24.5 ± 2.1 | 26.1 ± 1.8 | 25.9 ± 2.5 |
| (kcal∙kg−1∙h−1) | 1.04 ± 0.08 5 | 1.02 ± 0.09 | 1.09 ± 0.07 7 | 1.08 ± 0.10 6 |
| RMRpred (kcal∙kg−1∙h−1) | 0.98 ± 0.05 5 | 0.99 ± 0.05 | 1.03 ± 0.05 5 | 1.04 ± 0.04 7 |
| RQrest | 0.76 ± 0.04 | 0.76 ± 0.04 | 0.76 ± 0.06 | 0.75 ± 0.04 |
| VO2max | ||||
| (L·min−1) | 2.9 ± 0.4 | 3.3 ± 0.4 3 | 4.1 ± 0.5 | 4.5 ± 0.5 3 |
| (mL∙kg−1∙min−1) | 48.3 ± 5.1 | 55.3 ± 4.1 4 | 56.8 ± 5.7 | 64.1 ± 6.1 4 |
| Women | Men | |||
|---|---|---|---|---|
| CON (n = 29) | END (n = 28) | CON (n = 24) | END (n = 24) | |
| METmax_ind | 13.3 ± 0.9 2 | 15.5 ± 1.0 1 | 14.9 ± 0.8 3 | 16.9 ± 0.7 1,2 |
| METmax_fix | 13.8 ± 1.4 | 15.9 ± 1.2 1 | 16.3 ± 1.6 | 18.3 ± 1.8 1 |
| r value | 0.69 4 | 0.24 | 0.78 4 | 0.10 |
| MAE | 0.9 ± 0.8 | 1.0 ± 0.9 | 1.5 ± 0.9 | 1.9 ± 1.3 |
| MAPE (%) | 6.6 ± 6.2 | 6.8 ± 6.2 | 10.3 ± 5.9 | 11.3 ± 7.6 |
| SEE | 0.63 | 1.03 | 0.52 | 0.70 |
| Women | Men | |||
|---|---|---|---|---|
| CON (n = 29) | END (n = 28) | CON (n = 24) | END (n = 24) | |
| Light activity (e.g., sitting tasks, Code 11580, 1.5 METs) | ||||
| AEE_ind (kcal∙h−1) | 94 ± 10 | 91 ± 9 | 117 ± 12 | 114 ± 12 |
| AEE_fix (kcal∙h−1) | 91 ± 10 1 | 89 ± 10 | 108 ± 11 3 | 106 ± 11 2 |
| Mean difference AEE_ind—AEE_fix (kcal∙h−1) | 3 ± 7 | 2 ± 8 | 9 ± 8 | 8 ± 10 |
| AEE_pred (kcal∙h−1) | 89 ± 5 2 | 88 ± 5 1 | 110 ± 8 2 | 110 ± 8 2 |
| Mean difference AEE_ind—AEE_pred (kcal∙h−1) | 6 ± 7 | 3 ± 8 | 7 ± 8 | 4 ± 8 |
| Moderate activity (e.g., organizing room, Code 05125, 4.8 METs) | ||||
| AEE_ind (kcal∙h−1) | 301 ± 31 | 291 ± 30 | 375 ± 37 | 365 ± 40 |
| AEE_fix (kcal∙h−1) | 292 ± 32 1 | 286 ± 30 | 346 ± 36 3 | 340 ± 35 2 |
| Mean difference AEE_ind – AEE_fix (kcal∙h−1) | 10 ± 23 | 5 ± 24 | 29 ± 26 | 25 ± 33 |
| AEE_pred (kcal∙h−1) | 283 ± 16 2 | 281 ± 17 1 | 353 ± 26 2 | 352 ± 27 2 |
| Mean difference AEE_ind—AEE_pred (kcal∙h−1) | 18 ± 24 | 11 ± 24 | 22 ± 24 | 13 ± 27 |
| Vigorous activity (e.g., stair climbing, Code 17130, 8.0 METs) | ||||
| AEE_ind (kcal∙h−1) | 502 ± 52 | 486 ± 49 | 625 ± 62 | 608 ± 66 |
| AEE_fix (kcal∙h−1) | 486 ± 54 1 | 477 ± 51 | 576 ± 60 3 | 566 ± 58 2 |
| Mean difference AEE_ind—AEE_fix (kcal∙h−1) | 16 ± 38 | 9 ± 41 | 48 ± 43 | 42 ± 55 |
| AEE_pred (kcal∙h−1) | 472 ± 27 2 | 468 ± 29 1 | 589 ± 43 2 | 587 ± 44 2 |
| Mean difference AEE_ind—AEE_pred (kcal∙h−1) | 30 ± 39 | 18 ± 40 | 36 ± 41 | 21 ± 45 |
| Very vigorous activity (e.g., running 11 mph, Code 12130, 16 METs) | ||||
| AEE_ind (kcal∙h−1) | 1004 ± 103 | 971 ± 99 | 1249 ± 124 | 1216 ± 132 |
| AEE_fix (kcal∙h−1) | 972 ± 107 1 | 953 ± 101 | 1152 ± 119 3 | 1132 ± 117 2 |
| Mean difference AEE_ind—AEE_fix (kcal∙h−1) | 32 ± 75 | 18 ± 81 | 97 ± 85 | 84 ± 110 |
| AEE_pred (kcal∙h−1) | 944 ± 54 2 | 934 ± 57 1 | 1177 ± 85 2 | 1174 ± 89 2 |
| Mean difference AEE_ind—AEE_pred (kcal∙h−1) | 59 ± 78 | 36 ± 80 | 72 ± 81 | 42 ± 89 |
