Positioning the Value of Dietary Carbohydrate, Carbohydrate Quality, Glycemic Index, and GI Labelling to the Canadian Consumer for Improving Dietary Patterns
Abstract
1. Introduction
2. Methods
2.1. Study Design
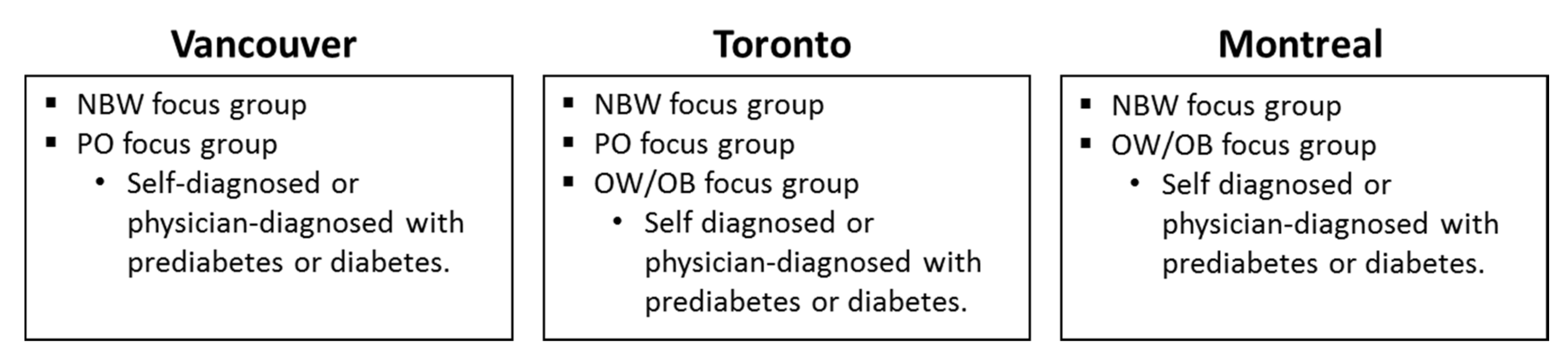
2.2. Focus Groups
3. Ethics
4. Results
4.1. Defining and General Perceptions of Dietary Carbohydrate
- ■
- “I don’t worry about carbs” (NBW, Vancouver)
- ■
- “I’ve never had a problem with carbs and weight gain. But as I get older I try to make my carbs count more.” (NBW, Vancouver)
- ■
- “It (carbohydrate) does give you energy. If I don’t have carbs I do feel light-headed.” (NBW, Vancouver)
- ■
- “Carbs are fundamental to the human diet. I don’t understand why, but they are required.” (NBW, Vancouver)
- ■
- “Carbs are probably my favourite foods to eat. Probably the tastiest” (NBW, Vancouver)
- ■
- “We need carbs. The good carbs those that are complex that are naturally occurring in the food. If I cut down too much it doesn’t work for me. But I want to avoid the white sugar, the refined sugar.” (NBW, Montreal)
- ■
- “If you don’t have health problems you will have less of a tendency to watch this closely” (NBW, Montreal)
- ■
- “Carbs and weight gain” (NBW, Vancouver)
- ■
- “I’ve tried to cut out bread intake to lose weight” (NBW, Toronto)
- ■
- “A lot of my friends are way healthier than I am. Gym buffs. That’s the first thing they tell me: Cut breads, pasta, and all that nonsense” (NBW, Toronto)
- ■
- “I’ve always associated it as an indulgence. Something that, if I eat too much, I will gain weight. It’s something that I feel like I’ve had to cut back on or not eat a lot of. Because I love it too much” (NBW, Vancouver)
- ■
- “Growing up, carbohydrates are the base of your diet... A lot of diet advice was low fat and fat is bad and use low fat diets to try to lose weight. Later on, you started to hear more information from research that having too much sugar in your diet and too many simple carbohydrates is a really bad thing. And you can have good fats and that is ok. It’s something where I originally had one idea about it (carbohydrate), but that has changed over the course of my life.” (NBW, Vancouver)
- ■
- “There is guilt associated with carbs even though we haven’t been properly educated that carbs are needed as part of a proper diet.” (NBW, Vancouver)
- ■
- “I like the carbs.” (PO, Vancouver)
- ■
- “Having bread and pasta with a group of friends is great.” (PO, Vancouver)
- ■
- “Comforting–especially if you are eating food that you were brought up eating. Then you are told you can’t do that anymore. Psychologically it is very frustrating. Especially if you get together with family and there is that wonderful and comforting feast. It’s an emotional connection. You justify it. It is a part of the celebration connecting with friends and family.” (PO, Vancouver)
- ■
- “Perception of carbs being bad” (PO, Vancouver)
- ■
- “I was told by doctor to stay away from all the ‘white’ stuff… those are carbs that convert into sugars.” (PO, Vancouver)
- ■
- “I was always taught that carbs make you gain weight.” (PO, Toronto)
- ■
- “I started eating healthier. Less fast food. I tried to cut down on breads and starches. For breakfast, I would just do an egg scramble and not eat the toast…” (PO, Toronto)
- ■
- “I never eat bread either. That is a big thing. Cutting out bread and pasta makes a huge difference” (PO, Toronto)
- ■
- “I went to Pinterest for a lot of recipes on how to lose weight, for meal plans that they suggest. They always said to cut out the carbs.” (PO, Toronto)
- ■
- “It is engrained in us that carbs are not really good, but you really do need them. I said satisfying because I feel great after eating them.” (PO, Vancouver)
- ■
- “Carbs are always looked upon as a bad thing. But then again, especially with athletes, you need the carbs. It’s not just athletes, everyone needs carbs. It’s that balance of good vs. bad.” (PO, Vancouver)
- ■
- “You can’t eat anything white. I love potatoes, I love rice, I love pasta. Potatoes and bread are the hardest things to get rid of.” (OW/OB, Toronto)
- ■
- “I cut out a lot of my carbs.” (OW/OB, Toronto)
- ■
- “We don’t have the choice” (OW/OB, Montreal)
- ■
- “I have frustration for pasta. I love pasta. I am not happy about that.” (OW/OB, Montreal)
4.2. Perceptions of Dietary Carbohydrate: Word Association
4.3. Familiarity with Carbohydrate Quality
- ■
- “No idea” (OW/OB, Toronto)
- ■
- “I don’t believe there is a quality of carbs.” (OW/OB, Toronto)
- ■
