Abstract
Nutritional management is an important component of the treatment of pediatric overweight and obesity, but clinicians struggle to keep abreast with the abundant literature. Therefore, our aim is to provide a tool that integrates the current recommendations and clinical expertise to assist dietitians and other practitioners in their decision making about the nutritional management of pediatric overweight and obesity. To construct this practice-based evidence-informed framework, we conducted a systematic review of the guidelines on nutritional management of pediatric overweight or obesity in 2 databases and in the grey literature. We analyzed and synthesized recommendations of 17 guidelines. We selected the recommendations that were common to at least 30% of the guidelines and added by consensus the recommendations relevant to clinical expertise. Finally, we structured the framework according to the Nutritional Care Process in collaboration with a specialized team of dietitians who assessed its validity in clinical practice. The framework contributes to facilitate the integration of evidence-based practice for dietitians by synthesizing the current evidence, supporting clinical expertise, and promoting structured care following Nutrition Care Process model for children and adolescents with obesity.
1. Introduction
Obesity in children and adolescents reaches alarming rates and the World Obesity Federation and the World Health Organization are calling to action in order to reduce the prevalence of pediatric obesity and its many associated physical, psychological, and social consequences [1]. Risk factors for obesity in children and adolescents are numerous and interact with a high level of complexity. Therefore, treatments integrating multiple targets at various levels are deemed the most effective for weight management: i.e., lifestyle interventions including diet, physical activity and behavior changes, and, for patients under 12 years old, targeting the whole family [2,3,4,5,6,7]. Qualified dietitians can contribute effectively to this complex task by providing their expertise on nutritional assessment, diagnosis, intervention and evaluation [8]. In adults, a meta-analysis including 69 studies concluded that dietitian-delivered lifestyle interventions achieve greater relative weight loss, compared to non-dietitian-lead interventions [9].
To provide effective care, dietitians adhere to evidence-based practice (EBP) that is about, according to the International Confederation of Dietetic Associations, “asking questions, systematically finding research evidence, and assessing the validity, applicability and importance of that evidence. This evidence-based information is then combined with the dietitian’s expertise and judgment and the client’s or community’s unique values and circumstances to guide decision-making in dietetics” [10]. Regarding research evidence in obesity treatment, the scientific societies, professional associations and expert groups have issued practice guidelines. These are aimed to “offer coherently sequenced recommendations based on the best available evidence aimed at everyday decision-making situations” [11] and should be “informed by a systematic review of evidence and an assessment of the benefits and harm of alternative care options“ [12]. However, the highest level of evidence (randomized controlled trial) is rarely available in the field of pediatrics, and even less so in dietetics and nutrition where multifaceted interventions are difficult (if not unethical) to standardize in a controlled fashion [13]. In such circumstances, professional expertise is more than crucial in everyday decision-making situations.
With the number of clinical guidelines expanding rapidly, practitioners struggle to stay abreast. Time is often cited as a major barrier for integrating research into practice [14,15] and synthesizing guidelines into a practical tool supporting the clinicians’ decision-making during their interaction with their patients would be helpful. Furthermore, the importance of adapting knowledge to the context is now recognized to support evidence implementation and has been described as an essential step in knowledge translation [16,17,18].
With a focus on EBP, the Academy of Nutrition and Dietetic has developed the Nutritional Care Process (NCP), a systematic approach contributing to high quality nutrition care. This approach helps dietitians structuring their actions in four distinct but interrelated steps: nutrition assessment, diagnosis, intervention and monitoring/evaluation [19,20]. In order to assist the dietitians, but also the other practitioners involved in pediatric weight management to apply these principles, we propose a practice-based evidence-informed framework modeled on the NCP. The aim of this paper is to describe the development of this tool and in particular to: (1) provide a review of the evidence on the dietary and nutritional management of pediatric overweight and obesity, (2) synthesize these evidences into recommendations fitting the NCP-model and (3) propose a framework, drawn from the literature, adapted and expended with professional expertise, for the nutritional management of pediatric obesity. This tool leaves room for individual adaptations based on the professionals’ expertise and the patient’s unique circumstances.