| Women | Men | |||
|---|---|---|---|---|
| CON (n = 29) | END (n = 28) | CON (n = 24) | END (n = 24) | |
| Sedentary or light activity lifestyle (PAL 1.53) | ||||
| TEE_ind (kcal∙day−1) | 2303 ± 237 | 2229 ± 226 | 2866 ± 285 | 2790 ± 303 |
| TEE_fix (kcal∙day−1) | 2230 ± 246 1 | 2188 ± 232 | 2645 ± 273 3 | 2598 ± 268 2 |
| Mean difference TEE_ind—TEE_fix (kcal∙day−1) | 73 ± 173 | 41 ± 186 | 222 ± 196 | 192 ± 253 |
| TEE_pred (kcal∙day−1) | 2167 ± 124 2 | 2146 ± 131 1 | 2702 ± 195 2 | 2694 ± 204 2 |
| Mean difference TEE_ind—TEEpred (kcal∙day−1) | 136 ± 180 | 83 ± 183 | 164 ± 186 | 96 ± 205 |
| Active or moderately active lifestyle (PAL 1.76) | ||||
| TEE_ind (kcal∙day−1) | 2649 ± 272 | 2564 ± 260 | 3297 ± 327 | 3210 ± 348 |
| TEE_fix (kcal∙day−1) | 2565 ± 283 1 | 2517 ± 267 | 3042 ± 314 3 | 2989 ± 308 2 |
| Mean difference TEE_ind—TEE_fix (kcal∙day−1) | 84 ± 199 | 47 ± 214 | 255 ± 225 | 221 ± 291 |
| TEE_pred (kcal∙day−1) | 2493 ± 143 2 | 2468 ± 151 1 | 3108 ± 224 2 | 3099 ± 234 2 |
| Mean difference TEE_ind—TEEpred (kcal∙day−1) | 157 ± 207 | 95 ± 211 | 189 ± 215 | 111 ± 236 |
| Vigorous or vigorous active lifestyle (PAL 2.25) | ||||
| TEE_ind (kcal∙day−1) | 3387 ± 348 | 3277 ± 332 | 4215 ± 418 | 4102 ± 445 |
| TEE_fix (kcal∙day−1) | 3279 ± 361 1 | 3217 ± 342 | 3889 ± 402 3 | 3821 ± 394 2 |
| Mean difference TEE_ind—TEE_fix (kcal∙day−1) | 108 ± 254 | 60 ± 273 | 326 ± 288 | 282 ± 372 |
| TEE_pred (kcal∙day−1) | 3186 ± 183 2 | 3156 ± 193 1 | 3974 ± 287 2 | 3962 ± 300 2 |
| Mean difference TEE_ind—TEEpred (kcal∙day−1) | 201 ± 265 | 122 ± 270 | 241 ± 274 | 141 ± 301 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Heydenreich, J.; Schutz, Y.; Melzer, K.; Kayser, B. Comparison of Conventional and Individualized 1-MET Values for Expressing Maximum Aerobic Metabolic Rate and Habitual Activity Related Energy Expenditure. Nutrients 2019, 11, 458. https://doi.org/10.3390/nu11020458
Heydenreich J, Schutz Y, Melzer K, Kayser B. Comparison of Conventional and Individualized 1-MET Values for Expressing Maximum Aerobic Metabolic Rate and Habitual Activity Related Energy Expenditure. Nutrients. 2019; 11(2):458. https://doi.org/10.3390/nu11020458
Chicago/Turabian StyleHeydenreich, Juliane, Yves Schutz, Katarina Melzer, and Bengt Kayser. 2019. "Comparison of Conventional and Individualized 1-MET Values for Expressing Maximum Aerobic Metabolic Rate and Habitual Activity Related Energy Expenditure" Nutrients 11, no. 2: 458. https://doi.org/10.3390/nu11020458
APA StyleHeydenreich, J., Schutz, Y., Melzer, K., & Kayser, B. (2019). Comparison of Conventional and Individualized 1-MET Values for Expressing Maximum Aerobic Metabolic Rate and Habitual Activity Related Energy Expenditure. Nutrients, 11(2), 458. https://doi.org/10.3390/nu11020458