- “Oxymoron” (OW/OB, Toronto)
- ■
- “No such thing – sugar is sugar” (OW/OB, Toronto)
- ■
- “A carb is a carb” (OW/OB Montreal)
- ■
- “High in carbs but also high in fibre” (NBW, Vancouver)
- ■
- “I’ve never heard that term before. I assume it’s related to other nutritional value. I would be more interested in that. It feels more related to me.” (NBW, Vancouver)
- ■
- “Donut vs. oatmeal” (NBW, Toronto)
- ■
- “Fruits and vegetables are good quality” (NBW, Toronto)
- ■
- “Whole grains” (NBW, Toronto)
- ■
- “Difference between simple and complex carbs. The foods that contain the complex carbs will be better for your body.” (PO, Vancouver)
- ■
- “Complex carb—brown rice vs. white rice.” (PO, Toronto)
- ■
- “Sounds like good carb/bad carb.” (PO, Toronto)
- ■
- “Good carb? Anything bleached is bad—white rice, white pasta.” (PO, Toronto)
- ■
- “Whole wheat is better.” (PO, Toronto)
- ■
- “We are taught that whole wheat is better, but it’s not.” (PO, Toronto)
- ■
- “For me slow sugars would be good carbs, fast sugars would be bad carbs.” (OW/OB, Montreal)
- ■
- “Orange the fruit is good, the juice is bad.” (OW/OB, Montreal)
- ■
- “Everything that is slow is food that hasn’t been altered. Everything that is fast has been processed.” (OW/OB, Montreal)
4.4. Familiarity with the Glycemic Index
- ■
- “Anyone who is sick needs to be closely monitored. Anyone with a health concern” (NBW, Vancouver)
- ■
- “For diabetes” (NBW, Montreal)
- ■
- “Lists of different types of foods broken down into high sugars. Foods that have high sugar content vs. low. Gives me an indication as to which foods are better for me when it comes to low sugar and which are not as good for me because they have high sugar content.” (PO, Vancouver)
- ■
- “Glycemic index is negative” (PO, Toronto)
- ■
- “Associate with disease” (PO, Toronto)
- ■
- “A way to catch yourself” (OW/OB, Toronto)
- ■
- “You must follow this meal” (OW/OB, Toronto)
- ■
- “Announces bad news” (OW/OB, Montreal)
- ■
- “Sugar” (OW/OB Montreal)
4.5. Reaction to Educational Materials on the Glycemic Index
- ■
- “I liked reading this. Information was easy to digest. I am still curious about who is funding this but I also trusted it was science to a degree.” (NBW, Vancouver)
- ■
- “Made me understand everything else a little more.” (NBW, Vancouver)
- ■
- “As I’m shopping I’m not looking through all the information.” (NBW, Vancouver)
- ■
- “Easy to read” (NBW, Toronto)
- ■
- “Easy to understand” (NBW, Toronto)
- ■
- “Glycemic label would help me make better choices” (PO, Toronto)
- ■
- “Would be helpful for people to know I think, especially if diabetes runs in the family.” (PO, Toronto)
- ■
- “I really like this list. It tells you what’s good and what to not have as much of.” (OW/OB, Toronto)
- ■
- “Confirms what I knew (about the glycemic index) and makes me want to pay more attention to grocery shopping and the foods that I consume.” (NBW, Vancouver)
- ■
- “Talking about GI works. It’s easier to say ‘GI’ than carbohydrate quality.” (NBW, Vancouver)
- ■
- “In our minds, carbohydrates was the same as sugar. But even with sugar, we know there are good sugars and bad sugars. These sugar rich foods in general have a low glycemic index. In my mind it is still the same thing so this is strange. You have to define for me what carbohydrate is vs. what the glycemic index is. We know what the glycemic index is, but we don’t know what carbohydrates are.” (NBW, Montreal)
- ■
- “This is really good. The information about GI. Under grains—pasta and noodles, I thought they would be medium. It surprised me to see that they were low.” (PO, Vancouver)
- ■
- “I was surprised to see that the things we think are ‘healthy’ are ‘bad’.” (PO, Toronto)
- ■
- “Pasta is good” (PO, Toronto)
- ■
- “This is showing me I can have noodles and popcorn without feeling guilty - this whole thing is guilt ridden. I feel guilty for looking at a potato. Therefore, this is great and uplifting. It is a very dramatic thing to find out if you are diabetic.” (OW/OB, Toronto)
- ■
- “Surprised that foods that are high carb, low glycemic foods.” (OW/OB, Montreal)
- ■
- “Replace chart was good too” (NBW, Vancouver)
- ■
- “Don’t cut, just swap —something easier to do that can be maintained as a lifestyle.” (NBW, Toronto)
- ■
- “Being diagnosed and then given a lot of information can be confusing and overwhelming. What I found helpful with this was the reassurance that you don’t have to cut out everything, and just swap. That was a positive message to reassure you that you don’t have to give up your diet. So that is a positive message.” (PO, Vancouver)