2. Materials and Methods
2.1. Evidence Selection, Extraction and Analysis
We conducted a systematic literature review of the literature reviews and guidelines on nutritional management of pediatric overweight or obesity in two databases commonly used in healthcare (PubMed and Cochrane Library). In order to improve exhaustiveness, and specifically to avoid missing guidelines emanating from expert groups that have not been published in peer reviewed journals, grey literature was also included. The research equations are detailed in Table 1. The same inclusion and exclusion criteria were applied for reviews and guidelines. Inclusion criteria were: pediatric population (<18 years old), medical guidelines including nutritional management of overweight and obesity, reviews describing a nutritional intervention or treatment, publication date ranging between 2007 and 2017, in French, English or Italian. Exclusion criteria were: papers describing only nutritional prevention or health promotion interventions, focusing on specific ethnicity or gender, with no focus on practical aspects of nutritional intervention, or treating exclusively severe obesity. Two members of the team independently selected the reviews and guidelines, first on the adequacy of the title, then on the abstract and finally on the full-text. At each step, any disagreement was discussed until consensus was reached and a third author was consulted in case of doubt.

Table 1.
Databases and research equations for the systematic review of guidelines on nutritional management of pediatric overweight or obesity.
An evaluation of the methodological quality of the guidelines was conducted using a simplified grid inspired by the AGREE tool [21] assessing 5 domains (scope and purpose, rigor of development, clarity of presentation, applicability, editorial independence).
Two members of the team independently extracted the recommendations regarding the nutritional management of pediatric overweight and obesity from the 17 included guidelines. The recommendations were isolated, categorized by theme and organized following the 4 steps of Nutritional Care Process (NCP).
2.2. Development of the Structured Framework
In a first step, recommendations that were present in at least 30% of the guidelines were used to construct a preliminary framework. Because we could not find previous work publishing on the cut-off point, we chose 30% based on the descriptive analysis of our data. This allowed a selection of a large panel of recommendations. In a second step, the members (n = 9) of a specialized group for the prevention and treatment of pediatric obesity recognized by the Swiss Association of Registered Dietitians reviewed the preliminary framework, as well as the table listing all individual recommendations emerging from the guidelines. Based on their clinical expertise, recommendations that are regularly used in clinical practice were identified among the individual recommendations from the guidelines. Even if those recommendations were not mentioned in at least 30% of the guidelines, they were included in the framework while distinctly labeled.
2.3. Usability Evaluation
For this third step, in order to verify if the guideline was usable, it was tested by a dietician who was chosen because of her high expertise in the clinical field, her familiarity with the process of guidelines creation and her willingness to participate in the project. This experienced registered dietitian, who did not participate in the second step, selected four cases of children with obesity treated in her practice for an anonymous retrospective case study. Each treatment plan including several consultations was broken down into isolated steps. Nutrition assessment and interventions performed by the dietitian were identified from the patients’ records and compared with the framework. Finally, a semi-structured qualitative interview based on thirteen questions (detailed in Table S1) was conducted with the dietitian in order to assess the suitability of the framework into clinical practice.
3. Results
3.1. Evidence Selection
The initial search on PubMed resulted in 115 articles and 4 articles were included after selection. The search on Cochrane identified 3 reviews that did not meet the inclusion criteria. Finally, 16 guidelines were found in the grey literature, of which 3 had been identified through PubMed.