- ■
- “Simple swaps” (OW/OB, Toronto)
- ■
- “I’m excited about the swap thing. I know what I am going to swap with. I love it.” (OW/OB, Toronto)
- ■
- “I don’t want to feel like I can’t have something. I like the idea of swaps.” (OW/OB, Toronto)
- ■
- “If I saw this I wouldn’t pick up the pamphlet because I don’t have diabetes.” (NBW, Toronto)
- ■
- “If it was Health Canada it would be more general than just diabetes.” (NBW, Montreal)
- ■
- “It’s not that it doesn’t seem reliable, it doesn’t seem like its targeted to me.” (NBW, Montreal)
- ■
- “The title is a medical term, the ‘glycemic index’, if it was in parentheses and you put a more general term, if I had seen ‘glycemic index’ I would think it is not for me.” (NBW, Montreal)
4.6. Reaction to Glycemic Index Labelling on Food Products
- ■
- “Low GI seal is on white rice, on white corn, and on honey. I would think of those as really processed white carbs. Honey is just sugar. That would make me doubt whether this seal is telling me something reputable or important. I would want to do more reading on what this seal meant.” (NBW, Vancouver)
- ■
- “I’m always skeptical. I always look anyways, even if there is something on the front of the box. It doesn’t mean it is a guarantee.” (NBW, Montreal)
- ■
- “If it’s a trusted foundation in Australia then that’s the most effective. I’m thinking if that was swapped for the CDA (Canadian Diabetes Association [Diabetes Canada]) then that would be effective for me because I trust CDA.” (PO, Vancouver)
- ■
- “Certified by an organization” (OW/OB, Montreal)
- ■
- “Connected to research that was done by researchers according to statistics” (OW/OB, Montreal)
- ■
- “There are so many foods with so many logos. They use this as marketing. Sometimes it’s true, sometimes it’s not.” (OW/OB, Montreal)
- ■
- “If there is an association certified by them, it would add credibility” (OW/OB, Montreal)
- ■
- “Approved according to what criteria?” (OW/OB, Montreal)
5. Discussion
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Webster, D.; Sollid, K. Is Everyone Really on a Low-Carbohydrate Diet? Consumer Perceptions of Carbohydrates and Sugars. Cereal Foods World 2018, 63, 116–118. [Google Scholar]
- Brouns, F.; Bjorck, I.; Frayn, K.N.; Gibbs, A.L.; Lang, V.; Slama, G.; Wolever, T.M. Glycaemic index methodology. Nutr. Res. Rev. 2005, 18, 145–171. [Google Scholar] [CrossRef] [PubMed]
- Augustin, L.S.; Kendall, C.W.; Jenkins, D.J.; Willett, W.C.; Astrup, A.; Barclay, A.W.; Bjorck, I.; Brand-Miller, J.C.; Brighenti, F.; Buyken, A.E.; et al. Glycemic index, glycemic load and glycemic response: An International Scientific Consensus Summit from the International Carbohydrate Quality Consortium (ICQC). NMCD 2015, 25, 795–815. [Google Scholar] [CrossRef] [PubMed]
- American Diabetes Association. 4. Lifestyle Management: Standards of Medical Care in Diabetes. Diabetes Care 2018, 41, S38–S50. [Google Scholar] [CrossRef] [PubMed]
- Sievenpiper, J.L.; Chan, C.B.; Dworatzek, P.D.; Freeze, C.; Williams, S.L. Nutrition Therapy. Can. J. Diabetes 2018, 42, S64–S79. [Google Scholar] [CrossRef] [PubMed]
- Barclay, A.W.; Petocz, P.; McMillan-Price, J.; Flood, V.M.; Prvan, T.; Mitchell, P.; Brand-Miller, J.C. Glycemic index, glycemic load, and chronic disease risk--a meta-analysis of observational studies. Am. J. clin. Nutr. 2008, 87, 627–637. [Google Scholar] [CrossRef] [PubMed]
- Government of Australia. Australia New Zealand Food Standards Code–Schedule 4–Nutrition, health and related claims–F2017C00711. Government of Australia. Available online: https://www.legislation.gov.au/Details/F2017C00711 (accessed on 5 October 2018).
- Government of Australia. Australia New Zealand Food Standards Code – Schedule 5 – Nutrient profiling scoring method -F2017C00719. Government of Australia. Available online: https://www.legislation.gov.au/Details/F2017C00719 (accessed on 5 October 2018).
- The Glycemic Index Foundation. The GI Symbol Program. The Glycemic Index Foundation. Available online: https://www.gisymbol.com/ (accessed on 4 October 2018).
- Dworatzek, P.D.; Arcudi, K.; Gougeon, R.; Husein, N.; Sievenpiper, J.L.; Williams, S.L. Nutrition Therapy. Can. J. Diabetes 2013, 37, S45–S55. [Google Scholar] [CrossRef] [PubMed]
- Statistics Canada. Education in Canada: Key results from the 2016 Census. Statistics Canada. Available online: https://www150.statcan.gc.ca/n1/en/daily-quotidien/171129/dq171129a-eng.pdf?st=X8-OKpTy (accessed on 12 February 2019).
- Marketing Research and intelligence Association. Standards: Code of condcut for members. Marketing Research and Intelligence Association. Available online: https://mria-arim.ca/standards/code-of-conduct-for-members (accessed on 18 December 2019).
- Tobias, D.K.; Chen, M.; Manson, J.E.; Ludwig, D.S.; Willett, W.; Hu, F.B. Effect of low-fat diet interventions versus other diet interventions on long-term weight change in adults: A systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2015, 3, 968–979. [Google Scholar] [CrossRef]
- Sartorius, K.; Sartorius, B.; Madiba, T.E.; Stefan, C. Does high-carbohydrate intake lead to increased risk of obesity? A systematic review and meta-analysis. BMJ Open 2018, 8, e018449. [Google Scholar] [CrossRef]
- Naude, C.E.; Schoonees, A.; Senekal, M.; Young, T.; Garner, P.; Volmink, J. Low carbohydrate versus isoenergetic balanced diets for reducing weight and cardiovascular risk: A systematic review and meta-analysis. PLoS ONE 2014, 9, e100652. [Google Scholar] [CrossRef]
- Buyken, A.E.; Goletzke, J.; Joslowski, G.; Felbick, A.; Cheng, G.; Herder, C.; Brand-Miller, J.C. Association between carbohydrate quality and inflammatory markers: Systematic review of observational and interventional studies. Am. J. Clin. Nutr. 2014, 99, 813–833. [Google Scholar] [CrossRef] [PubMed]
- Santiago, S.; Zazpe, I.; Bes-Rastrollo, M.; Sanchez-Tainta, A.; Sayon-Orea, C.; De la Fuente-Arrillaga, C.; Benito, S.; Martinez, J.A.; Martinez-Gonzalez, M.A. Carbohydrate quality, weight change and incident obesity in a Mediterranean cohort: The SUN Project. Eur. J. Clin. Nutr. 2015, 69, 297–302. [Google Scholar] [CrossRef] [PubMed]
- Zazpe, I.; Sanchez-Tainta, A.; Santiago, S.; De la Fuente-Arrillaga, C.; Bes-Rastrollo, M.; Martinez, J.A.; Martinez-Gonzalez, M.A. Association between dietary carbohydrate intake quality and micronutrient intake adequacy in a Mediterranean cohort: The SUN (Seguimiento Universidad de Navarra) Project. Br. J. Nutr. 2014, 111, 2000–2009. [Google Scholar] [CrossRef] [PubMed]
- Zazpe, I.; Santiago, S.; Gea, A.; Ruiz-Canela, M.; Carlos, S.; Bes-Rastrollo, M.; Martinez-Gonzalez, M.A. Association between a dietary carbohydrate index and cardiovascular disease in the SUN (Seguimiento Universidad de Navarra) Project. NMCD 2016, 26, 1048–1056. [Google Scholar] [CrossRef] [PubMed]
- International Life Science Institute–North America. Carb Quality Workshop 2017; ILSI North America, 2 February 2017. Available online: http://ilsi.org/event/carb-quality-workshop-2017/ (accessed on 21 September 2018).
- Oldways Whole Grains Council. Whole Grain Stamp. Oldways. Available online: https://wholegrainscouncil.org/whole-grain-stamp (accessed on 4 October 2018).
- Jenkins, D.J.; Kendall, C.W.; Augustin, L.S.; Vuksan, V. High-complex carbohydrate or lente carbohydrate foods? Am. J. Med. 2002, 113, 30S–37S. [Google Scholar] [CrossRef]
- Brand-Miller, J.; McMillan-Price, J.; Steinbeck, K.; Caterson, I. Carbohydrates-the good, the bad and the whole grain. Asia Pac. J. Clin. Nutr. 2008, 17, 16–19. [Google Scholar] [PubMed]
- Wolever, T.M. Is glycaemic index (GI) a valid measure of carbohydrate quality? Eur. J. clin. Nutr. 2013, 67, 522–531. [Google Scholar] [CrossRef]
- Brand-Miller, J.; Hayne, S.; Petocz, P.; Colagiuri, S. Low-glycemic index diets in the management of diabetes: A meta-analysis of randomized controlled trials. Diabetes Care 2003, 26, 2261–2267. [Google Scholar] [CrossRef]
- Gogebakan, O.; Kohl, A.; Osterhoff, M.A.; Van Baak, M.A.; Jebb, S.A.; Papadaki, A.; Martinez, J.A.; Handjieva-Darlenska, T.; Hlavaty, P.; Weickert, M.O.; et al. Effects of weight loss and long-term weight maintenance with diets varying in protein and glycemic index on cardiovascular risk factors: The diet, obesity, and genes (DiOGenes) study: A randomized, controlled trial. Circulation 2011, 124, 2829–2838. [Google Scholar] [CrossRef]
- Larsen, T.M.; Dalskov, S.M.; van Baak, M.; Jebb, S.A.; Papadaki, A.; Pfeiffer, A.F.; Martinez, J.A.; Handjieva-Darlenska, T.; Kunesova, M.; Pihlsgard, M.; et al. Diets with high or low protein content and glycemic index for weight-loss maintenance. N Engl. J. Med. 2010, 363, 2102–2113. [Google Scholar] [CrossRef]