Ultimately, no reviews met the inclusion criteria and we included 17 guidelines, issued by 14 different scientific societies (in alphabetical order: Academy of Nutrition and Dietetics (n = 3 in 2007, 2013 and 2015) [22,23,24], American Academy of Pediatrics [8], Canadian Medical Association [25], Endocrine Society [26], European Association for the Study of Obesity [27], Haute Autorité de Santé [28], Institute for Clinical Systems Improvement [29], Institute for Healthy Childhood Weight [2], Institut National d’Excellence en Santé et Services sociaux [30], National Health and Medical Research Council [31], National Institute for Health and Care Excellence [32], New Zealand Ministry of Health (n = 2 in 2009 and 2016) [33,34], Scottish Intercollegiate Guidelines Network [35], Società Italiana di Pediatria and Società Italiana di Endocrinologia e Diabetologia Pediatrica [36].
3.2. Guidelines Extraction and Analysis
Most guidelines had a good methodological quality. Shortcomings related to the presentation of the methodology used to search and select the evidence. The detail of the evaluation is presented in Supplementary Table S2.
In total, 344 recommendations were extracted, from which 36 (10%) were present in at least half of the guidelines, and 57 (17%) in at least 30% of the guidelines. A summary of the recommendations classified by theme is presented in Table 2. The detail of these recommendations is presented in Supplementary Table S3.

Table 2.
Recommendations regarding nutritional assessment, diagnosis, intervention and monitoring and evaluation, frequency of citation and references of the 17 included guidelines.
The items related to general recommendations of treatment were similar across all guidelines, while precise recommendations were less common. The levels of evidence reported in the guidelines were mostly low and the recommendations were often based on expert consensus. A comparison of the different levels of evidence across guidelines was impossible because each guideline had a different grading scale. All guidelines considered the treatment of both pediatric overweight and obesity.
3.3. Development of the Structured Framework
The final framework (Figure 1) includes a total of 145 recommendations out of 344 identified in the 17 included guidelines. In the first step of development, we identified 57 recommendations common to at least 30% of the analyzed guidelines. In a second step, based on their clinical expertise, a group of specialized dietitians identified 88 additional recommendations from the guidelines that they regularly used in their practice but that were present in less than 30% of the guidelines. Those 88 recommendations were added to the framework and distinctly labeled. The framework follows the NCP 4-steps structure. We synthesized recommendations and included age groups when possible in the framework. Given that no guideline proposed nutrition diagnoses, we included six of them (in collaboration with the team of specialized dietitians) from the International Dietetics and Nutrition Terminology (IDNT) [37].
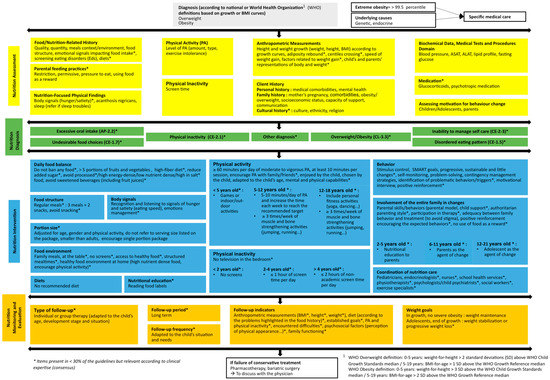
Figure 1.
Structured framework on the nutritional management of overweight and obesity in children and adolescents.
3.4. Usability Evaluation
The retrospective analysis of four cases revealed that the framework was complete, usable and coherent with clinical practice. Each nutrition intervention retrieved from the 4 patients’ records was already present in the framework and no new recommendation had to be added. The interviewed dietitian highlighted that the framework was helpful to structure the dietetic treatment while leaving enough liberty to adjust the treatment modality to the patient. She used the framework as a checklist to make sure that she did not miss any component. She emphasized that clinical expertise was essential to apply the framework effectively. Also, the framework was perceived as a communication tool that highlights the evidence supporting her practice to external stakeholders.
4. Discussion
Dietitians have an essential role in the treatment of obesity among children and adolescents. In this project, we identified the most common recommendations for nutritional management of pediatric overweight and obesity from guidelines and clinical expertise and organized them according to the NCP-model in order to propose a framework assisting expert decision-making.