- Ha, V.; Sievenpiper, J.L.; De Souza, R.J.; Jayalath, V.H.; Mirrahimi, A.; Agarwal, A.; Chiavaroli, L.; Mejia, S.B.; Sacks, F.M.; Di Buono, M.; et al. Effect of dietary pulse intake on established therapeutic lipid targets for cardiovascular risk reduction: A systematic review and meta-analysis of randomized controlled trials. CMAJ 2014, 186, E252–E262. [Google Scholar] [CrossRef] [PubMed]
- Jayalath, V.H.; De Souza, R.J.; Sievenpiper, J.L.; Ha, V.; Chiavaroli, L.; Mirrahimi, A.; Di Buono, M.; Bernstein, A.M.; Leiter, L.A.; Kris-Etherton, P.M.; et al. Effect of dietary pulses on blood pressure: A systematic review and meta-analysis of controlled feeding trials. Am. J. Hypertens. 2014, 27, 56–64. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.J.; De Souza, R.J.; Choo, V.L.; Ha, V.; Cozma, A.I.; Chiavaroli, L.; Mirrahimi, A.; Blanco Mejia, S.; Di Buono, M.; Bernstein, A.M.; et al. Effects of dietary pulse consumption on body weight: A systematic review and meta-analysis of randomized controlled trials. Am. J. Clin. Nutr. 2016, 103, 1213–1223. [Google Scholar] [CrossRef] [PubMed]
- Li, S.S.; Kendall, C.W.; De Souza, R.J.; Jayalath, V.H.; Cozma, A.I.; Ha, V.; Mirrahimi, A.; Chiavaroli, L.; Augustin, L.S.; Blanco Mejia, S.; et al. Dietary pulses, satiety and food intake: A systematic review and meta-analysis of acute feeding trials. Obesity (Silver Spring) 2014, 22, 1773–1780. [Google Scholar] [CrossRef] [PubMed]
- Sievenpiper, J.L.; Kendall, C.W.; Esfahani, A.; Wong, J.M.; Carleton, A.J.; Jiang, H.Y.; Bazinet, R.P.; Vidgen, E.; Jenkins, D.J. Effect of non-oil-seed pulses on glycaemic control: A systematic review and meta-analysis of randomised controlled experimental trials in people with and without diabetes. Diabetologia 2009, 52, 1479–1495. [Google Scholar] [CrossRef] [PubMed]
- Miller, V.; Mente, A.; Dehghan, M.; Rangarajan, S.; Zhang, X.; Swaminathan, S.; Dagenais, G.; Gupta, R.; Mohan, V.; Lear, S.; et al. Fruit, vegetable, and legume intake, and cardiovascular disease and deaths in 18 countries (PURE): A prospective cohort study. Lancet 2017, 390, 2037–2049. [Google Scholar] [CrossRef]
- Wang, X.; Ouyang, Y.; Liu, J.; Zhu, M.; Zhao, G.; Bao, W.; Hu, F.B. Fruit and vegetable consumption and mortality from all causes, cardiovascular disease, and cancer: Systematic review and dose-response meta-analysis of prospective cohort studies. BMJ 2014, 349, g4490. [Google Scholar] [CrossRef]
- Chiavaroli, L.; Kendall, C.W.C.; Braunstein, C.R.; Blanco Mejia, S.; Leiter, L.A.; Jenkins, D.J.A.; Sievenpiper, J.L. Effect of pasta in the context of low-glycaemic index dietary patterns on body weight and markers of adiposity: A systematic review and meta-analysis of randomised controlled trials in adults. BMJ Open 2018, 8, e019438. [Google Scholar] [CrossRef] [PubMed]
- Aziz, A.; Dumais, L.; Barber, J. Health Canada’s evaluation of the use of glycemic index claims on food labels. Am. J. Clin. Nutr. 2013, 98, 269–274. [Google Scholar] [CrossRef] [PubMed]
- Government of Canada. Technical Consultation on Health Canada’s Draft Guidance Document on Food Health Claims Related to Post-Prandial Glycaemia. Health Canada. Available online: https://www.canada.ca/en/health-canada/services/food-nutrition/public-involvement-partnerships/technical-consultation-draft-guidance-document-food-health-claims-related-post-prandial-glycaemia.html (accessed on 10 October 2018).
- International Carbohydrate Quality Consortium (ICQC); Jenkins, D.J.; Willett, W.C.; Astrup, A.; Augustin, L.S.; Baer-Sinnott, S.; Barclay, A.W.; Bjorck, I.; Brand-Miller, J.C.; Brighenti, F.; et al. Glycaemic index: Did Health Canada get it wrong? Position from the International Carbohydrate Quality Consortium (ICQC). Br. J. Nutr. 2014, 111, 380–382. [Google Scholar] [CrossRef] [PubMed]
- Wolever, T.M. Glycemic index claims on food labels: Review of Health Canada’s evaluation. Eur. J. Clin. Nutr. 2013, 67, 1229–1233. [Google Scholar] [CrossRef] [PubMed]
- International Organization for Standardization. ISO 26642:2010. Food products–Determination of the glycaemic index (GI) and recommendation for food classification. International Organization for Standardization. Available online: https://www.iso.org/standard/43633.html (accessed on 5 October 2018).
- The Glycemic Index Foundation. Product Eligibilility and Nutrient Criteria. The Glycemic Index Foundation. Available online: https://www.gisymbol.com/wp-content/uploads/2017/08/GI-Foundation-Product-Eligibility-and-Nutrient-Criteria-November-2015-2.pdf (accessed on 4 October 2018).
- Government of Canada. Health Claim Assessments. Health Canada. Available online: https://www.canada.ca/en/health-canada/services/food-nutrition/food-labelling/health-claims/assessments.html (accessed on 8 October 2018).
- Emrich, T.E.; Qi, Y.; Cohen, J.E.; Lou, W.Y.; L’Abbe, M.L. Front-of-pack symbols are not a reliable indicator of products with healthier nutrient profiles. Appetite 2015, 84, 148–153. [Google Scholar] [CrossRef] [PubMed]
| NBW Group (Vancouver, Toronto, Montreal) | PO Group (Vancouver, Toronto) | OW/OB Group (Montreal, Toronto) |
|---|---|---|
| Have always maintained a healthy body weight (BMI ≤ 24.9), Subjects not diagnosed with diabetes. | History of obesity (BMI ≥30), but have maintained a BMI ≤ 29.9 for at least two consecutive years at the time they were recruited for the study. Subjects with and without prediabetes or diabetes were recruited. Prediabetes or diabetes was self-diagnosed or diagnosed by a physician. | BMI ≥ 25.Subjects with prediabetes or diabetes were recruited. Prediabetes or diabetes was self-diagnosed or diagnosed by a physician. |
| Part 1: Exploration of Consumer Perspectives and Experiences Around Carbohydrate and Carbohydrate Quality. |
| What is a carbohydrate? |
| What does quality of carbohydrate mean? Are their criteria for carbohydrate quality? |
| Unprompted: explore ‘good’ versus ‘bad’ carbohydrates. |
| What makes a carbohydrate ‘good’ or ‘bad’? |
| How do subjects know if a carbohydrate is ‘good’ or ‘bad’? Where did they hear about the concepts of ‘good’ and ‘bad’ carbohydrates? [Probe for: whole food ingredients, ‘source of fibre’ and GI or glycemic response] |
| Activity: Word Association |
| Have subjects make a list of ‘good’ vs. ‘bad’ carbohydrate foods. |
| Discuss the functional health benefits of carbohydrate; beyond the notion of ‘good’ and ‘bad’. (Unprompted examples include energy, weight loss, less lethargic, and no crashing). |
| Part 2: Exploration of Consumer Perspectives and Experiences with the Glycemic Index |
| What is GI? |
| How did you learn about the GI? |
| What does low? Medium? High GI mean? |
| Are there any references to carbohydrate and the quality of carbohydrates GI? |
| What foods are associated with having a low, medium, or high GI? |
| What are subject’s current behaviors in seeking out low GI foods? |
| When are subject’s apt to seek out low GI Foods? Which eating occasions? |
| What are the trade-offs in making low GI food choices? |
| What benefits are subject’s seeking in their decision-making around GI? |
| Does low GI index relate to high carbohydrate quality? |
| Why is GI important to you? |
| What is ‘good’ or ‘bad’ about GI |
| What are subject’s current behaviors in seeking out low GI foods? |
| When are subject’s apt to seek out low GI Foods? Which eating occasions? |
| What are the trade-offs in making low GI food choices? |
| What benefits are subject’s seeking in their decision-making around GI? |
| Does low GI index relate to high carbohydrate quality? |
| Why is GI important to you? |
| What is ‘good’ or ‘bad’ about GI |
| What are the benefits associated with knowing the GI of a food over short term? And over the long term? |
| Explore expectations of the sensory experience around the different GI foods and low/high quality carbohydrates. |
| Does the sensory experience vary with the time of day and moments of consumption? |
| How does sensory and moments of consumption affect beliefs and behaviours around choosing low or high GI foods? |
| Activity: Introduce materials that discuss benefits of low GI foods (Figure S1). |
| How can GI be positioned as something that is ‘good for everyone’? |
| What attributes are the positive attributes of low GI foods? |
| Is there other language that consumers prefer to use when discussing GI or carbohydrate quality? |
| How are the concepts of GI and carbohydrate quality the same or different? |
| What will resonate most (GI or carbohydrate quality) with consumers? (Examples include blood sugar control, healthy carbohydrate, high fibre, low sugar). |
| Part 3: Discussion Pertaining to Low GI Labelling Concepts |
| Can a GI label or quality of carbohydrate label help shift beliefs and behaviours? |
| Specifically, does GI/GR or carbohydrate quality change opinions on food? |
| Activity: You will be assessing various concepts, ideas and labels that may appear online, on products and elsewhere. Evaluate and provide your own individual reactions to each concept, idea, and label ( Figure S2). |