Our analysis of current guidelines revealed a commonality of many general principles for the dietary and nutritional management of pediatric overweight and obesity, but also a lack of research on specific detailed questions related to everyday practice, such as age-based nutritional intervention or follow-up. While more research on nutrition interventions is necessary, it has to be recognized that this is also very challenging, because food-based or public health interventions involve too many components interacting in complex pathways [4,13]. Dietitians also often collaborate with other health care professionals in multidisciplinary, multi-model interventions. It is therefore almost impossible to isolate the impact of the sole nutritional care [39]. Pragmatic trials are an example of a new trend toward studies designed to inform practice and show real-world effectiveness of interventions [40]. Dietitians are uniquely and favorably positioned to participate in research projects using feasible and appropriate research designs to answer specific and practical questions.
Most of the included guidelines targeted medical treatment of pediatric overweight and obesity, resulting in few details of the nutritional management. Only 17% of the recommendations were commonly to 30% or more of the guidelines. The expertise of clinical dietitians seems essential to apply the framework with specific, pragmatic, and detailed advice. Since no guideline indicated durations of the first or following visits, the dietitians will have to adapt the content to their time constraints and the individual possibilities of their patients. In fact, the adaptation of knowledge to local context, or to dietetic practice in this case, is part of the steps of knowledge transfer process [18,41]. Of course, this step might represent a limitation of the tool as it introduces non-evidence-based recommendations, even if those are clearly labeled as such. This tool does not claim to be definitive. Indeed, it will have to be modified and enhanced after a period of field-testing that will enlarge the preliminary usability evaluation carried out by only one specialized dietitian. We also acknowledge that fact that we did not assess the methodological quality of the guidelines included in our analysis; therefore, recommendations from guidelines of variable methodological quality have the same weight in the framework. Lastly, the selection of guidelines was limited to the three languages mastered by our team what could lead to a selection bias.
Nevertheless, the strength of this paper is to provide a framework synthesizing the current literature based on a systematic analysis of each guideline, the extraction of each single recommendation and the expertise from clinical professionals. Our framework is coherent with the NCP and reinforces the use of this structured four-steps process to promote high quality of dietetics and nutrition care. Finally, the retrospective validity assessment demonstrated the relationship between the framework and the clinical practice and suggested a high potential of use by clinical dietitians.
5. Conclusions
This paper synthesizes the current recommendations on nutritional management of pediatric overweight and obesity with the expertise from experienced dietitians in an attempt to create a tool aiming to facilitate the integration of EBP for dietitians and to promote structured care following NCP-model.
Supplementary Materials
The following are available online at https://www.mdpi.com/2072-6643/11/2/362/s1, Table S1: Semi-structured questionnaire evaluating the usability of the framework in practice, Table S2: Quality assessment of guidelines included in the framework, Table S3: Detailed recommendations regarding nutritional assessment, diagnosis, intervention and monitoring and evaluation, frequency of citation and references of the guidelines.
Author Contributions
Conceptualization, analysis and synthesis of data: S.P., F.P. and S.B.D.T.; writing and revision: S.P., F.P.; S.B.D.T. and M.K.; L.S. participated to the interpretation of data and revised the manuscript critically with intellectual contribution, C.P. and M.V. were involved in the validation process and review the manuscript.
Funding
This research received no external funding. The APC was funded by HES-SO Genève.
Acknowledgments
The authors thank the specialized team of dietitians “POET” from the Swiss Association of Registered Dietitians for their involvement in the initiation and the validation of the framework. They also thank the dietitians from the CHU of Toulouse for their exchange of practices.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Taking Action on Childhool Obesity; World Health Organization. Available online: https://www.who.int/end-childhood-obesity/publications/taking-action-childhood-obesity-report/en/ (accessed on 8 February 2019).