| What do you personally resonate with most in this idea and/or logo and why? What is this concept communicating to you? |
| What do you find most compelling and why? What do you find least compelling and why? |
| On a personal level, how convincing is the concept/logo about using these products from a scale of 1 to 10, where 1 is not all and 10 is extremely convincing? |
| How important is having this logo on food products? Is it trustworthy and why? Credible? How is it persuasive to you? |
| Criteria | NBW Group | PO Group | OW/OB Group | Total | ||||
|---|---|---|---|---|---|---|---|---|
| Vancouver | Toronto | Montreal | Vancouver | Toronto | Toronto | Montreal | ||
| n | 7 | 7 | 6 | 7 | 7 | 7 | 6 | 47 |
| Gender (n) | ||||||||
| Male | 0 | 3 | 0 | 4 | 0 | 0 | 0 | 7 |
| Female | 7 | 4 | 6 | 3 | 7 | 7 | 6 | 40 |
| Age (n) | ||||||||
| 30–34 years | 4 * | 5 | 0 | 0 | 6 * | 0 | 0 | 15 |
| 35–40 years | 3 | 1 | 2 | 0 | 1 | 0 | 2 | 9 |
| 40–44 years | 0 | 1 | 3 | 1 | 0 | 1 | 2 | 8 |
| 45–49 years | 0 | 0 | 0 | 2 | 0 | 1 | 2 | 5 |
| 50–55 years | 0 | 0 | 1 | 4 | 0 | 5 * | 0 | 10 |
| Mean (SD) | 34.7 ± 3.9 | 33.4 ± 34.8 | 42 ± 7.0 | 49.3 ± 3.8 | 31.6 ± 4.2 | 53.9 ± 7.1 | 42.2 ± 5.0 | 41.0 ± 9.4 |
| Body weight (kg) (Mean ± SD) | 57.9 ± 10.4 | 64.2 ± 9.7 | 57.2 ± 6.5 | 72.9 ± 17.3 | 67.3 ± 6.5 | 86.3 ± 16.6 | 83.6 ± 20.5 | 69.9 ± 16.5 |
| BMI (Mean ± SD) | 21.3 ± 2.2 | 22.2 ± 1.9 | 21.9 ± 2.3 | 25.6 ± 3.2 | 23.3 ± 2.2 | 32.9 ± 5.2 | 31.0 ± 4.8 | 25.5 ± 5.3 |
| Waist circumference (inch) (Mean ± SD) | 27 ± 1.8 | 28.9 ± 3.7 | 29.2 ± 2.3 | 33.3 ± 3.9 | 29.9 ± 2.2 † | 38.1 ± 2.5 | 38.2 ± 7.0 | 32.0 ± 5.4 |
| Diabetes or prediabetes (Y/N) | N | N | N | Y | N | Y | Y | |
| Diagnosed | N/A | N/A | N/A | 4 | N/A | 7 | 2 | 13 |
| Non-diagnosed | N/A | N/A | N/A | 3 | N/A | 0 | 4 | 7 |
| Annual income (n) | ||||||||
| 50–59K | 0 | 1 | 1 | 2 | 3 | 2 | 3 * | 12 |
| 60–69K | 0 | 0 | 3 | 1 | 1 | 0 | 1 | 6 |
| 70–79K | 2 | 1 | 0 | 0 | 1 | 0 | 0 | 4 |
| 80–89K | 1 | 1 | 0 | 3 | 0 | 1 | 0 | 6 |
| 90–99K | 2 | 1 | 0 | 0 | 1 | 2 | 0 | 6 |
| > 100 K | 2 | 3 | 2 | 1 | 1 | 2 | 2 | 13 |
| Marital status | ||||||||
| Married/common law | 2 | 5 | 3 | 5 | 3 | 4 | 5 | 27 |
| Single/separated/divorced | 5 | 2 | 3 | 2 | 4 | 3 | 1 | 20 |
| Education | ||||||||
| Completed secondary | 1 | 0 | 3 | 2 | 3 | 2 | 1 | 12 |
| Completed post-secondary | 6 | 7 | 3 | 5 | 4 | 5 | 5 | 35 |
| Negative Word Association | Positive Word Association |
|---|---|
| NBW Group | |
| Vancouver: “bad”, “calories”, “overeating and feeling heavy”, “controversy”, “empty calories”, “weight gain” Toronto: “crashing”, “weight gain” Montreal: “calories”, “weight gain” | Vancouver: “craving and comfort food”, “gives you pleasure” Toronto: “tastes good, good feelings, cravings”, “bad carbs brings me back to happy memories”, “loving and warm”, “enjoyment now” Montreal: “energy”, “a boost that allows you to be awake”, “allows you to work” |
| PO Group | |
| Vancouver: “good and bad”, “weight gain”, “bad for you”, “confusion”, “negative because it raised my blood sugar”, “sluggish” Toronto: “fat”, “heavy”, “bad but good”, “guilty” | Vancouver: “thirst quenching”, “energy”, “athletes”, “bursts”, “sports” Toronto: “grandma”, “family”, “delicious”, “tradition”, “carbs are associated with our background and our culture”, “comfort food”, “filling”, “energy” |
| OW/OB Group | |
| Toronto: “wrong”, “compromised”, “hidden” Montreal: “diabetic coma” | Toronto: “a staple”, “comfort food”, “filling”, “tasty”, “soothing”, “socially acceptable”, “my mom’s house”, “grandma’s house”, “enjoyable”, “favourite food” Montreal: “gives you energy”, “something we find on labels” |
| NBW Group | PO Group | OW/OB Group |
|---|---|---|
Vancouver:
| Vancouver:
| Toronto:
|
Toronto
| Toronto
| |
Montreal
| Montreal
|
| Group | Positive Reactions | Negative Reactions |
|---|---|---|
| NBW Group | “I would pay attention to a low GI number because what I learned about it a low GI number was better for me.” (NBW, Vancouver) “To me that (GI) trumps carbs because we need carbs and the GI index is a way of saying whether it is a complex or simple carb. It is more of an indicator. To me, carb doesn’t tell me as much information.”(NBW, Vancouver) “Packaging is colourful and bright. Even if I didn’t know about GI, I would associate it with positive things” (NBW, Vancouver) “Must mean that it is under a certain level, whatever GI is. Obviously the lower the GI the better for you. I still don’t know what it means, but the lower the better” (NBW, Vancouver) “I like the idea” (NBW, Toronto) “I love it. Shows me what is good about this (food)” (NBW, Toronto) “I don’t have to cut carbs out” (NBW, Toronto) “Guide when I’m grocery shopping to make things easier and quicker” (NBW, Toronto) “It’s not just about eating protein” (NBW, Toronto) “Means that its certified, that it is low” (NBW, Montreal) “At the grocery store, if I knew what this was and I was informed, and I saw one loaf of bread with a stamp and one without. I would take the one with the stamp because then I know that it is low glycemic. But we are not diabetes, we just want to avoid it. We have to be informed ahead of time. If you know it will inform your choice” (NBW, Montreal) “I think it would be a good thing. It would make things easier” (NBW, Montreal) “It allows to make better choices” (NBW, Montreal) “It has to come with information. If I hadn’t seen it on TV before or somewhere, it would say nothing to me. There has to be a campaign” (NBW, Montreal) “With a foundation, it would be better” (NBW, Montreal) “Certified is stronger in my mind” (NBW, Montreal) | “No because I don’t know enough about it” (NBW, Vancouver) “It’s not something to worry about. I’ve never noticed any bad health effects from eating one or the other” (NBW, Vancouver) “We generally know the difference between good and bad food, but we don’t categorize that as high GI or low GI.” (NBW, Vancouver) “If I had a weight problem, I think I would be researching it more” (NBW, Vancouver) “If I saw it I probably wouldn’t pay attention because, to me, it would still be a calorie and fat. The only way I would be if the store had a marketing campaign and tell me why I need to know this” (NBW, Vancouver) “Doesn’t do anything for me because I’m uneducated on what GI means” (NBW, Vancouver) |
| PO Group | “This is for overall health” (PO, Toronto) “Easy to explain” (PO, Toronto) “Grabs your attention” (PO, Toronto) “Stamp means it’s healthier for you” (PO, Toronto) “I would look at the logo and associate it with a “good thing” (PO, Toronto) “Certified makes it look like it’s a good thing” (PO, Toronto) “Use QR codes or website to provide information on what low GI is” (PO, Toronto) | “Gimmicky. Having that in front of me doesn’t change anything. Honey has a low GI thing and it’s sugar” (PO, Vancouver) “ “Certified and foundation” sound too much like a phrase or trying to hard” (PO, Vancouver) “I don’t like the wording, I don’t trust it. I don’t know what they are” (PO, Vancouver) “A glycemic index label means nothing at this point” (PO, Toronto) |
| OW/OB Group | “Would be good, would be easy, nobody has time to read all the labels” (OW/OB, Toronto) “Inform me so I can make the right decisions” (OW/OB, Toronto) “You can eat healthy, here are the options” (OW/OB, Toronto) “It’s fine. I would definitely pick one over the other if I see that” (OW/OB, Toronto) “Makes grocery shopping easier” (OW/OB, Toronto) “I like knowing what I’m supposed to buy” (OW/OB, Toronto) “Help you figure it out” (OW/OB, Toronto) “There is food that I can eat and don’t need to go all over the place to figure it out” (OW/OB, Toronto) | “I don’t trust it which foundation authorizes it—they lie all the time” (OW/OB, Toronto) “Don’t say it’s certified” (OW/OB, Toronto) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marinangeli, C.P.F.; Castellano, J.; Torrance, P.; Lewis, J.; Gall Casey, C.; Tanuta, J.; Curran, J.; Harding, S.V.; Jenkins, D.J.A.; Sievenpiper, J.L. Positioning the Value of Dietary Carbohydrate, Carbohydrate Quality, Glycemic Index, and GI Labelling to the Canadian Consumer for Improving Dietary Patterns. Nutrients 2019, 11, 457. https://doi.org/10.3390/nu11020457
Marinangeli CPF, Castellano J, Torrance P, Lewis J, Gall Casey C, Tanuta J, Curran J, Harding SV, Jenkins DJA, Sievenpiper JL. Positioning the Value of Dietary Carbohydrate, Carbohydrate Quality, Glycemic Index, and GI Labelling to the Canadian Consumer for Improving Dietary Patterns. Nutrients. 2019; 11(2):457. https://doi.org/10.3390/nu11020457
Chicago/Turabian StyleMarinangeli, Christopher P. F., Joanna Castellano, Peg Torrance, Joanne Lewis, Carolyn Gall Casey, Jackie Tanuta, Julianne Curran, Scott V. Harding, David J. A. Jenkins, and John L. Sievenpiper. 2019. "Positioning the Value of Dietary Carbohydrate, Carbohydrate Quality, Glycemic Index, and GI Labelling to the Canadian Consumer for Improving Dietary Patterns" Nutrients 11, no. 2: 457. https://doi.org/10.3390/nu11020457
APA StyleMarinangeli, C. P. F., Castellano, J., Torrance, P., Lewis, J., Gall Casey, C., Tanuta, J., Curran, J., Harding, S. V., Jenkins, D. J. A., & Sievenpiper, J. L. (2019). Positioning the Value of Dietary Carbohydrate, Carbohydrate Quality, Glycemic Index, and GI Labelling to the Canadian Consumer for Improving Dietary Patterns. Nutrients, 11(2), 457. https://doi.org/10.3390/nu11020457