- Altman, M.; Wilfley, D.E. Evidence Update on the Treatment of Overweight and Obesity in Children and Adolescents. J. Clin. Child Adolesc. Psychol. 2014, 44, 521–537. [Google Scholar] [CrossRef] [PubMed]
- Colquitt, J.L.; Loveman, E.; O’Malley, C.; Azevedo, L.B.; Mead, E.; Al-Khudairy, L.; Ells, L.J.; Metzendorf, M.-I.; Rees, K. Diet, physical activity, and behavioural interventions for the treatment of overweight or obesity in preschool children up to the age of 6 years. Cochrane Database Syst. Rev. 2016, 3. [Google Scholar] [CrossRef]
- Mead, E.; Brown, T.; Azevedo, L.B.; Whittaker, V.; Jones, D.; Olajide, J.; Mainardi, G.M.; Corpeleijn, E.; O’Malley, C.; Beardsmore, E.; et al. Diet, physical activity and behavioural interventions for the treatment of overweight or obese children from the age of 6 to 11 years. Cochrane Database Syst. Rev. 2017, 6. [Google Scholar] [CrossRef] [PubMed]
- Al-Khudairy, L.; Loveman, E.; Colquitt, J.L.; Mead, E.; Johnson, R.E.; Fraser, H.; Olajide, J.; Murphy, M.; Velho, R.M.; O’Malley, C.; et al. Diet, physical activity and behavioural interventions for the treatment of overweight or obese adolescents aged 12 to 17 years. Cochrane Database Syst. Rev. 2017, 6. [Google Scholar] [CrossRef] [PubMed]
- Coppock, J.H.; Ridolfi, D.R.; Hayes, J.F.; Paul, M.S.; Wilfley, D.E. Current Approaches to the Management of Pediatric Overweight and Obesity. Curr. Treat. Options Cardio. Med. 2014, 16, 343. [Google Scholar] [CrossRef] [PubMed]
- Ho, M.; Garnett, S.P.; Baur, L.; Burrows, T.; Stewart, L.; Neve, M.; Collins, C. Effectiveness of Lifestyle Interventions in Child Obesity: Systematic Review With Meta-analysis. Pediatrics 2012, 130, e1647–e1671. [Google Scholar] [CrossRef]
- Barlow, S.E.; Ervin, C.; Ludwig, D.S.; Saelens, B.E.; Schetzina, K.E.; Taveras, E.M.; Spear, B.A. Recommendations for Treatment of Child and Adolescent Overweight and Obesity. Pediatrics 2007, 120, 254. [Google Scholar] [CrossRef]
- Sun, Y.; You, W.; Almeida, F.; Estabrooks, P.; Davy, B. The Effectiveness and Cost of Lifestyle Interventions Including Nutrition Education for Diabetes Prevention: A Systematic Review and Meta-Analysis. J. Acad. Nutr. Diet. 2017, 117, 404–421. [Google Scholar] [CrossRef]
- Final Report of the International Confederation of Dietetic Associations (ICDA) Evidence-based Practice Working Group. Available online: https://www.internationaldietetics.org/Downloads/ICDA-Report-Evidence-based-Dietetics-Practice-2010.aspx (accessed on 8 February 2019).
- Timmermans, S.; Mauck, A. The Promises And Pitfalls Of Evidence-Based Medicine. Health Affairs 2005, 24, 18–28. [Google Scholar] [CrossRef]
- Institute of Medicine (US) Committee on Standards for Developing Trustworthy Clinical Practice Guidelines. Clinical Practice Guidelines We Can Trust; National Academies Press (US): Washington, DC, USA, 2011.
- Blumberg, J.; Heaney, R.P.; Huncharek, M.; Scholl, T.; Stampfer, M.; Vieth, R.; Weaver, C.M.; Zeisel, S.H. Evidence-based criteria in the nutritional context. Nutr. Rev. 2010, 68, 478–484. [Google Scholar] [CrossRef]
- Byham-Gray, L.D.; Gilbride, J.A.; Dixon, L.B.; Stage, F.K. Evidence-Based Practice: What Are Dietitians’ Perceptions, Attitudes, and Knowledge? J. Am. Diet. Assoc. 2005, 105, 1574–1581. [Google Scholar] [CrossRef] [PubMed]
- Thomas, D.E.; Kukuruzovic, R.; Martino, B.; Chauhan, S.S.; Elliott, E.J. Knowledge and use of evidence-based nutrition: a survey of paediatric dietitians. J. Hum. Nutr. Diet. 2003, 16, 315–322. [Google Scholar] [CrossRef] [PubMed]
- Toman, C.; Harrison, M.B.; Logan, J. Clinical practice guidelines: necessary but not sufficient for evidence-based patient education and counseling. Patient Educ. Couns. 2001, 42, 279–287. [Google Scholar] [CrossRef]
- Légaré, F.; Fervers, B.; Harrison, M.B.; Graham, I.D. Adapting clinical practice guidelines to local context and assessing barriers to their use. CMAJ 2009, 182, E78–E84. [Google Scholar]
- Harrison, M.B.; Graham, I.D.; Fervers, B.; Hoek, J.V.D. Adapting knowledge to local context. In Knowledge Translation in Health Care; Wiley: Hoboken, NJ, USA, 2013; pp. 110–120. [Google Scholar]
- Writing Group of the Nutrition Care Process/Standardized Language Committee. Nutrition care process and model part I: the 2008 update. J. Am. Diet. Assoc. 2008, 108, 1113–1117. [Google Scholar] [CrossRef] [PubMed]
- Writing Group of the Nutrition Care Process/Standardized Language Committee. Nutrition care process part II: using the International Dietetics and Nutrition Terminology to document the nutrition care process. J. Am. Diet. Assoc. 2008, 108, 1287–1293. [Google Scholar] [CrossRef] [PubMed]
- Brouwers, M.; Kho, M.; Browman, G.; Burgers, J.; Cluzeau, F.; Feder, G.; Fervers, B.; Graham, I.D.; Grimshaw, J.; Hanna, S.E.; et al. AGREE II: Advancing guideline development, reporting and evaluation in healthcare. CMAJ 2010, 182, E839–E842. [Google Scholar] [CrossRef] [PubMed]
- Academy of Nutrition and Dietetics. Pediatric Weight Management. Major recommendations (2007). Available online: https://www.andeal.org/vault/pq57.pdf (accessed on 10 December 2018).
- Academy of Nutrition and Dietetics. Pediatric Weight Management. Major recommendations (2015). Available online: https://www.andeal.org/vault/pq140.pdf (accessed on 10 December 2018).
- Hoelscher, D.M.; Kirk, S.; Ritchie, L.; Cunningham-Sabo, L.; Academy Positions Committee. Position of the Academy of Nutrition and Dietetics: Interventions for the Prevention and Treatment of Pediatric Overweight and Obesity. J. Acad. Nutr. Diet. 2013, 113, 1375–1394. [Google Scholar] [CrossRef]
- Lau, D.C.; Douketis, J.D.; Morrison, K.M.; Hramiak, I.M.; Sharma, A.M.; Ur, E.; Obesity Canada Clinical Practice Guidelines Expert Panel. 2006 Canadian clinical practice guidelines on the management and prevention of obesity in adults and children [summary]. CMAJ 2007, 176, S1–S13. [Google Scholar] [CrossRef]
- Styne, D.M.; Arslanian, S.A.; Connor, E.L.; Farooqi, I.S.; Murad, M.H.; Silverstein, J.H.; Yanovski, J.A. Pediatric Obesity—Assessment, Treatment, and Prevention: An Endocrine Society Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 2017, 102, 709–757. [Google Scholar] [CrossRef]
- Baker, J.L.; Farpour-Lambert, N.J.; Nowicka, P.; Pietrobelli, A.; Weiss, R. Evaluation of the Overweight/Obese Child—Practical Tips for the Primary Health Care Provider: Recommendations from the Childhood Obesity Task Force of the European Association for the Study of Obesity. Obes. Facts 2010, 3, 5. [Google Scholar] [CrossRef]
- Haute Autorité de Santé. Surpoids et obésité de l’enfant et de l’adolescent. Available online: https://www.has-sante.fr/portail/jcms/c_964941/fr/surpoids-et-obesite-de-l-enfant-et-de-l-adolescent-actualisation-des-recommandations-2003 (accessed on 22 December 2018).
- Institute for Clinical Systems Improvement. Prevention and Management of Obesity for Children and Adolescents. 2013. Available online: https://www.ohcoop.org/wp-content/uploads/Clinical-Guidelines-Prevention-and-Management-Obesity-in-Children-and-Adolscent.pdf (accessed on 8 February 2019).
- Institut national d’excellence en santé et en services sociaux. Traitement de l’obésité des enfants et des adolescents en 1re et 2e ligne: guide de pratique clinique. Volet I; INESSS: Montreal, QC, Canada, 2012. [Google Scholar]
- Turner, L.R.; Harris, M.F.; Mazza, D. Obesity management in general practice: does current practice match guideline recommendations? Med. J. Aust. 2015, 202, 370–372. [Google Scholar] [CrossRef] [PubMed]
- National Institute for Health Care Excellence. Obesity: Identification, assessment and management. Available online: https://www.nice.org.uk/guidance/cg189/resources/obesity-identification-assessment-and-management-pdf-35109821097925 (accessed on 22 December 2018).
- Ministry of Health; Clinical Trials Research Unit. Clinical Guidelines for Weight Management in New Zealand Children and Young People; Ministry of Health: Wellington, New Zealand, 2009.
- Ministry of Health. Clinical Guidelines for Weight Mangagement in New Zealand Children and Young People; Ministry of Health: Wellington, New Zealand, 2016.
- Scottish Intercollegiate Guidelines Network. Handbook of Disease Burdens and Quality of Life Measures; Springer-Verlag: New York, NY, USA, 2010; p. 4315. [Google Scholar]
- Società Italiana di Pediatria; Società Italiana di Endocrinologia e Diabetologia Pediatrica. Consensus su diagnosi, trattamento e prevenzione dell’obesita del’bambino e dell’adolescente. Available online: https://docs.sip.it/Consensus_Obesita_2017.pdf (accessed on 22 December 2018).
- Academy of Nutrition and Dietetics. Manuel de référence de la terminologie internationale de diététique et de nutrition (TIDN); Presses de l’Université de Laval: Québec, QC, Canada, 2013. [Google Scholar]
- Epstein, L.H.; Valoski, A.; Wing, R.R.; McCurley, J. Ten-Year Follow-up of Behavioral, Family-Based Treatment for Obese Children. JAMA 1990, 264, 2519. [Google Scholar] [CrossRef] [PubMed]
- Vanherle, K.; Werkman, A.; Baete, E.; Barkmeijer, A.; Kolm, A.; Gast, C.; Ramminger, S.; Höld, E.; Kohlenberg-Müller, K.; Ohlrich-Hahn, S.; et al. Proposed standard model and consistent terminology for monitoring and outcome evaluation in different dietetic care settings: Results from the EU-sponsored IMPECD project. Clin. Nutr. 2018, 37, 2206–2216. [Google Scholar] [CrossRef] [PubMed]
- Ford, I.; Norrie, J. Pragmatic Trials. N. Engl. J. Med. 2016, 375, 454–463. [Google Scholar] [CrossRef] [PubMed]
- Graham, I.D.; Logan, J.; Harrison, M.B.; Straus, S.E.; Tetroe, J.; Caswell, W.; Robinson, N. Lost in knowledge translation: Time for a map? J. Contin. Educ. Health Prof. 2006, 26, 13–24. [Google Scholar] [CrossRef] [PubMed]
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).